Glaucoma Screened at the Ophthalmology Clinic of PZaGa Hospital Androva Mahajanga, Madagascar.
Rasoanirina Onja Tiana Valisoa1, Andriambelo Ravaka Hariniaina2, Miray Louis de Gonzague3*, Randrianarivelo Tahiriniaina4, Andriamahenina Ando Mathieu5, Randrianirina Jean Baptiste de La Salle6, Raobela Léa7
1Ophthalmology department, university hospital PZaGa Androva Mahajanga, Madagascar
2Ophthalmology department, university hospital Anosiala, Antananarivo, Madagascar
3Ophthalmology department, university hospital Tambohobe Fianarantsoa, Madagascar
4General practitioner, Mahajanga, Madagascar
5Ophthalmology department, university hospital PZaGa Androva Mahajanga, Madagascar
6Orthopaedic Surgery and Traumatology department PZa-Ga Androva Mahajanga, Madagascar
7Ophthalmology department, university hospital Joseph Ravoahangy Andrianavalona Antananarivo, Madagascar
*Corresponding author: Miray Louis de Gonzague, ophtalmologist at university hospital Tambohobe Fianarantsoa, Madagascar.
Received: 16 February 2024; Accepted: 05 March 2024; Published: 02 April 2024;
Article Information
Citation: Rasoanirina Onja Tiana Valisoa, Andriambelo Ravaka Hariniaina, Miray Louis de Gonzague, Randrianarivelo Tahiriniaina, Andriamahenina Ando Mathieu, Randrianirina Jean Baptiste de La Salle, Raobela Léa. Glaucoma Screened at the Ophthalmology Clinic of PZaGa Hospital Androva Mahajanga, Madagascar. Journal of Ophthalmology and Research. 7 (2024): 28-32.
DOI: 10.26502/fjor.2644-00240092
View / Download Pdf Share at FacebookAbstract
Introduction: Glaucoma is an anterior optic neuropathy, usually bilateral but often asymmetric characterised by the association of pathological excavation of the optic disc, visual field alteration, an open or closed iridocorneal angle and often ocular hypertony.
Materials and Methods: This was a prospective, cross-sectional, descriptive study over a period of 8 months from October 2017 to May 2018 carried out in the Ophthalmology Clinic of university hospital Professeur ZAFISAONA Gabriel Mahajanga. The purposes of this study were to determine the prevalence, identify the risk factors and describe the epidemio-clinical aspects of glaucoma.
Results: Among the 3660 patients examined during the study period, 31 cases of glaucoma were diagnosed, representing a frequency of 0.84%. Male predominance was observed with a sex ratio of 2.10. The mean age was 65.07 +/- 0.12 years. Among the general risk factors for glaucoma recorded, hypertension ranked first with 38.70% of cases, followed by diabetes with 12.90% of cases. Local risk factors were previous eye surgery (10.82%), followed by eye trauma (6.45%). The visual field was agonic in 24.19% of cases and seven cases of total blindness were found (11.66%).
Conclusion: Glaucoma was discovered late. All patients with a family history of glaucoma and aged 40 or over should be screened systematically during ophthalmological consultations.
Keywords
<p>Blindness, Glaucoma, Neuropathy, Prevalence, Screening.</p>
Article Details
1. Introuduction
Glaucoma is an anterior optic neuropathy, usually bilateral but often asymmetric, characterised by the combination of pathological excavation of the optic disc, alteration of the visual field, an open or closed iridocorneal angle and often ocular hypertony [1]. Glaucoma is the leading cause of irreversible blindness in the world; it affects adults between the ages of 35 and 70 and occurs earlier in myopics and melanoderma patients. It is a major and serious public health problem. Its seriousness resides in its frequency and in the fact that it is not well known. At the end of the second millennium, the number of glaucoma sufferers was estimated at 66 million (7 million among Africans), including 7 million blind people [2].
The prevalence of glaucoma in France is 2%, according to results published by the French glaucoma committee [3]. In South Africa, among the Zulu people, the prevalence of glaucoma is around 5.6% [4]. In Madagascar, there are no national prevalence figures, as the descriptive and analytical epidemiology of glaucoma has not been perfectly defined, which justifies a study of glaucoma.The purposes of this study were to determine the prevalence, risk factors, epidemiological and clinical aspects of glaucoma at the Ophthalmology Clinic of the university teaching hospital Professeur Zafisaona Gabriel Mahajanga.
