Deleterious Impact of Non-Diabetic Cataract Surgery on the Values of Biomarkers of Oxidative Stress and Metabolic Syndrome in Kinshasa
Christian Mwembo Nkolomonyi1 , Moise Mvitu Muaka1,2, Edith Mboyo Efeko1, Ndimbani Malosa Franck2, Nganga Nkanga Mireille Solange3, Héritier Mawalala Malengele5,6, Christian Kisoka Lusunsi4,5, Benjamin Longo-Mbenza4,5,7*
1Department of Specialties, Service of Ophthalmology, University Clinics of Kinshasa, Kinshasa, University of Kinshasa, Democratic Republic of Congo
2Faculty of Medicine, Kongo University
3Department of Medical Biology, University Clinics of Kinshasa
4Department of Internal Medicine, Cardiology Service, University Clinics of Kinshasa, Kinshasa, University of Kinshasa, Democratic Republic of Congo
5Department of Public Health, Lomo University of Research, Kinshasa, University of Kinshasa, Republic Congo Democratic
6Department of Radiology, University Clinics of Kinshasa, Kinshasa, University of Kinshasa, Democratic Republic of Congo
7Walter Sisulu University, Department of Health, Umthatha , South Africa
*Corresponding author: Benjamin Longo-Mbenza. Department of Internal Medicine, Cardiology Service, University Clinics of Kinshasa, Kinshasa, University of Kinshasa, Democratic Republic of Congo, Department of Public Health, Lomo University of Research, Kinshasa, University of Kinshasa, Republic Congo Democratic.
Received: 14 August 2023; Accepted: 20 August 2023; Published: 06 November 2023
Article Information
Citation: Christian Mwembo Nkolomonyi, Moise Mvitu Muaka, Edith Mboyo Efeko, Ndimbani Malosa Franck, Nganga Nkanga Mireille Solange, Héritier Mawalala Malengele, Christian Kisoka Lusunsi, Benjamin Longo-Mbenza. Deleterious Impact of Non-Diabetic Cataract Surgery on the Values of Biomarkers of Oxidative Stress and Metabolic Syndrome in Kinshasa. Journal of Ophthalmology and Research. 6 (2023): 62-68.
DOI: 10.26502/fjor.2644-00240086
View / Download Pdf Share at FacebookAbstract
Study Background and Purpose: Cataract is considered a structural marker of systemic metabolic disorders. Its association with metabolic syndrome (MS) and oxidative stress has only been well established in diabetic patients. The objective of the present study was to evaluate the impact of non-diabetic cataract surgery on biomarkers of SM and oxidative stress according to the pre-post operative phases.
Material and Methods: This was a mixed study, a consecutive series combining an intervention (quasi-experimental study before and after cataract surgery), a documentary study (patient file), a comparative and evaluative approach involving 163 patients over the age of 40, during a period from September 1 to December 31, 2022 at the MASINA Ophthalmological Center. Nominal variables were presented as frequencies, while quantitative variables as means ± SD. Pearson's Chi-Square test and Yates' Chi-Square test were used to compare the proportions between two groups. The threshold for statistical significance was set at any value of P<0.05.
Results: Of a total of 163 patients, 60.1% (n=98) were men versus 39.9% (n=65) women. Nearly 81.6% (n=133) of the patients were of an advanced age-Senior ≥ 60 years old. Cataract surgery very significantly induced a deleterious impact on the rest of the components of the metabolic syndrome/insulin resistance-oxidative stress-atherosclerosis: the increase in mean BMI values (23.7 ± 4.1 vs 32.8 ± 5.4; P<0 .0001), CT (124.9±46.5 vs 279.6±88.7 mg/ dL ; P<0.0001), LDL (94.5±34.1 vs 191.4±65.9 mg/ dL ; P<0.0001), TG (90.7± 45.9 vs 200.6±73.9 mg/ dL ; P<0.0001) and glycaemia (92.7±8.1 vs 101.8±10.6 mg/ dL ; P<0.0001) in the postoperative phase being higher than those of the before surgery while the mean values of PAS, PAD, HDL and Albumin (P<0.0001) of the postoperative phase were lower than those of the phase before cataract surgery. Biomarkers of insulin resistance and atherogenicity were very significantly higher after cataract surgery: TYG (8.2±0.5 vs 9.2±0.4; P<0.0001), CT/HDL ratio (2.6±1.1 vs 16.9±28 ; P<0.0001), LDL/HDL ratio (1.93±0.8 vs 11.5±19.8; P<0.0001), TG/HDL ratio (1.8±0.9 vs 11.7±25.4; P<0.0001), Non HDL (74.9±48.3 vs 247.4 ±102.4mg/ dL ; P<0.0001).
