A Case Report of ST-Segment Elevation Myocardial Infarction due to Emotional Stress Caused by Spontaneous Coronary Artery Dissection in A Young Male
Farman Ali1*, Khurram Arshad1*, Rabia Latif2, Aman Ullah3, Yazan Alamro1, FNU Raheela4 , FNU Zafarullah5
1Department of Internal Medicine Corewell Health Dearborn Hospital, Dearborn, MI, USA
2Department of Internal Medicine McLaren Flint Hospital, Flint, MI, USA
3St. Joseph Mercy Oakland Hospital, Pontiac, USA
4Internal Medicine, Chandka Medical College, Larkana, Pakistan
5Interventional Cardiology, Ascension Borgess Hospital, Kalamazoo, USA
*Corresponding author: Khurram Arshad, Department of Internal Medicine Corewell Health Dearborn Hospital, Dearborn, MI, USA.
Note: Farman Ali and khurram Arshad are equal contributor and share 1st co-authorship.
Received: 29 April 2024; Accepted: 06 May 2024; Published: 21 May 2024
Article Information
Citation: Farman Ali, Khurram Arshad, Rabia Latif, Aman Ullah, Yazan Alamro, FNU Raheela, FNU Zafarullah. A Case Report of ST-Segment Elevation Myocardial Infarction due to Emotional Stress Caused By Spontaneous Coronary Artery Dissection In A Young Male Cardiology and Cardiovascular Medicine. 8 (2024): 215-218.
View / Download Pdf Share at FacebookAbstract
Spontaneous Coronary Artery Dissection (SCAD) is a rare condition that can present as an Acute Coronary Syndrome (ACS), including ST-Segment Elevation Myocardial Infarction (STEMI). It is often underdiagnosed for various reasons. It is frequently reported in young females in association with fibromuscular dysplasia as an underlying condition. In literature, only a few cases of SCAD have been reported associated with emotional stress. In our case, a 29-year-old male who presented with acute onset chest pain and initial emergency department presentation was consistent with STEMI.
Keywords
<p>Drug-eliciting stent (DES); Left anterior descending (LAD); Spontaneous coronary artery dissection (SCAD); ST-segmental myocardial infarction (STEMI)</p>
Article Details
Introduction
Spontaneous Coronary Artery Dissection (SCAD) is an infrequent condition, and it can present as an acute coronary syndrome (ACS). Patients with SCAD can present with chest pain alone, ST-segment elevation myocardial infarction (STEMI), ventricular fibrillation, and sudden death [1]. Annual incidence of SCAD is about 0.2%-1.1% among patients undergoing coronary angiography for ACS. In the United States, yearly, more than 800 cases of SCAD are diagnosed, and these numbers are increasing [1]. The mean age of SCAD diagnosis is about 40 years and above, and it is more common in females (70-80%) than males [2]. Precipitating factors include connective tissue disorders, vigorous exercise, emotional anxiety, coronary artery vasospasm, use of hormonal pills for contraception, menstrual periods, and pregnancy. These have been described to be associated with SCAD [3]. Saw et al. reported a case series highlighting fibromuscular dysplasia (FMD) as a distinct predictive factor for coronary artery dissection, particularly when concomitant with precipitating factors such as emotional stress [4]. In rare instances, emotional stress alone has been reported to lead to SCAD without many CAD risk factors.
Case Presentation
A 29-year-old African American male with a history of depression presented to the emergency department (ED) with severe retrosternal chest pain that started about four hours ago. The chest pain started after finding out about the sudden death of his sister. It was severe in intensity and associated with nausea and diaphoresis. The patient denied any prior medical history of heart disease, diabetes mellitus, hypertension, or family history of heart disease; social history was negative for smoking or any illicit drug use. Upon presentation to ED, the patient was slightly hypotensive with a blood pressure of 95/55; other vital signs were stable. EKG showed significant ST-segment elevation in leads V1-V6. (Figure 1)Blood workup was unremarkable except for elevated cardiac troponins I level at 0.21 ng/ml (normal 0.0 to 0.03 ng/ml). The patient was given aspirin, sublingual nitroglycerin, and heparin drip after the bolus and eventually started on nitroglycerine drip due to persistent chest pain. STEMI code was activated, and the patient emergently underwent cardiac angiography after cardiology evaluation.
