A Rare Occurrence of an Intraosseus Squamous Cell Carcinoma in Association with Squamous Odontogenic Tumor of Mandible
Nilesh D Pardhe*,1, Pradakhshana Vijay2, Manika Arora3, Nikunj Mathur4
1Independent Researcher in Dentistry, Former Head - Department of Oral & Maxillofacial Pathology, NIMS Dental College, Jaipur, India
2Senior Resident, Department of Oral Pathology, KGMU, Lucknow, India
3Former Lecture -Department of Oral & Maxillofacial Pathology, NIMS Dental College, Jaipur, India
4Reader, Department of Oral Medicine & Radiology, Government Dental College, Jaipur, India
*Corresponding author: Nilesh D Pardhe, Former Head of Department, Oral & Maxillofacial Pathology, NIMS Dental College, Jaipur, E-703, Ashadeep Green Avenue, Jagatpura, Jaipur, India.
Received: 19 September 2021; Accepted: 30 September 2021; Published: 09 October 2021
Article Information
Citation: Nilesh D Pardhe, Pradakhshana Vijay, Manika Arora, Nikunj Mathur. A Rare Occurrence of an Intraosseus Squamous Cell Carcinoma in Association with Squamous Odontogenic Tumor of Mandible. International Journal of Applied Biology and Pharmaceutical Technology 12 (2021): 393-396.
View / Download Pdf Share at FacebookAbstract
Squamous odontogenic tumor (SOT) reported for the first time by Pullon et al in 1975was described and classified as a distinct pathological entity by the World Health Organization (WHO) in 1992 [1]. A rare benign neoplasm, it can locally infiltrate and extend to neighboring structures such as the maxillary sinuses and nasal cavity. Clinically it presents itself as an asymptomatic swelling in the alveolar process, with most cases being accidentally reported on routine dental radiographs [2]. Histologically, it is composed of well-differentiated squamous epithelium in a fibrous stroma [1]. Published scientific literature accounts for approximately 47 cases of SOT [3]. Considering the rarity of this tumor, the malignant transformation of this benign tumor is even rarer with only 2 cases reporting its occurrence [4, 5]. To the best of author’s knowledge, malignant transformation of SOT into squamous cell carcinoma (SCC) is the first to be documented from the South-East Asian subcontinent. We herein report an extremely rare occurrence of SOT with malignant transformation exhibiting an aggressive bone destruction of mandible.
Keywords
<p>Squamous Odontogenic Tumour, Primary Intraosseous Squamous Cell Carcinoma</p>
Article Details
Introduction
Squamous odontogenic tumor (SOT) reported for the first time by Pullon et al in 1975was described and classified as a distinct pathological entity by the World Health Organization (WHO) in 1992 [1]. A rare benign neoplasm, it can locally infiltrate and extend to neighboring structures such as the maxillary sinuses and nasal cavity. Clinically it presents itself as an asymptomatic swelling in the alveolar process, with most cases being accidentally reported on routine dental radiographs [2].
Histologically, it is composed of well-differentiated squamous epithelium in a fibrous stroma [1].
Published scientific literature accounts for approximately 47 cases of SOT [3]. Considering the rarity of this tumor, the malignant transformation of this benign tumor is even rarer with only 2 cases reporting its occurrence [4, 5].
To the best of author’s knowledge, malignant transformation of SOT into squamous cell carcinoma (SCC) is the first to be documented from the South-East Asian subcontinent. We herein report an extremely rare occurrence of SOT with malignant transformation exhibiting an aggressive bone destruction of mandible.
