Effectiveness of Prenatal Perineal Massage in Reducing the Risk of Perineal Trauma during Vaginal Delivery in Nulliparous Women: A Meta-Analysis and Evidence Based Review
Nupur Hajela*, Kari Anne Turner, Jennifer Roos, Monica Rivera
Department of Physical Therapy, California State University, Fresno, California, United States
*Corresponding author: Nupur Hajela, Department of Physical Therapy, California state University, Fresno 5315 Campus Drive M/S PT29 Fresno, CA 93740-8031, USA
Received: 06 October 2021; Accepted: 14 October 2021; Published: 26 October 2021
Article Information
Citation:
Nupur Hajela, Kari Anne Turner, Jennifer Roos, Monica Rivera. Effectiveness of Prenatal Perineal Massage in Reducing the Risk of Perineal Trauma during Vaginal Delivery in Nulliparous Women: A Meta-Analysis and Evidence Based Review. Journal of Women’s Health and Development 4 (2021): 136-150.
DOI: 10.26502/fjwhd.2644-28840068
View / Download Pdf Share at FacebookAbstract
Background: Perineal injury occurs in 85% of all women who experience a vaginal, delivery. Perineal injury involves an episiotomy and/or a laceration. Urinary incontinence (UI) is the most frequently reported morbidity following a perineal injury.
Objectives: To synthesize the existing literature to determine if perineal massage should be performed in pregnant women as preparation for their vaginal delivery to reduce the likelihood and severity of perineal trauma.
Study Design: PubMed, PEDro, International Journal of Gynecology & Obstetrics, were searched. Incidence of episiotomy and degree of perineal laceration were measured following vaginal delivery.
Methods: This meta-analysis included controlled clinical trials studying 2,877 primipara women with an average age of 28 years old. All women had medically uncomplicated pregnancies and full-term vaginal deliveries. Articles were appraised for quality using the PEDro Scale.
Results: Seven controlled trials met the inclusion criteria and were included for analysis. The most important finding of this meta-analysis is that perineal massage reduced the severity of perineal injury during vaginal delivery. Women who practiced perineal massage in their third trimester were 21% less likely to have third and fourth degree perineal lacerations. In addition, dynamic perineal massage reduces the risk of third and fourth degree tears by 16% and episiotomy by 13%. In terms of frequency of perineal massage i.e. daily versus 3-4 times a week, the results suggest that daily perineal massage have a statistically significant effect in reducing the risk of first degree tear by 416%.
Conclusions: Perineal massage reduces the severity of perineal injury. This will allow women to return to their prior level of function at an increased rate and reduce the likelihood of secondary morb
Keywords
<p>Antenatal, Nulliparous, Episiotomy, Urinary Incontinence, Post-Partum</p>
Article Details
1. Introduction
Eighty-five percent of women sustain a perineal injury during a vaginal delivery [1]. The World Health Organization provided a statement regarding recomm-endations for preventing perineal trauma during labor which stated perineal massage improves likelihood of maintaining the integrity of the perineum and reduces the risk of tears [2]. A Cochrane Database of Systematic Reviews published in 2017 by Aasheim, Nilsen, Reinar, and Lukasse reviewed 5 studies comparing massage vs. routine care related to severity [3]. This review had over 2,400 participants which found reduced severity of tears in the group receiving massage [3]. Injury to the perineum leads to a variety of secondary morbidities during the postpartum period. Urinary incontinence (UI) is the most frequently reported long-term morbidity following perineal trauma [4, 5]. Up to 40% of women with post-partum UI, continue to experience UI for the duration of their lifetime [6]. A longitudinal study conducted in 2006 determined that 42% of women continued to experience symptoms of UI 12 years following their vaginal delivery [7]. Handa, Blomquist, McDermott, Friedman, and Munoz published a cohort study in 2012 including more than 400 participants, and found that perineal lacerations were associated with pelvic floor disorders event 5-10 years post-delivery [8]. The most common pelvic floor disorders noted were both urinary and anal incontinence and prolapse.8 Perineal injuries are a concern for health care providers due to their tendency to contribute to long-term secondary morbidities such as UI [9, 10]. Physical Therapists are integral in post-delivery care because 43% of women with UI report limitations in their physical activity [11]. Prolonged limitations occur because women with UI often avoid exercise due to psychological difficulties related to the fear of an involuntary release of urine [11]. Reduction in physical activity over time, not only increases risk factors for general health status but also contributes to ongoing pelvic floor dysfunction.
