Predictors of Dental Care Services Before and After the onset of the Covid-19 Pandemic among undergraduates at a U.S. University
Alvarez V1*, Short JL2, Weinstein AA3, Deakin TK2, Mejia PJ2, Maciarz J2, Dhaliwal SK1, Lokko F1, Farid Azar S1, de Jonge E1, Cheskin LJ1
1Department of Nutrition and Food Studies, College of Public Health, George Mason University, Fairfax, VA, USA
2Department of Psychology, George Mason University, Fairfax, VA, USA
3Department of Global and Community Health, George Mason University, Fairfax, VA, USA
*Corresponding Author: Vanessa Alvarez, Department of Nutrition and Food Studies, College of Public Health, George Mason University, Fairfax, VA, USA.
Received: 15 July 2025; Accepted: 22 July 2025; Published: 28 July 2025
Article Information
Citation: Alvarez V, Short JL, Weinstein AA, Deakin TK, Mejia PJ, Maciarz J, Dhaliwal SK, Lokko F, Farid Azar S, De Jonge E, Cheskin LJ. Predictors of Dental Care Services Before and After the onset of the Covid-19 Pandemic among undergraduates at a U.S. University. Dental Research and Oral Health. 8 (2025): 85-91.
View / Download Pdf Share at FacebookAbstract
Objective: To analyze predictors of dental service use over 2 years among students aged 18-24 at a large public university.
Methods: Participants were 349 first-year students from the 2019 cohort of the Mason Health Starts Here longitudinal study. We examined measures of enabling or impeding factors, such as health resources, family characteristics, psychological functioning, health behaviors, and self-rated health to predict receipt of dental services in 2019 and 2021.
Results: Approximately 75% of students received dental exams in the year before entering college (pre-pandemic) and 74% reported dental exams two years later, after the onset of the COVID-19 pandemic. There was a trend for females to receive more dental services than males after the onset of the pandemic, not before. We found significant relationships between receiving dental exams and eye exams, physical exams, possessing health insurance, self-rated health, and anxiety. Receiving eye exams, health insurance, and self-rated health explained significant unique variance in receiving dental exams at time 1 (T1). T1 dental exams correlated significantly with completing dental exams two years later. Receiving dental exams, financial support from parents, and a sense of hope explained significant unique variance in self-rated health at T1.
Conclusions: Health behaviors of completing multiple types of medical exams, resources such as health insurance, and psychological characteristics such as self-rated health and anxiety were related to completing dental exams. Increased access to health insurance and habitual use of medical services were found to help enable and motivate increased use of preventive dental services.
Keywords
<p>Dental services, Physical exams, Health insurance, Self-rated health, Anxiety, Young adults</p>
Article Details
Introduction
Young adulthood in the U.S. has often been characterized as emerging adulthood which suggests a gradual process of exploration of different roles and identities over time. Young adults from marginalized populations (e.g., low income or ethnic/racial minority groups) sometimes experience an accelerated adulthood in that they assume adult roles (e.g., leaving home, entering labor force full-time, and becoming parents) earlier than their more privileged counterparts or a prevented adulthood where they lack the opportunities to assume adult roles [1-3]. Young adulthood is usually a time of increasing independence and assuming responsibilities for personal health behaviors.
Andersen proposed a behavioral model of health services to explain pursuit of medical care [4]. It included individual and contextual factors divided into predisposing factors (i.e., those linked with desire for care, like social factors (i.e., education or social ties) and biological factors (i.e., sex or age)), enabling resources such as perceived access to health care or disposable income (i.e., financial and organizational factors that could affect use of health care services), and need factors such as perceived (i.e., self-rated, subjective health) and evaluated health (i.e., illnesses diagnosed by provider). Evolutions of the model included consideration of the health care system, elaborated measures of health service use, and consumer satisfaction (phase 2), and health status outcomes that allowed for measurements of access to include dimensions relevant to health policy and health reform (phase 3) [5]. The most recent version of the model emphasizes the dynamic and recursive nature of health services use, including feedback loops, and the importance of understanding individual determinants in the context of the community. Overall, the final model examines access to medical care based on predisposing, enabling, and need contextual and individual characteristics, health behaviors, and outcomes such as perceived health [6].