Case Report
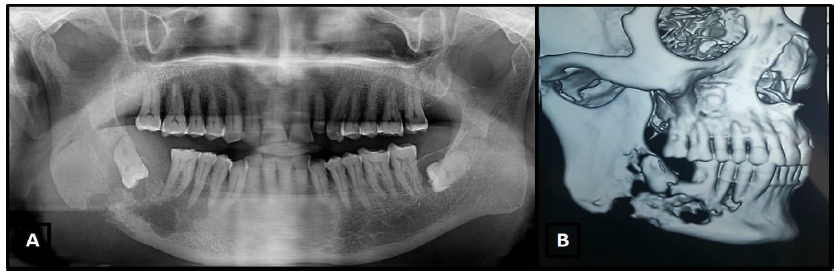
A 69 year old male patient presented with pain and tenderness in the right mandibular molar region. The patient underwent a 2nd molar extraction 2 months back, the unhealed socket of which was evident on clinical examination. Radiographic examination (OPG & CT) revealed an irregular destructive radiolucent lesion extending from the mandibular right 1st premolar to the impacted Mandibular right 3rd molar and infiltrating into the ramus with gross destruction and perforation of the cortical plates and pathologic fracture in the mandibular angle region (Fig. A & B). Based on the clinical and radiographic features, a preliminary diagnosis of osteomyelitis was considered. Surgical exploration of the lesion was performed and the bits of excised tissues were subjected for histopathological examination, whitish brown in color, measuring about 1.7 x 1.5, 1.0x 0.8 and 0.7 x 0.5cm.
Figure A: Panoramic radiograph showing irregular radiolucent areas present peri-apically extending from the 1st premolar to 1st molar and impacted 3rd molar teeth, involving the cortical plate.
Figure B: Computed tomography image shows wide osteolytic areas with irregular cortical plate destruction in the 1stpremolar molar area extending till the inferior border of cortex.
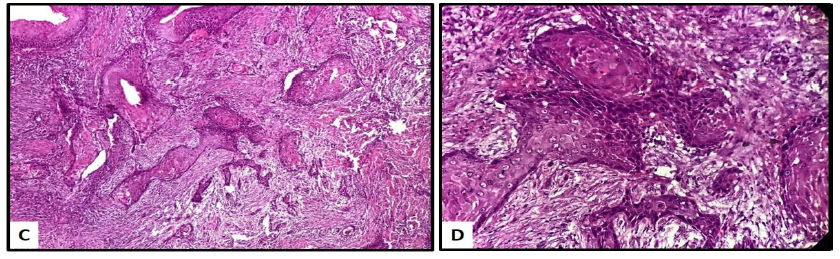
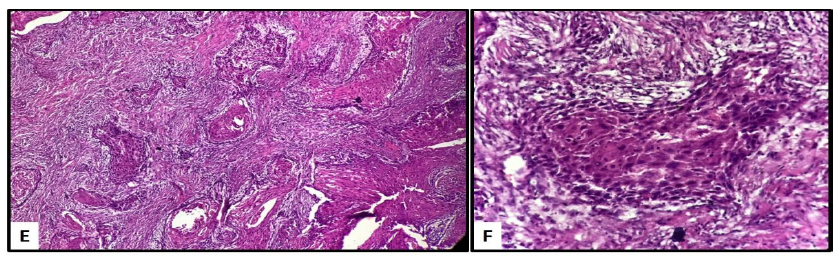
The microscopic examination revealed well differentiated islands of squamous epithelium set in mature fibrous stroma. The epithelial islands showed no evidence of peripheral columnar cells, palisading nuclei, or stellate reticulum in it, being the diagnostic criteria for SOT (Fig. C & D).
The most conspicuous feature was the simultaneous presence of a few foci of atypical cells arranged peripherally on these islands. These features suggested the conspicuous presence of squamous cell carcinoma along with islands of SOT. Thus, correlating the clinical, radiological and histopathologic findings a diagnosis of a simultaneous occurrence of SCC with SOT was considered (Fig. E & F).
Patient was referred back to the surgery department for further treatment.
