Causal Factors Involving Family Physicians And/or Dentists that Affect the Six-Year Survival of Elderly Individuals
Tanji Hoshi*
Department of Urban Science, Tokyo Metropolitan University, Japan
Corresponding Author: Tanji Hoshi, Department of Urban Science, Tokyo Metropolitan University, 192-0364 Minamioosawa 1-1 Hachiooji City, Tokyo, Japan.
Received: 08 September 2025; Accepted: 18 September 2025; Published: 16 October 2025
Article Information
Citation:
Tanji Hoshi. Causal Factors Involving Family Physicians And/or Dentists that Affect the Six-Year Survival of Elderly Individuals. Journal of Women’s Health and Development. 8 (2025): 51-59.
DOI: 10.26502/fjwhd.2644-288400140
View / Download Pdf Share at FacebookAbstract
Background: Living a long life is a reward for everyone. This study examines socioeconomic factors, physical, mental, and social health, lifestyle, and the prevalence of diseases as related factors in individuals with only a family physician and those with only a family dentist, investigating the causal structure of the survival rate in relation to these factors. Methods: In September 2001, a self-administered questionnaire was sent to 16,462 elderly residents of Tama City, Tokyo. A total of 13,066 responses were received, resulting in a response rate of 79.4%. The Survival Dayss up to 2007 were recorded. Results: Having only a dentist was significantly associated with a more prolonged six-year survival compared to having only a physician for both sexes. Additionally, "Socioeconomic Status" (latent variable) was identified as the primary causal factor of the "Three Health Factors." Regarding the cause and effect of having a [Physician and/or Dentist] (observed variable) on Survival Days, “Socioeconomic Factors," the "Three Health Factors," and ?Treated Diseases? were identified as confounding variables. Conclusions: The main factor influencing survival time was the patient's recommended socioeconomic status, particularly access to a family dentist. Additionally, socioeconomic factors are fundamental drivers that impact the reduction of treatable diseases through lifestyle choices and the maintenance of mental, physical, and social health. Choosing only a family dentist instead of a family physician was significantly linked to longer survival. Trial Registration Data The analytical data from this study are available from the UMIN SYSTEM in Japan as an open system (https://upload.umin.ac.jp/cgi-bin/fileshare/upload.cgi?DELETE=1&on=589518, Accessed July 1, 2025). Personal registration is required for data specifications. Additionally, analytical data and materials can be obtained from the first author via the following email address: star@onyx.dti.ne.jp (T. Hoshi, first author).
Keywords
<p>Family dentist; Survival Days; Socioeconomic status; Confounding factors; Elderly people</p>
Article Details
Background
In a country like Japan, where the population is aging rapidly, maintaining healthy longevity has become increasingly important [1]. Japan has established two main goals: promoting healthy longevity and preventing premature death. The "Healthy Japan 21 Plan" was launched in 2000 to achieve these objectives [2]. The plan emphasized the importance of maintaining oral health, highlighting the benefits of a balanced diet and offering recommendations to promote healthy lifestyle choices. The Japan Dental Association published a report on the scientific basis for dentists' role in promoting health and longevity [3]. The report noted that women’s survival rate remained stable when they had more than 10 teeth remaining and their oral hygiene was good [4]. In another study, the occurrence of aspiration pneumonia was significantly lower in the intervention group compared to the control group, which did not receive oral hygiene care support from the institutionalized patients, and survival rates were maintained [5]. An oral hygiene examination of 2,900 people visiting a dental clinic in Minato-ku, Tokyo, revealed that good oral hygiene has a positive impact on quality of life (QOL), which is related to health and life satisfaction, and improves survival [6]. In this way, there is a strong connection between having a family dentist and increased survival rates. However, this connection might be misunderstood if we do not account for confounding factors, which are variables related to both the cause and the effect. We demonstrated that socioeconomic factors can influence excellent lifestyle habits that promote physical, mental, and social health, and supporting these habits ultimately leads to longer, healthier survival [7].To verify the causal structure and identify potential confounding factors, a covariance structure analysis tool should be employed. However, research on covariance structure analysis regarding the relationship between having only a dentist and survival days was not found during a search at the Library of Congress PubMed.
