Prediabetes, Periodontitis and Atherosclerotic Cardiovascular Disease: Associations in a Nested Case-Control study
Eisfeld M1#, Schulte B2,3#, Schlicht K1,3, Mewes L4, Lieb W5, Spille JH6, Naujokat H6, Schreiber S2,3, Dörfer C7, Wiltfang J6, Laudes M1,2,3, Schulte DM1,2,3, Graetz C7, Wagner J3,6*
1Institute of Diabetes and Clinical Metabolic Research, University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany
2Department of Internal Medicine I, University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany
3Cluster of Excellence, Precision medicine in inflammation, Christian-Albrechts-University of Kiel, Kiel, Germany
4Department of Prosthodontics, Geriatric Dentistry and Craniomandibular Disorders, Charité-Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin, Humboldt-Universität zu Berlin and Berlin Institute of Health, Berlin, Germany
5Institute of Epidemiology, Christian-Albrechts-University Kiel, Kiel, Germany
6Department of Oral and Maxillofacial Surgery, University-Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany
7Clinic of Conservative Dentistry and Periodontology, University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany
#Authors contributed equally to this article
*Corresponding Author: Dr. Juliane Wagner, Department of Oral and Maxillofacial Surgery, University-Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany
Received: 23 November 2023; Accepted 04 December 2023; Published: 15 January 2024
Article Information
Citation: Eisfeld M, Schulte B, Schlicht K, Mewes L, Lieb W, Spille JH, Naujokat H, Schreiber S, Dörfer C, Wiltfang J, Laudes M, Schulte DM, Graetz C, Wagner J. Prediabetes, Periodontitis and Atherosclerotic Cardiovascular Disease: Associations in a Nested Case-Control study. Dental Research and Oral Health. 7 (2024): 01-07.
View / Download Pdf Share at FacebookAbstract
Periodontitis and type-2-diabetes are mutually dependent on each other with an increased risk of atherosclerotic cardiovascular disease (ASCVD). Underdiagnosed Prediabetes is also associated with ASCVDs, but without approved therapy. Thus, this study aimed to investigate whether there is an association between periodontitis and prediabetes.
For a systems medicine approach n=746 subjects from the Kiel Food Chain Plus (FoCus)-cohort were included. Mild (n=245) and severe (n=128) periodontitis were compared with case-matched controls (n=373) in occurrence of prediabetes. P-values below 0.05 after adjustment due to multiple testing (Benjamini and Hochberg) were considered statistically significant.
Subjects with severe periodontitis and an assumed prediabetes with a homeostasis model assessment Insulin resistance value between 2 and 5 had significantly higher fasting glucose (102.5[96.25-108.75]mg/dl vs 98[91.5-103] mg/dl;median[IQR];p=0.047). With an extended prediabetes range (glucose 90-125mg/dl) subjects without diabetes and severe periodontitis had significantly higher fasting glucose levels than controls (103[98-109]mg/dl vs 99[93.75-105]mg/dl;p=0.02). Correlations analyses showed that severe periodontitis and fasting glucose in subjects without diabetes with a fasting glucose of 90-125 mg/dl are significantly correlated (r=0.21;p=0.02). ASCVDs were significantly more frequent in cases with periodontitis (overall) and severe periodontitis (OR1.6 and 2.1;p=0.02).
For the first time, a connection between the inflammatory metabolic disease periodontitis and prediabetes could be shown. Our data suggest, that the cutoff for systemic effects on impaired glucose tolerance might be set to lower levels than nowadays, especially for periodontitis. Further studies are indicated to investigate mutual disease triggers and therapy effects. The therapy of periodontitis could represent the first rational therapy of prediabetes.
Keywords
<p>Atherosclerotic cardiovascular disease, ASCVD, Diabetes, Impaired glucose tolerance, Inflammation, Prediabetes, Periodontitis</p>
Article Details
Abbreviations
atherosclerotic cardiovascular disease ASCVD
American Diabetes Association ADA
German Ministry of Education and Research/Bundesministerium für Bildung und
Forschung BMBF
Coronary heart disease CHD
The Kiel Food Chain Plus FoCus
Introduction
Systemic diseases such as diabetes mellitus and atherosclerosis are known to be associated with systemic metabolic inflammation and appear not only to be related to each other, but also to periodontitis [1-3].
