Continuing Development of Stroke Services using the Structured Judgement Review
Jade Anne Thomas1, Katja Adie2*, Kyaw Lin Saw3
1Eldercare Registrar (ST4), Royal Cornwall Hospital, Treliske, Truro TR1 3LQ, UK
2Consultant in Stroke and Eldercare, Royal Cornwall Hospital, Treliske, Truro TR1 3LJ, UK; Honorary Lecturer, University of Exeter Medical School, St Luke's Campus, Exeter, EX1 2LU, UK
3Trust Doctor (Stroke Medicine,) Royal Cornwall Hospital, Treliske, Truro TR1 3LQ, UK
*Corresponding author: Katja Adie, Consultant in Stroke and Eldercare, Royal Cornwall Hospital, Treliske, Truro TR1 3LQ, UK; Honorary Lecturer, University of Exeter Medical School, Stocker Rd, Exeter EX4 4PY, UK
Received: 19 September 2019; Accepted: 25 September 2019; Published: 30 September 2019
Article Information
Citation: Jade Anne Thomas, Katja Adie, Kyaw Lin Saw. Continuing Development of Stroke Services using the Structured Judgement Review. Cardiology and Cardiovascular Medicine 3 (2019): 373-393.
View / Download Pdf Share at FacebookAbstract
The Royal Cornwall Hospitals Trust (RCHT) has undertaken a series of in-depth mortality reviews following publication of data demonstrating the trust to be an outlier for stroke associated mortality. This report of our 2017-18 data follows published outcomes and recommendations from the primary 2016-17 RCHT review. Our patients have high numbers of comorbidities, sustained moderate to severe strokes with a high hemorrhagic to ischemic stroke ratio. Patient care was reviewed using the Structured Judgement Review (SJR) process and care received was deemed as good to excellent in the majority of cases. Analysis of specific cases of low care scores has led to further recommended changes for local practice including; increased staffing levels on the stroke unit, increased number of hyperacute stroke beds, collaboration with primary care to prioritize AF detection and management, improved anticoagulation reversal processes within the emergency department and implementation of recommendations of national stroke guidelines for blood pressure control for haemorrhagic strokes.
Keywords
<p>Stroke; Mortality; Structured Judgement review (SJR); Mortality Review; Stroke Care</p>
Article Details
Introduction
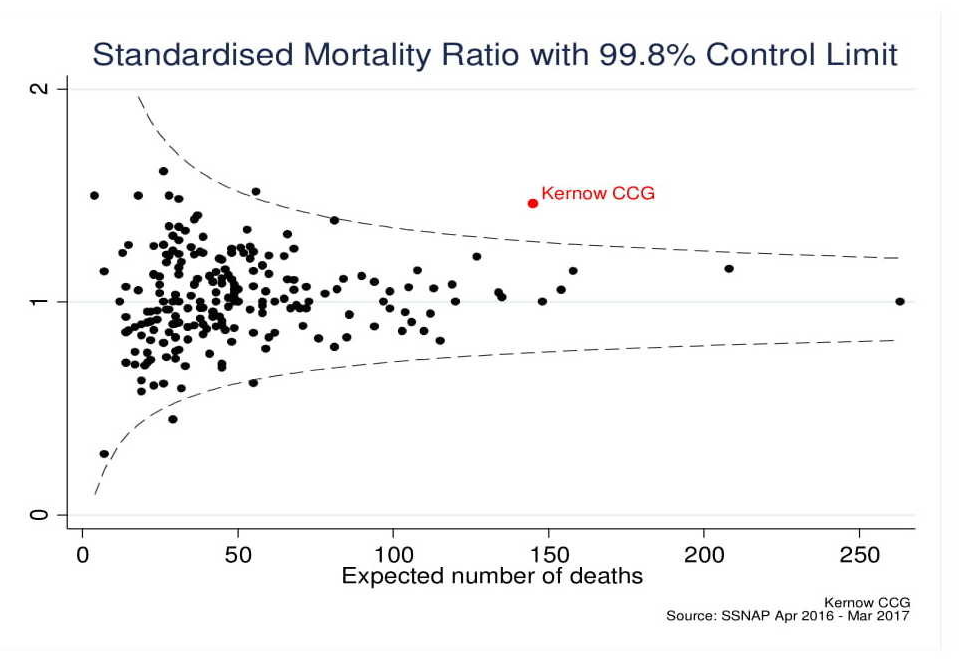
In 2015-16 the Royal Cornwall Hospitals Trust (RCHT) was demonstrated as having higher stroke associated mortality rates than national average [1]. The 2016-17 Sentinel Stroke National Audit Programme (SSNAP) continued to show RCHT as an outlier for stroke related mortality, having observed 172 deaths in comparison to the 139 expected deaths predicted using standardised mortality ratios (SMR) [2,3]. A crude mortality rate of 21% was demonstrated with a SMR of 1.45 (Figure 1.) This instigated an in-depth local mortality review using the Royal College of Physicians Structured Judgement Review (SJR) process [4]. Published results of our 2016-17 mortality review catalysed changes to the trusts’ stroke services including improved diagnostic coding, formation of an AF working group with primary care, development of a business case for new CT scanning facilities, and work on improved quality of record keeping [5,6]. This report summarises our secondary review of stroke related deaths from 2017-18 data and the ongoing development of stroke services at the RCHT.