Conclusion: The present study confirmed that cataract is a structural marker of systemic disorders and a state of pre-hypertension, pre-diabetes, preatherosclerosis and oxidative stress in Bantu patients. A multidisciplinary postoperative follow-up is necessary.
Keywords
<p>Cataract, Surgery, Biomarkers, Metabolic Syndrome, Oxidative Stress, Insulin Resistance, Kinshasa.</p>
Article Details
1. Introuduction
Traditionally, cataracts have been a huge global health burden [1,2]; it is characterized by the presence of lens opacity and by different pathological forms [1,3].
Epidemiological data highlight the prevalence, risk factors and predictors of medico-social complications characteristic of cataract in wealthy countries with modern surgical techniques and procedures [3,4]. Among the risk factors for cataracts, there is age, any age in general but especially advancing age, more vulnerable than congenital-infant age, arterial hypertension, excessive alcohol consumption, active smoking, diabetes mellitus, myopia, uveitis, glaucoma and certain medications (corticosteroids)[5,6]. Thus, the literature has also incriminated cataract as a component of the metabolic syndrome (diabesity including type 2 diabetes mellitus, abdominal/visceral obesity, arterial hypertension and dyslipidemia [7,8].
In the Democratic Republic of Congo (DRC), fragmentary (hospital) [9] and animal model [10] studies report the frequency of traumatic complications linked to the cataract itself and to cataract surgical techniques. Identifying and treating modifiable risk factors could not only reduce the risk of cataract formation but also improve postoperative functional prognosis [2,11].
The general objective of this study was to evaluate the impact of non-diabetic cataract surgery on pro-oxidant, pro-inflammatory-metabolic biomarkers according to the pre- and post-operative phases.
2. Methods:
2.1 Study design and framework
It was a mixed study, consecutive series combining an intervention (quasi-experimental study before and after cataract surgery), a documentary study (patient file), a comparative and evaluative approach between the months of September and December 2022 at the Ophthalmological Center of MASINA.
2.2 Study population: Non -diabetic patients with cataracts, aged over 40, who consulted the Masina Ophthalmological Center (COM) during the study period were our target population. Included in this study: any non-diabetic patient with a clinical and ophthalmological diagnosis of cataract followed and operated on at the COM, having carried out a preoperative and postoperative biological assessment including the dosage of Triglycerides, total cholesterol, HDL-cholesterol , LDL-cholesterol, albumin, and having consented freely, during the period of our study. The following were excluded from the study: all patients operated on for cataract recognized as diabetic; all patients operated on for cataract without biological assessment; all non-consenting cataract patients.
The general formula for calculating the sample size (Ni) considered the following values: Incidence (P= probability, estimated proportion=0.92); Q= 1-P=1-0.08; Z alpha = Standard deviation equal to 1.96 for α (risk of concluding that there is a difference that does not actually exist) =0.05; D= tolerated margin of error=0.04. Thus (Zα= Z²xQ( 1-Q) /D² = 170 participants.
2.3 Data collection: It was done on the basis of an ad hoc data collection sheet. A patient interview was conducted by the principal investigator for 30-40 minutes to collect epidemiological, environmental and health data.
Body weights (kilo) were measured to the nearest 100 grams in lightly dressed and barefoot patients on a Seca scale , previously calibrated each morning, on a flat and stable surface. Height (m) was measured using the height gauge near Cm.
All participants benefited from a complete, detailed ophthalmological examination defined as follows: gross and corrected visual acuity (VA) measured with standard optotypes, on the Monnoyer scale for educated patients and optotypes Snellen E for participants with a low level of education (illiterate); examination of the general anterior segment and the lens in particular, according to the Van Herick method , carried out using the Haagstreit 900 brand biomicroscope ( Switzerland ); the measurement of the intraocular pressure carried out using a Goldmann applanation tonometer and estimated in mmHg; examination of the fundus by the direct method using a Heine beta 200 ophthalmoscope (Germany).