2. Methods
This was a prospective, cross-sectional, descriptive study over 8 months period from October 2017 to May 2018 performed in the Ophthalmology Clinic of the university hospital ZAFISAONA Gabriel Mahajanga. We included in the study all patients aged 40 and over with glaucoma who consulted during the study period and consented to participate in the survey. All patients who did not consent to the survey or who suffered from another ocular pathology were excluded from the study. Data were collected from the patient survey, using the "survey form" consisting of questionnaires as a collection tool. We evaluated the epidemiological and clinical data. We studied sociodemographic variables such as age, gender, place of residence and patients' level of education. The clinical variables studied were personal and family history, ocular history, and clinical examination data. Word processing and tables were created using Microsoft Office 2013. Data entry and analysis were carried out using SPSS® 20 software, which has a significant p-value of less than 0.05. The investigator obtained informed consent from the patients before taking any action. The survey was conducted in a place out of sight and earshot in order to respect confidentiality. Survey forms were coded to ensure that participants remained anonymous. The questionnaires were not used for any other purpose.
Table 1: Distribution of patients according to the level of education
|
Level of education |
N |
% |
|
Illiterate |
7 |
22,58 |
|
Primary |
12 |
38,70 |
|
Secondary |
9 |
29,03 |
|
Higher level |
3 |
9,67 |
|
TOTAL |
31 |
100 |
Table 2: Risk factors of glaucoma
|
Risk factors |
N |
% |
|
Hypertension |
12 |
38,70 |
|
Diabetes |
4 |
12,90 |
|
Cataract |
1 |
3,22 |
|
Ocular surgery |
4 |
10,82 |
|
Ocular traumatism |
2 |
6,45 |
3. Results
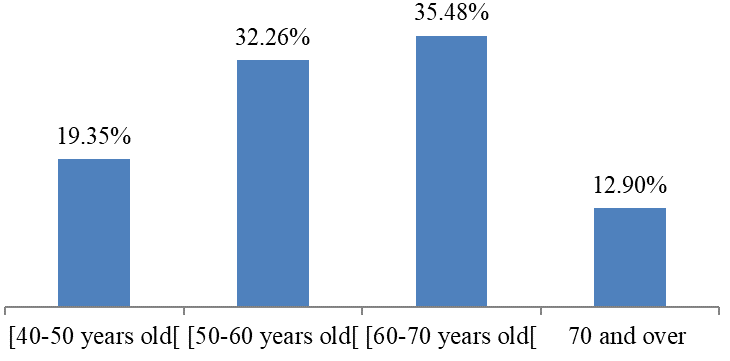
Among the 3660 patients examined during the study period, 31 cases of glaucoma were diagnosed, representing a frequency of 0.84%. There was a predominance of males (67.74%) and females (32.25%) with a sex ratio of 2.10. Our patients ranged in age from 40 to 80 years, with over 80% aged between 50 and 80 years. The mean age was 65.07 +/- 0.12 years (Figure 1). In our series, 22.58% of patients could neither read nor write, 38.70% had primary education, 29.03% secondary education and 9.67% higher education. Half (68.20%) of the patients with glaucoma came from rural areas.
Among the general risk factors for glaucoma recorded, hypertension ranked first with 38.70% of cases, followed by diabetes with 12.90% of cases. As for local risk factors, previous ocular surgery was the most common with 10.82% of cases, followed by ocular trauma with 6.45% of cases (Table 2). Only 4 patients thet means 12.90% of cases, had had 2 or more consultations at the Ophthalmology Clinic. We found 7 cases of total blindness, or 11.66% (Table 3).
The rest of the results will be presented taking into account the eyes affected and not the cases. Thus, Table 4 covers only 39 eyes with glaucoma. The 17.94% of initial IOPs were in the range 30 to 39 mmHg and 5.12% of our patients had IOPs greater than 50 mmHg. We found an excavation of 0.9 in 12 eyes that means 38.7% (Table 5). The visual fieldof 15 eyes (24.19%) were agonic (Table 6).
