Innovation in the Italian National Health System and the Cost-Reducing Impact of E-Health and Telemedicine: The special case of the Telemedicine Project of the Casa Sollievo della Sofferenza Hospital (Apulia Region)—When Information and Communication Technology Comes to the Aid of the Territory
Matteo Maria Cati
University of Bologna, Department of Economics, 2 Scaravilli Square, 40126 Bologna – Italy
*Corresponding author: Matteo Maria Cati, University of Bologna, Department of Economics, 2 Scaravilli Square, 40126 Bologna – Italy
Received: 16 December 2022; Accepted: 22 December 2022; Published: 28 December 2022
Article Information
Citation: Matteo Maria Cati. Innovation in the Italian National Health System and the Cost-Reducing Impact of E-Health and Telemedicine: The special case of the Telemedicine Project of the Casa Sollievo della Sofferenza Hospital (Apulia Region)—When Information and Communication Technology Comes to the Aid of the Territory. International Journal of Applied Biology and Pharmaceutical Technology 13 (2022): 051-063.
View / Download Pdf Share at FacebookAbstract
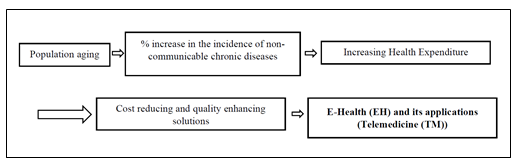
The recent events of the COVID-19 pandemic, caused by the SARS-CoV-2 virus, have dramatically and suddenly changed the dynamic interactions among the various elements of the complex social and economic texture of most countries around the globe, such as Italy, accelerating the digital transformation in many areas of human activity and in particular in the health care sector. After having defined e-health (Figure 1) and some of its applications, with particular reference to telemedicine, the following important research question is addressed: what are the factors that contribute to the successful introduction of telemedicine? To answer this question, this article focuses on the recent efforts of the Italian Health Legislation to increase e-health literacy and to incentivize the health care system to adopt the new tools of information and communication technologies. In particular, the role of telemedicine is highlighted for its cost-reducing effect, particularly when dealing with patients affected by chronic, noncommunicable diseases. For this purpose, the author considers as a special case study the implementation strategy of the Telemedicine project of the Casa Sollievo della Sofferenza, a private Catholic hospital in Southern Italy, as an example of excellence.
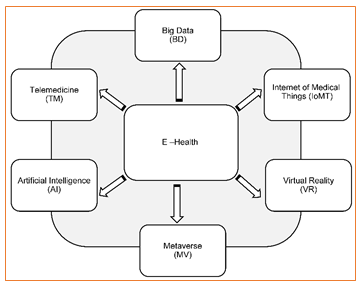
Figure 1: (Graphic presentation) – E-Health and some of its applications
Keywords
E-Health, Telemedicine, Information and Communication Technologies, Health Policy, Health Legislation
E-Health articles, Telemedicine articles, Information and Communication Technologies articles, Health Policy articles, Health Legislation articles
Article Details
1. Introduction
The COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus [1-5], has had devastating global effects in terms of death tolls and the overall number of infections. The spread of the virus and the resulting drastic emergency measures, that were introduced almost everywhere, particularly in Italy [6-8], to reduce the transmission and proliferation of the infection and the formation of clusters of infected people
- dramatically and suddenly changed the dynamic interactions taking place among the various elements that compose the complex system of the social and economic texture;
- accelerated the digital transformation in many areas of human activity [9,10].
The health emergency measures, such as lockdowns and curfews, introduced by governments [11] have conditioned billions of families and businesses to relate with the surrounding environment in a completely different way and raised very heated debates on the possible undemocratic nature of these interventions [12,13]. In the past two years, smart working, distance learning and e-health have become aspects of peoples' daily routines [14]. COVID-19 disrupted life in general and the way public and private organizations function. Many companies were forced to allow their employees to work at home, and many people had to integrate digital technologies into their working lives.
There is no doubt that the pandemic, together with other factors such as the evolution of the population’s structure in Europe and in Italy, has accelerated the pace of digital transformation [15,16] in many sectors of the economy, including health care and education. Even if, at this stage, it is not clear what will be the future impact of such a new trend [17], it is evident that it has determined organizational changes and the need to redesign business strategies. As many observers have noted, the rapid introduction of e-health will most likely reshape the future health industry, which represents one of the most important sectors of the world economy [18].
Public and private initiatives aimed at promoting the usage of the tools of information and communication technologies (ICT) in health care must in any case be supported by the presence of a regulatory framework at the national and international levels.
This article focuses on the recent efforts of the Italian health legislation to increase e-health literacy and to incentivize the health care system to adopt the new tools of ICT with particular reference to telemedicine. For this purpose, the author considers the implementation of the Telemedicine project of the Casa Sollievo della Sofferenza, a private Catholic hospital in Southern Italy, as a special case study as an example of excellence.
2. E-health and the recent evolution of the European and Italian population’s structure
The usage of the tools of Information and Communication Technologies (ICT) in the health sector, namely, e-health, such as telemedicine [19], is not new news, given the following:
- progressive population aging, particularly of the European (Figure 2) and Italian (Figures 3a and 3b) populations. The size of population changes of a country or of a group of countries depends mainly on four factors: births, deaths, migration flows and exceptional and unpredictable events (such as the COVID-19 pandemic). What immediately catches the eye in Figure 2 is that the population structure of the EU—which comprises the populations of 27 countries (children: 0-14 years; working-age population: 15-64 years; elderly: 65 years and over)—is expected, between 2019 and 2050, to change, with fewer working-age people and an increasingly elderly population.
