Orthodontic Treatment Combined with Miniscrew Anchorage for an Angle Class II Division 1 Case with Severe Crowding and TMDs
Naoto Hirose*, Makoto Yanoshita, Azusa Onishi, Yuka Yamauchi, Sayuri Nishiyama, Mami Takano, Eri Tsuboi, Naoki Kubo, Kotaro Tanimoto
Department of Orthodontics and Craniofacial Developmental Biology, Hiroshima University Graduate School of Biomedical and Health Sciences, Hiroshima, Japan
*Corresponding Author: Naoto Hirose, Assistant professor, Director of clinic., Department of Orthodontics and Craniofacial Developmental Biology, Hiroshima University Graduate School of Biomedical and Health Sciences, 1-2-3 Kasumi, Minami-ku, Hiroshima 734-8553, Japan
Received: 12 August 2020; Accepted: 21 August 2020; Published: 27 August 2020
Article Information
Citation: Naoto Hirose, Makoto Yanoshita, Azusa Onishi, Yuka Yamauchi, Sayuri Nishiyama, Mami Takano, Eri Tsuboi, Naoki Kubo, Kotaro Tanimoto. Orthodontic Treatment Combined with Miniscrew Anchorage for an Angle Class II Division 1 Case with Severe Crowding and TMDs. Dental Research and Oral Health 3 (2020): 129-140.
View / Download Pdf Share at FacebookAbstract
The case report describes that the treatment of an Angle Class II and division 1 malocclusion in adult with excessive overjet and high mandibular angle case. The patient has also severe crowding on maxilla and mandible and temporomandibular disorders (TMD). The treatment was performed by use of 0.018×0.025-inch slot straight wire appliances with four first premolars’ extraction. The improvement of excessive overjet was achieved by the proclination of anterior teeth by use of temporary anchorage devices (TADs). After completion of orthodontic treatment, the molar relationships on both sides were almost normalized to Class I and proper overjet and overbite were acquired. Improvement of facial and occlusal problems was acquired. The symptoms of TMDs have been stable due to the continuous care through the treatment period. TADs are considered as a very useful material in terms of the anchorage of molars for the achievement of a large amount of incisor retraction and molar intrusion.
Keywords
Orthodontic Treatment, Angle Class II and Division I Malocclusion, TADs, TMD
Orthodontic Treatment articles, Angle Class II and Division I Malocclusion articles, TADs articles, TMD articles
Orthodontic Treatment articles Orthodontic Treatment Research articles Orthodontic Treatment review articles Orthodontic Treatment PubMed articles Orthodontic Treatment PubMed Central articles Orthodontic Treatment 2023 articles Orthodontic Treatment 2024 articles Orthodontic Treatment Scopus articles Orthodontic Treatment impact factor journals Orthodontic Treatment Scopus journals Orthodontic Treatment PubMed journals Orthodontic Treatment medical journals Orthodontic Treatment free journals Orthodontic Treatment best journals Orthodontic Treatment top journals Orthodontic Treatment free medical journals Orthodontic Treatment famous journals Orthodontic Treatment Google Scholar indexed journals Angle Class II and Division I Malocclusion articles Angle Class II and Division I Malocclusion Research articles Angle Class II and Division I Malocclusion review articles Angle Class II and Division I Malocclusion PubMed articles Angle Class II and Division I Malocclusion PubMed Central articles Angle Class II and Division I Malocclusion 2023 articles Angle Class II and Division I Malocclusion 2024 articles Angle Class II and Division I Malocclusion Scopus articles Angle Class II and Division I Malocclusion impact factor journals Angle Class II and Division I Malocclusion Scopus journals Angle Class II and Division I Malocclusion PubMed journals Angle Class II and Division I Malocclusion medical journals Angle Class II and Division I Malocclusion free journals Angle Class II and Division I Malocclusion best journals Angle Class II and Division I Malocclusion top journals Angle Class II and Division I Malocclusion free medical journals Angle Class II and Division I Malocclusion famous journals Angle Class II and Division I Malocclusion Google Scholar indexed journals temporomandibular disorders articles temporomandibular disorders Research articles temporomandibular disorders review articles temporomandibular disorders PubMed articles temporomandibular disorders PubMed Central articles temporomandibular disorders 2023 articles temporomandibular disorders 2024 articles temporomandibular disorders Scopus articles temporomandibular disorders impact factor journals temporomandibular disorders Scopus journals temporomandibular disorders PubMed journals temporomandibular disorders medical journals temporomandibular disorders free journals temporomandibular disorders best journals temporomandibular disorders