Therefore, this study investigated the relationship between the number of days of survival and whether elderly individuals in the suburbs of Tokyo are mainly cared for by family dentists or family physicians alone. It also explored how socioeconomic factors, physical, mental, and social health, disease status, and lifestyle habits are interconnected, including their indirect effects. The aim was to clarify these structural causal relationships using covariance structural analysis. Understanding how these factors influence survival can help develop effective strategies to improve survival rates, emphasizing the importance of maintaining good oral hygiene.
Methods
Study Design
A cohort survey was conducted with older adults. In September 2001, we administered a questionnaire to people aged 65 and older living at home in Tama City, a suburb of Tokyo. The total number of subjects was 16,462, and 13,066 (79.4%) responded with informed consent and returned the self-administered questionnaire by mail. We verified their survival status and the number of days they survived until September 2007. The 921 individuals who relocated to another city were excluded from the analysis.
Questionnaires and Measurements
Family Physicians and/or Dentists
At the end of the six-year follow-up, survival rates were significantly higher for patients who had only a family dentist, followed by those who saw both a physician and a dentist. The lowest survival rates were observed among patients who had only a family physician. In this study, we divided the subjects into three groups. The participants in Group 1 were individuals who had only a family physician. Group 2 included those who had both a primary physician and a dentist. Group 3 consisted of people who visited only their family dentist. The reason for dividing them into these three groups is that covariance structure analysis requires variability in the observed variables.
Socioeconomic Status
Regarding socioeconomic status, the annual income of married couples was categorized into four groups: less than 1 million yen (approximately $7,142 US dollars), less than 3 million yen, less than 7 million yen, and more than 7 million yen. Using factor analysis, age—considered to be linked with the couple's annual income—was also included as a socioeconomic factor.
Three Health Factors
This study investigated three aspects of health: physical, mental, and social health. The physical health parameters included basic activities of daily living (BADL) [8] and instrumental activities of daily living (IADL) [9]. The BADL score was based on four questions: "Can you go to the toilet by yourself?", "Can you take a bath by yourself?", "Can you cook your meals every day?" and “Can you buy your daily necessities?". Participants received 1 point for each function they could perform, and the total score ranges from 0 to 4, with higher scores indicating a higher level of basic activity capacity.
The IADL score was determined by questions like "Can you deposit or withdraw money from your bank account?", “Do you deal with a set of insurance and pension documents?", and "Can you read books and newspapers?" Similar to the BADL score, the IADL score ranges from 0 to 3.
Mental health was evaluated through self-reported subjective health data from a 2001 survey. The question asked was "Do you think you are healthy?" [10]. The question about life satisfaction was "Are you satisfied with your daily life?" [11]. Social health was assessed based on how often people went out and communicated with neighbors. The survey asked respondents how frequently they went out [12]. Additionally, communication with neighbors was measured in terms of how often it occurred [13]. The options for each question are shown in Table 2.
Lifestyle
The recommended habit items were considered healthy lifestyle habits if they were significantly related to the number of days to survive up to 6 years. Maintaining a longer Survival Days was observed in the group that consumed alcohol. Smoking was in the group that did not smoke from the beginning of the study. Therefore, the group that consumed alcohol and did not smoke from the start of the study was divided into three groups, each with 1 point, ranging from 0 to 2 points [14].
Treated Diseases
The conditions most strongly associated with reduced survival after 6 years were hypertension, cerebrovascular disease, diabetes, heart disease, and liver disease. Consequently, the score for the number of treated conditions ranges from 0 to 5 points.
Data Analysis
The data were analyzed using IBM's SPSS and AMOS software (version 28). For statistics involving continuous variables by category, a one-way analysis of variance was performed. To compare differences between categories, the Kendall τ test was used. Covariance structure analysis was employed to identify causal relationships within a hypothetical model containing latent variables. To clarify the latent variables in the causal structure model, an exploratory factor analysis with varimax rotation was conducted using the maximum likelihood method. The fit of the causal structure model was assessed using the normed fit index (NFI), incremental fit index (IFI), and the approximate root mean square error (RMSEA) [15, 16]. All estimates are standardized constants. A difference was considered statistically significant if the p-value was less than 1%.