In 2018 the American College of Obstetricians and Gynecologists (ACOG) Committee provided an update to clinical management guidelines for perineal lacerations occurring during vaginal delivery [12]. The most severe lacerations, 3rd and 4th degree, include involvement of the anal sphincter complex and are referred to as obstetric anal sphincter injuries (OASIS) (Figure 1). Current management of third and fourth degree tears require surgery under anesthesia within the first 12 hours of vaginal delivery tosuture the anal complex and perineum [13]. Second degree tears may also require suturing to assist in proper healing of the perineal muscles and soft tissues [13]. Perineal massage can be performed by an obstetric gynecologist (OB-GYN), midwife, physical therapist, or by self. The purpose of perineal massage is to stretch the vaginal opening and surrounding perineal muscles using external manual pressure [14]. Self-perineal massage involves the use of inserting one or two fingers 3-5 cm into the vagina using a lubricant (almond or calendula oil) and applying a constant sweeping, downward motion or by holding a static, steady pressure along the inferior-lateral regions of the perineum (Figure 2) [15-17]. Parameters for perineal massage vary from 5-10 minutes daily and are frequently monitored by pain level [15-17]. Women are educated to apply enough pressure to feel a mild burning sensation to ensure the perineum is being stressed enough to make physiological changes in the tissue [15-17]. Their hands should be washed to avoid any infections.
Perineal massage has been studied in the past, particularly by midwives, who performed perineal massage on women during active labor. Pre-existing research has demonstrated that perineal massage during labor is effective at reducing perineal trauma [18, 19]. A randomized controlled trial conducted in 2017 with a sample of 195 nulliparous women determined that perineal massage during active labor significantly reduced the frequency of episiotomy and severity of perineal laceration [19]. If perineal massage during active labor can prevent perineal trauma, then preparatory perineal massage during the pre-partum period may have even greater effects. This is based on the notion that soft tissue changes take 4-6 weeks to occur [20]. Beginning perineal massage 4-6 weeks prior to the expected due date should allow time for true soft tissue changes [20]. This may lead to an even greater reduction in perineal trauma when compared to perineal massage performed solely during active labor. Perineal massage during the third trimester of pregnancy has been researched, although results have been inconclusive, and no meta-analysis has been performed to date. The purpose of this meta-analysis is to determine if perineal massage during the third trimester should be performed in pregnant nulliparous women in preparation for vaginal delivery.
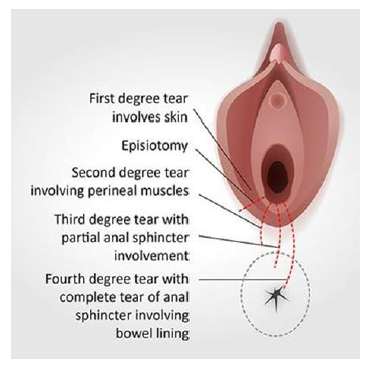
Figure 1: Grades of obstetrical anal sphincter injury (OASIS). Illustrates different level of degree of tear (1st degree, 2nd degree, 3rd/4th degree tear and episiotomy. Adapted from Royal College of Obstetricians & Gynecologists.

Figure 2: Perineal massage technique. Self-perineal massage involves the use of inserting one or two fingers 3-5 cm into the vagina using a lubricant and applying a constant sweeping, downward motion or by holding a static, steady pressure along the inferior-lateral regions of the perineum Adapted from Períneo Information.
2. Methods
2.1 Search strategy and inclusion and exclusion criteria
This meta-analysis was structured in accordance with the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses”, better known as the PRISMA guidelines [20]. Databases searched included PubMed, Physiotherapy Evidence Database Scale (PEDro), OneSearch via Henry Madden Library, and the International Journal of Gynecology & Obstetrics. The literature search commenced in July 2019 and concluded in October 2019. One reviewer performed a preliminary screen of articles based on titles and abstracts from peer-reviewed journals only. Randomized-controlled trials, controlled clinical trials, meta-analyses, and systematic reviews were filters applied to all searches. The search used various combinations of the following words and phrases: perineal massage, antenatal, pregnancy, antepartum, and perinatal. Secondary searches occurred after reviewing references of all included articles to determine if they met search criteria.
To be included in this meta-analysis, all studies needed to be controlled clinical trials. Studies were comprised with one experimental group that involved perineal massage compared to a control group that received routine care during pregnancy. Nulliparous and multiparous women were separated in the included studies. Women of all ages who performed perineal massage for at least 4 weeks during the third trimester of their pregnancy were eligible. All participants were expecting a vaginal delivery over a cesarean section. Premature deliveries defined as prior to 37 weeks of gestation were excluded due to smaller fetus size. Babies that are premature place less stress on the pelvic floor during vaginal delivery and bias results for perineal massage. Women with medically complicated pregnancies that placed them at risk for prolonged labor such as from multiple gestation, preeclampsia, and neurological disorders associated with fatigue were excluded since it would bias results against perineal massage. Participants were also excluded if they were at risk for a cesarean delivery.