Systolic blood pressure (SBP) and diastolic blood pressure (DBP) measurements were respectively recorded on the arm, along the path of the humeral artery, previously detected using the tip of the index finger. , middle finger, ring finger in patients who had been comfortably installed for 10 minutes in a seated position (mmHg); using the sphygmometer with mercury height.
Regarding the biological profile, the values were repeated before and after surgery. Fasting blood glucose was measured in plasma using the ONE TOUCH glucometer to confirm or refute the absence of diabetes mellitus after fasting blood glucose.
CT, LDL-C, HDL-C, Albumin and triglycerides were assayed by the same Biochemistry laboratory of the University Clinics of Kinshasa, on serum, from whole blood without anticoagulant, taken between 7 a.m. and 10 a.m., at the ulnar vein of the fasting participant. The assays were performed by the semi-automatic clinical chemistry analyzer ( Mindray ).
2.4 Definitions of concepts and operational definitions:
Senility/aging characterized frailty in patients ≥60 years old (senior or elder) versus adulthood = 40-59 years.
This quasi-experimental/interventional study included the following phases of the perioperative period:
The preoperative phase included the evaluation of the patients by the anesthesiologists and the cataract surgeon with the normal values of SBP, DBP, CT, HDLc , TG and blood glucose (Bio markers) on Day 1;
The postoperative phase evaluated the directions of the variations of the biomarkers towards the increase, the stability and the decrease after cataract surgery between D1 and D30 of the metabolic syndrome complex, circulating biomarkers-inflammation-atherogenicity-pro-oxidants.
Hypoalbuminemia was defined by albuminemia < 35 g/L which reflected protein -energy malnutrition, inflammation, immune deficiency.
2.5 Atherogenicity: Non-HDL Cholesterol is the differential between total cholesterol and HDLc , it summarizes the sum of the two potentially atherogenic fractions of cholesterol, namely LDL cholesterol and HDL [12]. In patients considered to be at high cardiovascular risk, this level is between 130 and 159 mg/ dL . The Triglyceride- Glucose index ( TyG Index) makes it possible to determine insulin resistance; it is a more effective biomarker than its separate components for identifying abnormalities in Glucose metabolism [13]. Its normal value is set at 8.5. The total/HDL cholesterol ratio is used to measure cardiovascular risk. Its normal value should be < 5 [13]. HDL/LDL; TG/HDL ratio ≥ 2.5, Triglyceride-Glucose Index and Body Mass Index ( TyG -BMI) is a simple, powerful and clinically useful surrogate marker for early identification of insulin resistance [14,15].
A body mass index (BMI) ≥25 Kg/m² and ≥30 Kg/m² respectively define overweight and obesity.
The Metabolic Syndrome (SM) was defined according to NCEP-ATP III by the presence of at least 3 of the following criteria: PA≥130/85 mmHg, TT>83 Cm, Fasting blood sugar >126 mg/dl, HDL-c <40 mg/ dL , triglyceride >150 mg/ dL [16].
2.6 Statistical analyses: Data were entered using Excel 2016 software, and analyzed using IBM SPSS 26 software.
For the descriptive and comparative approaches before and after cataract surgery, the univariate analyzes considered the nominal variables (qualitative or categorical) in the form of frequencies (n= effective) and proportions (%) while the quantitative variables/ ( saltatory or continuous) were presented as means ± SD, minimum and maximum. Pearson's Chi-Square test and Yates' Chi-Square test were used to compare the proportions between two groups. The trend chi-square function was used to calculate the odds ratio ( odds ratio=OR) and biological exposure gradients (causal association criterion) between ≥3 groups. Student 's t-test was used to compare mean values of normally distributed (symmetric) variables between two groups. Analysis of variances (ANOVA) compared mean values of symmetric variables between ≥ 3 groups. The mean values of the asymmetric variables were compared between two groups according to the nonparametric test of U (the rank sum) while the nonparametric Kruskal test was used to compare the mean values between ≥3 groups.
For the evaluative approaches for the intervention Before-After cataract surgery, the proportions of the phase After cataract surgery (Y = second measurement), were compared to those of the phase Before cataract surgery (X = first measurement) according to the statistical test, non-parametric alternative of MC Nemar.
K= (AB)² /A+B.