Methods
Case notes from patients admitted with stroke as a primary diagnosis between 1st April 2017 and 31st March 2018 who died within 30 days of admission were reviewed. Of the 135 identified cases 80 sets of notes were available at the time of audit. Variables collected from case notes included; patient comorbidities, stroke type, National Institute Health Stroke Severity Scale (NIHSS), pre morbid Modified Rankin Scale alongside demographic data, length of stay, and incidence of aspiration pneumonia.
The NIHSS is a measure of stroke severity. The scale is composed of 11 items and scored from 0-42 depending on level of impairment; a score of 1-4 indicates minor stroke, 5-15 moderate stroke, 16-20 moderate to severe, and 21-42 severe stroke [7]. The second scale used within our review was the Modified Rankin Scale (MRS,) the MRS is frequently used within stroke statistics to gauge the level of disability of a patient pre and post stroke [8]. The scale is pictorial with a description of the patients’ level of dependence from 0- no symptoms, 3- moderate disability, to 6- dead.
Data on specific targets for quality stroke care measured by the SNAPP were also collated. This included arrival to stroke unit within 4 hours, swallow screen within 4 hours, and consultant review within 24 hours [9].
The structured judgement review (SJR) process was utilised to provide a validated 2 stage review of care [4]. The first stage requires the reviewer to provide independent subjective ratings for each phase of care received (admission and initial care, perioperative and procedural care, ongoing care, and end-of-life care.) The ratings are graded from 1 (poor care) to 5 (excellent care) and include qualitative comments informing the judgement. The final part of the SJR looks at avoidability of death (see Table 1,) the reviewer accounts for all information gained from the case note review in providing an overall score. If the initial reviewer’s score is 1 or 2 (very poor or poor accordingly,) then a second review takes place within the hospital governance process. Explicit comments are again provided to justify scoring and highlight areas in need of improvement. Our mortality reviews were undertaken by consultants and registrars working within the stroke department.
|
Avoidability Of Death Score |
|
6: Definitely not avoidable |
|
5: Slight evidence of avoidability |
|
4: Possibly avoidable but not very likely (Less than 50:50) |
|
3: Probably avoidable (more than 50:50) |
|
2: Strong evidence of avoidability |
|
1: Definitely avoidable |
Table 1: Structured Judgement Review Avoidability of Death Score
Results
In the 2017-18 audit 926 patients were admitted with a stroke and of these 135 patients died (14.6%). The median age of patients who died was 83 years (IQR 73-88.) Twenty five patients (31%) had haemorrhagic and fifty five had ischaemic strokes (69%). Median length of stay was 7 days (IQR 3-10).