2.2 Study selection
Nulliparous, pregnant women of all ages with normal, uncomplicated pregnancies were included in this study. Perineal massage was defined as any hands-on manual technique using external pressure without assistance from instruments. This could be performed as a static hold along the inferior and lateral borders of the vaginal opening or as a dynamic motion across the perineum. Perineal massage was compared to standard routine care during pregnancy. Standard routine care is defined as patient education, simple pelvic floor muscle training exercises involving kegels, and regular OB-GYN visits approximately once a month during the first two trimesters of pregnancy and every two weeks during the last trimester [21-23]. Outcome measures included the rate of occurrence of an episiotomy and the presence of OASIS. There are many factors that affect the decision to perform an episiotomy such as the physician’s experience and clinical decision making skills, the weight of the infant, and the circumference of the baby’s head [13]. Although the occurrence of episio-tomies is trending down since 2006, episiotomies are still commonly performed today and are therefore relevant to use as an outcome measure [13]. The grading scale to determine the presence of OASIS is used universally across obstetrical care providers [24]. Inspection for perineal injury following vaginal delivery is performed with adequate lighting by a trained health care provider. The examiner places one index finger into the anus and the ipsilateral thumb into the vagina and uses a “pin-rolling” technique to assess the thick-ness of the perineum [24]. They then grade the severity of OASIS using a scale broken down into first, second, third, and fourth degree tears.
2.3 Quality of evidence
The quality of the studies used in this meta-analysis were reviewed using the PEDro Scale [25]. The PEDro Scale was created to rate the quality of clinical trials using an 11-point scoring system [25]. Criteria in the PEDro Scale assesses threats to internal and external validity by analyzing potential biases and errors in experimental design. This scale has been an integral factor in the evolution of evidence-based practice in the physical therapy field, allowing physical therapists to choose the highest quality research to incorporate into their clinical practice. A score between 6-10 is considered high-quality literature, 4-5 fair quality, and 3 and less poor quality [26].
2.4 Data processing and statistical analysis
Data was extracted from 7 observational studies. In each study, the data was organized into following categories: episiotomy, 1st degree tear, 2nd degree tear, 3rd/4th degree and no tear. A two group comparison was used for each meta-analysis, comparing the number of subjects in the 1st degree tear category to the number of subjects who had no tears. This comparison was repeated comparing the subjects with episiotomy, 2nd degree and 3rd/4th degree tears to the subjects who had no tears. The statistical method was the Log Odds Ratio, which was converted to the Log Risk Ratio. For all meta-analyses, the inverse variance weighting method and random effects model were implemented [27]. The statistical workbook Meta-Essentials was used to achieve effect sizes (ES), combined effect sizes, confidence intervals at 95th percentile (CI) and creation of the forest plots. Analyses of sample sizes of all groups to calculate the overall relative risk (RR) and relative risk reduction (RRR) of episiotomy, first degree, second degree, and third and fourth degree tears was performed. Outcomes were combined across studies and effect sizes are depicted in forest plots depicted in figure 3(A-D). Two secondary sub-analyses were performed: one sub-analysis was using the risk ratio model comparing the types of massage: static vs dynamic. The second sub-analysis was a comparison between the frequencies of massage, daily massage versus three to four times per week. For both secondary sub-analyses, the weighting method used was the inverse variance with random effects as the subgroup weighting.
3. Results
3.1 Study selection
A total of 7 studies were included to be a part of this meta-analysis. The database search produced a total of 125 results. Eighteen results were immediately discarded due to duplicates across databases. The titles and abstracts of the 107 results were examined and 75 articles were excluded as they did not match the appropriate search criteria. The remaining 32 articles were analyzed further and eventually rejected due to lack of meeting the appropriate inclusion/exclusion measures of the PICO i.e. population, intervention, comparison, outcome. The residual 7 studies were chosen for data comparison. The PEDro scale further analyzed the remaining articles to distinguish the level of quality. The PRISMA diagram was created to explain the study selection process in greater detail (Figure 4).
3.2 Summary of results
The most important finding of this meta-analysis is that perineal massage reduced the severity of perineal injury during vaginal delivery. All 7 studies analyzed the risk of acquiring an episiotomy after performing perineal massage for at least 4 weeks. The relative risk reduction (RRR) was the primary data used to determine the effectiveness of reducing the risk of an OASIS after using perineal massage.
3.3 Effects of perineal massage on episiotomy and degree of tear
The results show that there was a statistically significant reduction in risk in 3rd and 4th degree tears by instituting perineal massage (RR 0.79, 95% CI 0.62, 0.99), z = -2.63, p=.008. Therefore, women who practiced perineal massage were 21% less likely to have third and fourth degree perineal lacerations. This is a noteworthy finding because medical management of third and fourth degree lacerations involves emergency surgery under anesthesia to repair the perineum [28]. The risk reduction was 10% in episiotomy (RR 0.90, 95% CI 0.79, 1.02), z = -2.15, p = 0.032 but did reach statistical significance. Finally, there was only 8% reduction in risk of first degree (RR 0.92, 95% CI 0.78, 1.08), z = -1.24, p = 0.215 and second degree perineal tears (RR 0.92, 95% CI 0.76, 1.11), z = -1.14, p = 0.256 respectively compared to third and fourth degree tears following perineal massage (Table 1). It is important to realize that first and second degree tears are more ideal outcomes when compared to third and fourth degree tears. If less women are experiencing third and fourth degree tears, then more women are likely experiencing first and second degree tears thereby reducing sedentary lifestyle and secondary morbidities.
3.4 Sub analysis – dosage of perineal massage
The results from the sub-analysis indicate that there was no statistical difference between the studies performing dynamic compared to the static type of massage in each of the subcategories of tears or the episiotomy. There was however, significant results in the subcategory of the dynamic massage in the 3/4th tear, showing that the probability of the event with dynamic massage is 0.84 with a 95% CI (0.75, 0.93). Also, there are significant effects of dynamic massage on episiotomy, showing that the probability of an episiotomy with dynamic massage is 0.87 with a 95% CI (0.77, 0.98). For the sub-analysis comparing frequency of perineal massage i.e. daily versus 3-4 times a week, the results suggest that daily perineal massage have a statistically significant effect in reducing the risk of first degree tear (RR 0.84, 95% CI 0.71, 0.98).
3.5 Study characteristics
The studies included in this meta-analysis were conducted by the following authors Labrecque et al. [29], Labrecque et al. [30], Shimada et al. [31], Shipman et al. [32], Ugwu et al. [15], Bodner et al. [33], and Mei-dan et al. [16]. The risk of bias within each study was assessed using the PEDro Scale scores. The PEDro scores of the seven studies ranged from 5-9/10 with an average Pedro score of 7/10. All trials included a comparison group that did not receive the intervention being studied as well as point measures for at least three outcomes. The PEDro scale results for each study is listed in Table 1.
All studies were conducted between the years 1994-2018. They were organized by a medical doctor (MD), nurse, midwife, or OB-GYN. Sample sizes ranged from 46-1034 participants with an average sample size of 413 participants and a total sample size of 2,877 women included in this meta-analysis. Table 3 displays the study details and patient characteristics in greater depth. Participant groups from each of the studies used in this meta-analysis included the following characteristics: nulliparous, practiced perineal massage for at least four weeks prior to their planned due date. It is important to note that the parameters and techniques of perineal massage varied amongst the seven included studies. Four of the articles including Labrecque et al. [29], Labrecque et al. [30], Shipman et al. [32], and Ugwu et al. [15] performed perineal massage using a dynamic, continuous sweeping motion along the perineum. Two of the articles including Bodner et al. [33] and Mei-dan et al. [16] performed perineal massage using a static, constant pressure to stretch the perineum and enlarge the vaginal opening. Shimada et al. did not specify the technique used while performing perineal massage [31]. Labrecque et al. [29], Labrecque et al. [30], Ugwu et al. [15], and Mei-dan et al. [16] required perineal massage to be performed daily while Shimada et al. [31], Shipman et al. [32], and Bodner et al. [33] required it to be performed 3-4 times per week. The time perineal massage was performed varied from 4-10 minutes across all studies.
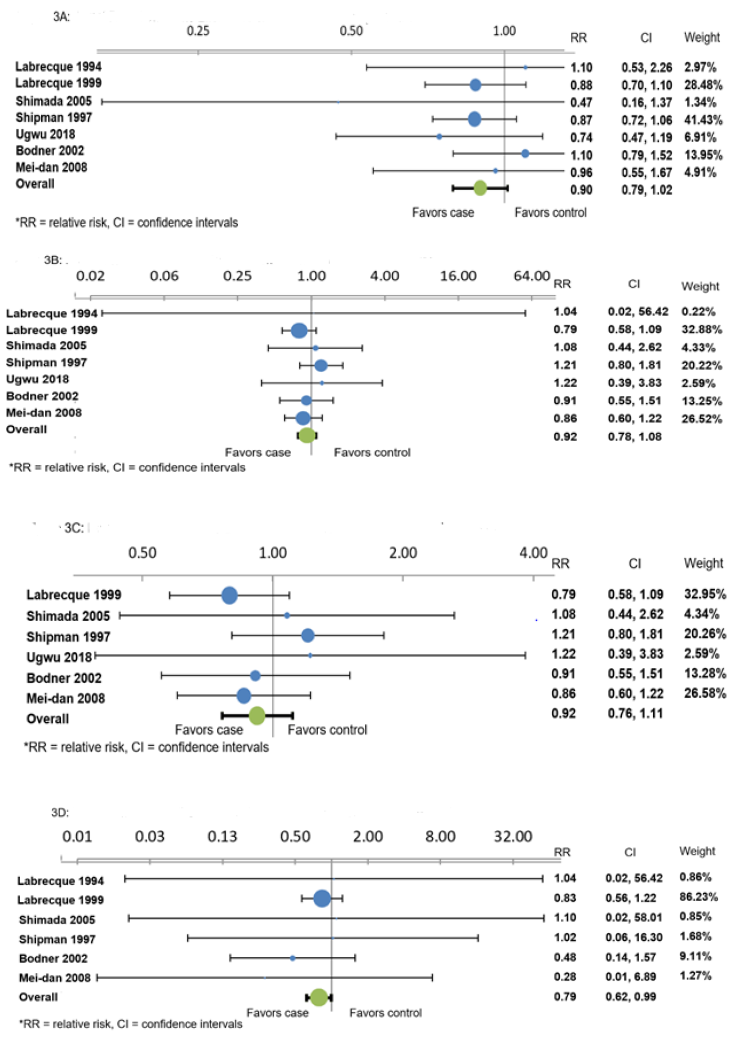
Figure 3A-D: Forest plot showing the effects of perineal massage on Figure on 3A) episiotomy 3B) First degree tears 3C) Second degree tears 3D) Third and Fourth degree tear. RR stands for relative risk.
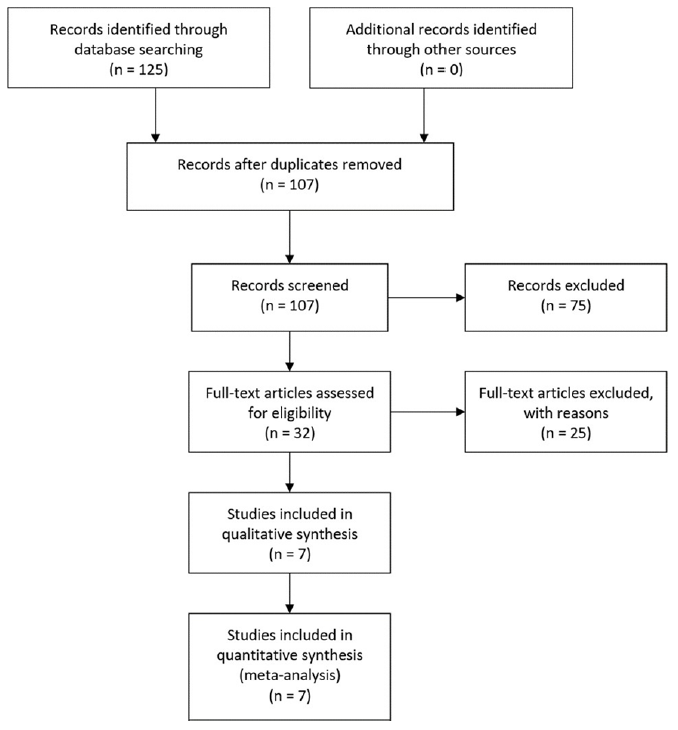
Figure 4: PRISMA (Preferred Reporting Items of Systematic Reviews and Meta analyses) diagram outlining article selection. The PRISMA flow diagram for the systematic review detailing the database searches, the number of abstracts screened and the full texts retrieved. Finally, 7 studies were included for the meta- analysis.
|
Outcome Measure |
RR with 95% CI |
RRR |
z score |
p value |
|
Episiotomy |
0.90 (0.79,1.02) |
10% |
-2.15 |
0.032 |
|
1st Degree Tear |
0.92 (0.78,1.08) |
8% |
-1.24 |
0.215 |
|
2nd Degree Tear |
0.92 (0.76,1.11) |
8% |
-1.14 |
0.256 |
|
3rd & 4th Degree Tear |
0.79 (0.62,0.99) |
21% |
-2.63 |
0.008 |
Table 1: Results: Effects of perineal massage on episiotomy and different levels of degree of tear. Relative risk (RR), and confidence intervals (CI), relative risk reduction (RRR).
|
PEDro Criteria |
Labrecque 1994 |
Labrecque 1999 |
Shimada 2005 |
Shipman 1997 |
Ugwu 2018 |
Bodner 2002 |
Mei- dan 2008 |
|
Random Allocation |
X |
X |
X |
X |
X |
- |
- |
|
Allocation Concealed |
X |
X |
X |
X |
X |
- |
X |
|
Baseline Comparability |
- |
X |
X |
- |
X |
X |
X |
|
Blind Subjects |
- |
- |
X |
- |
- |
- |
- |
|
Blind Therapists |
- |
- |
X |
- |
- |
- |
- |
|
Blind Assessors |
- |
X |
- |
X |
X |
- |
X |
|
Adequate follow-up |
X |
X |
X |
- |
X |
X |
- |
|
Intention to treat analysis |
- |
X |
X |
X |
- |
X |
X |
|
Between group comparisons |
X |
X |
X |
X |
X |
X |
X |
|
Point Estimates and variability |
X |
X |
X |
X |
X |
X |
X |
|
Total Score |
5 |
8 |
9 |
6 |
7 |
5 |
6 |
Table 2: Physiotherapy Evidence Database Scale (PEDro) Scale of Eligible Studies.
|
Study |
Origin |
Subject (n) |
Average Age (yrs.) |
Inclusion |
Perineal Massage Type |
Perineal Massage Frequency |
Perineal Massage Duration (min) |
|
Labrecque 1994 |
Canada |
46 |
not specified |
32- to 34-week- preg-nant nulliparas |
Dynamic |
Daily for 6 weeks |
5-10 |
|
Labrecque 1999 |
Canada |
1034 |
28 |
Women without a previ-ous vaginal birth during the third trimester |
Dynamic |
Daily for 5-6 weeks |
10 |
|
Shimada 2005 |
Japan |
63 |
not specified |
Women without previ-ous vaginal birth bet-ween 34 to 36 weeks |
not specified |
4x week for 4 weeks |
5 |
|
Shipman 1997 |
England |
861 |
28 |
Nulliparous women |
Dynamic |
3-4x week for 6 weeks |
4 |
|
Ugwu 2018 |
Nigeria |
108 |
28 |
All primigravidae with uncomplicated singleton pregnancies in cephalic presentations, at 34–36 weeks gestation, with-out uterine contractions |
Dynamic |
Daily for 4-6 weeks |
10 |
|
Bodner 2002 |
Australia |
531 |
28 |
Primiparous women who were expecting a normal vaginal birth of a singleton baby with cephalic presentation |
Static |
3-4x week for 6 weeks |
5-10 |
|
Mei-dan 2008 |
Israel |
234 |
26 |
Nulliparous women at 30–34 weeks gestation planning a vaginal delivery |
Static |
Daily for 6 weeks |
10 |
Table 3: Study details and patient characteristics.
4. Discussion
The purpose of this meta-analysis was to determine the effectiveness of perineal massage on reducing the likelihood of perineal trauma during vaginal delivery in pregnant women during third trimester. Although a meta-analysis exists on the use of perineal massage during active labor, a meta-analysis examining the use of regular perineal massage during the third trimester of pregnancy does not exist [4]. A systematic review on digital perineal massage during the third trimester was conducted by Beckmann et al. in 2013, which found a statistically significant reduction in the incident of episiotomies in women who practice perineal massage [34]. However, Beckmann et al. did not distinguish parameters of perineal massage to ensure proper technique [34]. In 2018, Ugwu et al. published a randomized control trial on perineal massage during the third trimester that found a reduction of episiotomies to be statistically significant [15]. The findings from this study determined that perineal massage is effective at reducing the risk of trauma during vaginal delivery, especially reducing the risk of third and fourth degree tear. For these reasons, the null hypothesis was rejected which stated that there would be no change in risk of perineal trauma when performing prenatal perineal massage. Based on the subgroup analysis, dynamic perineal massage seems to provide better outcomes in reducing the risk of third and fourth degree tear. Further, while comparing frequency of perineal massage i.e. daily versus 3-4 times a week, the results suggest that daily perineal massage have a statistically significant effect in reducing the risk of first degree tear. Although these sub-analysis findings indicate statistically significant results for particular type of tear, these findings should be taken with caution as it is a sub analysis. No group differences were seen between type of massage (static vs dynamic) in the reduction of tears. So the type of perineal massage and frequency of application of perineal massage doesn’t seem to be as critical, however there appears to be a consistent reduction of tears with a significant reduction in 3rd/ 4th degree. Evidence is inconclusive on the dosage of perineal massage and therefore it is important to draw attention towards the need for appropriate dosage. The standardize dosage would encourage regular use of perineal massage and establish efficacy of this technique in clinics, thereby providing evidence based practice in this less researched yet significant area. It’s important to realize that perineal massage is like stretching any other muscle and doing it more frequently will lead to better outcomes [35]. Even if it doesn’t necessarily have direct effect on reducing the risk of a particular type of tear, it may have a global effect on reduction in perineal pain in three months [36].
4.1 Threats to internal validity
Random allocation of selected participants into groups was present in all studies with the exception of Bodner et al. [33] and Mei-dan et al. [16]. Mei-dan et al.16 allowed participants to choose the massage group or control group, while Bodner et al. [33] did not mention randomization of groups or concealment of allocation. This is a threat to internal validity since selection bias may have been present when sorting participants into groups. Blinding of assessors who determined perineal outcomes was present in four out of seven studies. Assessors were not blinded in Labrecque et al. [29], Shimada et al. [31], or Bodner et al. [33], however, all assessors used the OASIS standardized grading scale to determine the degree of laceration [24]. Recipients of perineal massage were blinded in one study, Shimada et al. [31]. Since the participants did not know what the researchers were measuring, the recipients of massage were considered blinded in this one study. All other participants across studies were not considered blinded to the treatment since they knew the purpose for perineal massage. Women in all the studies performed perineal massage at home unsupervised. Although most researchers called participants weekly to assess compliance throughout the course of treatment this is a threat to validity. Researchers were relying on the participant’s honesty to determine compliance and correctness of massage technique within the assigned parameters. Threats to External & Construct Validity
Although multiparous women were considered in this meta-analysis, existing literature predominantly studied nulliparous women. The eligible studies which matched the PICO included women who were experiencing their first expected vaginal delivery. This is a threat to external validity since the results of the study are not representative of all women. Women experiencing their second, third, fourth, etc. vaginal delivery were not represented in this meta-analysis. Previous research has determined that nulliparous women are at a higher risk for perineal injury, particularly third and fourth degree tears [37]. If perineal massage works for nulliparous women, the population most at risk, it will likely work for multiparous women, as well [37].
Furthermore, it is important to note that all women involved in this meta-analysis were recruited at medical facilities. This may have affected participant compliance with perineal massage and is a threat to external validity because the results do not represent all women, such as women who did not attend these medical facilities. Also, none of the studies included in this meta-analysis were conducted in the United States and is predominantly representative of Canadian and European women. Shipman et al. (n=861) provided pelvic floor muscle training exercises including kegels to both the intervention and control groups within his study [32]. The study was included in this meta-analysis due to both groups performing the same exercises at baseline. Also, it has been reported that 69% of women perform some type of pelvic floor muscle training exercises including kegels throughout their pregnancy [38]. The seven studies’ (n =2,016) control groups included standard routine care that involved regular OB-GYN visits throughout the duration of pregnancy with no educational instruction on perineal massage.
4.2 Limitations
Lack of utilization of a standardized grading scale to measure the amount of pressure applied during perineal massage is a limitation to this study. Across studies, women were given subjective forms of measuring manual pressure during massage. Two of the studies, Mei-dan et al. [16] and Ugwu et al. [15] instructed women to apply pressure until the area felt “numb”, then move to new location and repeat the same process. Shipman et al. instructed women to apply enough pressure to feel “tingling” but no pain [32]. The four remaining studies made no mention of using a standardized way to measure pressure. Another potential limitation to this study was lack of supervision during perineal massage application. Women performed perineal massage at home by self or by partner. Although each study either called the women weekly or recommended they fill out a diary to encourage compliance, the researchers were relying on the participant’s subjective determination to report if massage was being performed correctly. Given that it was a subjective reporting by the women recruited in the study, the results should be accepted with caution.
4.3 Clinical implications
This meta-analysis reinforces the literature on the effectiveness of prenatal perineal massage at reducing the severity of perineal injury following vaginal delivery. Women who have normal, uncomplicated pregnancies should be informed on the benefits of beginning perineal massage during their third trimester of pregnancy. The American Academy of Family Physicians has deemed perineal massage to be a safe and well-accepted form of conservative treatment to reduce perineal trauma [39]. Specialized pelvic health physical therapists are trained in performing perineal massage and interventions that treat incontinence as well as other pelvic health dysfunctions. Although general physical therapists may not perform perineal massage, they are qualified to provide patient education regarding the literature on perineal massage and provide a referral to a pelvic health physical therapist. Specialty trained physical therapists can incorporate perineal massage for appropriate patients receiving therapy for other musculoskeletal dysfunction during pregnancy. Collaboration among healthcare providers treating women during pregnancy can aid to build relationships to provide comprehensive treatment plans including perineal massage.
4.4 Future research
Although research demonstrates that perineal massage is effective at reducing the risk of perineal injury, more information is needed on how perineal massage should be performed. Specific guidelines should determine the appropriate amount of pressure to be applied to the perineum to induce soft tissue changes. This could be measured in a standardized way by using the Numeric Pain Rating Scale (NPRS) [40]. Future research should consider two intervention groups: dynamic massage and static massage. The NPRS should be used to monitor pain level in both groups to standardize the amount of pressure being applied during massage. In addition, future studies should be performed in the United States on this topic.
5. Conclusion
The literature presented in this meta-analysis demonstrated that prenatal perineal massage during the third trimester of pregnancy in primipara women is an effective conservative treatment to reduce the severity of perineal lacerations during vaginal delivery. These results were found to be statistically significant especially for third and fourth degree tears. Therefore, healthy, nulliparous women should be informed on the likely benefits of prenatal perineal massage by their health care providers and referred to a pelvic health physical therapist for appropriate instruction and education. Research should continue to be conducted on this topic to better understand and standardize the way perineal massage should be administered to induce the most positive and optimal outcomes in postpartum women.
References
- Shahoei R, Zaheri F, Nasab LH, et al. The effect of perineal massage during the second stage of birth on nulliparous women perineal: A randomization clinical trial. Electronic physician 9 (2017): 5588-5595.
- WHO recommendation on techniques for preventing perineal trauma during labour. The Reproductive Health Library (2018).
- Aasheim V NA, Reinar LM, Lukasse M. Perineal techniques during the second stage of labour for reducing perineal trauma. . Cochrane Database of Systematic Reviews 2017 (2017).
- Aquino CI, Guida M, Saccone G, et al. Perineal massage during labor: a systematic review and meta-analysis of randomized controlled trials. The Journal of Maternal-Fetal & Neonatal Medicine 33 (2020): 1051-1063.
- Bulchandani S, Watts E, Sucharitha A, et al. Manual perineal support at the time of childbirth: a systematic review and meta-analysis. BJOG 122 (2015): 1157-1165.
- Thom DH, Rortveit G. Prevalence of postpartum urinary incontinence: a systematic review. Acta Obstet Gynecol Scand 89 (2010): 1511-1522.
- Viktrup L, Rortveit G, Lose G. Risk of Stress Urinary Incontinence Twelve Years After the First Pregnancy and Delivery. Obstet Gynecol 108 (2006): 248-254.
- Handa VL, Blomquist JL, McDermott KC, et al. Pelvic floor disorders after vaginal birth: effect of episiotomy, perineal laceration, and operative birth. Obstet Gynecol 119 (2012): 233-239.
- Contributors P. Pelvic Floor Anatomy. Physiopedia (2020).
- Contributors P. Pelvic Floor Muscle Function and Strength. Physiopedia (2019).