top journals temporomandibular disorders free medical journals temporomandibular disorders famous journals temporomandibular disorders Google Scholar indexed journals temporary anchorage devices articles temporary anchorage devices Research articles temporary anchorage devices review articles temporary anchorage devices PubMed articles temporary anchorage devices PubMed Central articles temporary anchorage devices 2023 articles temporary anchorage devices 2024 articles temporary anchorage devices Scopus articles temporary anchorage devices impact factor journals temporary anchorage devices Scopus journals temporary anchorage devices PubMed journals temporary anchorage devices medical journals temporary anchorage devices free journals temporary anchorage devices best journals temporary anchorage devices top journals temporary anchorage devices free medical journals temporary anchorage devices famous journals temporary anchorage devices Google Scholar indexed journals
Article Details
1. Introduction
An Angle Class II and division 1 malocclusion in adult
with excessive average and the high mandibular angle case is a difficult case in orthodontic treatment [1, 2]. If the patient had severe crowding or temporomandibular joint disorders (TMD), the treatment would be more difficult to achieve the goal. The molar distalization for gaining the space sometimes occurs the clockwise rotation of mandible and that makes the convex profile worse. Moreover, in patients with TMD, it is important to make orthodontic plans with less burden on TMJ and observe the condition of temporomandibular joint during orthodontic treatment. In addition, the orthodontic treatment for the Japanese patients sometimes become complicated because of their original maxillofacial characteristics that the alveolar bone is relatively small to arrange all teeth in the correct position. Therefore, in order to accomplish the ideal goal of this case, it was necessary to make full use of orthodontic techniques and useful devices and conduct the orthodontic treatment carefully. Orthodontic miniscrew anchorage, which is also called temporary anchorage devices (TADs), has been recently developed and well known the effectiveness even to ordinally people. The device is quite effective to correct severe malocclusions, especially Class II cases, and conduct camouflage treatments [3]. TADs can make it possible to fix molars tightly in the same place, move molars distally, impact teeth without bad side effects. Additionally, TADs work more effectively on intrusion of molars for the case with open bite. On the other hand, intrusion of maxillary molars worsens the excessive overbite in skeletal Class II patients. In such cases, it is a key point how to attain the vertical control of the maxillary anterior teeth.
2. Diagnosis
A 22 years and 2 months old Japanese woman came with complaints which are proclination of incisors on maxilla and severe crowding. The pretreatment extraoral and intraoral photographs (Figure 1) showed a large overjet and severe anterior crowding in mandible. The problems about profile were the facial convexity, a lip protrusion and a difficulty of mouth closure. The pretreatment dental casts (Figure 2) showed large overjet of 10.8 mm and overbite of 3.3 mm, Class III molar relationship of right side and Class II of left side, and arch length discrepancies of -5.0 mm on the maxillary arch and -14.2 mm on the mandibular arch. Occlusion was too unstable to occlude on a forward position or a backward at times. A panoramic radiograph showed that four upper and lower third molars of which especially lower two were placed horizontally. Initial lateral and posteroanterior cephalometric radiographs were taken in centric occlusion. The cephalometric analysis demonstrated a moderate skeletal Class II relationship (ANB angle, 4.6°: SNA angle 80.6 indicates approximately normal and SNB angle 76.0 slightly a retrognathic mandible tendency), retroclinaion of the mandible (FMA, 34.7°). In addition, it presented severe labial inclination of upper (U1 to SN angle, 119.5) and lower (IMPA, 98.3°) incisors, an acute interincisal angle (101.8°) (Figure 3). The patient has been having symptoms of temporomandibular joint (TMJ) for approximately 5 years before initial visit of our clinic. Click noise on the left TMJ in mouth opening was presented at an initial examination. Also, the patient has been realizing pains on left TMJ at times. MR images showed anterior disc displacement on both sides which were irreducible on right TMJ and reducible on left. Moreover, the deformity of mandibular condyles on both side, which are called ‘osteophyte’, were observed. The periphery of left condyle also presented joint effusion which represents inflammation.