Results
Number of Objects Analyzed
We analyzed 12,145 individuals, comprising 5,664 men and 6,481 women, all of whom were over the age of 65 (Table 1).
The sex distributions of the variables used in this study have been described in other studies [17].
|
Age Groups |
Total |
|||||
|
65-69 |
70-74 |
75-79 |
80-84 |
85- |
||
|
Men |
1,044 |
2,128 |
1,289 |
652 |
551 |
5.664 |
|
18.4% |
37.6% |
22.8% |
11.5% |
9.7% |
100% |
|
|
Women |
1,090 |
2,045 |
1,476 |
966 |
904 |
6,481 |
|
16.8% |
31.6% |
22.8% |
14.9% |
13.9% |
100% |
|
|
Total |
2,134 |
4,173 |
2,765 |
1,618 |
1,455 |
12,145 |
|
17.6% |
34.4% |
22.8% |
13.3% |
12.0% |
100% |
|
Table 1: Analytical subjects by age and sex.
Survival Days at 6 Years and Associated Factors
The cumulative survival rate, as determined by Kaplan-Meier analysis, was 85.9% for men and 92.4% for women in the family dentist-only group after 6 years. In the family physician-only group, the rates were 76.0% and 76.6% for men and women, respectively, and 82.0% and 90.4% for those who had both a physician and a dentist, with a significant difference according to the generalized Wilcoxon test among the three groups for both sexes. In terms of Survival Days, the group with only the family dentist lived the longest, with men surviving an average of 2,018.1 days (Standard Deviation: SD: 420.8) and women surviving an average of 2,082.9 days (SD: 400.1). The next longest was the group with both a family dentist and an internist, with men surviving an average of 1,969.4 days (SD: 482.5) and women surviving an average of 2,060.7 days (SD: 356.7).
The Survival Days for the family physician-only group was the shortest, at 1,902.5 days (SD: 556.4) for men and 1,905.3 days (SD: 547.8) for women. One-way ANOVA revealed significant differences between the physician-only and dentist-only groups.
Additionally, the group with only a family dentist performed significantly better than the group with only a family physician across all relevant variables examined in this study (Table 2). This suggests that the group with only a family dentist was healthier than the group with only doctors.
Cox proportional hazards analysis, a multivariate method that includes all observed variables with the number of days of survival as the dependent variable, revealed a significant association between younger age and maintaining subjective health in both sexes. In men, nonsmokers and BADL scores were significantly related. Having only a family dentist was identified as a significant factor for Survival Days in women. This multivariate method only reveals direct effects, while indirect effects and related structures remain unknown. Therefore, we aimed to clarify these related structures using covariance structure analysis.
Causal Structure with 6 Years of Survival
Results of Exploratory Factor Analysis
To analyze the covariance structure, we conducted an exploratory factor analysis to identify the underlying latent variables. The first factors were [BDAL] ([ ]means observed variable), [IADL], [going outside], and [Survival Days]. The second factor included [Treated Disease] and [Having a Physician and/or Dentist], each defined as observed variables related to [Survival Days]. The third factor consisted of [Subjective Health], [Life Satisfaction], [Communication with the Neighborhood], and [Lifestyle Scores]. This third factor, along with the first factor, [BDAL], and [IADL], was used to create the "Three Health Factors” (" " indicates a latent variable). The fourth factor comprises age and marital annual income, which we term "Socioeconomic Status." The combined variance explained by these four factors was 42.5% (Table 3). The Cronbach's alpha coefficients were 0.74 for the first factor, 0.55 for the second, 0.14 for the third, and 0.38 for the fourth.