Table 3: Distribution of patients according to visual acuity
|
Visual acuity |
N |
% |
|
Light perception negative |
7 |
11,66 |
|
Light perception positive |
6 |
10 |
|
20/4000 |
8 |
13,33 |
|
20/2000 |
13 |
21,66 |
|
20/200 |
0 |
0 |
|
20/100 |
0 |
0 |
|
20/63 |
10 |
16,66 |
|
20/50 |
4 |
6,66 |
|
20/40 |
0 |
0 |
|
20/32 |
1 |
1,66 |
|
20/25 |
4 |
6,66 |
|
20/20 |
5 |
8,33 |
|
TOTAL |
60 |
100 |
Table 4: Distribution of affected eyes according to initial intraocular pressure ranges.
|
Intervals of intraocular pressure |
Number of affected eyes |
|
|
N |
% |
|
|
21 à 29 mmHg |
29 |
74,35 |
|
30 à 39 mmHg |
7 |
17,94 |
|
40 à 49 mmHg |
1 |
2,56 |
|
50mmHg and over |
2 |
5,12 |
|
TOTAL |
39 |
100 |
Table 5: Distribution of patients according to fundus examination
|
Excavation |
N |
% |
|
0,3 |
0 |
0 |
|
0,4 |
0 |
0 |
|
0,5 |
2 |
6,45 |
|
0,6 |
8 |
25,80 |
|
0,7 |
5 |
16,12 |
|
0,8 |
4 |
12,90 |
|
0,9 |
12 |
38,70 |
|
TOTAL |
31 |
100 |
Table 6: Distribution of patients according to visual field findings
|
Visual field |
N |
% |
|
Arcuate scotomas |
6 |
9 ,67 |
|
Paracentral scotomas |
8 |
12,90 |
|
Nasal step defects |
13 |
20,96 |
|
Agonic |
15 |
24,19 |
|
Blindness |
3 |
4,83 |
|
Not done |
17 |
27 ,41 |
|
TOTAL |
62 |
100 |
4. Discussion
Among the 3660 patients examined during the study period, 31 cases of glaucoma were diagnosed, representing a frequency of 0.84%. This frequency is significantly lower than those observed by Moukouri E [5] in Yaoundé who found 1.67% and those reported in Nigeria, 1.23% [6]. Our values only partially reflect the importance of glaucoma in our environment, where 2/3 of the population live in rural areas, without access to specialised ophthalmology consultations, and willingly go to traditional healers and village healers who readily attribute their suffering to witchcraft. In sub-Saharan Africa, prevalence varies from one country to others. Studies performed in Cameroon by Ellong A [7] put it at around 5%. In our study, men accounted for 67.74% of cases compared with 32.25% for women. The predominance of males in chronic open-angle glaucoma was also confirmed by a study conducted by Sounouvou in Benin, who reported a rate of 64% [8].
On the other hand, Bron A [9] observed a predominance of women in France, with a proportion of 53.6%. This difference could be explained by the fact that women's living conditions and the lack of development of the gender approach in developing countries mean that they go for consultations less often than men. Glaucoma is spread very widely throughout the different stages of life. Our series was characterised by the elderly. In 90% of cases, they were aged over 50, with an average age of 65.07 +/- 0.12 years and extremes of 40 and 80 years. The same trend was reported by Bron A [9], who found an average age of 66.4+/12.4 years in France. Sounouvou I et al [8] in Benin reported that 32.6% of patients were aged 65 and over. Glaucoma occurs mainly in people over the age of 40, and its frequency increases with age.
However, the glaucoma can be discovered as early as the third or fourth decade of life, particularly when there is a family history. The majority (90.31%) of patients surveyed were illiterate, and only 9.67% had completed tertiary education. This differs from the study in Mali, where Ramatoulaye et al [10] reported that 67.33% of patients were educated. Knowledge of eye care is linked to the level of education, as people with primary education or no education easily develop negative attitudes to accessing care. More than half (68.20%) of the patients surveyed live in rural areas, compared with 37.80% in urban areas. Sounouvou [8] also found that 82% of patients in Benin came from rural areas. Delcourt C et al [11] highlighted a low prevalence of glaucoma in rural patients in France (0.52%).
This difference is explained by the absence of health centres with an ophthalmology service in rural areas in developing countries such as ours, unlike in other countries. The distance of the service from people's homes is a major problem, with many patients travelling many kilometres before having access to eye care. Our results showed that hypertension was the main risk factor, with a rate of 38.70%. The incidence of hypertension was 13.3% in Congo Brazzaville [12] and 30% in France [13]. Hypertension is thought to lead to microangiopathy, which reduces blood flow to the optic nerve, causing ischaemia and increasing the risk of visual field defect [14]. An increase in blood pressure of 10 mm Hg is physiologically accompanied by a concomitant rise in intraocular pressure of around 1 mm Hg, which probably explains the relationship between hypertension and ocular hypertony. A large number of epidemiological studies indicate a link between hypertension and glaucoma [15].
Diabetes was the second most common risk factor, with a frequency of 12.90%. This frequency is similar to those of Makita BC et al in the Congo, who found a frequency of 14.7% [16].
None of the patients in our series had a history of ocular hypertony, which may be explained by the low frequency of access to eye care, but also perhaps by the non-practice of systematic measurement of intraocular pressure (IOP) after the age of 40. However, IOP is almost 4.5%, as reported respectively by Balo in Togolese and Bernardin [17] in Tananarivians. On the other hand, our rate remains lower than those noted by Tchabi [18], who reported 6.8% in Benin.
Sleep apnoea was not found in any of the patients in the study. Various studies have shown that there is probably a link between glaucoma and sleep apnoea syndrome. Blumen [14] found that more than 60% of patients in France had sleep apnoea syndrome.
Sleep apnoea syndrome is associated with nocturnal desaturation and sympathetic hyperresponsiveness, which may be detrimental to the vascularisation and oxygenation of the optic nerve. No history of vasospasm was found in our study. Vasospasm is often characterised by sectorial involvement of the optic disc, which is usually pale and poorly coloured [15]. None of our patients had a known family history of glaucoma. The existence of genetic factors has long been recognised in the pathogenesis of glaucoma. The disease is 15 times more frequent in subjects whose close relatives have glaucoma. Myopia accounted for 9.2% of our cases. Mitchell [19] highlighted that glaucoma is more common in myopic patients than in visually impaired patients without glaucoma. High myopia makes the globe more vulnerable to ocular hypertonia, and diagnostic problems are regularly encountered because of the papillary and perimetric alterations that coexist in this ametropia and in glaucoma.
The majority of our patients had low visual acuity and 21.66% of patients had finger-counting visual acuity, 16.66% with 3/10, MDD in 13.33% and PL- in 11.66%. Our series is similar to that of Tchabi S et al [18], 15% of whose patients had visual acuity limited to positive light perception, finger counting represented 32.9% of their sample, and 29% had 3/10. Some authors have found higher figures than ours, such as Daghfous F et al [20] found in their Tunis study that 45.5% of eyes had visual acuity of less than 3/10. Patients are seen at a very advanced stage of their glaucoma, which explains the deterioration in visual acuity. In 74.35% of cases, patients had intraocular pressure values in the range 21 to 29 mmHg, and 17.94% of patients had IOP values greater than 30 mmHg. Loukil L et al in Tunisia [21] also found high IOP (22.78%). Our study shows that 38.7% of the patients consulted had a papillary excavation of 0.9. Ramatoulaye K found at the Institut d'Ophtalmologie Tropicale de l'Afrique that papillary excavation was greater than 0.8 in the right eye (39%) and in the left eye (42.5%) on fundus examination [10]. A large papillary excavation can be considered as a sign of glaucoma progression before visual field deterioration.
Most of our patients had a delay in treatment, which led to the advanced anatomical lesions of the optic nerve seen on the fundus. In our series, we observed 24.19% of agonic visual field and 20.96% of step nasal defects. The study conducted by Laplace O et al [22] showed that the visual field was moderately impaired in 20% of cases and severely altered in 80%. This can be explained by the absence of systematic consultations and a lack of information and awareness, as is the case in developed countries; in addition, the shortage of hospital infrastructure contributes to this issue.
5. Conclusion
Our study was carried out in the Ophthalmology Department of the CHU PZaGa with the aim of determining the prevalence, risk factors and epidemio-clinical aspects of glaucoma in the Ophthalmology Clinic of university hospital Professeur Zafisaona Gabriel Mahajanga. In this study, the prevalence of glaucoma was 0.84%. The majority of patients were aged between 50 and 80 years. The incidence of glaucoma increases with age, and is highest in people with lower levels of education and from rural areas. It is more common in subjects with a history of diabetes, high blood pressure, trauma and eye surgery. Glaucoma is a disease that prognosis remains problematic due to the failure to diagnose it early. Hence the importance of raising awareness among doctors and the general public. From this study, we were able to highlight the frequency of cases that were discovered very late at the agonic stage and even at the stage of total blindness. Emphasis should be placed on the need for a systematic ophthalmological consultation for any patient with a family history of glaucoma aged 40 or over. The department therefore needs to strengthen its institutional, human, material and financial resources in order to reach out much more to the public.