Figure 1: Pretreatment extraoral and intraoral photographs of patient.
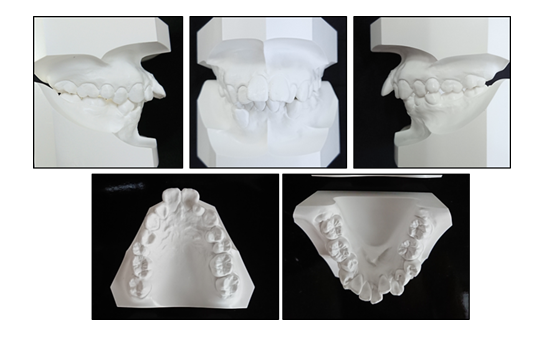
Figure 2: Pretreatment dental casts.
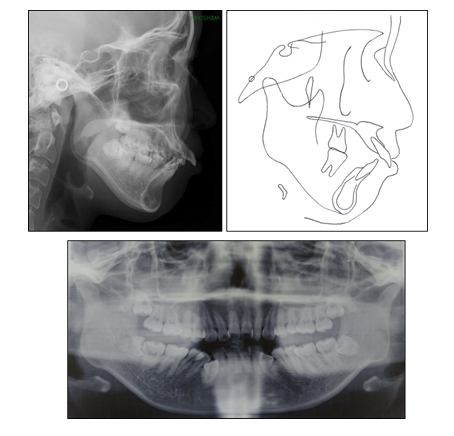
Figure 3: Pretreatment panoramic, lateral cephalometric radiograph and cephalometric tracing.
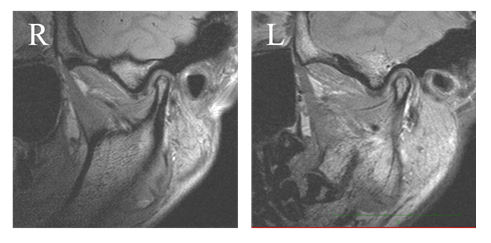
Figure 4: Sagittal MR image of temporomandibular joint.: R, right TMJ L, left TMJ.
3. Treatment Objectives
The main treatment objectives were to normalize overjet and overbite, resolve severe crowding, establish close and tight occlusion with Class I molar relationship, and improve the protrusive facial profile without making TMD worse.
4. Treatment Alternatives
The following orthodontic options were presented to the patient.
- Extract the maxillary and mandibular first premolars. In addition, TADs (Dual-Top Auto Screw, Proseed, Tokyo) on the center of palate were to be used as a maximum anchorage for the retraction of the maxillary anterior teeth and distalization of maxillary molars. TADs were to be put on mandible on both side for distalization of mandibular right molars for the purpose of improvement of mandibular anterior crowding.
- Before starting orthodontic treatment, oral appliance therapy was supposed to be used for the purpose of declining inflammation in TMJ and make the occlusion stable.
The patient presented less skeletal discrepancy (ANB angle, 5°) though it has the excessive overjet. This is a reason why we proposed the normal orthodontic treatment without surgery. After we discussed the treatment plans with the patient, she understood and accepted it.