A similar trend can be observed in Italy. In 2019, on the basis of the data of the Italian National Bureau of Statistics (ISTAT) [20], of 60 million 391 thousand residents (60,391,000),
____________________________
- the population aged 65 and over represented 23.2% of the total;
- that up to 14 years of age 13%;
- that in the range 15-64 years 63.8%;
- and the average age approached the milestone of 46 years.
________________________________
Although long-term forecasts on population trends are uncertain and must be continuously updated, the Italian National Bureau of Statistics (ISTAT) [21] predicts that by 2050, the overall population in Italy will be 54.2 million individuals (52,400,000):
________________________________
- people aged 65 and over could represent 35% of the total;
- young people up to 14 years of age, 11.7% of the total, thus recording a slight decrease;
- those in the range 15-64 years 53.3%;
- and the average age should approach approximately 50 years. In this case, the ratio between those over 65 and young people would be 3 to 1.
_________________________________
These trends will have important implications
- at the macro level (countries, governments, business, civil society, the household sector and business sector, health and social security systems, labor market)
- and at the micro level (individuals, individual firms, pension entitlements and so on).
The most relevant problem for the health care systems of countries such as Italy, in which the population is progressively aging, is the increase in the incidence of noncommunicable chronic diseases in the total population, and the COVID-19 pandemic has become particularly pressing concern [22]. In this regard, the 2022 Annual Report of the Ambrosetti European House Center for Italian Public and Private Health Studies [23] focused on noncommunicable chronic diseases (among which the most common are neoplasms, cardiovascular and cerebrovascular diseases, chronic respiratory illness, diabetes and mental disorders) that are more likely to affect the elderly population (65 years of age and over), and it has highlighted that in 2020,
Figure 2: Population Pyramids, EU-27, 2019 and 2050 (% share of total population)
Source: Eurostat (demo_pjangroup) and (proj_19np)
- in Europe, based on Eurostat data and as indicated by the European Commission initiative of June 2022 "Healthier Together - EU Non – transmissible diseases" [24,25],
- 6% of European citizens (of 447.7 million individuals [26]) had a problem due to the presence of one or more nontransmissible (noncommunicable) chronic diseases;
- in particular, 65% of those over 65 and 70% of those over 75 were affected by one of the aforementioned pathologies.
- in Italy, people with at least one chronic disease represent 40.9% of the population (59,236,213 individuals [27]), of whom more than 90% are individuals over 75 years of age.
It is intuitive to imagine that the progressive aging of the European and Italian populations, as illustrated in the demographic pyramids (Figures 2, 3a and 3b); the reduction in the mortality rate due to therapeutic and technological innovations; the lack of prevention and of a culture aimed at adopting correct lifestyles will increase the share of citizens in Italy and in Europe who are affected by noncommunicable chronic diseases and comorbidities;
The progressive increase in population aging and the number of individuals with chronic diseases will have a strong impact on the evolution of health expenditure in Europe and Italy.
Recent data show that in 2020, the share of health expenditure in the EU due to chronic illness was equal to approximately 70-80% of the total, corresponding to approximately 700 billion Euros per year. In Italy, health care expenditure for chronically ill people is equal to approximately 67 billion euros, corresponding to 50-60% of the total health expenditure.
The recent evolution of health expenditure in Italy between 2018–2022 and the forecasts for 2023–2025 (Table 1) clearly reveal the following:
Table 1: Italy - Data on Health Expenditure (in millions of Euro), as a % change with respect to the previous year, as a % of real GDP, from 2018 to 2022 and forecasts for 2023–2025.
(Source: Memorandum of the Court of Accounts on the Update Note of the 2022 Economy and Finance Document – available at: https://www.corteconti.it/HOME/Documenti/DettaglioDocumenti?Id=3d140efb-aaf5-4f27-b177-03951626b38f and Chamber of Deputies - Parliamentary documentation - The Level of Funding of the National Health Service in 2022– available at: https://temi.camera.it/leg18/temi/tl18_il_fabbisogno_sanitario.html)
|
2018 |
2019 |
2020 |
2021 |
2022 |
2023 |
2024 |
2025 |
|
|
Health Expenditure (millions of Euros) |
114,423 |
115,661 |
122,721 |
127,834 |
133,998 |
131,724 |
128,708 |
129,428 |
|
% change previous year |
- |
1.10 |
6.10 |
4.17 |
4.82 |
-1.70 |
-2.29 |
0.56 |
|
As a % of real GDP |
6.0 |
6.40 |
7.40 |
7.17 |
7.04 |
6.62 |
6.20 |
6.02 |
- Due to the COVID-19 pandemic, health expenditure underwent strong growth between 2020 and 2021, corresponding to a 6.10% change with respect to the previous year and a 7.40% percentage growth rate with respect to real GDP. Such a growing trend is expected to continue through 2022.
- For various reasons (including the need to contain public spending and reduce the public debt-to-real GDP ratio as required by the European Union, global geopolitical events that have led to an increase in energy costs and of the rate of inflation), the recent Update Note of the 2022 Economic and Financial Document [28,29] drawn up by the Italian Government foresees in 2023 and 2024 a substantial decrease in health expenditure (also considering the plans to reduce health expenditure implemented in various Italian regions to contain total public health expenditure [30-35]):
- between 2022 and 2023, the expenditure will decrease from 133,998 to 131,724 million euros, corresponding to a 1.7% decrease in health expenditure with respect to the previous year;
- between 2023–2024, the expenditure will decrease from 131,998 to 128,708 million euros, i.e., a 2.29% decrease with respect to the previous year.
