A Case of Cytomegalovirus Corneal Endotheliitis in a Juvenile Male with a History of Repeated Intraocular Hypertension
Hisataka Fujimoto*, Junichi Kiryu
Department of Ophthalmology, Kawasaki Medical School, 577 Matsushima, Kurashiki, 701-0192 Okayama, Japan
*Corresponding author: Hisataka Fujimoto, Department of Ophthalmology, Kawasaki Medical School, 577 Matsushima, Kurashiki, 701-0192 Okayama, Japan.
Received: 16 June 2022; Accepted: 24 June 2022; Published: 29 June 2022
Article Information
Citation: Hisataka Fujimoto, Junichi Kiryu. A Case of Cytomegalovirus Corneal Endotheliitis in a Juvenile Male with a History of Repeated Intraocular Hypertension. Journal of Ophthalmology and Research 5 (2022): 117-120.
DOI: 10.26502/fjor.2644-00240066
View / Download Pdf Share at FacebookAbstract
Purpose: Here we report a case of cytomegalovirus corneal endotheliitis in the right eye of a young boy with a history of repeated intraocular hypertension.
Observations: The patient’s right eye had a history of four episodes of cytomegalovirus corneal endotheliitis with the intraocular hypertension. His ages at these occurrences were 9.91, 10.03, 12.12, and 12.67 years. In each event, keratic precipitates including coin-shaped lesions, the cytomegalovirus characteristic types of keratic precipitates, focal corneal stromal edema coincidence with coin-shaped lesions were observed and diagnosed as cytomegalovirus corneal endotheliitis with trabecular meshwork inflammation that caused the intraocular hypertension. In each event, topical ophthalmic solutions including 0.1% betamethasone 5 times a day and 0.4% ripasudil twice a day led to remission within 7 days. At the last cytomegalovirus corneal endotheliitis recurrence, cytomegalovirus was detected in the aqueous humor by qualitative polymerase chain reaction at the concentration of 1.78×104 copies/mL
Conclusion and Importance: In this case, cytomegalovirus corneal endotheliitis occurred at 9 years of age. To the best of our knowledge, this patient is the youngest reported worldwide.
Keywords
<p>cytomegalovirus, corneal endotheliitis, juvenile, intraocular hypertension</p>
Article Details
1. Intruduction
Corneal endotheliitis, characterized and defined as localized corneal oedema with keratic precipitates (KPs), often results in severe corneal endothelial dysfunction (1,2). In 2006, Koizumi et al. reported the first case of cytomegalovirus (CMV)-related corneal endotheliitis in which CMV DNA was detected in aqueous humor by polymerase chain reaction (PCR) (3). CMV has received focus as the factor causing anterior segment inflammation in immunocompetent eyes suffering from inflammatory diseases such as uveitis with and without ocular hypertension (4,5). CMV is considered an important factor in corneal endotheliitis (6–8). Clinical or observational knowledge of CMV-related endotheliitis is continuously increasing and accumulating (6–11). Early diagnostic actions and resulting early phase interventions and treatments have been proposed (12–14). Here we report the youngest CMV-related endotheliitis case to date. Only the right eye was involved, and the patient had a history of endotheliitis accompanied by four episodes of ocular hypertension.
2. Case Description
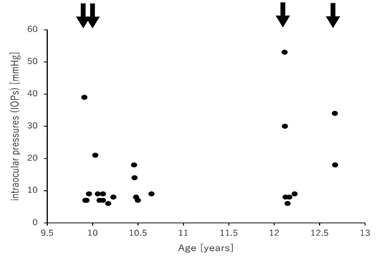
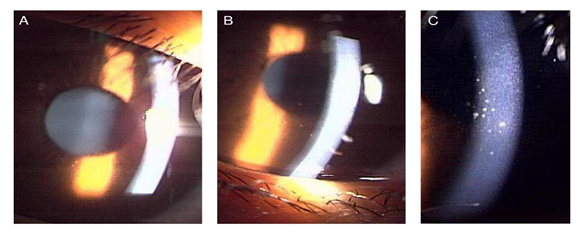
This case involved a young boy with no previous medical history or systemic diseases. The right eye of this patient had a history of 4 episodes of CMV corneal endotheliitis with intraocular hypertension (Figure 1). The intraocular pressures (IOPs) were measured using a non-contact tonometer (NT-4000; NIDEK Co., Ltd, Japan). The ages of these event occurrences were 9.91, 10.03, 12.12, and 12.67 years. In each event, characteristic KPs including coin-shaped lesions were detected (Figure 2). At the same time, an anterior segment optical coherence tomography (AS-OCT) CASIA 2 (Tomey Corporation, Nagoya, Japan) examination revealed coincident focal or sometimes diffuse corneal stromal edema (Figure 3). His right eye was diagnosed with CMV-related corneal endotheliitis and trabecular meshwork inflammation causing the intraocular hypertension. For each event, topical use of ophthalmic solutions including 0.1% betamethasone 5 times a day and 0.4% ripasudil twice a day led to remission within 7 days. At the last CMV corneal endotheliitis recurrence, CMV was detected from the aqueous humor by qualitative PCR at the concentration of 1.78×104 copies/mL.