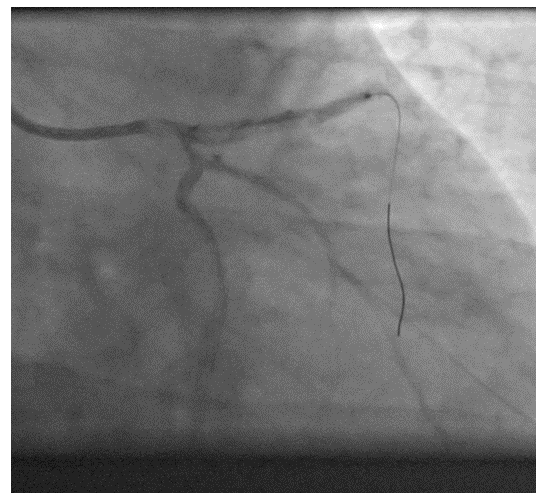
Coronary angiography showed proximal left anterior artery (LAD) occlusion with TIMI 0 flow to distal LAD and diagonal branch (Figure2).
Due to the severity of symptoms and worsening hypotension during the procedure, no intravascular ultrasonography (IVUS) was performed, and after balloon angioplasty, a drug-electing stent (DES-Xience 3.5x38mm) was placed. (Figure 3) Post-stent angiogram showed haziness in proximal LAD and thrombus in distal LAD; multiple runs of aspiration were performed with good blood flow distally.
There was no atherosclerosis of coronary arteries on angiography except for the presence of a thrombus, and likely, the patient has SCAD with subsequent thrombus formation (Figure 4).
The patient was monitored in the critical care unit for close monitoring after the procedure, and his symptoms improved remarkably. An echocardiogram showed a left ventricle ejection fraction (LVEF) of 30-35% with akinesis of the apex without ballooning. Cardiac magnetic resonance imaging (MRI) did not show a left ventricle thrombus or aneurysm. Ultrasonography of the carotid and renal arteries was also performed, and no evidence of fibromuscular dysplasia was found. The patient was placed on appropriate medical therapy and was discharged home in stable condition after five days of admission. The patient has been followed up in the cardiology clinic, and his LVEF did not improve after three months of goal-directed medical therapy. He underwent an implantable cardioverter defibrillator (ICD) for primary prevention of cardiac arrhythmia.
Discussion
Our patient presented with typical symptoms of ACS accompanied by chest pain, significant electrocardiogram (EKG) changes and elevated cardiac troponins I. The initial differential diagnosis was STEMI, pericarditis (given diffuse ST-segment elevations on EKG), and myocarditis. As our patient lacks risk factors for coronary artery disease (CAD), the patient's young age and the temporal association between chest pain and emotional distress might indicate an initial non-coronary chest pain syndrome. However, the presence of ischemic EKG changes, along with elevated troponins, necessitated an exploration of non-atherosclerotic causes of coronary ischemia, such as vasospasm, embolism, and coronary dissection.