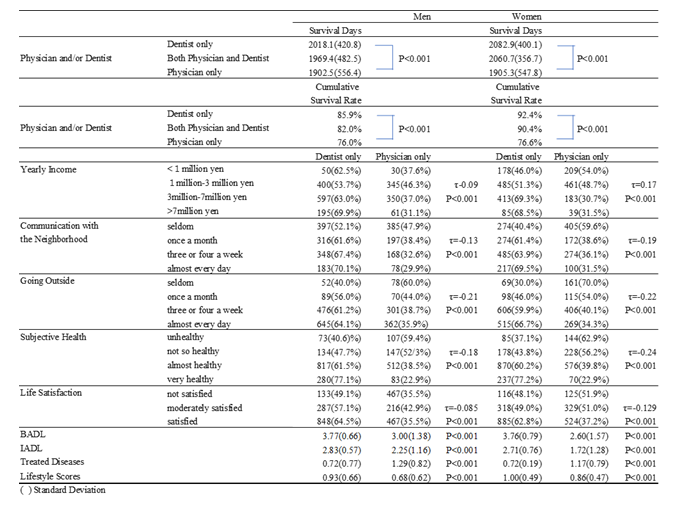
Table 2: Relationships between the Survival Days for six years and correlational observed factors by sex.
|
Factors |
||||
|
1 |
2 |
3 |
4 |
|
|
BADL |
0.943 |
-0.102 |
-0.200 |
-0.107 |
|
IADL |
0.747 |
-0.104 |
-0.214 |
-0.200 |
|
Going Outside |
-0.416 |
0.070 |
0.366 |
0.244 |
|
Survival Days |
0.324 |
-0.111 |
-0.175 |
-0.240 |
|
Treated Diseases |
-0.081 |
0.982 |
0.161 |
0.040 |
|
Having a Physician and/or Dentist |
0.131 |
-0.290 |
-0.156 |
-0.209 |
|
Subjective Health |
-0.322 |
0.321 |
0.533 |
0.072 |
|
Life Satisfaction |
-0.082 |
0.074 |
0.456 |
-0.011 |
|
Communication with the Neighborhood |
-0.199 |
0.072 |
0.416 |
0.169 |
|
Lifestyle Score |
0.057 |
-0.045 |
-0.211 |
-0.079 |
|
Age Groups |
-0.321 |
0.119 |
0.003 |
0.687 |
|
Marital Annual Income |
0.028 |
-0.017 |
-0.226 |
-0.294 |
Table 3: Results of exploratory factor analysis.
Structure of Factors Related to Survival Days
[Survival Days] was used as the dependent variable. "Socioeconomic status" and the "Three Health Factors" were used as the explanatory latent variables. [Treated Diseases] and [Having a Physician and/or Dentist] were set as the observed explanatory variables, and models with a high degree of fit were examined. The final structural causal model was chosen based on its higher fit indices; NFI and IFI were close to 0.9, and the RMSEA was near 0.05. Therefore, it was adopted as the final model, based on the literature [15, 16]. All associations were analyzed using standardized coefficients. In this causal structure analysis, we assessed the overall effect, including both indirect and direct effects (Table 4).
|
Men |
Women |
Total |
||
|
“Socioeconomic Status”⇒⌈Physician and/or Dentist⌋ |
0.612 |
0.197 |
0.184 |
|
|
“Socioeconomic Status”⇒⌈Survival Days⌋ |
0.552 |
0.159 |
0.235 |
|
|
Standardized |
“Socioeconomic Status”⇒ "Three Health Factors” |
0.704 |
0.507 |
0.521 |
|
Direct Effect |
⌈Physician and/or Dentist⌋⇒⌈Survival Days⌋ |
0.001 |
0.001 |
0.001 |
|
⌈Physician and/or Dentist⌋⇒⌈Treated Diseases⌋ |
0.254 |
0.287 |
0.287 |
|
|
⌈Treated Diseases⌋⇒⌈Survival Days⌋ |
-0.035 |
-0.029 |
-0.038 |
|
|
“Three Health Factors”⇒⌈Physician and/or Dentist⌋ |
0.356 |
0.109 |
0.074 |
|
|
“Three Health Factors”⇒⌈Treated Diseases⌋ |
-0.202 |
-0.196 |
-0.198 |
|
|
“Three Health Factors”⇒⌈Survival Days⌋ |
0.294 |
0.329 |
0.286 |
|
|
Standardized |
“Socioeconomic Status”⇒⇒⌈Survival Days⌋ |
0.592 |
0.330 |
0.380 |
|
Total Effect |
⌈Treated Diseases⌋⇒⇒⌈Survival Days⌋ |
-0.035 |
-0.029 |
-0.038 |
|
“Three Health Factors”⇒⇒⌈Survival Days⌋ |
0.056 |
0.335 |
0.294 |
|
|
“ ” : Latent variable?⌈⌋: Observed variable? ⇒: Direct Effect?⇒⇒:Total Effect |
||||
Table 4: Direct and total effect on “Survival Days” by sex.