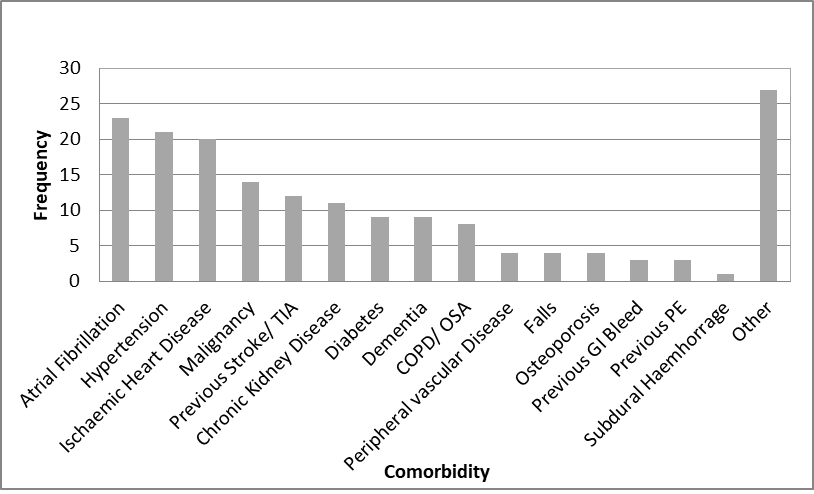
In relation to pre stroke morbidity, Forty seven patients had 3 or more comorbidities (59%) and only 3 patients had no known prior health conditions. Unsurprisingly the majority of comorbidities were cardiovascular risk factors, 23 patients with atrial fibrillation (29%) and 21 patients with hypertension (26%).
The patients reviewed had a median MRS score of 2 prior to admission indicating slight disability. The median NIHSS score on admission was 19 (IQR 14-26) indicating moderate to severe stroke.
The SJR audit results are summarised in Table 2. Care was deemed good or excellent in 91.3% of the cases. Similarly high scores were documented for quality of record keeping. Judgement comments included regular senior reviews, appropriate use of palliative pathway, good quality admission record, and prompt family discussions. Secondary review was undertaken for 5 cases (8.7%) with scores of 2 or below. Management of anticoagulation surrounding stroke (reversal in 1 case and initiation of anticoagulation in 1 case) were among rational for low scores, alongside quality of documentation, level of nursing input and timing of medical reviews.
|
Care Score |
Quality of Records |
Overall Care |
|
5 (Excellent) |
56 |
45 |
|
4 |
17 |
28 |
|
3 |
5 |
2 |
|
2 |
2 |
4 |
|
1 (Very Poor) |
0 |
1 |
|
Overall |
80 |
80 |
Table 2: SRJ Results for Quality of Record Keeping and Overall Care
88% of deaths were seen as unavoidable during the second part of the SJR rankings. In no cases was a score of 0-2 demonstrating strong evidence of avoidability given. 5 cases were given intermediate scores of 3-5, reviewers comments for these judgements are summarised in Table 3.
|
Avoidabilty of Death Score |
Reasons for Scoring |
|
5: Slight evidence of avoidability |
Lack of equipment (mittens for nasogastric tube) Delay in giving medications and management Poor documentation Blood pressure control in haemorrhagic stroke |
|
4: Possibly avoidable but not very likely (less than 50:50) |
Poor documentation Poor medical input Poor control of Blood pressure after ischaemic stroke Consideration of earlier imaging in event of deterioration |
|
3: Probably avoidable (more than 50:50) |
Missed opportunity of treating AF in community Consideration for early percutaneous feeding tube Post thrombolysis bleed (no protocol violation) |
Table 3: Avoidability of Death Results
Care at the RCHT measured by SSNAP key indicators compared favorably when considering all stroke admissions, higher than national average rates for arrival to stroke unit within 4 hours, swallow screen within 4 hours and consultant review within 24 hours were demonstrated [9]. However, patients who died had poorer scores for all three measures (Table 4). Aspiration pneumonia rates were reviewed as the association with stroke mortality is highly recognized, though not a measure on the national database, 40% of the audited cohort had a diagnosis of aspiration pneumonia documented within their stay.