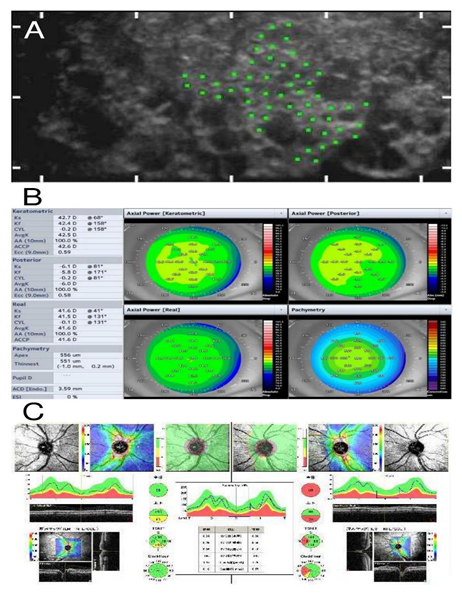
Figure 3: The representative findings of the right eye at the initial visit to our hospital after the 4th event. A non-contact-type specular microscope (Cell Check 16; Konan Co., Ltd., Japan) image revealed the damage to the corneal endothelium but did not exhibit corneal endothelium density loss (A). An anterior-segment optical coherence tomography (AS-OCT) CASIA 2 (Tomey Corporation, Nagoya, Japan) examination revealed diffuse corneal stromal edema (B). The optic nerve and macula (ILM-IPL/INL) exhibited no thinning of the retinal ganglion cell layer in the right or left eye (C).
3. Discussion
Corneal endotheliitis, the primary type of corneal endothelium–specific inflammation, was first described by Khodadoust et al. in 1982 (1). It is characterized by corneal oedema and KPs and/or dysfunction of corneal endothelium cells. The corneal endotheliitis is considered a viral infection accompanied by the herpes simplex virus (HSV)(15,16), varicella-zoster virus (VZV), and mumps virus(17,18). Although cases of corneal endotheliitis often test negative for HSV and VZV and are unresponsive to acyclovir treatment, those cases are considered idiopathic prior to CMV involvement and their prognosis is poor due to a lack of adequate treatment.
Here we report a case of juvenile CMV-related endotheliitis. The right eye was involved and had a history of four episodes of endotheliitis accompanied by ocular hypertension. In all of history, the inflammation subsided with the topical use of steroids and Rho kinase inhibitors. To the best of our knowledge, this is the youngest case reported worldwide. CMV-related endotheliitis primarily involves middle-aged and elderly individuals. However, this case indicates that increased attention should be provided to younger generations regarding CMV-related endotheliitis.
The main limitation of the present study is its retrospective design and small sample size. Our results require verification in a future prospective randomized masked study. The data here suggest that examining a large cohort of patients with versus without ocular hypertension will confirm that the suspicion of CMV leads to the endotheliitis diagnosis and enables subsequent intervention.
4. Conclusions
In this case, CMV corneal endotheliitis was observed in a 9-year-old boy. This demonstrates that attention should be paid to younger patients with suspected CMV.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
Author Contributions
The Author Contributions section is mandatory for all articles, including articles by sole authors. If an appropriate statement is not provided on submission, a standard one will be inserted during the production process. The Author Contributions statement must describe the contributions of individual authors referred to by their initials and, in doing so, all authors agree to be accountable for the content of the work.