The contraction in health care spending over the next two years will also have a strong impact on the evolution of the health care sector (considering the endemic shortage of health personnel (in particular doctors and nurses) in emergency rooms, hospitals and in the Italian territory).
If we now jointly consider the previous issues and, in particular, the following:
- progressive aging of the population (the resident population in Italy is decreasing: from 59.2 million in 2021 to 57.9 million in 2030 and to 54.2 million in 2050 [36]). The ratio between individuals of working age (15-64 years) and those of nonworking age (0-14 years and 65 years of age and older) will go from approximately three to two in 2021 to approximately one to one in 2050, and in particular, the projections of the Italian National Institute of Statistics predict that for every 280 elderly people, there will be 100 young people in 2051).
- the resulting increase in the incidence of total noncommunicable chronic diseases, which the World Health Organization (WHO) [37,38] considers to be the cause of 75% (accounting for 486,663 victims of noncommunicable chronic diseases) of overall deaths in Italy of people aged 70 years or older in 2019 (most recent available information);
- the greater burden that this will place on health expenditure (the health incidence will rise to 9.5% of GDP in 2050 [39] due to the progressive aging of the population and the greater numerical importance of noncommunicable chronic diseases);
it is intuitive to imagine that precedence will be given to cost-reducing solutions, i.e., to health policies aimed at reducing costs and increasing the effectiveness and efficiency in the provision of health services, such as, as indicated by the European Commission, e-health (also known as digital health), given the cost-reducing impact of digital health for both the organization and the patients. As a recent study states [40]:
“Digital health interventions have significant potential to improve safety, efficacy, and quality of care, reducing waste in healthcare cost.”
3. E-health and telemedicine
Electronic health (e-health) applies the tools of information and communication technologies (ICT) to health care. Various definitions of e-health have been given in the literature [41-43] and by international and national entities. The WHO [44] defines e-health as follows:
“cost-effective and secure use of information and communication technologies (ICT) in support of health and health-related fields. It encompasses multiple interventions, including telehealth, telemedicine, mobile health (mHealth), electronic medical or health records (eMR/eHR), big data, wearables, and even artificial intelligence. The role of eHealth has been recognized as pivotal in attaining overarching health priorities such as universal health coverage (UHC) and the Sustainable Development Goals (SDGs).”
On the other hand, the European Union [45], with particular reference to its members’ states, suggests that e-health:
“can improve access to healthcare and boost the quality and effectiveness of the service offered. E-health describes the application of information and communications technologies across the whole range of functions that affect the health sector”.
The Italian Ministry of Health refers to e-health as “the use of tools based on information and communication technologies to support and promote disease prevention, diagnosis, treatment and monitoring and health and lifestyle management”. In other words, “E-Health can be defined as a set of technologies applied with the help of the internet, in which health care services are provided to improve quality of life and facilitate health care delivery” [46].
All definitions have a common denominator, meaning that they all combine
- information technology,
- telecommunications,
- and medicine
and highlight the main purpose of e-health [47], that is, to expand health care locally, regionally, nationwide and universally to improve the well-being of individuals [48,49]. The most common applications of e-health are telemedicine, big data, the metaverse, artificial intelligence, the internet of medical things (e.g., surgical devices and implantable devices) and virtual reality (see Figure 1 – graphical representation).
The systematic study of the applications of e-health, such as telemedicine, both at the macro level (within a nation) and at the micro level (locally in public or private hospital structures) requires the following:
_________________________________
the identification [50] of
- the needs [51] that e-health fulfills;
- the determinants of e-health demand [52];
- the determinants of e-health supply [53]; and
- whether e-health facilitates access [54] to care.
_________________________________
At the base of the introduction of e-health, there are the needs that it is supposed to satisfy. However, what does the term "need" mean, and in particular, what does it mean when referring to e-health? To be able to define it, it is necessary first to identify the meaning of health care and then to find the definition of health need.
The term health care [55] “means treatment, prevention and supportive care that is effective – either alone or as part of a care pathway – in improving, maintaining, or slowing the deterioration of health now or in the future (or both)”. Before defining the notion of health need, as well as the definition of health care, there is an equally relevant concept, that is, ‘access to health care’, whose importance has been reiterated on many occasions by the European Commission [56]. ‘Access to health care’ is the right of everyone to “timely access to affordable, preventive and curative health care of good quality”. The concept of health need is strictly linked to both the notions of health care and access to health care. In fact, health needs are defined as “the right care (meaning cost – effective care) provided in the right place and the right time”.
During the worst period of the COVID-19 pandemic, a new, urgent need arose to avoid direct contact between patients and doctors since such contact was becoming a potential source of contagion. The acceleration of the transition from face-to-face visits to remote visits using ITC tools has given the impetus to the use of some of the e-health applications, among which telemedicine (an application of e-health whose demand and supply were weak before the beginning of the pandemic and delivered in mostly experimental conditions) stands out in importance.
The WHO [57] defines telemedicine as follows:
“the provision of healthcare services at a distance with communication conducted between healthcare providers seeking clinical guidance and support from other healthcare providers (provider-to-provider telemedicine); or conducted between remote healthcare users seeking health services and healthcare providers (client-to-provider telemedicine)”.
The World Health Assembly Resolution on Digital Health (W.H.O. 2018) [58] recognizes “the important role of digital technologies, such as Telemedicine, to strengthen the health system, to improve the Universal Health Coverage (UHC) (i.e. to ensure the quality, accessibility and affordability of health care services”) [59] and to ensure the achievement of other purposes of the Sustainable Development Goals (SDGs) [60,61]. E-health and its applications, such as telemedicine, can improve health and decrease health inequality.