Periodontitis patients have a significantly higher risk of developing ASCVD as periodontitis appears to contribute to the inflammation of the arterial wall due to atherosclerotic plaque and also promotes its destabilisation and rupture [4]. Besides, patients with periodontitis have an increased risk of developing diabetes [5]. Furthermore, both, increased gingival inflammation, as an early stage of periodontal inflammation, and periodontitis are found significantly more often in patients with type 1 and type 2 diabetes mellitus [6]. Consequently, diabetes mellitus increases the risk of periodontitis and periodontitis worsens the metabolic metabolism of diabetes [1,7], which can subsequently lead to the development of premature atherosclerotic cardiovascular diseases (ASCVDs) [8,9]. ASCVD is defined by the following diseases: acute coronary syndrome (myocardial infarction, stable and unstable angina pectoris), arterial revascularization, stroke, transient ischemic attack and peripheral arterial disease [16,17].
This is also known for prediabetes and the development of ASCVDs. Prediabetes is defined as an impaired glucose tolerance or impaired fasting glucose and is considered a precursor to diabetes [10]. Based on the fasting glucose values, the American Diabetes Association (ADA) [11] defines prediabetes as 100-125 mg/dl, the World Health Organization (WHO) as 110-125 mg/dl [12]. Both define manifest diabetes among other diagnostic criteria from a fasting glucose of 126 mg/dl. In a large Danish study, Yahyavi et. al could recently show that the highest risk of developing major adverse cardiovascular events was found in subjects with HbA1c just below the diagnostic threshold for diabetes [13]. Only a few studies regarding an impaired glucose tolerance and periodontal diseases are preexistent so far [14]. Moreover, the severity of the hyperglycemia seems to correlate with the severity of the periodontitis [5-7]. Whereby even early prediabetic states with incipient insulin resistance seem to lead to the degradation of periodontal tissue [15].
Thus, the aim of this study was to evaluate associations between periodontitis and an impaired glucose tolerance and to elucidate the connections of the evil triangle (pre-) diabetes, periodontitis and ASCVD.
Methods
FoCus-cohort
The Kiel Food Chain Plus (FoCus) cohort was built up in a period from 2011 to 2014 for population-based research in metabolic inflammation. It was funded by the German Ministry of Education and Research (BMBF) an comprises 1837 individuals in total [16].
Measurement of serum parameters
Phenotyping of the patients and controls regarding body mass index (weight [kg]/height [m]²), glucose [mg/dl] (normal range 55-115 mg/dl), insulin [μU/ml] (normal range 2.6-24.9 µU/ml), Homeostasic Model of Assessment Insulin resistance (HOMA-IR, Insulin [μU/ml] * glucose [mg/dl]/405), lipoprotein(a) [mg/l] (normal range: <300 mg/l) and triglycerides [mg/dl] (normal range: <200 mg/dl) was performed as previously described by our group [16].
Case definitions
Periodontitis
Phenotyping of the dental status was performed for 373 patients and gender-, smoking-, age-, and BMI-matched controls as already published by our group in 2019 [17]. It could be stratified due to severe periodontitis cases with tooth loss (n= 128) and mild periodontitis cases (n=245).
Diabetes and prediabetes
Diabetes cases were defined via self-report in the questionnaire: Did a physician diagnose diabetes?. In addition, this was compared with the answer to further self-reported questions about diabetes: “Which treatment do you get for your diabetes?” and “In which year has your diabetes been diagnosed?”. Two participants had to be excluded due to inconsistent answers.
Due to two different definitions by the ADA and the WHO, subjects with a fasting glucose level on the one hand of <100 mg/dL (ADA) and on the other hand of <110 (WHO) were considered as non-diabetic subjects, when they also indicated that no physician diagnosed a diabetes before, and they additionally did not take any antidiabetic medication.
ASCVD
Phenotyping of ASCVD was performed according to a questionnaire.
The subjects were asked the following questions:
Have you ever had CHD (coronary heart disease) diagnosed?
Did a physician diagnose a myocardial infarction?
How far can you walk without pain?
Did a physician diagnose an apoplexia?
Answering the first three questions in the affirmative, plus a pain-free walking distance under 500m, led to inclusion in the ASCVD group.