In our case, coronary angiography confirmed the presence of SCAD in the proximal LAD artery, with superimposed thrombus formation that had dislodged distally as well. SCAD is frequently insufficiently characterized by angiography, as the narrowing induced by the intramural hematoma can be misinterpreted as an atherosclerotic disease [5]. Newer intracoronary imaging modalities, including intravascular ultrasound (IVUS) and optical coherence tomography (OCT), can help clinicians make a definite diagnosis when the initial diagnosis is uncertain [5]. SCAD is defined by the spontaneous, non-iatrogenic separation of coronary artery layers caused by bleeding, leading to the development of an intramural hematoma. There are two proposed mechanisms suggested: one involves an intimal tear leading to dissection and hemorrhage, resulting in the formation of a false lumen; the other involves rupture of vasa vasorum leading to intramural hemorrhage and medial dissection without an intimal tear. Subsequently, the development of an intramural hematoma can cause pressure on the true lumen, leading to downstream ischemia and infarction [3]. SCAD is more frequently seen in females, and according to one study, fibromuscular dysplasia (FMD) is commonly associated with underlying conditions in these patients [4]. Other contributing factors may include physical trauma, emotional stress, use of oral contraceptive pills (OCPs), and underlying connective tissue disorders. Although rare, extreme emotional stress can lead to SCAD in young males without FMD, underscoring the importance for clinicians to remain vigilant regarding the varied presentations of this clinical entity, as timely management can yield favorable clinical outcomes. Management of SCAD presenting as acute myocardial infarction (AMI) is not very clear as there are no definite guidelines. Patients with stable vital signs and having adequate coronary artery blood flow distal to the coronary artery dissection on angiography can be managed conservatively. Medical management includes antiplatelets and beta-blocker therapy. Patients with SCAD are prone to have prothrombotic changes in the coronary vasculature resulting from intimal tears. Therefore, empiric use of dual antiplatelet therapy with aspirin and clopidogrel may hold promise in mitigating these thrombotic changes. These patients should take aspirin for lifelong because it has few side effects. On the other hand, clopidogrel can be continued for up to a year, although there is no clear data regarding optimal duration [6]. Beta-blockers such as metoprolol and carvedilol help by reducing the shear forces on the arterial wall, potentially preventing the dissection and hemorrhage from worsening. The effectiveness of statins in treating SCAD has not been thoroughly investigated. Anticoagulation therapy using intravenous heparin or enoxaparin might carry the risk of worsening the extension of coronary dissection [6].
Patients who are hemodynamically unstable or continue to have persistent chest pain should undergo percutaneous coronary intervention (PCI), particularly if the dissection affects the main coronary arteries, such as the left main or proximal LAD. Performing PCI on dissected coronary arteries can be difficult, and IVUS or OCT may be employed to ensure optimal stent placement. If the dissection affects the left main coronary artery or multiple coronary arteries, or if initially PCI is unsuccessful, coronary artery bypass grafting (CABG) may be a viable option [6]. The utilization of bioresorbable vascular scaffolds (BVS) for treating nonatherosclerotic coronary artery disease is a potential strategy for managing SCAD cases presenting as STEMI or who are hemodynamically unstable [7].
Conclusion
SCAD should be considered in the differential diagnosis of patients presenting with anginal symptoms, particularly in young individuals exhibiting EKG changes and lacking typical cardiac risk factors. Treatment options may involve conservative medical management, incorporating antiplatelets and antianginal agents. For patients with lesions affecting the major coronary arteries, PCI may be appropriate. While antiplatelet therapy is frequently indicated, the optimal duration of administration remains uncertain. Differentiating SCAD from coronary atherosclerotic disease as the cause of AMI early on is essential, as the treatment approaches for these conditions differ significantly. If conventional angiography fails to detect SCAD, emerging imaging techniques like IVUS and OCT can help in identifying subtle distinctions between SCAD and CAD.
Funding sources
Self Funded
Conflict of Interest statement
None to Declare
References
- Tweet MS, Hayes SN, Pitta SR, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 126 (2012): 579-588.
- Vanzetto G, Berger-Coz E, Barone-Rochette G, et al. Prevalence, therapeutic management and medium-term prognosis of spontaneous coronary artery dissection: results from a database of 11,605 patients. Eur J Cardiothorac Surg 35 (2009): 250-254.
- Singh GD, Nishimura M, Rogers JH, et al. Pain at the game: spontaneous coronary artery dissection. Am J Med 127 (12): 1160-1163.
- Saw J, Poulter R, Fung A, et al. Spontaneous coronary artery dissection in patients with fibromuscular dysplasia: a case series. Circ Cardiovasc Interv 5 (2012): 134-137.
- Paulo M, Sandoval J, Lennie V, et al . Combined use of OCT and IVUS in spontaneous coronary artery dissection. JACC Cardiovasc Imaging 6 (2013): 830-832.
- Yip A, Saw J. Spontaneous coronary artery dissection-A review. Cardiovasc Diagn Ther 5 (2015): 37-48.
- Onuma Y, Serruys PW. Bioresorbable scaffold: the advent of a new era in percutaneous coronary and peripheral revascularization? Circulation F123 (2011): 779-797.





 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 