One recent study explored the factors associated with dental service based on the Andersen Model of health services [7]. This review of 41 studies, included 10 on children/adolescents and 31 on adults from countries across South America, North America, Europe, Asia, and Africa. Based on mostly observational and cross-sectional studies, they assessed dental service use in a continuum between the last six months to ever visiting a dentist. They concluded that certain predisposing characteristics, enabling resources, and need factors are associated with dental services among children, whereas results are more mixed for adults when assessing correlates such as age, gender, education, ethnicity, and income for dental service use. Children/adolescents’ dental service use was associated with higher age, higher income, and greater oral health needs. In adults, they noted that half the studies found an association between increased education and increased dental service use and reviewed studies indicated a positive association between social support and usual source of care and dental service use. Moreover, 6 of 10 studies found a positive association between oral health problems in adults and dental service use, whereas 4 others found no such association. In both child and adult groups, need factors alone did not fully explain use. Study authors concluded that longitudinal studies and studies that explore psychosocial and personality-related factors are required to clarify determinants of dental service use.
A scoping review focusing mostly on articles published between 2016 and 2020 concluded that the research to date is still lacking about the conceptual links and feedback loops based on the Andersen model, proposing the need for more comprehensive research to assess the topic. Results showed that income (84.6%) and insurance status (59.6%) were the most frequently studied enabling factors [8].
The Mason Health Starts Here prospective cohort study of college students includes a variety of psychosocial measures including parental education, financial support, and health insurance of participants, and health behaviors including medical exams, sleep, and alcohol use, and perceived physical and mental health measures [9]. Longitudinal analyses allow examination of the health-related behaviors of these college students with college progress and performance.
Given the age of our sample, consisting of young adults 18-24 years of age, we wanted to assess whether a group of university students are more similar to children or middle-aged adults in the predictors of their dental service use. We also wanted to include some variables about psychological functioning to expand the Andersen Model of health services.
We hypothesized that student's completion of dental, eye, and physical health exams would be related to each other and to self-rated health indicating preventive efforts to maintain good physical health. We also hypothesized that students’ dental exams, personal health insurance, financial support from parents, perceived stress, anxiety, sense of hope, alcohol use, and sleep quality would be related to self-rated health.
Materials and Methods
Participants
The sample from the 2019 Mason cohort included 349 first-year students and 65.6% female and 34.4% males. The age range was 18 to 24 (98% were aged 18 or 19). The sample was 37.2% white, not Hispanic, 12.6% white Hispanic, 24.6% Asian, 11.3% black, not Hispanic, 1.7% black Hispanic, 7.8% two or more races, and 4.8% other identified race students. These percentages were similar to the university population. For fathers’ highest educational level, 6.7% completed some high school, 15.7% were high school graduates, 12.7% completed some college, 3.2% completed an associate’s degree, 21.1% completed college, 26.9% completed a graduate degree, and 13.7% were missing. For mothers’ highest educational level, 8.5% completed some high school, 13.7% were high school graduates, 10.4% completed some college, 6.2% completed an associate’s degree, 27.6% completed college, 20.1% completed a graduate degree, and 13.4% were missing.
Procedures
This study was approved by the university Institutional Review Board and conducted with young adults beginning to study for undergraduate degrees at George Mason University in Virginia. First-year students were recruited via flyers, class presentations, online videos, and individual emails. The first cohort of the study began in the Fall 2019 semester, pre-pandemic, as part of a longitudinal study. The overall response rate was 31% (349/1131) recruited from the population of 3,763 new students and was generally representative of the university. Questionnaires were offered each year as the students progressed through college. There were also optional physical exams and blood tests during the first and fourth years.
Measures
Physical exam completion was assessed with single items designed for the study: “Thinking about the last 12 months, did you see a doctor, nurse, or other health professional for the following: dental, eye, and physical” exams (no = 0 and yes = 1).
Insurance coverage was assessed with the question: What is your primary source of health insurance? There were 8 options. The response “I don’t have health insurance” was scored a 0 and any source of health insurance was scored a 1 for the presence of health insurance.
Financial support was assessed with the question: Do you receive any financial support? The response choices were 1 = Not at all, 2 = Have minimum support, 3 = Have support, 4 = Have good support, and 5 = Have very good/generous support.
Anxiety symptoms were measured with the Patient Reported Outcomes Measurement Information System [10]. The PROMIS assesses individual functioning across various domains of well-being and has been extensively validated in multiple age groups (including young adults) as part of a large multi-year initiative by the National Institute of Health. Respondents report their experiences of these emotions over the past 7 days using a 5-point Likert scale (‘Never’ to ‘Always’). Internal consistency was 0.95 for this study.