Statistical analysis
Statistical analysis and graphics were performed using R [18]. Regarding the descriptive statistics, the t test, the Wilcoxon signed rank test, the Wilcoxon rank sum test, the McNemar test and the χ2 test were used to check for significance. P-values below 0.05 were considered statistically significant. The Pearson correlation coefficient was used in correlation analyzes in form of a point biserial correlation. As part of the multiple testing, the p-values were adjusted using the false discovery rate according to Benjamini and Hochberg.
Results
Prediabetes and diabetes parameters significantly increased in severe periodontitis
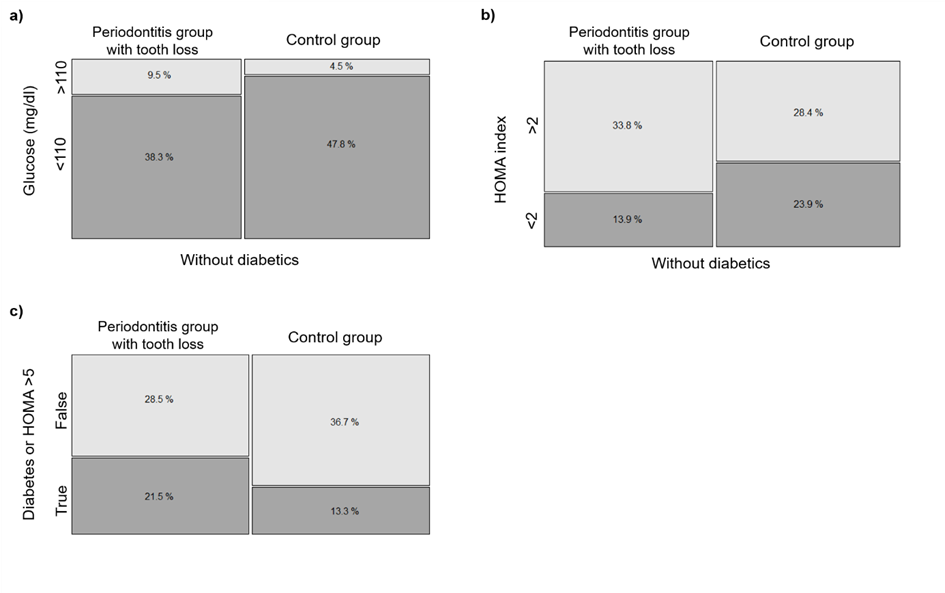
Analysing the periodontal status of participants with no diabetes (n=201) and a fasting glucose <100 [mg/dl] (ADA) or <110 [mg/dl] (WHO) showed that there can significantly fewer periodontitis cases with a severe form found in each group (OR 1.8 and 2.6; p=0.06 and p=0.046) than in each group of subjects with no diabetes and a fasting glucose ≥100 [mg/dl] or ≥110 [mg/dl] (Figure 1a). In the group of subjects without diabetes, there were also significantly fewer subjects with severe periodontitis in the range of HOMA <2 than in the range of HOMA ≥2 (OR 2; p=0.046; Figure 1b).
On the other hand, our diabetes subjects suffered more often on a severe form of periodontitis than the participants without diabetes (OR 1.5, p=0.2), but the significance level was not reached (p>0.05). Adding the HOMA index as a further criterion, it was shown that severe periodontitis was significantly more common in subjects with diabetes or a HOMA index >5 or both than in the remaining subjects (OR 2.1; p=0.027; Figure 1c).
Figure 1: a) Mosaicplot of the relative frequencies of fasting glucose >110 or <110 [mg/dl] and the membership of the subjects to the periodontitis group with tooth loss or to the control group, diabetics excluded (100% corresponds to n=201). p=0.046.
b) Mosaicplot of the relative frequencies of HOMA index >2 or <2 and the membership of the subjects to the periodontitis group with tooth loss or to the control group, diabetics excluded (100% corresponds to n=201). p=0.046.
c) Mosaicplot of the relative frequencies of the presence of diabetes or HOMA index >5 or both and the membership of the subjects to the periodontitis group with tooth loss or to the control group (100% corresponds to n=256). p=0.027.