5. Treatment Progress
Before orthodontic treatment, oral appliance therapy commenced. The use of stabilization type splint was demanded every night when sleeping (Figure 5A). After 6 months use, the unstable occlusion was getting improved gradually through appliance therapy and the frequency of pain of left TMJ was decreasing. Moreover, the mandibular position was sifted slightly backward (1mm) after 6 months therapy, therefore we conducted the minor modification of the treatment plans. First, two TADs (Figure 5B), which the diameter was 2.0 mm and thread length was 6.0 mm, was placed on the middle of the palate under local anesthesia. Two weeks after implantation, transpalatal bar was tied with ligation wires to TADs. Next, 4 first premolars in the maxilla and the mandible were extracted, and 0.018×0.025-inch slot straight wire appliances were placed on both arches. Leveling and alignment were started on maxillo-mandibular dentition with the use of 0.014-inch nickel-titanium wire. After completion initial alignment, the wires replaced into 0.016×0.022 stainless steel archwires and upper and lower canines on both sides were started to retract with elastic chains. Then, 0.016×0.022-inch stainless steel wires were used for an anterior retraction phase. The crimpable hooks, which were put on the mesial portion from lateral teeth bracket on arch wire, were linked to first molar brackets with power chain elastics and the retraction of anterior teeth were started. Anterior excessive overbite was simultaneously corrected by intrusion of maxillary and mandibular anterior teeth using the archwires added bite opening curve (reverse curve) during the retraction phase. About 1 year later, the distal movement of anterior teeth were achieved, and then detailing phase was started. IPC was used for 5 months for the right lower molars distalization. The purpose was to gain the extra space to arrange teeth because the space for alignment was slightly short on lower right dentition. Once the orthodontic objectives had been achieved, the all brackets were removed and fixed appliances were put on the lingual portion of upper and lower anterior teeth. Together with these retainers, Begg type retainer was set on maxilla and clear retainer (splint type for TMD) was on mandible. The patient was instructed to wear the retainers every night when sleeping for several years and then gradually decreasing the wearing time depending on the stability of occlusion.

Figure 5: Treatment progress: A) at the beginning of active treatment; B) canine retraction phase; C) anterior teeth retraction phase.
6. Treatment Results
The patient’s orthodontic problems were almost completely improved through orthodontic treatment. The posttreatment facial photographs showed a good facial proportion. The protrusion of both lips and the mentalis strain on mouth closure were dramatically improved. The intraoral photographs and a dental cast showed that the molar relationships on right side was normalized to Class I and that on left remained slight Class II because of maicrodontia of maxillary left lateral incisor. In addition, proper overjet (from 10.8 mm to 3.0 mm) and overbite (from 3.3 to 1.5 mm) were acquired (Figure 7, 8). A functional occlusion with stable posterior support and adequate anterior guidance were achieved. The difficulty of mouth closure due to the upper incisors’ protrusion was completely improved. The posttreatment cephalometric radiographs (Figure 9)
and the pre-post treatment cephalometric superposition
(Table 1) indicated that the treatment goals have been mostly accomplished. The maxillary incisors were dramatically retroclined and positioned backward (Maxillary incisors distalization was almost 10 mm. U1-SN was decreased 119.5° from 110.3° and U1-AB was decreased from 17.8 mm to 7.9 mm). The mandibular incisors were also retroclined (IMPA was changed from 98.3° to 94.2° and FMIA was changed from 47.1° to 49.5°). The antero-posterior position of maxillary first molars has been kept firmly during the treatment by use of TADs. The severe crowding on lower incisors were well released by combination use of TADs and Class III elastics. Sagittal skeletal pattern was slightly sifted toward more Class II tendency (ANB: from 4.6° to 6.1°, FMA: from 34.7° to 36.3°). The possible reasons of the result were the change of habitual occlusal position and/
or the morphological change of condyle caused by TMD. The posttreatment panoramic X-ray images showed that the maxillary and the mandibular dentition had proper root parallelism with no apparent root and bone resorption. A stable occlusion and balanced profiles have been still maintained for 2 years in retention period.