Although the effectiveness of telemedicine compared to in-person visits is still being studied, considering its relative ease of use (in comparison with respect to other e-health applications) with a variety of telecommunication tools such as smartphones, tablets, telephones and others, it may be useful to deepen the discussion of this issue.
One of the recent questions affecting the health care system is what factors influence its performance. Among them (on the basis of the list given by the WHO [57]), the following stand out in terms of relevance:
- “relative geographical inaccessibility (of hospitals, polyclinics, medical clinics…);
- low demand for services;
- delayed provision of care;
- low adherence to clinical protocols;
- costs to individuals/patients;
- costs to doctors and hospitals;
- health expenditure trend”.
If we look at the literature, it seems clear that the introduction of telemedicine may have a beneficial effect [62] in solving, with reference to the previous list, problems of geographical inaccessibility, low demand for services, and delayed provision of care, and it may have cost-reducing effects (see points e), f) and g)). More specifically, as we will see, the cost-reducing effect of telemedicine may particularly concern the following type of costs:
|
Direct Costs |
Indirect Costs |
|
For individuals/patients Travel Costs |
For individuals/patients The loss of a working day |
|
For the organizations and the health system Consultation prices (Hospitals) |
For the organization and the health system § occupation of physical space and material resources consumption of involved hospitals; § greater pressure on administrative and clinical services; § overload of the specialty’s appointment schedule |
Table 2: Direct and Indirect Costs that Telemedicine may Decrease.
Barriers to free access to health care services, as well as problems of quality and affordability, were already relevant issues in many OECD countries prior to the beginning of the COVID-19 pandemic, which has highlighted these issues further.
A recent OECD report [63] suggests that in 2019,
- access to health care, at the origin of unmet needs, is often compromised by limited availability or affordability;
- more than 30% of the population in countries such as Italy had accessibility problems since care was delayed or forgone due to waiting times and/or transportation difficulties;
- 23% of the low-income population delayed or did not look for care due to affordability issues.
In summary, there are many occasions where the health needs of individuals are unfortunately not met. Unmet needs are a common measure [64] of access to health care in Europe and in OECD countries and are quite helpful in identifying the limits, which were present before the COVID-19 pandemic and that the spread of the virus further highlighted, of a nation’s health care system and the spaces for improvement, where technological innovation plays a crucial role.
4. The special case of the Telemedicine Project of the Casa Sollievo della Sofferenza Hospital
We have seen how the COVID-19 pandemic has highlighted the strengths and weaknesses of the Italian national health system, such as the following:
- systematic shortage of medical and health care personnel, particularly in emergency departments;
- evolution of public health expenditure (see Table 1), which increased during the pandemic and is now expected to decrease over the next two years, 2023 and 2024, in an effort to remedy the problems of high structural public debt;
- health spending reduction plans (namely, the health spending review) in the most indebted Italian regions (i.e., regions that have a structural health deficit greater than 5% of ordinary financing and have health revenues), implying cuts in health spending and investments [65]; currently, in Italy, there are seven regions that apply reduction plans (Abruzzo, Calabria, Campania, Lazio, Molise Puglia and Sicily), two of which (Molise and Calabria) are administered by special commissioners;
- the need for greater capillary coverage and territorial surveillance to better cope with any future pandemics and the country's demographic dynamics to guarantee effective coverage of the health needs and more effective prevention policies of the entire population and throughout the Italian territory, divided between the industrialized regions of the north and the agricultural regions in central Italy and the south;
- the importance of accredited private hospital structures, which often make up for the shortcomings of public health and are often marginalized or excluded from public health investments.
In addition, the spread of the virus has accelerated, both in the northern regions and in the central and southern regions, the digital transformation and, in particular, the use of ICT tools that, as the current literature now recognizes [66,68], improve the quality, accessibility and affordability of health care services, i.e., universal health coverage (U.H.C.). In Italy, several hospitals started intensifying the implementation of telemedicine (in particular, televisits) projects to exploit the beneficial effects that the digital transformation [69,70] has been proven to provide during the worst period of the pandemic.
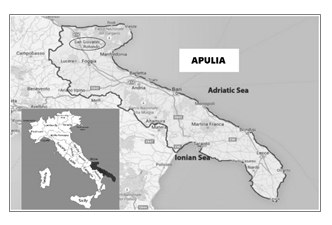
One of the Italian cutting-edge projects concerning the provision of telemedicine services and, in particular, televisits has been implemented and carried out by the Hospital Casa Sollievo della Sofferenza (House for the Relief of Suffering), founded by the famous Italian Capuchin Father Pio of Pietrelcina, located in San Giovanni Rotondo, a town in Apulia (see Figure 1), one of the regions of Southern Italy. Despite its particular territorial location (San Giovanni Rotondo, 565 meters above sea level and approximately 45 minutes from Foggia, is the third most important city in the Apulia region but cannot be reached by train or by airplane but only with private transport or by bus), the aforementioned hospital represents one of the few examples of excellence in a private accredited hospital in Southern Italy, if not the only one, with 865 beds, ISO 9001-2015 certification and involvement in cutting-edge biomedical research.
Considering the particular territorial conformation of Italy, with the more industrialized North and the agricultural South, the results obtained by the Padre Pio Hospital position it as a state-of-the-art health care facility in terms of quality and quantity of services provided in the area and the skills of the managers running the hospital, despite public health management that is not always favorable to health facilities of that type. Such excellence has been recognized in the rankings, based on factors such as cost, advanced technology, quality treatment and others, drawn up by Newsweek in ‘The World's Best Hospitals 2022’ (available online at: https://www.newsweek.com/worlds-best-hospitals-2022/italy). Casa Sollievo della Sofferenza is in 29th place and is indicated as the best hospital in Southern Italy.