Self-rated health (SRH) was measured with one item that asked, “Would you say your health is excellent, very good, good, fair, or poor?” Responses range from 1 (poor) to 5 (excellent). SRH is strongly correlated with objective health status [11]
Alcohol use was measured with the Alcohol Use Disorders Identification Test (AUDIT) [12]. A 10-item scale assessing alcohol consumption, drinking behaviors, and alcohol- related problems, which is used to identify individuals at risk of an alcohol use disorder [10]. The psychometric properties of the AUDIT have been examined in multiple age groups, including undergraduate drinkers. Internal consistency is above 0.70 for these samples.
Sleep Quality was measured with the Brief Pittsburgh Sleep Quality Index (B-PSQI). The 6 item B-PSQI was taken from the larger 19 item PSQI [13,14]. The items from the B-PSQI form five of the original six component scores that range from 0 to 3 points. Some items require filling in blanks, and others have four choices to measure sleep quality, latency, duration, efficiency, and disturbances. The B-PSQI was shown to have good internal consistency and reliability (alpha = 0.81, omega = 0.85) and good convergent validity.
Perceived stress was measured by a 4-item questionnaire on a 5-point Likert scale adapted from Cohen et al.’s Perceived Stress Scale [15]. Participants are prompted with items that assess the extent to which they perceive situations in their life as being stressful. Each item is rated from 1 (‘very often’) to 5 (‘never’). High scores indicated more perceived stress. Positively stated items (e.g., “how often do you feel capable of handling a stressful event?”) are reverse coded. We found an internal consistency of 0.84 for this study.
Hope was measured with the 8-item Adult Hope Scale [16]. The AHS measures two facets of hope: Agency, or goal-directed energy and Pathways, or planning to meet goals. Items are rated from 1 (definitely false) to 8 (definitely true). We found an internal consistency of 0.87 for this study.
Participants’ grade point average for the first semester of college was obtained from the university registrar.
Data analysis
Data was analyzed using SPSS. We analyzed self-reports of whether students completed dental, physical, and eye exams, family characteristics, psychological functioning, health resources, health behaviors, and self-rated health. Correlational analyses were conducted to examine associations between receiving dental exams and other study variables.
Results
Descriptive statistics including means, standard deviations, minimum and maximum observed values were computed and are presented in table 1.
|
Variable |
N |
Mean |
Standard Deviation |
Minimum |
Maximum |
Possible Range |
|
T1 Dental Exams |
319 |
0.749 |
0.434 |
0 |
1 |
0 – 1 |
|
Eye Exams |
316 |
0.594 |
0.492 |
0 |
1 |
0 – 1 |
|
Physical Exams |
321 |
0.854 |
0.354 |
0 |
1 |
0 – 1 |
|
Insurance Coverage |
343 |
0.936 |
0.245 |
0 |
1 |
0 – 1 |
|
Financial Support |
349 |
3.1 |
1.302 |
0 |
5 |
0 – 5 |
|
Anxiety |
349 |
2.442 |
0.928 |
1 |
5 |
1 – 5 |
|
Self-Rated Health |
338 |
3.25 |
0.949 |
1 |
5 |
1 – 5 |
|
Alcohol Use |
346 |
1.61 |
3.031 |
0 |
17 |
0 - |
|
Sleep Quality |
293 |
4.44 |
2.798 |
0 |
14 |
0 – 14 |
|
Perceived Stress |
341 |
2.687 |
0.75 |
1 |
4.95 |
1 – 5 |
|
Hope |
321 |
6.156 |
1.022 |
2.75 |
8 |
1 – 8 |
|
Grade Point Average |
276 |
3.23 |
0.673 |
0.6 |
4 |
0 – 4 |
|
T2 Dental Exams |
89 |
0.742 |
0.44 |
0 |
1 |
0 – 1 |
Table 1: Observed Means, Standard Deviations, and Ranges for Study Variables
In preliminary analyses, we found no sex differences in completion of health exams and no relationship between either mother’s or father’s education level and completion of health exams at time 1 in 2019 or time 2 in 2021. At time 2 in 2021, there was a trend for females to get more dental exams than males did (t = 1.937, p = 0.056).