Figure 6: Posttreatment extraoral and intraoral photographs of patient.

Figure 7: Posttreatment dental casts.
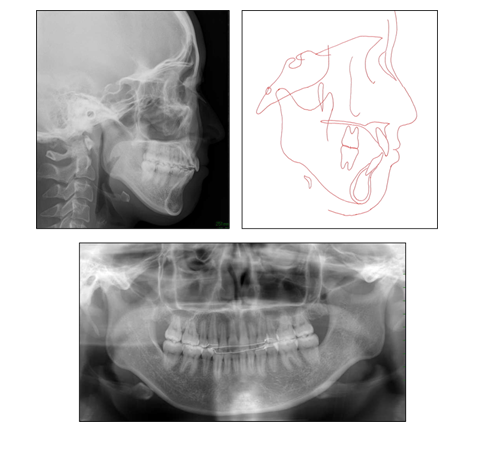
Figure 8: Posttreatment panoramic, lateral cephalometric radiograph and cephalometric tracing.
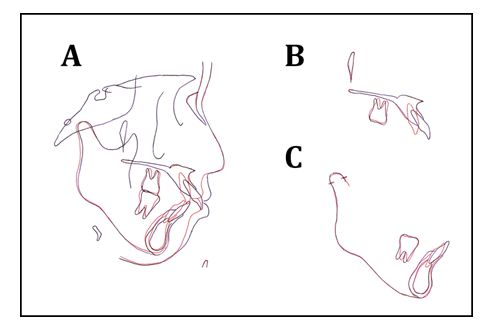
Figure 9: Superimposed tracings of the pretreatment and posttreatment lateral cephalometric radiographs: A) Overall; B) maxilla; C) mandible.
|
Location |
Measurement |
Pretreatment |
Posttreatment |
Norm |
|
Skeltal |
||||
|
Maxilla to cranial base |
SNA (º ) |
80.6 |
80.6 |
79.9 ± 2.4 |
|
Mandible to cranial base |
SNB (º ) |
76 |
74.5 |
77.7 ± 2.7 |
|
Maxillomandibular |
ANB (º ) |
4.6 |
6.1 |
2.9 ± 1.8 |
|
FMA (º ) |
34.7 |
36.3 |
28.8 ± 5.6 |
|
|
Dental |
||||
|
Maxillary dentition |
U1 to SN (º ) |
119.5 |
100.3 |
104.5 ± 7.0 |
|
U1 to AB (mm) |
17.8 |
7.9 |
9.4 ± 2.1 |
|
|
Mandibular dentition |
IMPA (º ) |
98.3 |
94.2 |
91.3 ± 5.4 |
|
FMIA (º ) |
47.1 |
49.5 |
59.9 ± 10.6 |
|
|
L1 to AB (mm) |
6.9 |
4.2 |
6.2 ± 2.1 |
|
|
Intermaxillary dental relationship |
Interincisal angle (º ) |
101.8 |
123.5 |
124.5 ± 11.6 |
Table 1: pre-post treatment cephalometric superposition.
7. Discussion
Maxillary protrusion is one of the most common malocclusions characterized as protrusion of upper lip caused dentally and/or skeletally. This type of malocclusion has a lot of problems which are the high rate of dental trauma [4], the difficulty of mouth closure which leads to bad oral habits [5] and development of TMD [6], besides esthetical problems [7]. The key success factor for improvement of maxillary protrusion is how to effectively maintain the same position of molars without mesial movement and store the space which are gained by premolar extraction. The way to maintain the molar position tightly is generally performed with two orthodontic devices which are head gear or TADs. The use of TADs at present could be the most useful device for making orthodontic treatment predictable, especially for the severe case without surgery [3]. In the present case, TADs which were implanted on palate worked effectively for the achievement of a large amount of anterior teeth movement, a molar anchorage and an intrusion of molars. TADs also be useful for preventing the extrusion of maxillary molars as an opposite reaction of the wire attached with bite opening curve, which contributed to the accomplishment of the impaction of maxillary anterior teeth. This orthodontic approach, which prevents molar extrusion and mandibular clockwise rotation, is necessary for the skeletal Class II case with deep bite and a high mandibular plane angle [3]. Generally speaking, Japanese patients have severe dental discrepancy due to small jawbone and narrow dentition, which sometimes makes orthodontic treatment more complicated and difficult. The Japanese basically presents more convexity of profile compared with Caucasian [8]. The proclination of anterior teeth is considered to be the consequences of dento-skeletal discrepancy on a jaw bone. TADs are necessary for the treatment of such crowding cases or severe maxillary protrusion cases [9].