The service area of the Casa Sollievo della Sofferenza Hospital (hereafter simply C.S.S.) includes mainly the
southern regions (considered rural areas with respect to the more industrialized North) of Puglia, Basilicata, Sicily, Campania, Molise, Abruzzo and Calabria, representing 18,253,329 million people, corresponding to approximately 30.9% of the overall population in Italy (58,983,000 individuals as of January 1st, 2022, on the basis of the data from the Italian National Bureau of Statistics (ISTAT)). In this scenario, the COVID-19 pandemic has clearly accelerated the digital transformation and e-health literacy [71,72], with particular reference to telemedicine, considered the ideal tool to avoid direct contact between patients and doctors, and in the health care sector. Taking advantage of the acceleration in the use of ITC tools and anticipating the Italian legislation [73-77], since July 2022, Casa Sollievo della Sofferenza has implemented the first Televisits for the Gastroenterology Operative Unit (with reference to inflammatory bowel disease) [78] and for the operative units dedicated to pain management. Over time, the project will be extended to over thirty specialties.
The telemedicine project implemented by C.S.S. is part of a broader vision proposed (see the Project Work -Hospital-Territory integration in the management of the post-acute or chronic phase of patients. A shared management in the light of the DM 77 and the funds of the Piano Nazionale di Ripresa e Resilienza (PNRR) [79] (Apulia Region)) by recent Italian legislation (Ministerial Decree 77, 2022). This legislation pertains to the role of hospitals and the need to integrate hospital care with territorial care and to cope with the new scenarios and new health needs due to the epidemiological (COVID-19 pandemic caused by the SARS-CoV-2 virus), demographic (progressive aging of the population) and social (economic inequalities) transition. In addition, there are needs due to the spending health review implemented by the Italian government following the high health deficit in various regions, particularly in Apulia.
As a result, “the recent legislation (such as the so called ‘spending review’ and DM 70 in 2021) in this regard provided for the decrease in the number of accredited hospital places financed by the Regional Health Service, equal to no more than 3.7 bed places per 1000 inhabitants, and 0.7 bed places per 1000 inhabitants for rehabilitation and long-term post-acute care. Hence the need to identify alternative forms to hospitalization and enhance the specialist outpatient network, especially for the system of care dedicated to chronic diseases” [80]. A profound modernization (DM 77 in 2022 and expected subsequent changes) of territorial healthcare and a further variation of the standards in hospitals, such as the number of beds per 1000 inhabitants, is foreseen in the various legislative updates in place.
Even if the data are not yet available, the televisits project, started during the COVID-19 pandemic and still ongoing, of the gastroenterology operative unit (with reference to inflammatory bowel disease) of the Casa Sollievo della Sofferenza Hospital is an example of the effort to increase and improve the effectiveness of health coverage with particular reference to noncommunicable chronic diseases.
This project fits well into the problems that the literature [81-84] on the practical applications of telemedicine and televisits (even in rural areas [85]) has highlighted in terms of the following:
- solving problems of territorial accessibility to hospital and outpatient clinics;
- finding effective alternatives to rehospitalization of discharged patients with chronic diseases;
- its cost-reducing effects with particular reference to the following:
- decrease in costs for patients and their families (less travel and less time wasted);
- reduction in costs for hospital structures and doctors who provide telemedicine services and, in particular, televisits.
Furthermore, telemedicine and televisits seem to improve the quality, accessibility and affordability (through a cost reduction for both patients and hospitals) of health services, i.e., U.H.C. and its effectiveness.
A reliable metric [86] to track progress in achieving U.H.C. is the notion of effective coverage, which the WHO defines as [87] “people who need health services obtain them in a timely manner and at a level of quality necessary to obtain the desired effect and potential health gains”.
The events that occurred during the pandemic and the current situation of the Italian health system, with particular reference to the Apulia region where the Casa Sollievo della Sofferenza Hospital is based, have highlighted the emergence of unmet needs for various reasons (from the pandemic health emergency to problems due to territorial distances and transportation costs, waiting lists, and convenience). These circumstances, as also highlighted by the various OECD reports, even before the start of the pandemic, gave the opportunity to detect the presence of a part of the population whose health needs, due to various barriers, were not met and who were therefore in a certain way left behind. For this reason, the ongoing telemedicine and televisits projects for chronic nontransmissible diseases [88] fit well in the so-called Tanahashi framework [89], on the basis of which health coverage can be examined through a series of dimensions, i.e..
|
Availability |
Health care facilities, goods, services and programs together with a functioning public health system have to be available in sufficient quantity |
|
Accessibility |
Health care facilities, goods, and services have to be accessible in the jurisdiction of the state, without discrimination to anyone |
|
Acceptability |
Health care facilities, goods, and services must be culturally appropriate and respectful of medical ethics |
|
Contact |
Actual contact between the service provider and the user |
|
Effectiveness |
Barriers in treatment adherence, provider compliance and diagnostic accuracy |
Furthermore, health facilities, goods and services must be scientifically and medically appropriate and of good quality.
The Tanahashi framework is useful for determining the reasons why there might be subsets of a given population that access and benefit from health care services and others are that do not through the identification of the following:
- barriers (i.e., factors that hinder the target population from making the appropriate use of the health service offered);
- facilitating factors (factors that enable the target population to make full use of the health service offered).
The telemedicine and televisits project implemented by the Casa Sollievo della Sofferenza, particularly for chronic nontransmissible diseases, seems to be able to fill part of the gap between the target population that currently is unable to access the required health services and the actual health coverage and to benefit not only patients but also hospitals due to its cost-reducing impact.