We found significant correlations between receiving dental services at time 1 and eye exams (0.198), physical exams (0.159), health insurance (0.147), anxiety (-0.127), self-rated health (0.171), and anxiety (-0.127) as noted in table 2. Time 1 receipt of dental exams in 2019 was correlated .556 with Time 2 dental exams in 2021. There were no other time 1 variables correlated with receiving dental exams at time 2 in 2021.
We found significant correlations between self-rated health and receiving dental exams (0.171), financial support (0.155), sleep problems (-0.181), anxiety (-0.229), perceived stress (-0.315), and perceptions of hope (0.364).
Note: p<0.05 (*), p<0.01 (**), p<0.001 (***)
Table 2: Correlations Between Study Variables
Multiple regression analyses of variables significantly correlated with dental exams showed that they explained 9% of the variance in receiving dental exams (F = 5.613, p < 0.001). Receiving eye exams, having health insurance, and self-rated health explained significant unique variance in receiving dental exams as shown in table 3. There was also a trend for physical exams to explain unique variance in receiving dental exams (p = 0.057).
|
R |
R2 Change |
F |
Beta |
t |
p-value |
|
|
Predictors as a Set |
0.3 |
0.09 |
5.613 |
<.001*** |
||
|
Eye Exams |
0.155 |
2.721 |
.007** |
|||
|
Physical Exams |
0.109 |
1.911 |
0.057 |
|||
|
Having Insurance |
0.124 |
2.175 |
.030* |
|||
|
Self-Rated Health |
0.119 |
2.028 |
.043* |
|||
|
Anxiety |
-0.074 |
-1.28 |
0.202 |
Table 3: Cross-sectional Regression Analyses of Predictors of Dental Exams at Time 1.
Multiple regression analyses of variables significantly correlated with self-rated health showed that they explained 19% of the variance in self-rated health (F = 10.005, p < .001). Receiving dental exams, financial support, and hope explained significant unique variance in self-rated health as shown in table 4.
|
R |
R2 Change |
F |
Beta |
t |
p-value |
|
|
Predictors as a Set |
0.431 |
0.186 |
10.005 |
<.001*** |
||
|
Dental Exams |
0.155 |
2.601 |
.010* |
|||
|
Financial Support |
0.165 |
2.949 |
.003** |
|||
|
Sleep Problems |
-0.062 |
-1.06 |
0.29 |
|||
|
Anxiety |
0.009 |
0.129 |
0.898 |
|||
|
Perceived Stress |
-0.092 |
-1.163 |
0.246 |
|||
|
Hope |
0.27 |
4.057 |
<.001*** |
Note. * = p < .05; ** = p < .01; *** = p < .001.
Table 4: Cross-sectional Regression Analyses of Predictors of Self-Rated Health at Time 1.
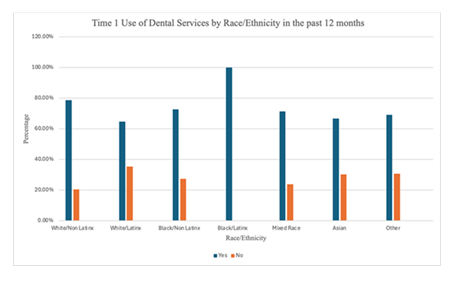
Figure 1: Shows the use of dental services by race/ethnicity in the past 12 months. We conducted a chi-square analysis to compare the groups and there were no significant differences.
Discussion
The majority of participants in our study reported getting dental exams at time 1 (75%) and time 2 (74%) two years later. This is comparable to previous research. A study focusing on the dental health practices of more than one million U.S. college students found that 76.6% reported a dental exam and cleaning in the last year [17]. Receipt of time 1 dental exams before the pandemic was the only significant predictor of receiving dental exams 2 years later. This suggests the importance of developing regular schedules for medical services and is something that medical providers can facilitate by scheduling future appointments at the time of exams. In our study, there was a trend for more females than males to have annual dental visits after the COVID-19 pandemic started. Previous studies have found that men are less likely to seek preventive treatment with respect to dental exams, blood pressure monitoring, and serum cholesterol monitoring [18].