|
Deceased patients N=80 |
All stroke admissions N=926 |
National Average SSNAP |
|
|
Arrival to stroke unit within 4 hours |
46.25% |
60.20% |
57.10% |
|
Swallow screen within 4 hours |
66.25% |
80.50% |
75.40% |
|
Consultant review within 24 hours |
61.25% |
86.30% |
83.30% |
|
Aspiration Pneumonia |
40% |
No data |
No data |
Table 4: RCHT performance compared to SSNAP Key Indicators [9]
Discussion
The audited cohort was shown to be older than national average for stroke (83 vs 79 years), with moderate to severe stroke severity, a higher proportion of haemhorragic vs ischaemic strokes -31% compared to 25% national average, was also seen [3]. Poor premorbid status was demonstrated by high numbers of comorbidities and median MRS scores of 2 (national average 0 for all stroke admissions) [3]. The standardised mortality ratio takes into account age, atrial fibrillation, type and severity of stroke, however number of comorbidities or level of function prior to stroke (reflected in pre-morbid MRS scores) are not accounted for [2].
Of patients dying from stroke within our audited population 29% had atrial fibrillation (AF) as a known co-morbidity. Timely identification and management of AF is paramount to stroke prevention [10] and better detection and management of AF may lead to reduction in stroke and mortality. Results from our audit were presented to the stroke mortality board. The local care quality commission AF working group, formed following commissioners’ recognition of AF management as a priority, are currently working with the primary care teams to improve detection and management of AF in the community.
Overall the majority of patients received good to excellent care during their admission. Of the 80 patients dying from their stroke, 65 patients passed away on the stroke unit (81%). 2 of the 5 cases reviewed as having care scores of 2 or below were cared for on non-stroke units, emphasising the importance of stroke unit care. Review of specific cases showed timely nursing input and medical review as rationale for care scores of <2 in two cases. The standard of documentation was again, as per the 2017 review, commented on as an area for improvement. The audit findings provide evidence for the need to increase nursing and medical staffing on the stroke unit.
Management of blood pressure (1 haemorrhagic stroke case and 1 ischaemic) was also provided as reasoning for intermediate avoidability of death scores. The higher than national average mortality in haemorrhagic stroke patients has been recognised as an area for improvement at our stroke unit. The recognition and prompt action for reversal of anticoagulation in haemorrhagic stroke and blood pressure management are key to reduction of stroke morbidity and mortality [11,12]. Both of these fundamental aspects were recognized for improvement within our audit in a very small number of cases. For prompt management of anticoagulation reversal in required cases a new international normalised ratio (INR) point of care machine was installed within the emergency department and guidance targets of reversal of INR within 1 hour of arrival for haemorrhagic stroke patients implemented. A new local guideline for managing blood pressure in haemorrhagic stroke has also been implemented in line with Royal College of Physicians stroke guidelines [12].
Our review was limited to a selection of cases that were available during the time of audit and did not include all patients who have died of stroke in the time period and we may have missed other significant issues. Unfortunately resource constraints and access to notes did not allow review of all patients.
A further limitation was that the review was conducted by consultants and registrars within the stroke department raising opportunity for judgement bias recognized and raised by the assessors at trusts mortality meeting [1]. Mortality review is also prone to reviewer bias, leading reviewers to judge that a case has a lower quality of care than it actually is [13]. All reviewers were trained in the methodology and made aware of the above biases. An interdepartmental review was recommended last year and we have incorporated into our clinical service as sufficient specialist knowledge of impact of care on outcomes is required, alongside an in depth knowledge of the local policies and patient pathway in order to make department specific recommendations.
Conclusion
The RCHT stroke team undertakes ongoing mortality review in response to stroke associated mortality data. The majority of patients received good to excellent care and the stroke units overall performance with regards to SNAPP measured of quality stroke care is average. Our audit aimed to review in-depth aspects of care for improvement through a case by case basis. The identified areas of care for improvement are among those known to influence stroke outcomes; management of anticoagulation, treatment of blood pressure post stroke, time spent on acute stroke unit, nursing input and medical team reviews. Future focus for continued improvement of stroke services at RCHT is through increased staff levels and training, implementation of improved blood pressure management guidelines and improved ED resources for anticoagulation reversal. Better detection and management of AF in the community may lead to a reduction of AF associated strokes. The results of the interventions will take time to be embedded and influence data, but are important steps forward in the ongoing development of local stroke services and improving stroke associated mortality rates.
Conflicts of interests
None
Acknowledgements
We would like to thank Mr Richard Barrett, cardiac information system administrator, Royal Cornwall Hospital Trust for provision of data.
Author contributions
- Report author, data interpretation
- Report author, mortality review assessor, data collection, data interpretation
- Report author, mortality review assessor, data collection, data interpretation
References
- Sentinel Stroke National Audit Program. SSNAP key indicators. CCG portfolio April 2015-March 2016, 2016. Available online at strokeaudit.org/results/Clinical-audit/Clinical-CCG-LHB-LCG.aspx (Accessed 9/5/2018).
- Bray BD, Campbell J, Cloud GC, et al. Derivation and External Validation of a Case Mix Model for the Standardized Reporting of 30-Day Stroke Mortality Rates. Stroke 45 (2014): 3374-3380.
- Sentinel Stroke National audit Program. Mortality Public Table for SSNAP admissions 2016-2017. Sentinel Stroke National Audit Program SSNAP. Kings College London. 2017. https://www.strokeaudit.org/results/Clinical-audit/National-Results.aspx (accessed 23/8/2019)
- Royal College of Physicians. Using the structured judgement review method – a clinical governance guide to mortality case record reviews, 2016.
- Thomas J, Saw KL, Adie K. Stroke mortality audit using the Structured Judgement Review method. Clinical Medicine 19 (2019): 185-187.
- Hutchinson A, Coster JE, Cooper KL, et al. A structured judgement method to enhance mortality case note review: development and evaluation. BMJ Quality and Safety 22 (2013): 1032-1040.
- National Institute of Health, National Institute of Neurological Disorders and Stroke. Stroke Scale. https://www.ninds.nih.gov/sites/default/files/NIH_Stroke_Scale_Booklet.pdf. (accessed 24/8/2019)
- Bonita R, Beaglehole R. Modification of Rankin Scale: Recovery of motor function after stroke. Stroke 19 (1988): 1497-1500.
- Sentinel Stroke National audit Program. SSNAP Annual Results Portfolio for April 2017-March 2018 admissions and discharges. Kings College London. https://www.strokeaudit.org/results/Clinical-audit/National-Results.aspx (accessed 24/8/2019)
- Hart RG, Pearce LA, Aguilar MI. Meta-analysis: Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 146 (2007): 857-867.
- Parry-Jones AR, Di Napoli M, Goldstein JN, et al. : Reversal strategies for vitamin K antagonists in acute intracerebral hemorrhage. Ann Neurol 78 (2015): 54–62.
- Intercollegiate Stroke Working Party. National clinical guidelines for stroke. Royal College of Physicians 2016; 5th edition: 65-67.
- Hutchinson A, Coster JE, Cooper KL, Pearson M, McIntosh A, Bath PA. A structured judgement method to enhance mortality case note review: development and evaluation. BMJ Quality and Safety 22 (2013): 1032-1040.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 