Effects of the "Three Health Factors" and "Socioeconomic Status" on Survival Days After 6 Years
The most impactful direct effect on the dependent variable [Survival Days] was from the "Three Health Factors," with an estimated value of 0.29. Better subjective health was associated with more prolonged survival, and higher [ADL] and [IADL] scores also correlated with increased lifespan. The direct effect of "Socioeconomic Status" on [Survival Days] was 0.24. The direct effect of [Having a Physician and/or Dentist] on [Survival Days] was almost zero, as shown in the final model in Figure 1.
When analyzing the combined direct and indirect effects on [Survival Days], "Socioeconomic Status" showed the highest estimate at 0.38. This was followed by "Three Health Factors" at 0.29 (Table 4). The direct effect of "Socioeconomic Status" on the "Three Health Factors" was 0.52. Therefore, "Socioeconomic Status" serves as the foundation for determining [Survival Days]. The coefficient for predicting the number of [Survival Days] was 22% (Figure 1).
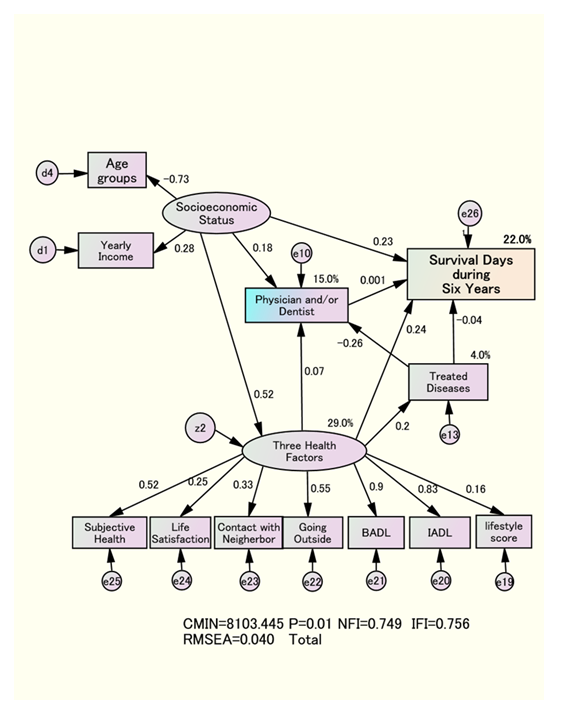
Figure 1: Structure relationships among Survival Days and explanatory factors.
Causal Relationship between Having a Physician and/or Dentist and Survival Days
“Socioeconomic Status" directly influences [Having a Physician and/or Dentist], with an estimated coefficient of 0.18. The coefficient of determination for [Having a Physician and/or Dentist] is 15%. The remaining 85% of factors are unknown. The tendency to visit only the family dentist forms the basis for explaining the preference for a young age and high annual income of the couple, indicating a connection with “Socioeconomic Status.” Additionally, the direct effect of the "Three Health Factors" on [Having a Physician and/or Dentist] was calculated to be 0.07. This shows that better health factors make it easier to choose a dentist over a physician.
Causal Structure of Survival Days for Treated Diseases
The direct effect of the "Three Health Factors" on Treated Diseases was -0.20, and the explanatory power of "Treated Diseases" was only 4%. The direct effect of Treated Diseases on Survival Days was minor, at 0.04. The more diseases that require treatment, the fewer days a person can survive, but this also means that the direct effect becomes smaller.