For quantitative variables, the bet t-test (t-test) was used to compare the paired sample means of the two variables for a single group (non-diabetic, non-hypertensive cataract patients before-after). Indeed, this procedure calculated the differences between the values of the two variables for each observation and tested whether the mean differs from 0.
2.7 Statistical inference: Statistical inference was interpretative according to the following steps:
The hypothesis formulated was zero (H0 = no difference between two variables); Consider the likelihoods of the observation under the hypothesis H0 for the value of the probability P<0.05 (degree of statistical significance).
2.8 Ethical considerations: This study carried out in patients obtained the approval of the National Ethics Committee of the Democratic Republic of Congo under number N°376/CNES/BN/PMMF/2022 of August 4, 2022 and in compliance with the recommendations of the Declaration of Helsinki III (declaration-Helsinki-1964-2015-08-20).
3. Results:
The variables of interest were presented before and after cataract surgery; the univariate and multivariate analyzes considered the comparisons of the mean values and the proportions of the variables of interest in a quasi-experimental/before-after intervention manner. The extent and determinant of the incidence of Visual Impairments (VI) were presented postoperatively.
3.1. General characteristics of the population
3.1.1. Age
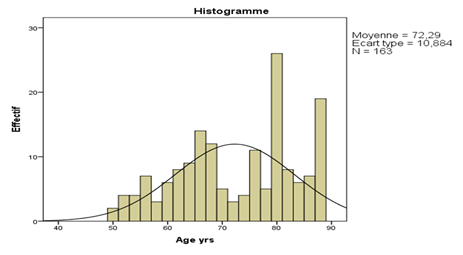
In this study population, the average age was 72 ± 10 years, with extremes ranging from 50 to 88 years (Figure 1).
3.1.2. Sex
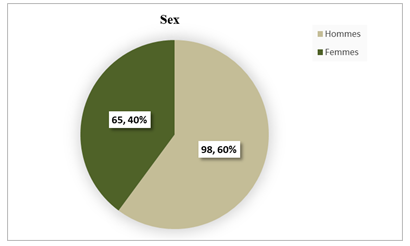
Out of a total of 163 patients, a male predominance was found with 60% (n=98) against 40% (n=65) of women. The sex ratio was close to 2 Male: 1 Female (Figure 2).
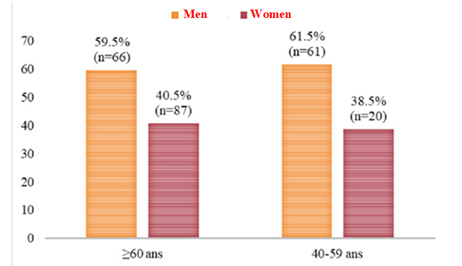
The age distribution of all patients was normal (symmetrical) despite its multimodal appearance. Nearly 81.6% (n=133) of patients were of an advanced age-Senior ≥ 60 years against nearly 18.4% (n=30) of patients whose age was < 60 years adult in the total population (Figure 3).
3.2 Comparative approaches for the values of structural-circulating markers of cardiometabolic risk before and after surgery
Except for TT, cataract surgery very significantly induced a deleterious impact on the rest of the components of the metabolic syndrome/insulin resistance-oxidative stress-atherosclerosis: the increase in mean values of BMI, CT, LDL, TG and glycemia in the postoperative phase being higher than those of the phase before cataract surgery while the average values of PAS, PAD, HDL and Albumin of the postoperative phase were lower than those of the phase before cataract surgery (Table 1).
Table 1: Average values of structural markers before and after surgery
|
Variables of interest |
Mean±SD Before |
Mean ±SD After |
P-value |
|
Anthropometric |
|||
|
· BMI Kg/m2 |
23.7±4.1 |
32.8±5.4 |
<0.0001 |
|
· TT Cm |
109.3±30.5. |
111.7±29.4 |
0.479 |
|
Hemodynamics |
|||
|
· NOT |
181.6±43 |
136.7±14.3 |
<0.0001 |
|
· PAD |
87.6±10.8 |
75.9±5.6 |
<0.0001 |
|
Organic |
|||
|
· CT |
124.9±46.5 |
279.6±88.7 |
<0.0001 |
|
· HDL-C |
49.9±7.3 |
32.2±21.4 |
<0.0001 |
|
· LDL-C |
94.5±34.1 |
191.4±65.9 |
<0.0001 |
|
· XL |
90.7±45.9 |
200.6±73.9 |
<0.0001 |
|
· blood sugar |
92.7±8.1 |
101.8±10.6 |
<0.0001 |
|
· Albumin |
46.6±5.5 |
23.9±15.6 |
<0.0001 |
3.3. Atherogenicity indices
All insulin resistance and atherogenicity biomarkers were very significantly higher in the post cataract surgery phase than during the pre-surgery phase (Table 2).
Table 2: Variation of atherogenicity biomarkers before and after surgery
|
Variable |
Mean ± SD Before |
Mean±SD After |
P-value |
|
TYG |
8.2±0.5 |
9.2±0.4 |
<0.0001 |
|
TC/HDL ratio |
2.6±1.1 |
16.9±28 |
<0.0001 |
|
LDL/HDL ratio |
1.93±0.8 |
11.5±19.8 |
<0.0001 |
|
TG/HDL ratio |
1.8±0.9 |
11.7±25.4 |
<0.0001 |
|
No HDL mg/ dL |
74.9±48.3 |
247.4±102.4 |
<0.0001 |
4. Discussion
This section recalled the object relating to the pejorative impact of surgery on structural-circulating markers before and after cataract surgery.
Contrary to the data of the literature with a neutral influence of the sex in the presence of cataract, the present study carried out in Kinshasa (western of the DRC), a study recently carried out in Lubumbashi (South-East of the DRC) [13], a Nigerian study (West Africa) and one carried out in Greece [13] rather incriminate the male predominance in cataract according to a sex ratio of 2 men: 1 woman. It is difficult to think of a causal association in the absence of a prospective study and confounding factors related to accessibility to care, education and higher care in men than in women in the DRC.
This study looked at non-diabetic cataract patients with an advanced age, similar on average to the average cataract age of 62 years in Mali and the average age of 64 years for cataract patients in Nigeria [17]. But considering age ≥ 60 years, nearly 82% of cataract patients in the present study were far higher than 74% in Mali [18] and 72% in Lubumbashi[13]. It is the currently high life expectancy in Africa explained by the demographic transition and by vaccination, the fluorescent economic development despite the socio-economic and politico-military crises. Overall, the present study confirmed the meaning of SM in patients with cataract [13]: Nearly 95% of patients admitted for cataract surgery had SM specific to Sub-Saharan Africa (TT≥81 Cm) [2]. But if it were necessary to consider the TT≥ 80 Cm, 100% of the patients of the present study would present the SM according to IDF [2]. Indeed, SM is characterized by a constellation of several biomarkers and structural markers that increase the risk of cardiovascular disease, type 2 diabetes mellitus, and stroke [9].
SM-Insulin resistance-atherosclerosis-inflammation-oxidative stress-for cataract set after surgery
In the present study, cataract surgery exaggerated the proportions of Hypo-albuminemia (Inflammation, oxidative stress and protein -energy malnutrition) [19], hypo HDL- cholesterolemia (inflammation-oxidative stress), high levels of CT/ HDLc , LDLc / HDLc , Non HDLc (Atherosclerosis-cardiometabolic risk) and IR-TYG (Biomarkers currently approved as insulin resistance) [13].
By ruling out the confounding variables (Age, TT, PAD, HDLc , LDLc , TG, Glycemia, Albumin, CT/ HDLc , TYG, LDL/ HDLc and non- HDLc ), the rise in BMI (specific structural markers of subcutaneous regional adiposity in the Bantu)[20], here the decrease in SBP ( vaso-constriction reactive to haemorrhage and component of tissue hypoperfusion) and dyslipidemia defined by the increase in total cholesterol (bad cholesterol pro atherosclerosis is incriminated in visual disturbances) remained significantly associated with non-diabetic cataract.
The study by Heydari B et al. [21,22] showed that hypercholesterolemia, hypertriglyceridemia, elevation of LDL-C and blood sugar levels are significantly associated with the presence of cataracts. As these authors pointed out, the results of the present study plead in favor of the development of health promotion activities in our environment, in order to control these modifiable factors within populations at risk.
Indeed, cataracts are associated with elevated serum CT, LDL-C, and TG levels, all of which are components of Metabolic Syndrome (MS). And in the present study, cataract surgery was accompanied by an explosion in the levels of structural markers and circulating biomarkers of SM, oxidative stress, inflammation as well as indices of atherogenicity. In addition, cataract surgery exaggerated oxidative stress with depletion of albumin (antioxidant biomarker) and HDL-C (pro-oxidant biomarker) levels[8]. Several studies have demonstrated the role of oxidative stress in the occurrence and maturation of cataracts, even in experimental models [23,24].
Furthermore, elevated blood glucose levels may be a phenomenon involved in the failure of the antioxidant enzyme system and the progressive peroxidation of lipids [25,26], even after cataract extraction.
On D30, the patients in this study presented a significant increase in the levels of BMI, total cholesterol (TC) and triglycerides (TG). The observation of an explosion of obesity, cholesterol and particularly TG has already been reported in a population of patients after heart transplantation [27,28] with persistence of high levels of TG beyond a follow-up of 3 years. In liver transplant patients, Yi Wu et al. [22,29] in China found that elevated TG levels predicted the onset of type 2 diabetes.
Overall, patients operated on for cataract can be considered to be in a state of pre-diabetes, as shown by the results of the present study, with a very high cardiovascular risk, requiring multidisciplinary follow-up in the immediate and distant postoperative period. .
To date, two hypotheses could be put forward in view of the results of this study:
- first, the effect of functional recovery on the behavior or eating habits (excessive consumption) of patients operated on for cataract;
- the influence of the degree of satisfaction of patients after cataract surgery on their lifestyle (sedentary lifestyle) following good functional recovery.
The present study had a degree of limitations related to the absence of inflammation biomarkers like CRP protein, oxidized LDL (oxidative stress), hyperthyroidism test, urinary examination (nephrotic syndrome, vomiting, Diarrhea, lupus) in front of the hypoalbuminemia. On the other hand, the strengths of the present study reside in the first result of a quasi-experimental approach (intervention before after cataract surgery) according to the calculation of the size of the sample and mathematical models (matched sample and rigorous discriminant analysis). Thus, temporality (time) in a longitudinal manner/monitoring demonstrated the causality of the exaggeration of the SM-Insulin resistance-Atherogenicity-inflammation-oxidative stress complex [20].
5. Conclusion
The present study confirmed that cataract is a structural marker and a pre-hypertension, pre-diabetic, pre-atherosclerotic state in poor Bantu patients.
Gender and age had no impact on the SM-insulin resistance-inflammation-atherosclerosis-oxidative stress components.
Overall, cataract surgery exaggerated SM-insulin resistance-inflammation-atherogenicity-oxidative stress components.
Further longitudinal studies should be conducted to elucidate these findings and explore the variations of these biomarkers beyond D30.
References
- Rizqillah N. The Role of Diabetes Mellitus in Causing Posterior Subcapsular Cataracts in Outpatients (Case From Indonesian Eye Hospital). Int. J Ophthalmol & Eye Sci 10 (2021): 467-471.
- Ang MJ, Afshari NA. Cataract and systemic disease: A review. Clin Exp Ophthalmol 49 (2021): 118-127.
- Lawani R, Pommier S, Roux L, et al. Magnitude and strategies of cataract management in the world. Med Trop (Mars) 67 (2007): 644-650.
- Bouguila H, Chebbi A, Zeghal I, et al. Complications of congenital cataract surgery. French J Ophthalmol 32 (2009):117.
- Nemet AY, Vinker S, Levartovsky S, et al. Is cataract associated with cardiovascular morbidity? Eye (Lond) 24 (2010): 1352-1358.
- Kim SI, Kim SJ. Prevalence and Risk Factors for Cataracts in Persons with Type 2 Diabetes Mellitus. Korean J Ophthalmol 20 (2006): 201-204.
- Longo-Mbenza B, Muaka MM, Mokondjimobe E, et al. Oxidative stress-elevated high gamma glutamyl transferase levels, and aging, intake of tropical food plants, migration and visual disability in Central Africans. Int J Ophthalmol 5 (2012): 493-498.
- Mvitu Muaka M, Longo-Mbenza B, Mona DT, et al. Reduced risk of metabolic syndrome due to regular intake of vegetables rich in antioxidants among African type 2 diabetics. Diabetes & Metabolic Syndrome: Clinical Res & Rev 3 (2010): 132-136.