5. Conclusions
The COVID-19 pandemic has accelerated the digital transformation and the use of new tools of ITC, such as telemedicine and televisits. During the post-COVID-19 era, e-health and its applications can become a relevant instrument capable of improving the provision and accessibility of health services, health care performance and the ability to achieve universal health coverage and the dimensions described by the Tanahashi framework. The pilot project for the implementation of televisits at the Casa Sollievo della Sofferenza Hospital, an international center of excellence in Southern Italy, is an example to be imitated.
Disclosures
The author has no conflicts of interest to declare.
Funding
The author has not received any funding
Acknowledgments:
I am sincerely grateful for the instructive conversations and information received from
- Doctor Michele Giuliani, Director General of the Casa Sollievo della Sofferenza Hospital, Institute for Scientific Hospitalization and Care (IRCCS);
- Doctor Francesco Perri, Director of the Gastroenterology Operative Unit, Casa Sollievo della Sofferenza, Scientific Hospitalization and Treatment Institute (IRCCS);
- Doctor Giuseppe D'Orsi, Director of the Neurology Operative Unit, Casa Sollievo della Sofferenza Hospital, Scientific Hospitalization and Treatment Institute;
- Doctor Michele Grifa Orthoptist at the Casa Sollievo della Sofferenza Hospital;
- Doctor Fabrizio Bossa, Medical Director, UOC Gastroenterology and Digestive Endoscopy, IRCCS Casa Sollievo della Sofferenza, Opera di San Pio da Pietrelcina;
- Doctor Nicola Fiorentino, journalist, Office of Communication and External Relations, IRCCS Foundation Casa Sollievo della Sofferenza Hospital, Work of Saint Pio of Pietrelcina.
Any mistakes are mine.
References
- Hu B, Guo H, Zhou P. et al.Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol 19 (2021): 141–154.
- Mohanty SK, Satapathy A, Naidu MM. et al.Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19) – anatomic pathology perspective on current knowledge. Diagn Pathol 15 (2020): 103.
- da Silva Torres MK, Bichara CDA, de Almeida MNS, Vallinoto MC, Queiroz MAF, Vallinoto IMVC, dos Santos EJM, de Carvalho CAM and Vallinoto ACR the Complexity of SARS-CoV-2 Infection and the COVID-19 Pandemic. Front Microbiol 13 (2022): 789882.
- del Rio C, Malani PN. COVID-19 in 2022—The Beginning of the End or the End of the Beginning? JAMA327 (2022): 2389–2390.
- de Souza AS, de Freitas Amorim VM, Guardia GDA, dos Santos FF, Ulrich H, Galante PAF, et al. Severe Acute Respiratory Syndrome Coronavirus 2 Variants of Concern: A Perspective for Emerging More Transmissible and Vaccine-Resistant Strains. Viruses 14 (2022): 827.
- Harari YN The world after coronavirus Financial Times (2020).
- Zbigniew Truchlewski, Waltraud Schelkle & Joseph Ganderson. Buying time for democracies? European Union emergency politics in the time of COVID-19, West European Politics 44 (2021): 5-6, 1353-1375.
- Gatto M et al. Spread and dynamics of the COVID-19 epidemic in Italy: Effects of emergency containment measures Proceedings of the National Academy of Sciences 117 (2020): 10484-10491.
- Nagel L. "The influence of the COVID-19 pandemic on the digital transformation of work", International Journal of Sociology and Social Policy 40 (2020): 861-875.
- Renata Gabryelczyk. Has COVID-19 Accelerated Digital Transformation? Initial Lessons Learned for Public Administrations,Information Systems Management 37 (2020): 303-309.
- Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci Prog 104 (2021): 368504211019854.
- Thomson S, Ip EC. COVID-19 Emergency Measures Are Hurting Democracy Globally. Am J Public Health 110 (2020): 1356-1357.
- SCHEININ, Martin, COVID-19 symposium: to derogate or not to derogate?Opinio Juris (2020).
- De' R, Pandey N, Pal A. Impact of digital surge during Covid-19 pandemic: A viewpoint on research and practice. Int J Inf Manage 55 (2020): 102171.
- Soto-Acosta P. COVID-19 Pandemic: Shifting Digital Transformation to a High-Speed Gear (2020): 1058-0530.
- Nagel L."The influence of the COVID-19 pandemic on the digital transformation of work", International Journal of Sociology and Social Policy 40 (2020): 861-875.
- DeFilippis E, Impink SM, Singell M. et al.The impact of COVID-19 on digital communication patterns. Humanit Soc Sci Commun 9 (2022): 180.
- Gotz D, Borland D. Data-Driven Healthcare: Challenges and Opportunities for Interactive Visualization. IEEE Comput Graph Appl 36 (2016): 90-96.
- Bitar H, Alismail S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: A rapid systematic review. Digit Health 7 (2021): 20552076211009396.
- Italian National Bureau of Statistics (ISTAT) - Demographic indicators. Press release. Resident population in Italy in (2019).
- [21] Italian National Bureau of Statistics (ISTAT) - Demographic forecasts. Press release. Resident population (forecasts) in Italy in (2050).
- 17° Rapporto Meridiano - Le Coordinate della Sanità. The Ambrosetti European House Center for Italian Public and Private Health Studies (2022).
- European Commission - Healthier Together - EU Non - trasmissible diseases (June 2022).
- Healthier together EU non communicable Diseases Initiative – European Commission (2022).
- Camera dei Deputati – Documentazione Parlamentare – Nota di Aggiornamento al DEF (NADEF) (2022).
- Eurostat – Newsrelease - EU 27 population (2020).
- Italian National Bureau of Statistics (ISTAT) Population Census and demographic dynamics (2020).