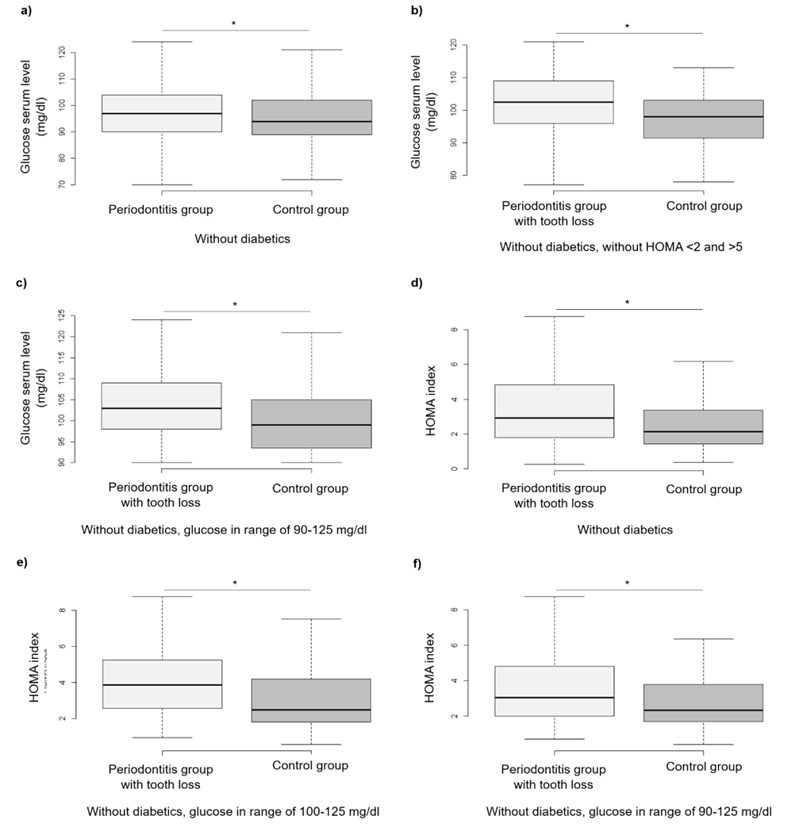
Comparisons with subjects without diabetes showed that in this group subjects with periodontitis had significantly higher fasting glucose levels than subjects without periodontitis (97 [90-104] mg/dl vs 94 [89-102] mg/dl, median [IQR]; p=0.04; Figure 2a). Using the prediabetes range of the ADA, subjects with a fasting glucose of 100-125 mg/dl, without diabetes and severe periodontitis had higher fasting glucose levels than the subjects in the same group without periodontitis (107 [103-111] mg/dl vs 105 [101.5-108.5] mg/dl, median [IQR]; p=0.1), but the significance level was not reached (p>0.05). Subjects without diabetes and severe periodontitis in the prediabetes range based on the HOMA index (HOMA 2-5) showed significantly higher fasting glucose levels than controls without periodontitis in this range (102.5 [96.25-108.75] mg/dl vs 98 [91.5-103] mg/dl, median [IQR]; p=0.047; Figure 2b). With an extended prediabetes range based on fasting glucose of 90-125 mg/dl, subjects without diabetes and severe periodontitis had significantly higher fasting glucose levels than controls without periodontitis (103 [98-109] mg/dl vs 99 [93.75-105] mg/dl, median [IQR]; p=0.02; Figure 2c).
Additionally, correlation analyses showed that severe periodontitis and fasting glucose in subjects without diabetes with a fasting glucose in the range of 90-125 mg/dl are significantly correlated (r=0.2; p=0.02). Whereas correlation analyses for a fasting glucose range of 100-125 mg/dl showed that severe periodontitis and fasting glucose in subjects without diabetes was not significantly correlated (r=0.1; p=0.2).
Moreover, in the group of subjects without diabetes, subjects with severe periodontitis also had significantly higher HOMA values than subjects without periodontitis (2.9 [1.8-4.8] vs 2.1 [1.4-3.4], median [IQR]; p=0.02; Figure 2d). Using again the prediabetes range of the ADA, subjects with a fasting glucose of 100-125 mg/dl, without diabetes and severe periodontitis had higher HOMA values than the subjects in the same group without periodontitis (3.9 [2.6-5.2] vs 2.5 [1.8-4.2], median [IQR]; p=0.035; Figure 2e). Expanding likewise the prediabetes range to 90-125 mg/dl, subjects without diabetes and severe periodontitis had significantly higher HOMA values than controls without periodontitis (3 [2-4.8] vs 2.3 [1.7-3.8], median [IQR]; p=0.02; Figure 2f).