- Raizada V, Mittal RK. Pelvic floor anatomy and applied physiology. Gastroenterol Clin North Am 37 (2008): 493-vii.
- ACOG Practice Bulletin No. 198. Prevention and Management of Obstetric Lacerations at Vaginal Delivery. Obstet Gynecol 132 (2018): e87-e102.
- Kilgore R. To episiotomy or not to episiotomy?. Herman & Wallace (2015).
- Shaikh F. Perineal Massage for Childbirth. Herman & Wallace. Herman & Wallace Blog Web site (2018).
- Ugwu EO, Iferikigwe ES, Obi SN, et al. Effectiveness of antenatal perineal massage in reducing perineal trauma and post-partum morbidities: A randomized controlled trial. J Obstet Gynaecol Res 44 (2018): 1252-1258.
- Mei-Dan E, Walfisch A, Raz I, et al. Perineal massage during pregnancy: A prospective controlled trial. Isr Med Assoc J 10 (2008): 499-502.
- Dieb AS, Shoab AY, Nabil H, et al. Perineal massage and training reduce perineal trauma in pregnant women older than 35 years: a randomized controlled trial. International Urogynecology Journal (2019).
- Demirel G, Golbasi Z. Effect of perineal massage on the rate of episiotomy and perineal tearing. International Journal of Gynecology & Obstetrics 131 (2015): 183-186.
- Shahoei R, Zaheri F, Nasab L, et al. The effect of perineal massage during the second stage of birth on nulliparous women perineal: A randomization clinical trial. Electronic Physician 9 (2017): 5588-5595.
- Contributers P. Soft Tissue Healing Physiopedia (2019).
- Staff MC. Prenatal care: 1st trimester visits. Mayo Clinic (2018).
- Staff MC. Prenatal care: 2nd trimester visits. Mayo Clinic (2018).
- Staff MC. Prenatal care: 3rd trimester visits. Mayo Clinic (2018).
- Harvey M-A, Pierce M, Walter J-E, et al. Obstetrical Anal Sphincter Injuries (OASIS): Prevention, Recognition, and Repair. Journal of Obstetrics and Gynaecology Canada 37 (2015): 1131-1148.
- PEDro Scale. Physiotherapy Evidence Database (2019).
- PEDro Score. The Strokengine Team (2019).
- Israel H, Richter RR. A Guide to Understanding Meta-analysis. J Orthop Sports Phys Ther 41 (2011): 496-504.
- Aigmueller T, Bader W, Beilecke K, et al. Management of 3rd and 4th Degree Perineal Tears after Vaginal Birth. German Guideline of the German Society of Gynecology and Obstetrics (AWMF Registry No. 015/079, October 2014). Geburtshilfe Frauenheilkd 75 (2015): 137-144.
- Labrecque M, Marcoux S, Pinault J-J, et al. Prevention of Perineal Trauma by Perineal Massage During Pregnancy: A Pilot Study. Birth 21 (1994): 20-25.
- Labrecque M, Eason E, Marcoux S, et al. Randomized controlled trial of prevention of perineal trauma by perineal massage during pregnancy. Am J Obstet Gynecol 180 (1999): 593-600.
- Shimada M. A Randomized Controlled Trial on Evaluating Effectiveness of Perineal Massage during Pregnancy in Primiparous Women. Journal of Japan Academy of Nursing Science 25 (2005): 22-29.
- Shipman MK, Boniface DR, Tefft ME, et al. Antenatal perineal massage and subsequent perineal outcomes: a randomised controlled trial. Br J Obstet Gynaecol. 1997;104(7):787-791.
- Bodner-Adler B, Bodner K, Mayerhofer K. Perineal massage during pregnancy in primiparous women. International Journal of Gynecology & Obstetrics 78 (2002): 51-53.
- Beckmann MM, Stock OM. Antenatal perineal massage for reducing perineal trauma. Cochrane Database Syst Rev (2013).
- Ellington JE RB, Criso S. Antenatal Perineal Massage Improves Women’s Experience of Childbirth and Postpartum Recovery: A Review to Facilitate Provider and Patient Education on the Technique. J Womens Health (2017).
- Labrecque M, Eason E, Marcoux S. Women's views on the practice of prenatal perineal massage. BJOG 108 (2001): 499-504.
- Landy HJ, Laughon SK, Bailit JL, et al. Characteristics associated with severe perineal and cervical lacerations during vaginal Obstet Gynecol 117 (2011): 627-635.
- Bø K AH, Haakstad L, Voldner N. Do pregnant women exercise their pelvic floor muscles?. International Urogynecology Journal 18 (2007):733-736.
- Seehusen DA, Raleigh M. Antenatal perineal massage to prevent birth trauma. Am Fam Physician 89 (2014): 335-336.
- Kahl C, Cleland JA. Visual analogue scale, numeric pain rating scale and the McGill pain Questionnaire: an overview of psychometric properties. Phys Ther Rev 10 (2005): 123-128.


 Impact Factor: * 3.4
Impact Factor: * 3.4 Acceptance Rate: 78.89%
Acceptance Rate: 78.89%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 