It has been reported that the case with Angle Class II division 1 with excessive overjet are associated with TMD. We assumed that temporomandibular joint disc derangement, which is considered to be the trigger of development of TMD, occurs easily in Angle Class II division 1 case. That is because the range of antero-posterior functional jaw movement is longer due to the gap between upper and lower incisors. Moreover, oral habits such as bruxism (clenching, grinding, tapping), crunching and unilateral chewing could worsen the symptoms of TMD [10]. In our clinic, all patients with TMD are supposed to examine the condition of TMJ with magnetic resonance imaging (MRI) and receive appliance therapy until the inflammation or deformity of condyle are alleviated. In this case, the both condyles developed the flattening in pretreatment examinations, therefore, the patient received the appliance therapy for 6 months. The use of class II elastics should be refrained as much as possible in order for condyle to be pushed backwardly in the case with TMD and TADs should be used as alternative., though it has not been proved that the connection between the use of intermaxillary class II elastic and the aggravation of TMD [11]. Root resorption is one of the common side effects which causes in orthodontic treatment [12]. It has been reported that the reasons of root resorption were an excessive orthodontic force, a continuous intrusive forth [13], long periods of applied force [14, 15], the proximity between root and cortical bone [16], morphological characteristics of apical root [17] and so forth, however it has been unclear yet. It is considered that root resorption is related to local ischemia around tooth [18, 19], however, it has recently reported root resorption is also related with genetic factors such as P2Rx7 gene [15], IL1-β polymorphism[20], Wnt signaling [21], osteopontin gene SNP [22] and so on. Fortunately, in this case, the posttreatment panoramic radiograph indicated no apparent root resorption in maxillo-mandibular dentition. I assumed that all we can do clinically to avoid severe root resorption during orthodontic treatment is to retract anterior teeth segment carefully without the contact to cortical bone, to use adequate weak fourth in the maxillary protrusion case and to shorten the treatment period.
8. Conclusion
This case report describes a 22-year-old Japanese adult patient who presented with a convex lateral profile, inclination of maxillary anterior incisors, severe discrepancy of mandibular anterior teeth and skeletal class II with retrognathic tendency of mandible. Treatments results achieved the patient’s profile and esthetic goals concerning about as well as intraoral normal overjet and overbite with proper interdigitation from canine to molar relationships.
Conflicts of Interest
The authors declare that they have no Conflicts of interest.
References
- Zhang N, Bai Y, Li S. Treatment of a Class II Division 1 malocclusion with miniscrew anchorage. American journal of orthodontics and dentofacial orthopedics : official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics 141 (2012): e85-e93.
- Pisek P, Manosudprasit M, Wangsrimongkol T, et al. Treatment of a severe Class II Division 1 malocclusion combined with surgical miniscrew anchorage. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics 155 (2019): 572-583.
- Ishida Y, Ono T. Nonsurgical treatment of an adult with a skeletal Class II gummy smile using zygomatic temporary anchorage devices and improved superelastic nickel-titanium alloy wires. American journal of orthodontics and dentofacial orthopedics : official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics 152 (2017): 693-705.
- Zaragoza AA, Catala M, Colmena ML, et al. Dental trauma in schoolchildren six to twelve years of age. ASDC journal of dentistry for children 65 (1998): 492-494, 39.
- Shetty SR, Munshi AK. Oral habits in children--a prevalence study. Journal of the Indian Society of Pedodontics and Preventive Dentistry 16 (1998): 61-66.
- Solberg WK, Bibb CA, Nordstrom BB, et al. Malocclusion associated with temporomandibular joint changes in young adults at autopsy. American journal of orthodontics 89 (1986): 326-330.
- Shell TL, Woods MG. Perception of facial esthetics: a comparison of similar class II cases treated with attempted growth modification or later orthognathic surgery. Angle Orthod 73 (2003): 365-373.
- Shimizu Y, Arx JDV, Ustrell JM, et al. Comparison of cephalometric variables between adult Spanish and Japanese women with Class I malocclusion. Journal of orthodontic science 7 (2018): 19.
- Katada H, Sueishi K. Case of Severe Maxillary Protrusion Accompanied by Crowding and Scissor Bite. The Bulletin of Tokyo Dental College 56 (2015): 243-251.
- Fujita Y, Motegi E, Nomura M, et al. Oral habits of temporomandibular disorder patients with malocclusion. The Bulletin of Tokyo Dental College 44 (2003): 201-207.
- Antunes Ortega AC, Pozza DH, Rocha Rodrigues LL, et al. Relationship Between Orthodontics and Temporomandibular Disorders: A Prospective Study. Journal of oral & facial pain and headache 30 (2016): 134-138.
- Arriola-Guillen LE, Aliaga-Del Castillo A, Ruiz-Mora GA, et al. Influence of maxillary canine impaction characteristics and factors associated with orthodontic treatment on the duration of active orthodontic traction. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics 156 (2019): 391-400.
- Faltin RM, Faltin K, Sander FG, et al. Ultrastructure of cementum and periodontal ligament after continuous intrusion in humans: a transmission electron microscopy study. European journal of orthodontics 23 (2001): 35-49.
- Casa MA, Faltin RM, Faltin K, et al. Root resorption on torqued human premolars shown by tartrate-resistant acid phosphatase histochemistry and transmission electron microscopy. Angle Orthod 76 (2006): 1015-1021.
- Sharab LY, Morford LA, Dempsey J, et al. Genetic and treatment-related risk factors associated with external apical root resorption (EARR) concurrent with orthodontia. Orthodontics & craniofacial research 18 (2015): 71-82.
- Horiuchi A, Hotokezaka H, Kobayashi K. Correlation between cortical plate proximity and apical root resorption. American journal of orthodontics and dentofacial orthopedics : official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics 114 (1998): 311-318.
- Nigul K, Jagomagi T. Factors related to apical root resorption of maxillary incisors in orthodontic patients. Stomatologija 8 (2006): 76-79.
- Melsen B. Biological reaction of alveolar bone to orthodontic tooth movement. Angle Orthod 69 (1999): 151-158.
- Pizzo G, Licata ME, Guiglia R, et al. Root resorption and orthodontic treatment. Review of the literature. Minerva stomatologica 56 (2007):31-44.
- Wu FL, Wang LY, Huang YQ, et al. Interleukin-1beta +3954 polymorphisms and risk of external apical root resorption in orthodontic treatment: a meta-analysis. Genetics and molecular research: GMR 12 (2013): 4678-4686.
- Lim WH, Liu B, Hunter DJ, et al. Downregulation of Wnt causes root resorption. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics 146 (2014): 337-345.
- Iglesias-Linares A, Yanez-Vico RM, Moreno-Fernandez AM, et al. Osteopontin gene SNPs (rs9138, rs11730582) mediate susceptibility to external root resorption in orthodontic patients. Oral diseases 20 (2014): 307-312.


 Impact Factor: * 3.1
Impact Factor: * 3.1 Acceptance Rate: 76.66%
Acceptance Rate: 76.66%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 