Correlations analyses also showed that severe periodontitis and HOMA index in subjects without diabetes with a fasting glucose in the range of 90-125 mg/dl are significantly correlated (r=0.2; p=0.04). In the fasting glucose range of 100-125 mg/dl, severe periodontitis and HOMA index were not significantly correlated in subjects without diabetes (r=0.2; p=0.07).
Figure 2: a) Box-whisker plot of the fasting glucose serum levels of subjects with (n=300) and without (n=312) periodontitis, diabetics excluded. Values outside the whiskers are not shown. *p=0.04
b) Box-whisker plot of the fasting glucose serum levels of subjects with (n=46) and without (n=47) severe periodontitis, diabetics excluded, range of HOMA index 2-5. Values outside the whiskers are not shown. *p=0.047
c) Box-whisker plot of the fasting glucose serum levels of subjects with (n=70) and without (n=80) severe periodontitis, diabetics excluded, range of fasting glucose 90-125 mg/dl. Values outside the whiskers are not shown. *p=0.02
d) Box-whisker plot of the HOMA indices of subjects with (n=96) and without (n=105) severe periodontitis, diabetics excluded. Values outside the whiskers are not shown. *p=0.02
e) Box-whisker plot of the HOMA indices of subjects with (n=46) and without (n=39) severe periodontitis, diabetics excluded, range of fasting glucose 100 -125 mg/dl. Values outside the whiskers are not shown. *p=0.035
f) Box-whisker plot of the HOMA indices of subjects with (n=70) and without (n=80) severe periodontitis, diabetics excluded, range of fasting glucose 90-125 mg/dl. Values outside the whiskers are not shown. *p=0.02
ASCVDs more frequent in severe periodontitis
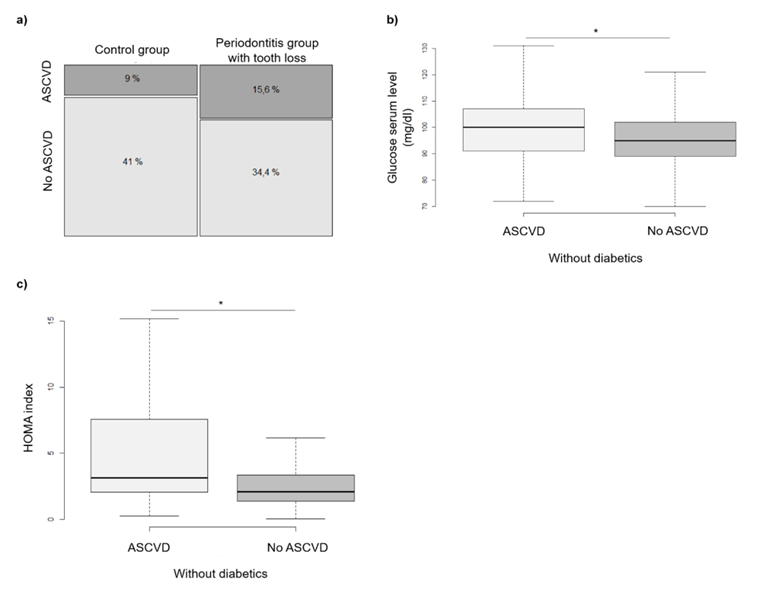
In the combined category 'ASCVD' (stroke, CHD, myocardial infarction and pain-free walking distance under 500m) significant differences could be found. ASCVDs were significantly more common in the entire periodontitis group and in the subgroup with tooth loss and assumed severe periodontitis (p<0.05). The OR was 1.6 (p=0.02) for the entire periodontitis group and 2.1 (p=0.02) for the subgroup with tooth loss (Figure 3a).
Prediabetes and diabetes parameters significantly increased in ASCVDs
Looking at the entire cohort, significant associations between ASCVDs and (pre-) diabetes were also shown. Subjects with ASCVDs had significantly more often diabetes than subjects without ASCVD (OR 4.5; p<0.001). Among subjects without diabetes, those with ASCVD showed significantly higher fasting glucose than those without ASCVD (p<0.05). The fasting glucose mean value of subjects with ASCVDs was 103.7 mg/dl, whereas the mean value of subjects without ASCVDs was 96.9 mg/dl (Figure 3b). Using the prediabetes range of the ADA, in the group of subjects without diabetes and a fasting glucose of 100-125 mg/dl were significantly relatively more cases of ASCVDs than outside this group (OR 1.95; p<0.05). In addition, among subjects without diabetes, those with ASCVDs had higher HOMA values than subjects without ASCVDs (3.15 [2.07-7.57] vs 2.11 [1.38-3.34], median [IQR]; p<0.001; Figure 3c).