- Mvitu M, Longo-Mbenza B. Type 2 diabetes mellitus, oxidative stress and visual impairment. Mauritius. European University Editions (2002).
- Diallo JW, Meda N, Ahnoux-Zabsonre A, et al. Résultats fonctionnels de la chirurgie de la cataracte par phacoalternative avec implantation en chambre postérieure: à propos de 300 cas à Bobo Dioulasso (Burkina Faso). Pan Afr Med J 20 (2015): 230.
- Dandona L, Dandona R. Revision of visual impairment definitions in the International Statistical Classification of Diseases. BMC Medicine 4 (2006): 7.
- 17 th SAFO - Société Africaine Francophone d’ophtalmologie. Cataract and Pathologies of the Posterior Segment (2022).
- Makumyaviri S, Lilangalanga J, Makumyaviri J, et al. Evaluation of the results of cataract surgery in adult patients followed at Saint Joseph Hospital in Kinshasa. Revue Médicale des Grands Lacs 11 (2020).
- Lumbu C, Mehl F, Kaimbo D, et al. Cataract in a bonobo from the “Lola ya bonobo” sanctuary Summaries of the 26th SFDP conference. Kinshasa (2013).
- Bernard J-A, Offret G. Anatomy of the lens (2022).
- Lin I-H, Lee C-Y, Chen J-T, et al. Predisposing Factors for Severe Complications after Cataract Surgery: A Nationwide Population-Based Study. J Clin Med 10 (2021): 3336.
- Kolawole OU, Ashaye AO, Mahmoud AO, et al. Cataract Blindness in Osun State, Nigeria: Results of a Survey. Middle East Afr J Ophthalmol 19 (2012): 364-371.
- Descamps O. Nouveautés 2016 en dyslipidémie (2016).
- Hong S, Han K, Park C-Y. The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic cardiovascular disease: a population-based study. BMC Med 18 (2020): 361.
- Zheng S, Shi S, Ren X, et al. Triglyceride glucose-waist circumference, a novel and effective predictor of diabetes in first-degree relatives of type 2 diabetes patients: cross-sectional and prospective cohort study. J Transl Med 14 (2016): 260.
- Jiang C, Yang R, Kuang M, et al. Triglyceride glucose-body mass index in identifying high-risk groups of pre-diabetes. Lipids Health Dis 20 (2021):161.
- Heydari B, Kazemi T, Zarban A, et al. Correlation of cataract with serum lipids, glucose and antioxidant activities: a case-control study. West Indian Med J 61 (2012): 230-234.
- Olawoye O, Ashaye A, Bekibele C, et al. A comparative evaluation of patients satisfaction with cataract surgical services in a public tertiary and a private secondary eye care facilities in Nigeria. Ann Afr Med 11 (2012): 157-162.
- Tarwadi K, Agte V. Linkages of antioxidant, micronutrient, and socioeconomic status with the degree of oxidative stress and lens opacity in indian cataract patients. Nutrition 20 (2004): 261-267.
- Longo-Mbenza B, Longokolo Mashi M, Lelo Tshikwela M, et al. Relationship between Younger Age, Autoimmunity, Cardiometabolic Risk, Oxidative Stress, HAART, and Ischemic Stroke in Africans with HIV/AIDS. ISRN Cardiol 2011 (2011):897908.
- Hashim Z, Zarina S. Antioxidant markers in human senile and diabetic cataractous lenses. J Coll Physicians Surg Pak 16 (2006): 637-640.
- Mbala FK, Mbangi JM, Nkodila AN, et al. Determinants of Regional Obesity (Visceral and Subcutaneous Obesity) within Cardiovascular Risk Factors in the Cardiology Department of the University Clinics of Kinshasa. WJCD 12 (2022): 444-456.
- Yildirim Z, Yildirim F, Ucgun NI, et al. The evaluation of the oxidative stress parameters in nondiabetic and diabetic senile cataract patients. Biol Trace Elem Res 128 (2009): 135-143.
- Wu Y, Jiang W, Yang X, et al. Postoperative serum triglyceride levels in predicting risk of new-onset diabetes mellitus in patients following liver transplantation. Zhejiang Da Xue Xue Bao Yi Xue Ban 50 (2021): 239-244.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