Funding
This study was supported in part by a research project grant (no. 03B-002) from Kawasaki Medical School (to H.F.).
Acknowledgments
We thank Koizumi N. and Yaida M. for their discussions, advice, and criticism, which greatly benefited this project.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding author, HF, upon reasonable request.
References
- Khodadoust AA, Attarzadeh A. Presumed Autoimmune Corneal Endotheliopathy. American Journal of Ophthalmology 93 (1982): 718-722.
- Suzuki T, Ohashi Y. Corneal Endotheliitis. Seminars in Ophthalmology 23 (2008): 235-240.
- Koizumi N, Yamasaki K, Kawasaki S, et al. Cytomegalovirus in Aqueous Humor from an Eye with Corneal Endotheliitis. American Journal of Ophthalmology 141 (2006): 564-565.
- Chee SP, Bacsal K, Jap A, et al. Clinical Features of Cytomegalovirus Anterior Uveitis in Immunocompetent Patients. American Journal of Ophthalmology 145 (2008): 834-840.
- van Boxtel LA, van der Lelij A, van der Meer J, et al. Cytomegalovirus as a Cause of Anterior Uveitis in Immunocompetent Patients. Ophthalmology 114 (2007): 1358-1362.
- Chee SP, Bacsal K, Jap A, et al. Corneal Endotheliitis Associated with Evidence of Cytomegalovirus Infection. Ophthalmology 114 (2007): 798-803.
- Shiraishi A, Hara Y, Takahashi M, et al. Demonstration of “Owl’s Eye” Morphology by Confocal Microscopy in a Patient with Presumed Cytomegalovirus Corneal Endotheliitis. American Journal of Ophthalmology 143 (2007): 715-717.
- Suzuki T, Hara Y, Uno T, et al. DNA of Cytomegalovirus Detected by PCR in Aqueous of Patient with Corneal Endotheliitis after Penetrating Keratoplasty. Cornea 26 (2007): 370-372.
- Yamauchi Y, Suzuki J, Sakai J, et al. A Case of Hypertensive Keratouveitis with Endotheliitis Associated with Cytomegalovirus. Ocular Immunology and Inflammation 15 (2007): 399-401.
- Koizumi N, Suzuki T, Uno T, et al. Cytomegalovirus as an Etiologic Factor in Corneal Endotheliitis. Ophthalmology 115 (2008) 292-297.e3.
- Anshu A, Chee SP, Mehta JS, et al. Cytomegalovirus Endotheliitis in Descemet’s Stripping Endothelial Keratoplasty. Ophthalmology 116 (2009): 624-630.
- Chan AS, Mehta JS, Al Jajeh I, et al. Histological Features of Cytomegalovirus-Related Corneal Graft Infections, its Associated Features and Clinical Significance. British Journal of Ophthalmology 100 (2016): 601-606.
- Chee SP, Jap A. Treatment Outcome and Risk Factors for Visual Loss in Cytomegalovirus Endotheliitis. Graefes Archives of Clinical Experimental Ophthalmology 250 (2012): 383-389.
- Koizumi N, Inatomi T, Suzuki T, et al. Clinical Features and Management of Cytomegalovirus Corneal Endotheliitis: Analysis of 106 Cases from the Japan Corneal Endotheliitis Study. British Journal of Ophthalmology 99 (2015): 54-58.
- Robin JB, Steigner JB, Kaufman HE. Progressive Herpetic Corneal Endotheliitis. American Journal of Ophthalmology 100 (1985): 336-337.
- Ohashi Y, Yamamoto S, Nishida K, et al. Demonstration of Herpes Simplex Virus DNA in Idiopathic Corneal Endotheliopathy. American Journal of Ophthalmology 112 (1991): 419-423.
- Maudgal PC, Missotten L, De Clercq E, et al. Varicella-Zoster Virus in the Human Corneal Endothelium: A Case Report. Bulletin of the Belgian Society of Ophthalmology 190 (1980): 71-86.
- Singh K, Sodhi PK. Mumps-induced corneal endotheliitis. Cornea 23 (2004): 400-402.
- Koizumi N, Yamasaki K, Kawasaki S, et al. Cytomegalovirus in Aqueous Humor from an Eye with Corneal Endotheliitis. American Journal of Ophthalmology 141 (2006): 564-565.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