- Dossier Camera dei Deputati - Documentazione Parlamentare - Nota di Aggiornamento al DEF (NADEF) (2022).
- Rapporto OASI – Osservatorio sulle Aziende e sul Sistema sanitario italiano – a cura di CERGAS (Centre for Research on Health ad Social Care Management) – Bocconi (2022).
- 5° Rapporto Gimbe sul Servizio Sanitario Nazionale – GIMBE Evidence for Health (2022).
- Ministero dell’Economia e delle Finanze - Ragioneria Generale dello Stato Rapporto n.° 9 - Il Monitoraggio della Spesa Sanitaria (2022).
- Camera dei Deputati - Documentazione Parlamentare – Il livello di Finanziamento del Servizio Sanitario Nazionale (2022).
- Ministero dell’Economia e delle Finanze (MEF). Banca Dati delle Amministrazioni Pubbliche – Servizio Sanitario Nazionale (SSN) (2022).
- 17° Rapporto Meridiano - Le Coordinate della Sanità. The Ambrosetti European House Center for Italian Public and Private Health Studies - Chapter 5 (2022).
- World Health Organization (W.H.O.) Newsroom - Non communicable diseases - 16 September (2022).
- World Health Organization (W.H.O.) Non communicable diseases data portal – Italy.
- Policy and Procurement in Health Care Meridiano Sanità: Il SSN non sarà più sostenibile nel (2050).
- Gentili A, Failla G, Melnyk A, Puleo V, Tanna GLD, Ricciardi W and Cascini F. The cost-eectiveness of digital health interventions: A systematic review of the literature. Front. Public Health 10 (2022): 787135.
- Eysenbach G. What is e-health? J Med Internet Res 3 (2001): e20.
- Oh H, Rizo C, Enkin M, Jadad A. What Is eHealth: A Systematic Review of Published Definitions J Med Internet Res 7 (2005): e1.
- Vial G. Understanding digital transformation: A review and a research agenda, The Journal of Strategic Information Systems 28 (2019): 118 – 144.
- Wyatt JC, Liu JL. Basic concepts in medical informatics. J Epidemiol Community Health 56 (2002): 808-12.
- World Health Organization (WHO) – definition of E-health.
- European Commission. E-health. Making healthcare better for European citizens: an action plan for a European e-health area (2004).
- Ippocrate E-health in the Italian and European Helatcare system (June 15, 2021).
- Abernethy A, Adams L, Barrett M, et al. The Promise of Digital Health: Then, Now, and the Future. NAM Perspect. (2022).
- World Health Organization (WHO) - Regional Office for Europe - From Innovation to implementation – ehealth in the WHO European Region (2016).
- Stewart E, Milton A, Yee H, Song M, Roberts A, Davenport T, et al. eHealth Tools That Assess and Track Health and Well-being in Children and Young People: Systematic Review J Med Internet Res 24 (2022): e26015.
- van Olmen, J. The Promise of Digital Self-Management: A Reflection about the Effects of Patient-Targeted e-Health Tools on Self-Management and Wellbeing. Int. J. Environ. Res. Public Health 19 (2022): 1360.
- Rodriguez Santana I, Mason A, Gutacker N, Kasteridis P, Santos R & Rice N. Need, demand, supply in health care: Working definitions, and their implications for defining access. Health Economics, Policy and Law(2021): 1-13.
- “Need is the capacity to benefit healht care. Health care means treatment, prevention and supportive care that is effective – either alone or as part of a care pathway – in improving, mantaining, or slowing the deterioration of health now or in the future (or both). Need is for ‘appropriate’ health care: this excludes care that is known to be cost-ineffective and includes cost-effective care. For care of unkown cost-effectiveness, need isfor the right care provided in the right place and at the right time.” See page 3 - Rodriguez Santana I, Mason A, Gutacker N, Kasteridis P, Santos R & Rice N. Need, demand, supply in health care: Working definitions, and their implications for defining access. Health Economics, Policy and Law (2021): 1-13.
- “The demand for health care is the level of use at which the perceived marginal health benefits of care equal the marginal cost of accessing care. Below this point, benefits outweight costs and individuals will continue to consume health care. The demand for health care depends on the patients’ and health care professionals’ perspectives of perceived benefits and costs. Benefits and costs are function of factors such as health status, distance from providers, demographics characteristics, health literacy, etc. For example, perceived and acutal helath gairns form caqre will vary with age, education and income; costs will depend on prices (e.g., co-payment for prescriptions), waiting times, time and travel costs for access, etc.” See page 5 - Rodriguez Santana I, Mason A, Gutacker N, Kasteridis P, Santos R & Rice N. Need, demand, supply in health care: Working definitions, and their implications for defining access. Health Economics, Policy and Law (2021): 1-13.
- “The supply of health care includes curative and preventive services and treatments provided by the health care system, so excludes informal care and social care.” See page 6 - Rodriguez Santana I, Mason A, Gutacker N, Kasteridis P, Santos R & Rice N. Need, demand, supply in health care: Working definitions, and their implications for defining access. Health Economics, Policy and Law(2021): 1-13.
- “Following our definition of need as being need for effective and/or appropriate health care, we define access as getting the right helath care in the right place at the right time”. See page 7 - Rodriguez Santana I, Mason A, Gutacker N, Kasteridis P, Santos R & Rice N. Need, demand, supply in health care: Working definitions, and their implications for defining access. Health Economics, Policy and Law(2021): 1-13.
- See page 3 - Rodriguez Santana I, Mason A, Gutacker N, Kasteridis P, Santos R & Rice N. Need, demand, supply in health care: Working definitions, and their implications for defining access. Health Economics, Policy and Law(2021): 1-13.