Predictors of Dental Exams
We found that receiving dental exams was significantly related to receiving eye exams and physical exams, possessing health insurance, self-rated health, and anxiety. When examining these variables together, eye exams, health insurance, and self-rated health explained significant unique variance in receiving dental exams. This is consistent with some of the proposed predisposing and enabling factors in the Andersen model [5]. Access to preventive healthcare services at universities is an important factor in the use of such services by students. Interventions that improve the use of healthcare services could include having a same-day walk-in policy, multiple ways to schedule appointments, advertising the high quality of primary prevention health services, and increasing accessibility for students. In a study of U.S. adolescents, logistic regression analyses revealed that lack of insurance, low family income, and low parental education level were significantly associated with the lack of preventive medical care [19]. Our study did not find parental education related to receiving any of the medical exams. In another study analyzing predictors of dental care use, Whites and Asians had a 10-20% higher proportion of dental service utilization at most ages compared with Blacks and Hispanics [20]. These effects decreased when they were adjusted for current income, insurance, and education. Being non-cisgender, non-Hispanic black, Hispanic, and receipt of free or reduced lunch were associated with less frequent dental visits [21]. There were no significant differences of receiving dental exams by race/ethnicity in our study. One study found that uninsured African American and Latinx populations use more preventive care in comparison to uninsured white populations [22].
Insurance coverage, socioeconomic factors, access to care on campus, and parental financial support may also affect the use of preventive healthcare services. Access to insurance appears to contribute to the contextual impacts of socioeconomic and racial disparities in the use of preventive services. Another study showed that socioeconomic positions were related to dental treatment, oral behaviors, and mental health [23]. It is also important to note that receiving an eye or physical exam has an impact on the number of those that have dental exams. It is often the primary health care provider who sees young people before they see a dental care professional and can encourage preventive health care [24]. Individuals with lower educational attainment were found to rely on their primary care providers for care [25]. Those attending 4-year universities are more likely to have had dental care in the previous year than students attending a 2-year college [17]. In addition, students at public universities reported more dental care in the previous year than those attending a private university.
Predictors of Self-Rated Health
Receiving dental exams, financial support, and hope explained significant unique variance in self-rated health. We examined self-rated health as an outcome because the Andersen model uses perceived health as an outcome. Regular dental exams help facilitate physical health. Psychological strengths like hope which measured both pathways (planning to meet goals) and agency (goal-directed energy) help provide motivation to maintain and improve physical and mental health. Previous research has found that high hope is linked to healthy behaviors such as fruit and vegetable consumption, being a nonsmoker, physical activity, and engaging in behavioral strategies for diet (such as portion control and limiting fat intake) [26]. Higher levels of education and having a usual source of care were both associated with greater use of preventive services [25].
Another important factor that may have affected use of preventive health care services was the COVID-19 pandemic, which began soon after the first year of data gathering for the Mason Cohort Study. A prior study found that after the COVID-19 pandemic began, there was a decrease in the delivery of preventive care services, which may cause delayed diagnoses with an increased mortality and increased health care costs [27].
We did not find a relationship between grade point averages and dental exams or self-rated health for the first semester of college. Other research has shown that high academic performance is positively related to physical, psychological health, social relations, and environment [27]. Perhaps we will see academic performance related to health later in college. We found evidence that anxiety was associated with dental exams. A study of late teenagers in India indicated 12-14 years as the mean age of first dental visit, with moderately high levels of anxiety (60.75%) for various dental procedures [28]. Only 4.16% had regular dental consultations, and 78.3% reported that general check-ups evoked anxiety. It is also important to consider the level of care that is available to students on campus, as students with better access to health services on campus also tend to have higher treatment use and the campus environment may help reduce anxiety [29].
Limitations
Limitations of the study included a somewhat small sample that could limit the generalizability of the results. Most measures were collected through self-reports that may be affected by social desirability and memory biases. Another limitation is the somewhat brief duration of the study over two years. There was substantial attrition in study participants two years later that limited power to detect significant relationships between the two time points. However, the study showed that the percentage of students receiving dental exams stayed stable from the time before the onset of the COVID-19 pandemic to the time afterward. Health behaviors such as nutritious food consumption, exercise, and reduced sitting should be studied in the context of the Andersen model and were not included in this study.
Conclusion
There were positive relationships between health insurance coverage and receiving dental, eye, and physical exams. Receiving physical exams, eye exams, and health insurance explained significant unique variance in receiving dental services. This suggests that improving access to these services may increase preventive dental care. There have been attempts to increase funding for preventive care of public-school students; however, the cost is a barrier. The next step in research is to assess whether the relationships between our study variables continue longitudinally over the course of the undergraduate years, and to examine the processes by which that happens.
References
- Lee JS, Waithaka EN. The intersections of marginalized social identities in the transition to adulthood: A demographic profile. Emerging Adulthood 5 (2017): 151-163.