Confounding Factors
The standardized estimate of the relationship between [Having a Physician and/or Dentist] and [Survival Days] was only 0.03 (Figure 2). However, in the final model shown in Figure 1, the standardized estimate from [Having a Physician and/or Dentist] for [Survival Days] was nearly zero for both men and women. Based on these findings, we conclude that the connections between [Having a Physician and/or Dentist] and [Survival Days] are affected by confounding factors such as "Socioeconomic Status," the "Three Health Factors," and [Treated Diseases].
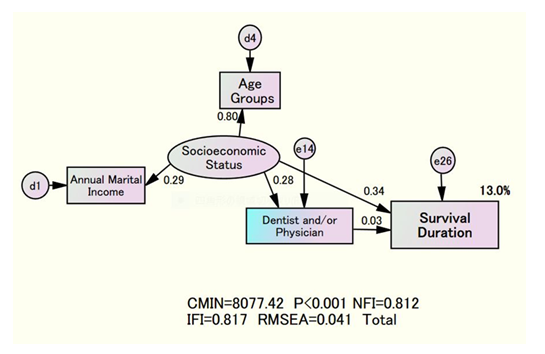
Figure 2: Structure relationship between Survival Days, "Socioeconomic Status”
Discussion
Causal Relationship Between Having a Physician and/or Dentist and the Number of Survival Days
The direct impact of [Having a Physician and/or Dentist] on "Survival Days" was estimated to be 0.03 (Figure 2). However, the final covariance structural analysis, which included all explanatory factors, showed that the direct effect of [Having a Physician and/or Dentist] on [Survival Days] was zero.
Based on our research, it is estimated that, according to the recommended "Socioeconomic Status," relying on family dentists rather than physicians improves the "Three Health Factors," which helps reduce [Treated Diseases] and increases [Survival Days] as a confounding factor (Figures 1 and 2). This study also showed that the cumulative survival rate was significantly higher in the group with only a family dentist than in the group with only family physicians. Reproducibility is essential. Therefore, previous studies [4] showing that a low dental residual index leads to shorter survival times are expected to clarify the possibility that confounding factors, including socioeconomic factors and the three health factors, contribute to unfavorable results by reducing the residual index.
These confounders support the findings of our previous study [18]. Some confounding factors suggest that healthy lifestyle habits do not directly cause a longer life. Instead, the attractiveness of the three health factors, influenced by socioeconomic factors, was linked to healthy longevity, with positive lifestyle habits seen as a consequence. Identifying confounders related to cause and effect remains a significant challenge in understanding their genuine relationship. Conversely, in the family physician-only group, the "number of days to live" decreased. These findings indicate that unfavorable socioeconomic conditions are connected to poor lifestyle habits and declining mental, physical, and social health, leading to more illnesses that require treatment. The near-future goal is to replicate these results quickly.
Significance of Having a Family Dentist
Ogden and Macluskey [19] demonstrated that oral hygiene-related health support provided by family dentists and dental hygienists offer patients a systematic and comprehensive approach to primary, secondary, and tertiary prevention. Reichart [20] suggested that family dentists should apply the four As (ask, advise, assist, and arrange), which are part of the European prevention strategy model, to help prevent disease. German researchers Gellrich et al. [21] reported that this support should be used to encourage early disease detection and activities that promote a healthier lifestyle, thereby fulfilling the role of a dentist. In this study, the presence or absence of a family dentist was confirmed solely through self-reporting, and diagnoses and their effects were not clarified. We need to address this challenge soon. Takada et al. [22] conducted dental check-ups and provided health education to 509 workers under 40 over two years. As a result, when the level of periodontal disease was assessed using the Community Periodontal Index Treatment Needs (CPITN), the percentage of men suspected of having periodontal disease dropped from 43% to 21% the following year. Future studies should do an interventional study, including randomly selected control groups.
Follow-up studies have shown that dentist-rated oral hygiene care is better in a group that sees a family dentist with a focus on prevention than in a group that sees a family dentist who focuses on treating toothaches. Additionally, sustained eating habits significantly contribute to survival, indicating a causal relationship [6]. In the future, clarifying the causal link between the circumstances surrounding family dentists and their subsequent healthy longevity, as well as their socioeconomic status, including their careers, is essential. New research is expected to examine factors such as motivation to visit the dentist and professional dental assessments of oral hygiene.
Collaboration between Family Physicians and Dentists
Extensive research reviews have shown that health support from primary care physicians can reduce health risks and contribute to improved patient outcomes and survival. This meta-analysis demonstrated that the primary care activities of primary care physicians are crucial in managing risk factors for illness and mortality. As a result, survival is maintained [23]. On the other hand, our study demonstrates that the lower survival rate in the family physician-only group compared to the family dentist-only group highlights the importance of recognizing that many diseases are influenced by socioeconomic and health factors that require treatment.
Oral infections, such as tooth decay and gum disease, can increase the risk of infective pericarditis. In this context, Yamaza et al. [24] emphasized the importance of treating oral sources of infection as part of dental care. This includes coordinating medical assessments before surgery for congenital heart disease. Therefore, fostering collaboration between medical and dental professionals is essential.
Future Research Topics
This study clarified the key structure of each factor in maintaining survival for over 6 years. However, the survey period for the "three elements of health" overlapped with those for "socioeconomic status" and [physicians and/or dentists,] so the true causal structure was not fully established. The next step is to conduct follow-up surveys at different times for each latent variable and verify reproducibility in subjects through random sampling. Improving this external validity remains a primary focus for future research. Other concerns in this study included the self-reported presence of family physicians and/or dentists, as well as the unclear diagnosis, treatment status, and effectiveness of healthcare workers. Future research should include objective oral health outcomes, as well as studies that assess healthy life expectancy, with the level of care needed as a dependent variable. Our previous studies showed that individuals who practiced better self-care to maintain oral health and sought preventive support from their dentist experienced improved oral hygiene and food intake, which was linked to better survival outcomes [6].
The reason women tend to live longer than men and visit a family dentist more frequently is probably due to their greater awareness of dental aesthetics. This topic deserves further investigation. Future studies should focus on large-scale, multigenerational longitudinal designs with intervention follow-ups to better understand the preventive and therapeutic benefits of oral hygiene.
Conclusions
The basis for assessing survival days among elderly individuals was the socioeconomic factors that contributed to forming a group of people who had only a dentist. Socioeconomic factors have also been shown to be causal structures that support maintaining mental, physical, and social health, as well as reducing the need for disease treatment. Choosing only the family dentist instead of the family physician was significantly associated with longer survival, indicating a structural causal relationship.
Declarations
Ethics Approval and Consent to Participate
The Tama city local government and Tokyo Metropolitan University signed an agreement to protect privacy and confidentiality. Here, mutual secrecy is strictly enforced. All analysis data are identified by ID only.
Consent for Publication
Informed consent was obtained from all the subjects involved in the study.
Competing Interests
The authors declare that they have no conflicts of interest. The funders had no role in the study design, data analysis, or interpretation.
Funding
This study was funded by a grant from the Japanese Ministry of Health, Labour and Welfare (Hone0-Health-042) and a Grant-in-Aid for Scientific Research (B) from the Japanese Ministry of Education, Culture, Sports, Science and Technology (No.15 31012 and 14350327). We also appreciate the financial support received from the Mitsubishi Foundation (2009-21) in 2009.
Authors' Contributions
T.H. summarized the entire sentence. The author has read and agreed to the published version of this manuscript.
Acknowledgements
The authors express particular gratitude to all the survey participants in Tama city, Tokyo, Japan.
Authors' Information
The first author, Tanji Hoshi (MD, Ph.D.), graduated from Fukushima Prefectural Medical University in 1978 and earned a Ph.D. from the Department of Public Health, Faculty of Medicine, The University of Tokyo in 1987. I dedicated my career to education, research, and practice in preventive medicine and public health. After working at the Ministry of Health and Welfare and the National Health Research Institute, I became a professor at Tokyo Metropolitan University. I worked there for 15 years and have mentored 24 doctors. The number of students earning a Ph.D. in philosophy has been the highest at our university.
References
- Labor Statistics Association. Trends in national hygiene 65 (2018): 82–84.
- Sakurai N, Hoshi T. The aim of health Japan 21. Hokennokagaku, 45 (2003).
- Scientific evidence of dental health and oral health that contributes to a healthy and long-lived society in 2015. Jpn Dent Assoc (2019).
- Fukai K, Takiguchi T, Ando Y, et al. Mortality rates of community-residing adults with and without dentures. Geriatr Gerontol Int 8 (2008): 152-159.
- Yoneyama T, Yoshida M, Matsui T, et al. Oral care and pneumonia. Oral care working group. Lancet 354 (1999): 515.
- Hoshi T, Yabuki T, Nagai H, et al. Causal structure of the existence of a family dentist and subsequent QOL and maintenance of survival. 8020. Hachi-Maru-Nii-Maru 15 (2016): 130–133.
- Hoshi T. SES. Dietary and lifestyle habits, three health-related dimensions, and healthy survival days. In The Structure of Healthy Life Determinants: Lessons from the Japanese Aging Cohort Studies; Hoshi, T., Kodama, S., Eds.; Springer: Singapore (2018) 134–189.
- Branch LG, Katz S, Kniepmann K, et al. A prospective study of functional status among community elders. Am J Public Health 74 (1984): 266-268.
- Koyano W, Shibata H, Nakazato K, et al. Measurement of competence: reliability and validity of the TMIG index of competence. Arch Gerontol Geriatr 13 (1991): 103-116.
- Kaplan GA, Camacho T. Perceived health and mortality: a nine-year follow-up of the human population laboratory cohort. Am J Epidemiol 117 (1983): 292-304.
- Rosella LC, Fu L, Buajitti E, et al. Death and chronic disease risk associated with poor life satisfaction: a population-based cohort study. Am J Epidemiol 188 (2019): 323-331.
- Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 109 (1979): 186-204.
- Seeman TE, Kaplan GA, Knudsen L, et al. Social network ties and mortality among the elderly in the Alameda County study. Am J Epidemiol 126 (1987): 714-723.
- Berkman LF. Health and ways of living: the Alameda County study. Oxford: Oxford University Press (1983).
- Finkel SE. Causal analysis with panel data. Thousand Oaks, CA, USA: Sage Publications (1995).
- Bentler PM, Dudgeon P. Covariance structure analysis: statistical practice, theory, and directions. Annu Rev Psychol 47 (1996): 563-592.
- Tano R, Hoshi T, Takahashi T, et al. The effects of family dentists on survival in the urban community-dwelling elderly. American Journal of Medicine and Medical Science 3 (2013): 156-165.
- Hoshi T. Causal structure for the healthy longevity based on the socioeconomic status, healthy diet and lifestyle, and three health dimensions, in Japan. In: Garg BS, editor. Health promotion - principles and approaches. Rijeka: Intech Open (2023) 1-19.
- Ogden GR, Macluskey M. An overview of the prevention of oral cancer and diagnostic markers of malignant change: 1. Prevention. Dent Update 27 (2000): 95-99.
- Reichart PA. Primary prevention of mouth carcinoma and oral precancerous conditions. Mund Kiefer Gesichtschir 4 (2000): 357-364
- Gellrich NC, Suarez-Cunqueiro MM, Bremerich A, et al. Characteristics of oral cancer in a central European population: defining the dentist's role. J Am Dent Assoc 134 (2003): 307-314.
- Takada Y, Maeda Y, Isada T. Characteristics of workers for whom oral hygiene education is effective. J Health Wellness Stat 51 (2004): 25-29.
- Wang Y, Wan EYF, Mak IL, et al. The association between trajectories of risk factors and risk of cardiovascular disease or mortality among patients with diabetes or hypertension: a systematic review. PLoS One 17 (2022): e0262885.
- Yamaza H, Takayama F, Ogasawara T, et al. A Case Report of Dental Treatment for Removing Sources of Oral Infection before Heart Surgery in a Patient with Noonan Syndrome through Medical Examination. Soc. Disabil. Oral Health, 41 (2020): 318–324.


 Impact Factor: * 3.4
Impact Factor: * 3.4 Acceptance Rate: 78.89%
Acceptance Rate: 78.89%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 