Figure 3: a) Mosaicplot of the relative frequencies of the parameter ASCVD and the membership of the subjects to the periodontitis group with tooth loss or to the matched control group (100% corresponds to n=256). p=0.02
b) Box-whisker plot of the fasting glucose serum levels of subjects with and without ASCVD, diabetics excluded. Values outside the whiskers are not shown. * p<0.05
c) Box-whisker plot of the HOMA indices of subjects with and without ASCVD, diabetics excluded. Values outside the whiskers are not shown. * p<0.001
Triglycerides increased in severe periodontitis
Blood lipids, lipoprotein (a) and triglycerides were compared between periodontal groups and controls. There were no significant differences in blood lipid diseases and lipoprotein a in any periodontitis group compared to matched controls.
In the case of triglycerides, subjects with periodontitis and tooth loss showed higher values than their controls (p=0.2; punadjusted=0.04).The mean value of the periodontitis group with tooth loss was 166.2 mg/dl and its controls 132 mg/dl.
Discussion
In our modern, industrialized western-hemisphere diseases on inflammatory basis like diabetes, periodontitis, and ASCVD increase [19].
It is known and accepted that treatment one of them affects the others positively. So, treating the periodontal inflammation can reduce the glycated hemoglobin A1c (Hba1c) [5,7]. High glucose levels seem to directly lead to increased inflammation. In addition, inflammatory cells such as neutrophils, monocytes and dendritic cells are generally increasingly activated in diabetes. Both leading to an increase in systemic inflammation [1,3,6]. It is assumed that the pro-inflammatory cytokines in periodontitis can enter the systemic circulation from the oral cavity and thus worsen the diabetes. Conversely, increased proinflammatory cytokines, which are systemically produced by diabetes, can worsen periodontitis [1].
For the first time, a connection between the inflammatory metabolic diseases periodontitis, prediabetes and ASCVD could be shown for subjects of the Kiel FoCus cohort.
Our data show that severe periodontitis is more prevalent in the presence of elevated fasting blood glucose. However, we also show that this is already the case for blood glucose changes below the common cut-offs for prediabetes (WHO 110 mg/dl, ADA 100 mg/dl). In addition, the analysis in our cohort indicates that in the presence of periodontitis, the median fasting blood glucose was 97 mg/dl and just not above 100 or 110 mg/dl. This suggests a systemic effect of altered blood glucose levels already below the previously common prediabetes diagnostic levels. This fits with the observations of a group from Spain. They describe an increased cardiovascular risk also already below the known prediabetes cut-off [20].
We could also show that ASCVDs were significantly more frequent in the overall periodontitis group and in the subgroup with severe periodontitis. In addition, subjects with severe periodontitis had higher triglycerides than matched controls without periodontitis. Considering the entire cohort, our data also showed a significant connection between (pre-) diabetes and ASCVD as already often described in literature [21,22].
In terms of precision medicine for chronic inflammatory diseases, this could mean that synergies between dentistry and medicine appear helpful for the individual diagnosis and therapy of periodontitis, - already - prediabetes and ASCVD. Further studies are indicated to investigate mutual disease triggers and therapy effects between periodontitis and prediabetes.
The limitations of the study mainly include the data collection as such. Large proportions of the data were collected by self-report in questionnaires, which is why we tried to combine the strongest diagnostic criteria in each case to achieve a case definition. As an internal control, we also compared the patients without diabetes with the periodontitis cases in range of fasting glucose <100/ <110 mg/dl, which showed, as expected, that there were significantly fewer cases here. On the other hand, when diabetes was diagnosed or there was a HOMA value >5 or both, significantly more periodontitis cases were recorded. This is in line with the common sense of today's scientific status and thus demonstrates the quality of our diagnosis selection criteria. In addition, we have already shown in some other studies that the present cohort demonstrates high quality and good selection criteria [16,17].
The treatment of early stages of inflammatory diseases often is a challenge. For early therapy, early diagnoses are needed. On the other hand, we need approved therapies, and last but not least, compliant patients. The therapy of periodontitis could represent the first rational therapy of prediabetes. Moreover, the current case definitions have to be re-considered in the future, especially when it comes to periodontitis.
First, however, it should be noted that even patients who have not yet been diagnosed with prediabetes, but who have elevated fasting glucose levels, are recommended to have regular dental visits in any case.
References
- Khumaedi AI, Purnamasari D, Wijaya IP, et al. The relationship of diabetes, periodontitis and cardiovascular disease. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 13 (2019): 1675-1678.
- Sanz M, Herrera D, Kebschull M, et al. Treatment of stage I-III periodontitis- The EFP S3 level clinical practice guideline. J Clinic Periodontology 47 (2020): 4-60.
- Graves DT, Corrêa JD, Silva TA (2019) The Oral Microbiota Is Modified by Systemic Diseases. Journal of Dental Research 98 (2019): 148-156.
- Hamilton JA, Hasturk H, Kantarci A, et al. Atherosclerosis, Periodontal Disease, and Treatment with Resolvins. Curr Atheroscler Rep 19 (2017): 57.
- Minty M, Canceil T, Serino M, et al. Oral microbiota-induced periodontitis: a new risk factor of metabolic diseases. Rev Endocr Metab Disord 20 (2019): 449-459.
- Huang Z, Pei X, Graves DT. The Interrelationship Between Diabetes, IL-17 and Bone Loss. Curr Osteoporos Rep 18 (2020): 23-31.
- Preshaw PM, Alba AL, Herrera D, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia 55 (2012): 21-31.
- Bahiru E, Hsiao R, Phillipson D, Watson KE. Mechanisms and Treatment of Dyslipidemia in Diabetes. Curr Cardiol Rep 23 (2021): 26.
- Schulte DM, Paulsen K, Türk K, et al. Small dense LDL cholesterol in human subjects with different chronic inflammatory diseases. Nutrition, Metabolism and Cardiovascular Diseases 28 (2018): 1100-1105.
- Hostalek U. Global epidemiology of prediabetes - present and future perspectives. Clin Diabetes Endocrinol 5 (2019): 5.
- American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care 44 (2021): S15-S33.
- World Health organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: Report of a WHO/IDF consultation (2006).
- Yahyavi SK, Snorgaard O, Knop FK, et al. Prediabetes Defined by First Measured HbA1c Predicts Higher Cardiovascular Risk Compared With HbA1c in the Diabetes Range: A Cohort Study of Nationwide Registries. Diabetes Care 44 (2021): 2767-2774.
- Kocher T, König J, Borgnakke WS, et al. Periodontal complications of hyperglycemia/diabetes mellitus: Epidemiologic complexity and clinical challenge. Periodontology 78 (2018): 59-97.
- Timonen P, Saxlin T, Knuuttila M, et al. Role of insulin sensitivity and beta cell function in the development of periodontal disease in adults without diabetes. J Clinic Periodontology 40 (2013): 1079-1086.
- Geisler C, Schlicht K, Knappe C, et al. Cohort profile: the Food Chain Plus (FoCus) cohort. Eur J Epidemiol 37 (2022): 1087-1105.
- Schulz J, Knappe C, Graetz C, et al. Secreted frizzled-related protein 5 serum levels in human periodontitis- A nested case- control study. Journal of Clinical Periodontology 46 (2019): 522-528.
- R Core Team. R: A language and environment for statistical computing (2019).
- International Diabetes Federation. IDF Diabetes Atlas, 10th edn. Brussels, Belgium (2021).
- Rossello X, Raposeiras-Roubin S, Oliva B, et al. Glycated Hemoglobin and Subclinical Atherosclerosis in People Without Diabetes. Journal of the American College of Cardiology 77 (2021): 2777-2791.
- Saeed A, Sun W, Agarwala A, et al. Lipoprotein(a) levels and risk of cardiovascular disease events in individuals with diabetes mellitus or prediabetes: The Atherosclerosis Risk in Communities study. Atherosclerosis 282 (2019): 52-56.
- Sinha A, Ning H, Cameron N, et al. Atherosclerotic Cardiovascular Disease or Heart Failure: First Cardiovascular Event in Adults With Prediabetes and Diabetes. Journal of Cardiac Failure 29 (2023): 246-254.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 76.66%
Acceptance Rate: 76.66%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 