- Hendry LB, Kloep M. Conceptualizing Emerging Adulthood: Inspecting the Emperor’s New Clothes? Child Development Perspectives 1 (2007): 74-79.
- Lee JS. An institutional framework for the study of the transition to adulthood. Youth & Society 46 (2014) 706-730.
- Andersen RM. Families’ use of health services: a behavioral model of predisposing, enabling, and need components (1968).
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter?. J Health Soc Behav 36 (1995): 1-10.
- Andersen RM. National health surveys and the behavioral model of health services use. Med Care 46 (2008): 647-653.
- Hajek A, Kretzler B, König HH. Factors Associated with Dental Service Use Based on the Andersen Model: A Systematic Review. Int. J. Environ. Res. Public Health 18 (2021): 2491.
- Zardak AN, Amini-Rarani M, Abdollahpour I, et al. Utilization of dental care among adult populations: a scoping review of applied models. BMC Oral Health 23 (2023): 596.
- Cuellar AE, Adams LM, de Jonge L, et al. Protocol for the Mason: Health Starts Here prospective cohort study of young adult college students. BMC Public Health 21 (2021): 897.
- Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol 63 (2010): 1179-1194.
- Meng Q, Xie Z, Zhang T. A single-item self-rated health measure correlates with objective health status in the elderly: a survey in suburban beijing. Front Public Health 2 (2024): 27.
- Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction 88 (1993): 791-804.
- Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28 (1989): 193-213.
- Sancho-Domingo C, Carballo JL, Coloma-Carmona A, et al. Brief version of the Pittsburgh Sleep Quality Index (B-PSQI) and measurement invariance across gender and age in a population-based sample. Psychological Assessment 33 (2020): 111-121.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior 24 (1983): 385.
- Snyder CR, Harris C, Anderson JR., et al. The will and the ways: Development and validation of an individual-differences measure of hope. Journal of Personality and Social Psychology 60 (1991): 570-585.
- Dewald, Lori EdD, ATC, et al. Dental Health Practices in US College Students: The American College Health Association-National College Health Assessment Findings. Journal of Health Disparities Research and Practice 9 (1991): 3.
- Vaidya V, Partha G, Karmakar M. Gender differences in utilization of preventive care services in the United States. J Womens Health (Larchmt) 21 (2021): 140-145.
- Yu SM, Bellamy HA, Schwalberg RH, et al. Factors associated with use of preventive dental and health services among U.S. adolescents1 1The opinions expressed in this paper are the authors’ and do not necessarily reflect the views or policies of the institutions with which the authors are affiliated. Journal of Adolescent Health 29 (2001): 395-405.
- Okunseri C, Okunseri E, Garcia RI, et al. Predictors of dental care use: Findings from the National Longitudinal Study of Adolescent Health. Journal of Adolescent Health 53 (2013): 663-670.
- Zhang L, Waselewski M, Nawrocki J, et al. Perspectives on dental health and oral hygiene practice from US adolescents and young adults during the COVID-19 pandemic. Plos One 18 (2023): e0280533.
- Cruden G, Kelleher K, Kellam S, et al. Increasing the Delivery of Preventive Health Services in Public Education. Am J Prev Med 51 (2016): S158-S167.
- Heaton LJ, Santoro M, Tiwari T, et al. Mental Health, Socioeconomic Position, and Oral Health: A Path Analysis. Prev Chronic Dis 21 (2024): E76.
- Kennedy B, Brunick A, Nilson W. Increasing access to dental care through primary health care prodiver education. Journal of Dental Hygiene (2007).
- Goodman MS, Sanders Thompson VL, Johnson CA, et al. Evaluating community engagement in research: Quantitative measure development. J Community Psychol 45 (2017): 17-32.
- Berg CJ, Ritschel LA, Swan DW, et al. The role of hope in engaging in healthy behaviors among college students. American journal of health behavior 35 (2011): 402-415.
- Laing S, Johnston S. Estimated impact of COVID-19 on preventive care service delivery: an observational cohort study. BMC Health Serv Res 21 (2021): 1107.
- Bhola R, Malhotra R. Dental Procedures, oral practices, and Associated Anxiety: A study on Late-teenagers. Osong Public Health and Research Perspectives 5 (2014): 219-232.
- Health and Academics | Healthy Schools | CDC (2025).
Article Views: 944
Journal Statistics




Discover More: Recent Articles
Grant Support Articles
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved!