Clinical Profile of Patients with Vogt–Koyanagi-Harada Disease at a Tertiary Eye Hospital in Bangladesh
Arzumand Binte Yousuf Muna1*, Pankaj Kumar Roy2, Tamjida Farhana3, Md. Ershadul Haque Rahat4, Masmum Sababa5, Rehnuma Sadia Siddiqua6, A. K. M Shahidur Rahman7
1Consultant Ophthalmologist, Lions Eye Institute and Hospital, Dhaka, Bangladesh
2Professor, Vitreo Retina Department, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh
3Consultant Ophthalmologist, Department of Ophthalmology, Combined Military Hospital (CMH), Dhaka, Bangladesh
4Assistant Registrar, Department of Ophthalmology, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh
5Assistant Registrar, Department of Ophthalmology, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh
6Consultant Ophthalmologist, Department of Ophthalmology, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh
7Medical Officer, Department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
Corresponding author:Dr. Arzumand Binte Yousuf Muna, Consultant Ophthalmologist, Lions Eye Institute and Hospital, Dhaka, Bangladesh
Received: March 20, 2023; Accepted: March 27, 2023;Published: March 31, 2023
Article Information
Citation: Muna ABY, Roy PK, Farhana T, Rahat MEH, Sababa M, Siddiqua RS, Rahman AKMS. Clinical Profile of Patients with Vogt–Koyanagi- Harada Disease at a Tertiary Eye Hospital in Bangladesh.Journal of Ophthalmology and Research. 6 (2023): 17-22.
DOI: 10.26502/fjor.2644-00240078
View / Download Pdf Share at FacebookAbstract
Background: Vogt-Koyanagi-Harada (VKH) disease is an autoimmune inflammatory disease characterized by bilateral panuveities affecting the young adults. Approximately 3% of the uveitis patients are VKH patients. Objective: To assess the clinical profile of patients with Vogt-Koyanagi- Harada (VKH) disease.
Methods: This cross-sectional observational study was conducted over 30 diagnosed patients of VKH disease in uvea clinic of National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh. Patients were selected according to specific selection criteria. All the relevant data were recorded in a pre-designed data collection sheet. Results were analyzed by statistical tests.
Results: The mean age of the study patients was 40.2±6.53 years, range 26-59 years. Out of 30 patients; 9(30%) were male and 21(70%) were female. Male to female ratio was 1:2.3. In this study we found all VKH diseases (100% cases) were in both eyes. The clinical type of VKH disease was classified as complete in 2 patients (4 eyes), incomplete in 17 patients (34 eyes), and probable in 11 patients (22 eyes). Regarding clinical presentation; posterior uveitis was in 14 eyes and panuveitis in 46 eyes. Twenty-six eyes (43.3%) had acute VKH disease, 24 eyes (40%) had convalescent stage, and 10 eyes (16.7%) had recurrent uveitis. Meningism [17(56.7%)] and headache [16(53.3%)] were the commonest acute presentations followed by vitiligo [10(33.3%)] and poliosis [3(10.0%)]. Sensorineural hearing loss was present in 2(6.7%) chronic cases. The ocular findings of slit-lamp examination were circumciliary congestion in 32 eyes (53.3%), keratic precipitates in 30 eyes (50.0%) and iris nodules in 10 eyes (16.7%). Fundus examination revealed that vitritis in 60 eyes (100%), optic disc involvement in 34 eyes (56.7%), exudative retinal detachment in 38 eyes (63.3%), sunset glow fundus in 32 eyes (53.3%), Dalen-Fuchs nodules in 16 eyes (26.7%) and choroidal detachment in 4 eyes (6.7%). We found 71.7% of VKH patients had substantial vision loss.
Conclusion: Vogt-Koyanagi-Harada disease is a bilateral, diffuse, granulomatous panuveitis, affects more in females of the middle age. Most of our VKH patients were in the chronic stage of the disease and had substantial vision loss. Early recognition and aggressive treatment of VKH disease result in good visual outcome.
Keywords
<p>Autoimmune Disorder, Clinical Profile, Uveitis, Visual Outcome, Vogt–Koyanagi-Harada Disease (VKH Disease).</p>
Article Details
Introuduction
Vogt-Koyanagi-Harada (VKH) disease is a granulomatous panuveitis with or without extraocular manifestations, leading to significant vision loss [1]. It is an autoimmune disorder that typically affects genetically susceptible individuals and clinically presents as bilateral panuveitis with exudative retinal detachments and hyperemic, swollen optic discs, which are associated with neurological and auditory manifestations [2, 3, 4]. VKH disease was initially divided into two distinct conditions: chronic severe anterior uveitis, alopecia, polio, perilimbal vitiligo and dysacusia are all symptoms of the Vogt-Koyanagi syndrome; Harada's disease is characterized by bilateral exudative uveitis and pleocytosis of cerebrospinal fluid [4, 5]. Later, Babel, Bruno, and McPherson noted that these findings represented a single, progressive syndrome, and the name was combined into VKHD syndrome [6]. Vogt-Koyanagi-Harada (VKH) disease has variable incidence. The incidence of VKH disease may vary according to geographical distribution and ethnicity [4]. The disease primarily affects the pigmented races [6]. It was reported that VKH disease is more prevalent in people with Asian, Hispanic, Indian, Native American, or Mediterranean origin, accounting for 7%–22.4% of uveitis referrals [7]. But it is almost uncommon in Caucasians and people of Turkish descent, where it accounts for <3% of uveitis referrals [7]. VKH disease commonly affects young females of second and fifth decades of life, at a ratio 2:1 [4, 6]. However, some studies have reported pediatric cases, elderly onset, and equal sex predilection [8]. Theories speculate that a T-cell mediated autoimmune response against one or more antigens linked to melanocytes; melanin and retinal pigment epithelium (RPE) may play a significant role in the disease despite the fact that the exact pathogenesis of the condition is unknown [3].
Early diagnosis and prompt and adequate treatment with immunosuppressive agent like corticosteroids and other immunomodulatory drugs may halt disease progression, prevent recurrence, prevent vision loss and visual morbidity. For proper diagnosis and management international diagnostic criteria of VKH was implemented in 2005 internationally [6]. As a bilateral vision threatening disease, without proper management VKH disease leads to blindness [4]. Therefore to prevent this blindness, first need to a clean cut diagnosis. Although ocular manifestations are common, VKH disease patients frequently land up in general physician’s clinic or they are referred to neurologist for their extra-ocular features and undergo unnecessary investigations/imaging, which may further delay the diagnosis and treatment. The disease has very good prognosis when managed in time by an ophthalmologist. The aim of this study was to assess the clinical profile of patients with VKH disease at a tertiary care hospital in Bangladesh.
Methodology
This hospital based observational study was carried out at Retina Department, National Institute of Ophthalmology and Hospital (NIO&H), Sher-e Bangla Nagar, Dhaka, Bangladesh from January 2021 to June 2021. A total of 30 patients with Vogt-Koyanagi-Harada (VKH) disease attended at the out- patient department (OPD) of NIO&H were included for this study by purposive sampling technique. The clinical records of these 30 patients diagnosed with VKH were reviewed for demographics, clinical signs, complications and visual outcome. All study patients underwent a complete ophthalmic examination, including measurement of best corrected visual acuity (VA), slit-lamp examination, applanation tonometry, dilated fundus examination with scleral indentation, colour fundus photography, fundus fluorescein angiography (FFA), optical coherence tomography (OCT) and ocular ultrasonography (selected cases- if the view of the fundus was not clear), Audiometry and tympanogram for evaluation of internal ear were done accordingly. External examination was done to evaluate the presence of poliosis and vitiligo skin, lashes, eyebrow, hairs etc. Each study patient was followed up at a regular interval during the study period.
Ethical implications: Ethical approval was taken from respective authority. The ethical principle of Helsinki declaration was followed.
Data analysis: Data were checked, cleaned and edited properly before analysis. Statistical analysis was carried out by using Statistical Package for the Social Sciences (SPSS) version 22.0 software. Descriptive statistics were used for the interpretation of the findings.
Results
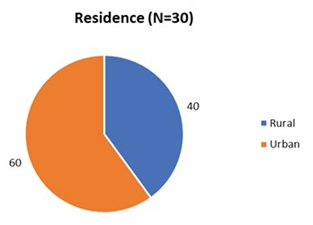
This study was intended to assess the clinical profile of VKH patients at NIO&H, Dhaka, Bangladesh. A total of thirty (30) diagnosed VKH patients were enrolled. The mean age of the study patients was 40.2±6.53 years and ranged was 26-59 years. Maximum (46.7%) study patients were in 41-50 years age group followed by 40% patients were in age group of 30-40 years. Of them male was 30% and female was 70%, a male to female ratio was 1:2.3 (Table- 1). Maximum study patients (60.0%) were came from urban area and 40.0% from rural area (Figure- 1).
It was observed that all cases of VKH disease were in both eyes (bilateral). The clinical type of VKH disease was classified as complete in 2 patients (4 eyes), incomplete in 17 patients (34 eyes), and probable in 11 patients (22 eyes). Clinical presentation was posterior uveitis in 14 eyes and panuveitis in 46 eyes. Twenty six eyes (43.3%) had acute uveitic VKH disease, 24 eyes (40%) had convalescent stage and 10 eyes (16.7%) had chronic recurrent uveitis (Table- 2).
Among the study patients; meningitis (56.7%) was
Table 1: Demographic characteristics of the study patients (N=30)
|
Variables |
Number of patients (n) |
Percentage (%) |
|
Age |
||
|
Mean±SD |
40.2±6.53 years |
|
|
Range |
(26 - 59) years |
|
|
Age groups (years) |
||
|
20-30 |
2 |
6.7 |
|
31-40 |
12 |
40 |
|
41-50 |
14 |
46.7 |
|
51-60 |
2 |
6.7 |
|
Gender |
||
|
Male |
9 |
30 |
|
Female |
21 |
70 |
|
Male to female ratio |
1.02.03 |
|
Table 2: Clinical characteristics of the study patients (N=30)
|
Clinical characteristics* |
Number (n) |
Percentage (%) |
|
Laterality |
||
|
Bilateral |
30 (patients) |
100 |
|
Anatomical classification |
||
|
Panuveitis |
46 (eyes) |
76.7 |
|
Posterior uveitis |
14 (eyes) |
23.3 |
|
Clinical types |
||
|
Probable |
22 (eyes) |
36.7 |
|
Incomplete |
34 (eyes) |
56.7 |
|
Complete |
4 (eyes) |
6.7 |
|
Course |
||
|
Acute uveitic |
26 (eyes) |
43.3 |
|
Convalescent stage |
24 (eyes) |
40 |
|
Chronic recurrent |
10 (eyes) |
16.7 |
*Multiple responses the commonest acute presentations followed by headache (53.3%), vitiligo (33.3%) and poliosis (10.0%). In chronic cases; sensorineural hearing loss was present in 2 (6.7%) cases (Table- 3).
The ocular findings of slit-lamp examination revealed that; circumciliary congestion was in 32 eyes (53.3%), keratic precipitates in 30 eyes (50.0%) and iris nodules in 10 eyes (16.7%) with the presence of anterior chamber flare and cells (Table- 4).
Fundus examination revealed that; vitritis in 60 eyes (100%), optic disc involvement in 34 eyes (56.7%), exudative retinal detachment in 38 eyes (63.3%), sunset glow fundus in 32 eyes (53.3%), Dalen-Fuchs nodules in 16 eyes (26.7%) and choroidal detachment in 4 eyes (6.7%) (Table- 5).
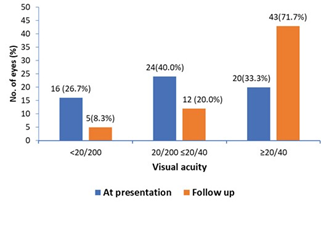
In this present study, 20 (33.3%) eyes presented with best corrected visual acuity (BCVA) of 20/200 or worse at presentation, at follow up visual acuity was ≥20/40 in 71.7% eyes. In 24(40.0%) eyes visual acuity was 20/200-≤20/40 at presentation and at follow up that was in 12(20.0%) eyes. In
Table 3: Distribution of diverse systemic manifestations (N=30)
|
Systemic manifestations* |
Number of patients (n) |
Percentage (%) |
|
Meningitis |
17 |
56.7 |
|
Headache |
16 |
53.3 |
|
Vitiligo |
10 |
33.3 |
|
Poliosis |
3 |
10 |
|
Hearing loss |
2 |
6.7 |
*Multiple responses
Table 4: Clinical findings on anterior segment manifestations
(N=30)
|
Anterior segment manifestations* |
Number of eyes |
Percentage (%) |
|
Circumciliary congestion |
32 |
53.3 |
|
Keratic precipitates (KP) |
30 |
50 |
|
Fine KPs |
22 |
36.7 |
|
Mutton fat KPs |
8 |
13.3 |
|
Iris nodules |
10 |
16.7 |
|
Flare |
38 |
63.3 |
|
1+ |
20 |
33.3 |
|
2+ |
14 |
23.3 |
|
3+ |
4 |
6.7 |
|
Cells |
44 |
73.3 |
|
1+ |
20 |
33.3 |
|
2+ |
22 |
36.7 |
|
3+ |
2 |
3.3 |
*Multiple responses
Table 5: Clinical findings on posterior segment manifestations
(n=30)
|
Posterior segment manifestations* |
Number of eyes |
Percentage (%) |
|
Vitritis |
60 |
100 |
|
1+ |
44 |
73.3 |
|
2+ |
12 |
20 |
|
3+ |
4 |
6.7 |
|
Disc hyperemia |
34 |
56.7 |
|
Disc edema |
34 |
56.7 |
|
Retinal detachment |
38 |
63.3 |
|
Posterior pole |
38 |
63.3 |
|
Periphery |
20 |
33.3 |
|
Sunset glow fundus |
32 |
53.3 |
|
Dalen-Fuchs nodules |
16 |
26.7 |
|
Choroidal detachment |
4 |
6.7 |
*Multiple responses
Discussion
Vogt-Koyanagi-Harada (VKH) disease is a multisystem autoimmune disorder that primarily targets melanocytes, affects the eye, skin, inner ear, and meninges. In the eye, the disease affects the uveal tract, manifesting as granulomatous panuveitis. Acute presentation is characterized by the presence of exudative retinal detachment with preservation of the choriocapillaris. In the chronic stage, the disease is characterized by the presence of Dalen-Fuchs nodules and focal chorioretinal atrophy with loss of retinal pigment epithelium [9]. In chronic stage, patients develop extraocular manifestations. This cross-sectional hospital based observational study was carried out in Retina Department, National institute of ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh. The clinical profiles of thirty patients with Vogt-Koyanagi-Harada disease (VKH) were evaluated.
In present study the age ranged between 26-59 years, mean age was 40.2±6.53 years and a male to female ratio was 1:2.3. The prevalence of VKH disease among female was found to be more than male in our study. The findings from our study as well as from the earlier reports show that women are more likely to develop VKH disease than men [10-13], whereas Soon-Phaik Chee et al. have reported equal distribution in both sexes [14]. Diallo et al. reported forty-one patients (16 men and 25 women) average age at diagnosis was 38.7 years [11]. Most studies suggest a female predominance among patients with VKH disease, as in our study [10-13]. Most studies reported a mean age at presentation was 35–45 years of age [10-14].
In the present study the clinical type of VKH disease was classified as complete in 2(6.7%) patients (4 eyes), incomplete in 17(66.7%) patients (34 eyes), and probable in 11(36.7%) patients (22 eyes). Regarding clinical presentation; posterior uveitis was in 14(23.3%) eyes and panuveitis in 46(76.7%) eyes. Twenty six eyes (43.3%) had acute uveitic VKH disease, 24 eyes (40%) had convalescent stage and 10 eyes (16.7%) had chronic recurrent uveitis. In agreement with this study Mahendra das et al. reported posterior uveitis in 15 eyes and panuveitis in 55 eyes [15]; thirty eyes (42.8%) had acute VKH disease, 28 eyes (40%) had chronic presentation, and 12 eyes (17.1%) had recurrent uveitis [15]. The findings of this present study were also similar to that of Ilknur Tugal-Tutkun et al. with regard to clinical types of the disease; where incomplete VKH (57.7%) was identified as the commonest followed by probable (33.8%) and complete forms (8.4%) [16]. A study by Bawazeer et al. demonstrated that; at presentation 28.1% had complete disease, 56.2% had incomplete disease and 15.6% had probable disease [12]. In another study 11.8% was classified as complete, 71% incomplete, and 8.9% as probable disease [17]. These findings were different from the results of this current study could be due to ethnic diversity.
Clinical manifestations of VKH syndrome depends on the stage of the disease [18-21]. There are four stages of VKH disease- prodromal stage, acute uveitic stage, convalescent stage and chronic recurrent stage. The prodromal stage resembles a viral illness characterised by headache, fever, orbital pain, nausea and dizziness, which lasts for 3-5 days. Patients usually complain of blurred vision, photophobia, hyperaemia of the conjunctiva and ocular pain. Uveitic stage presents with blurred visual acuity in both eyes, one eye was affected first. In 94% cases, second eye usually affected within 2 weeks [18]. This condition is characterised by thickening of the posterior choroid. This manifests clinically as hyperaemic oedematous optic disc, multiple serous detachments in the posterior pole, which can be extensive retinal oedema with elevation of peripapillary region. When the inflammation increases, it involves the anterior chamber presenting as a granulomatous panuveitis [18]. Chronic stage also known as the convalescent stage develops weeks after the uveitis has subsided. This characterised by depigmentation of the fundus and development of cutaneous features like poliosis and vitiligo. Perilimbal vitiligo (Sugiura’s sign) is also seen in this stage. The sunset glow fundus is due to the depigmentation of the peripheral fundus, which leads to a pale disc and reddish orange choroid. Recurrent stage consists of panuveitis with acute exacerbation of anterior uveitis. Iris nodules may appear in this stage. During this phase, most of vision-threatening complications like cataract, glaucoma and subretinal neovascularisation may develop [19]. In this context we found; twenty six eyes (43.3%) had acute uveitic VKH disease, 24 eyes (40%) had convalescent stage and 10 eyes (16.7%) had chronic recurrent uveitis.
According to present study meningitis (56.7%) was the commonest systemic manifestations followed by headache (53.3%), poliosis (10.0%), vitiligo (33.3%) and in chronic cases sensorineural hearing loss was present in 6.7% cases. In agreement with this study, Bawazeer et al. reported extra- ocular symptoms were common in their patients; where 50% patients presenting with headache, 9.3% had decreased in hearing and 40% with neck pain, 9.3% presented with poliosis, 15.6% with vitiligo and 25% alopecia [12]. Rao et al. found that 49% of VKH patients had headache and 36% had neck stiffness [22]. In accordance of this study Diallo et al. reported 17 patients complained of auditory and vestibular manifestations (41%): hearing loss (24%) and tinnitus (22%), while eleven patients had dermatological manifestations (27%) [11].
According to present study ocular findings of slit-lamp examination were circumciliary congestion in 32 eyes (53.3%), keratic precipitates in 30 eyes (50.0%) and iris nodules in 10 eyes (16.7%) with the presence of anterior chamber flare and cells. Fundus examination revealed that; vitritis in 60 eyes (100%), optic disc involvement in 34 eyes (56.7%), exudative retinal detachment in 38 eyes (63.3%), sunset glow fundus in 32 eyes (53.3%), and Dalen-Fuchs nodules in 16 eyes (26.7%). These findings were consistence with a couple of previous studies [18-21]. Nakayma et al.reported the most common anterior segment findings at presentation were anterior chamber cells in 87 eyes (39.2%), with 28 eyes (12.6%) having 2+ or greater cells, keratic precipitates in 32 eyes (14.4%), shallow anterior chamber in 16 eyes (7.2%) and intraocular pressure ≥22 mm Hg in 9 eyes (4.1%); Posterior segment findings were serous retinal detachment confined to the posterior pole in 202 eyes (91.0%), optic disc hyperaemia in 89 eyes (40.1%) [19].
In this study among the study patients; 33.3% eyes presented with best corrected visual acuity (BCVA) of 20/200 or worse at presentation, at follow up visual acuity was ≥20/40 in 71.7% eyes. In 40.0% eyes visual acuity was 20/200-≤20/40 at presentation and at follow up that was in 20.0% eyes. In 26.7% eyes visual acuity was <20/200 at presentation and at follow up that was in 8.3% eyes. In this context, Yang et al. reported most VKH patients had severely decreased vision at their first visit, BCVA of 20/200 in 45% of the individuals [20]. Read et al. observed visual acuity of 20/40 or better; 47 eyes (27%) with visual acuity of 20/50 to 20/100, and 69 eyes (40%) with visual acuity of 20/200 or worse [2].
The clinical features of VKH disease in South Asian countries are similar to the earlier reports [6-8], except for the increased presentations of posterior segment inflammations than the anterior segment reactions during the recurrences [9]. Extra ocular manifestations were not noticed in acute cases with aggressive management with systemic steroids and immunosuppressive therapy. Chronic and recurrent cases had extraocular manifestations at the time of presentation in majority of the cases. Early and aggressive therapy resulted in good visual outcome in majority of VKH disease patients.
Conclusion
Vogt-Koyanagi-Harada (VKH) disease is a bilateral, diffuse, granulomatous panuveitis, which occurs more in females of the middle age. Most of our patients were in the chronic stage of the disease and their substantial vision loss was found at the time of examination. Early diagnosis and aggressive treatment of VKH disease result in good visual outcome in typical VKH cases.
Limitations of the study
It was a single center study with a relatively small sample
size.
Recommendation
Further study with larger sample size may be reproduced
for a more conclusive result.
Conflicts of interest
The authors declared that they have no conflict of interest
regarding the publication of this article.
References
- Moorthy RS, Inomata H, Rao Vogt–Koyanagi– Harada syndrome. Surv Ophthalmol 39(4) (1995): 265– 292.
- Read RW, Rechodouni A, Butani N, et al. Complications and prognostic factors in Vogt–Koyanagi–Harada Am J Ophthalmol 131(5) (2001): 599–606.
- Norose K, Yano A. Melanoma specific Th1 cytotoxic T lymphocyte lines in Vogt–Koyanagi–Harada Br J Ophthalmol 80(11) (1996): 1002–1008.
- Shi T, Lv W, Zhang L, et Association of HLA-DR4/HLA-DRB1*04 with Vogt–Koyanagi–Harada disease: a systematic review and meta-analysis. Sci Rep 4(2014): 6887.
- Harada Clinical study of nonsuppurative choroiditis: a report of acute diffuse choroiditis. Acta Soc Opthalmol Jpn 30 (1926):356–378.
- Herbort CP, Mochizuki Vogt–Koyanagi–Harada disease: inquiry into the genesis of a disease name in the historical context of Switzerland and Japan. International ophthalmology 27(2) (2007): 67-79.
- Al Dhahri H, Al Rubaie K, Hemachandran S, et Patterns of uveitis in a University-Based Tertiary Referral Center in Riyadh, Saudi Arabia. Ocul Immunol Inflamm 10 (2014): 1–9.
- Wang Y, Chan Gender differences in Vogt– Koyanagi–Harada disease and sympathetic ophthalmia. J Ophthalmol 2014(2014): 157803.
- Rao NA. Pathology of Vogt–Koyanagi–Harada disease. International ophthalmology 27(2-3) (2007): 81-5.
- Kiyomoto C, Imaizumi M, Kimoto K, et Vogt- Koyanagi-Harada disease in elderly Japanese patients. Int Ophthalmol 27(2-3) (2007):149–53.
- Diallo K, Revuz S, Clavel-Refregiers G, et Vogt- Koyanagi-Harada disease: a retrospective and multicentric study of 41 patients. BMC ophthalmology 20(1) (2020):1-8.
- Bawazeer AM, Nizamuddin SH, Raffa LH, et al. Clinical characteristics of Vogt–Koyanagi–Harada syndrome in a tertiary medical centre in western region of Kingdom of Saudi Arabia. Journal of Taibah University Medical Sciences 8(1) (2013): 24-30.
- Islam SM, Tabbara Causes of uveitis at the Eye Centre in Saudi Arabia: a retrospective review. Ophthalmic Epidemiol 9(4) (2002): 239–249.
- Chee S-P, Jap A, Bacsal K. Spectrum of Vogt-Koyanagi- Harada disease in Singapore. Int Ophthalmol 27(2-3) (2007): 137–42.
- Mahendra das P, Kawali A, Bharti N, et al. The clinical spectrum of Vogt-Koyanagi-Harada syndrome: A single- center experience from South India. Internet Journal of Rheumatology and Clinical Immunology 26 (2013): 1(S1).
- Tugal-Tutkun I, Ozyazgan Y, Akova YA, et The spectrum of Vogt-Koyanagi-Harada disease in Turkey: VKH in Turkey. Int Ophthalmol 27(2-3) (2007):117–23.
- Kitamura M, Takami K, et al. Comparative study of two sets of criteria for the diagnosis of Vogt–Koyanagi– Harada’s Am J Ophthalmol 139(6) (2005): 1080– 1085.
- Hariharan L, Mohankumar A. Clinical profile of Vogt- Koyanagi-Harada syndrome in a tertiary eye care centre. Evid. Based Med. Healthc 4(70) (2017): 4191-4195.
- Nakayama M, Keino H, Watanabe T, et Clinical features and visual outcomes of 111 patients with new- onset acute Vogt-Koyanagi-Harada disease treated with pulse intravenous corticosteroids. British Journal of Ophthalmology 103(2)( 2019): 274-8.
- Yang P, Ren Y, Li B, et al. Clinical characteristics of Vogt–Koyanagi–Harada syndrome in Chinese patients. Ophthalmology 114(3) (2007): 606-14.
- Singh R, Gupta V, Gupta Pattern of uveitis in a referral eye clinic in north India. Indian J Ophthalmol 52 (2004): 121–12.
- Rao NA, Gupta A, Dustin L, Chee SP, et Frequency of distinguishing clinical features in Vogt-Koyanagi-Harada disease. Ophthalmology 117(3) (2010): 591-9.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