Acknowledements
We would like to acknowledge and thank A.Sh, the patient presented in this case, for providing us with permission to use images to help educate future clinicians.
Human Ethics
Consent was obtained by the patient in this study.
Conflicts of Interests
There are no conflicts of interest.
References
- Flament J. Pathologie du système visuel. Paris : Elsevier Masson (2002).
- Villain MA. Epidémiologie du glaucome. J Fr Ophtalmol 2 (2005): 209-212.
- Bron A, Nordmann JP, Baudouin C. Glaucome et hypertonie oculaire : importance de la pression intraoculaire cible dans la prise en charge thérapeutique en France. J Fr Ophtalmol 26 (2003) : 895-903.
- Rotchfor AP, Johnson G. Glaucoma in Zulus : a population-based cross-sectional survey in a rural district in South Africa. Arch Ophthalmol 120 (2002): 471–78.
- Moukouri E, Moli MC. Le glaucome chronique primitif à angle ouvert en milieu Camerounais. Méd Afr Noire 38 (1991): 8-9.
- Cepelic J, Cermohorsky M. the effects of adrenergic agonists on the adenyl atecyclase in albinor abbitciliary processes. Exp Eye Res 32 (1981): 291-99.
- Ellong A, Ebana C, Bella AL, et al. La prévalence des glaucomes dans une population de noirs Camerounais. Cahier de Santé 16 (2006): 204-207.
- Sounouvou I, Assavedo AR, Alamon S. Aspects socio-économique de la prise en charge du glaucome primitif à angle ouvert au Bénin. J Fr Ophtalmol 38 (2015): 809-814.
- Bron A. Traitement des glaucomes. Rev Prat 51 (2001): 2098-2201.
- Ramatoulaye K, Abdoulaye N, Minata K, et al. Etude du glaucome primitif à angle ouvert à l’Institut d’Ophtalmologie Tropical Africaine. Mali Méd 32 (2017): 2-5.
- Délcourt C, Bron A, Baudouin C. Prévalence et description du traitement par hypotonisants pour le glaucome et hypertonie oculaire en France. J Fr Ophtalmol 29 (2006): 1098-1106.
- Khoumouri R, Moussaoui K, Machoumi F, et al. Profil épidémiologique du glaucome chronique à angle ouvert à Marrakech. J Fr Ophtalmol 6 (2011): 476-479.
- Loukil L, Korchena N, Hachicha F, et al. Facteurs oculaire prédictifs de la progression du glaucome primitif à angle ouvert dans la population Tunisienne. J Fr Ophtalmol 36 (2013): 324-330.
- Blumen OE, Blumen M, Demonchy I, et al. Glaucome et ronflement : rechercher le syndrome d’apnée du sommeil. J Fr Ophtalmol 34 (2012): 396-399.
- Dugast P, Thiboust T, Blumen-Ohara E, et al. Faut-il une éducation des patients atteint de glaucome à angle ouvert ? J Fr Ophtalmol 127 (2011): 321-329.
- Makita BC, Madzou M, Botara E, et al. Prise en charge du glaucome chronique à angle ouvert et l’hypertonie oculaire à Brazzaville/Congo. J Fr Ophtalmol 2 (2006): 12-15.
- Bernardin P, Rabenatoandro C, Auzemery A. La trabéculectomie à Madagascar. Rev Int 11 (1994): 125-135.
- Tchabi S, Abouki C, Sounouvou I, et al. Observance aux traitements médicaux dans le glaucome primitif à angle ouvert. J Fr Ophtalmol 34 (2011): 624-628.
- Mitchell P, Hourihan F, Sandbach J, et al. The Relationship between glaucoma and myopia : the Blue Mountains Eye Study. Ophtalmol 106 (1999): 2010-2015.
- Daghfous F, Jeddy A, Sebai L, et al. Profil épidémiologique du glaucome à angle ouvert en Tunisie. Rev Int Trach (1991): 116-21.
- Loukil L, Korchene N, Hachicha F, et al. Facteurs oculaire prédictifs de la progression du glaucome primitif à angle ouvert dans la population Tunisienne. J Fr Ophtalmol 36 (2013): 324-330.
- Laplace O, Bron A, Nordmann JP. Prise en charge du glaucome chronique à angle ouvert et l’hypertonie oculaire par les ophtalmologistes français. J Fr Ophtalmol 29 (2006): 353-358.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