Discussion
SOT is the result of neoplastic transformation of epithelial cell rests of Malassez or rests of Serres. Its histogenesis involves variable inductive interactions between the odontogenic epithelium and ectomesenchyme with its embryological origin derived from the dental lamina [2, 6]. The first documentation of malignant variant of SOT can be dated back to 1984 by Norris et al, who reported the simultaneous occurrence of intraosseous squamous cell carcinoma in the mandible, in one case of bilateral maxillary SOT, however, his report could not state an evidence of its development from a SOT [5]. Hume et al reported an unusual case of keratoacanthoma-like SOT with a histological resemblance to squamous cell carcinoma [6]. Authors have also reported maxillary lesions, occurring in children, having a similar clinical presentation of SOT with a diagnosis of SCC [8, 9]. Ide et al, reported an Intraosseous squamous cell carcinoma arising in association with a squamous odontogenic tumour of the mandible, supporting his diagnosis by staining with p53 and Ki-67, the immunopositivity of which, seen in the tumor islands, lend support to the malignant change of SOT [4].
In our case, we observed characteristic patterns of SOT along with irrefutable presence of focal areas showing squamous cell carcinoma. As much as this histological picture suggests a malignant transformation of SOT, there also exists a possibility for the present squamous cell carcinoma to occur de novo and mimic the appearance of a more benign SOT or simply coexisting. Therefore, regardless of the rarity of this tumor, the validity of this benign lesion transforming into its malignant counterparts is still obscure. Nevertheless, a more careful distinction is required between SOT and primary intraosseous squamous cell carcinoma [5, 8, 20, 21].
Conclusion
Our case report interprets this lesion as an intraosseous SCC with probable origin from SOT. However, with application of appropriate immunohistochemical markers we can gain more clarity over the malignant transformation of SOT. Till then, the possibility of SOT being a risk-lesion for the subsequent development of squamous cell carcinoma cannot be refuted.
References
- Pullon PA, Shafer WG, Elzay RP, Kerr DA, Corio RL. Squamous odontogenic tumor. Report of six cases of a previously undescribed lesion. Oral Surg Oral Med Oral Pathol 40(1975): 616-30.
- Tarsitano A, Agosti R, Marchetti C. The diagnostic and surgical management of a multifocal calcifiyng epithelial odontogenic tumor in the mandible and maxilla associated with a squamous odontogenic tumor: first reported case in the literature. Oral Surg Oral Med Oral Pathol Oral Radiol 113 (2012): e6-11.
- Priscilla SC. Lúcio; Marcelo Augusto O. Sales; Gustavo P. Godoy; Rivadávio FB. Amorim. Squamous odontogenic tumor: report of a case of unusual involvement. Bras Patol Med Lab 51 (2015):427-431.
- Ide F, Shimoyama T, Horie N, Shimizu S. Intraosseous squamous cell carcinoma arising in association with a squamous odontogenic tumour of the mandible. Oral Oncol 35 (1999): 431–4.
- Norris LH, Baghaei-Rad M, Maloney PL, Simpson G, Guinta J. Bilateral maxillary squamous odontogenic tumors and the malignant transformation of a mandibular radiolucent lesion. J Oral Maxillofac Surg 42 (1984): 827-34.
- Siar CH, Nakano K, Ng KH, Tomida M, Nagatsuka H, Kawakami T. Squamous odontogenic tumor of the mandible: a case report demonstrating immunoexpression of Notch1, 3, 4, Jagged1 and Delta1. Eur J Med Res 15 (2010): 180-4.
- Hume WJ, Quayle AA. An unusual epithelial neoplasm of gingiva resembling the keratoacanthoma. British Journal of Oral and Maxillofacial Surgery 23 (1985): 366-70.
- Sacks HG, Holly R, Blum B, Joy ED. Maxillary alveolar mass in a 13-year-old boy. Journal of Oral and Maxillofacial Surgery 43 (1985): 958-63.
- Earle AS, Park CH, Vlastou C. Oral squamous cell carcinoma in children. Annals of Plastic Surgery 20 (1988): 148-52.
- Philipsen HP, Reichart PA. Squamous odontogenic tumor (SOT): a benign neoplasm of the periodontium. A review of 36 reported cases. Journal of Clinical Periodontology 23 (1996): 922-6.


 Impact Factor: * 3.0
Impact Factor: * 3.0 Acceptance Rate: 76.32%
Acceptance Rate: 76.32%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