- Tajani A and Juncker J. “European Pillar of Social Rights” (2017).
- WHO guideline: recommendations on digital interventions for health system strengthening. Geneva: World Health Organization (2019).
- World Health Organization - World Health Assembly Resolution on Digital Health (2018).
- See page ix, supra 57 (WHO guideline: recommendations on digital interventions for health system strengthening. Geneva: World Health Organization (2019).
- Sustainable Development is defined as” as the "ability to make development sustainable-to ensure that it meets the needs of the present without compromising the ability of future generations to meet their own needs". See World Commission on Environment and Development (WCED). Our Common Future (New York: Oxford University Press) 27 (1987): 15.
- Kates W, Robert, Thomas M. Parris & Anthony A. Leiserowitz. What is Sustainable Development? Goals, Indicators, Values, and Practice, Environment: Science and Policy for Sustainable Development 47 (2005): 8-21.
- Haleem A. et al. Telemedicine for healthcare: Capabilities, features, barriers, and applications, Sensors International, VL 2 (2021).
- OECD – Health at a glance 2019: OECD indicators.
- OECD Health Policy Studies – Health for Everyone? Social Inequalities in Health and Health Systems. Inequalities in unmet needs for health care (2019).
- Camera dei Deputati – Servizio Studi – VXIII Legislatura – La spendig review sanitaria (February 14, 2022).
- da Fonseca MH, Kovaleski F, Picinin CT, Pedroso B, Rubbo P. E-Health Practices and Technologies: A Systematic Review from 2014 to 2019. Healthcare 9 (2021): 1192.
- Abernethy A, Adams L, Barrett M, et al. The Promise of Digital Health: Then, Now, and the Future. NAM Perspect (2022).
- Lee P, Abernethy A, Shaywitz D, Gundlapalli AV, Weinstein J, Doraiswamy, PM, et al. Digital Health COVID-19 Impact Assessment: Lessons Learned and Compelling Needs. NAM perspectives(2022).
- Alonso, S.G., Marques, G., Barrachina, I. et al.Telemedicine and e-Health research solutions in literature for combatting COVID-19: a systematic review. Health Technol 11 (2021): 257–266.
- Baudier P. et al. Digital transformation of healthcare during the COVID-19 pandemic: Patients’ teleconsultation acceptance and trusting beliefs - Technovation 102547 (May 16th) (2022).
- Norman CD, Skinner HA. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res 8 (2006): e9.
- Brørs G, Norman CD, Norekvål TM. Accelerated importance of eHealth literacy in the COVID-19 outbreak and beyond. European Journal of Cardiovascular Nursing 19 (2020): 458-461.
- National guidelines for the provision of telemedicine services. State-Regions Agreement (Permanent Conference for relations between the State, the Regions and the Autonomous Provinces of Trento and Bolzano - Agreement, pursuant to article 4, paragraph 1, of the legislative decree 28 August 1997, n. 281, on the document containing "National guidelines for the provision of telemedicine services". Directory of documents No. 215/CSR of 17 December (2020)).
- National Telemedicine Guidelines - Ministry of Health.
- In addition to what is indicated in various publications of the Istituto Superiore della Sanità (ISS) such as: Ad interim indications for telemedicine assistance services during the COVID-19 health emergency - ISS COVID-19 Report (2020).
- DECREE 21 September 2022 Approval of guidelines for telemedicine services - Functional requirements and service levels. (22A06184) (GU General Series n.256 of 02-11-2022)
- DECREE 23 May 2022 n. 77 of the Ministry of Health with particular reference to Annex 1 - point 15 (Telemedicine) and point 16 (Information and quality systems).
- Bossa F, Valvano MR, Vetrone LM, Guerra M, Lopetuso LR, Carparelli S, Mignini I, Cocomazzi F, Napolitano D, Costantino A, Caprioli F, Gasbarrini A, Perri F, Papa A. Evaluation of factors associated with trust in telemedicine in patients with inflammatory bowel disease during COVID-19 pandemic: a multicenter cross-sectional survey. Eur Rev Med Pharmacol Sci 19 (2022): 7277-7284.
- The national recovery and resilience plan (PNRR), financed with the funds allocated by the Next Generation EU, a sort of post-pandemic Marshall Plan, dedicates its attention to health care in point 6 (called mission 6). The main purpose of the National Recovery and Resilience Plan is to secure the health system and to "respond to the vulnerabilities that emerged during the pandemic emergency but also to resolve pre-existing critical issues through the strengthening of infrastructures and the digitization of health services Of the 18.51 billion euros provided for by the PNRR and the Complementary Fund in Mission 6, no less than 16.53 billion euros (89.3%) can be territorialized, testifying to the central role of the Regions in the process of strengthening prevention and health services, their modernization and digitization" See Meridiano Sanità.
- Programma di formazione manageriale per la dirigenza del sistema sanitario – corso di fomrazione managenriale per dirigienti sanitari incaricati della direzione di struttura complessa di aziende ed enti del servisio sanitario della Regione Puglia – Anno 2022 - Project work - Interazione Ospedale-Territorio nella gestione della fase post-acuta o cronica dei pazienti. Una gestione condivisa alla luce del DM 77 e dei fondi del PNRR. (see page 7).
- Lang, Achim & Mertes, Alexander. E-Health Policy and Deployment Activities in Europe. Telemedicine journal and e-health: the official journal of the American Telemedicine Association 17 (2011): 262-8.
- Grigsby J, Rigby M, Hiemstra A, House M, Olsson S, Whitten P. Chapter 7: The diffusion of telemedicine. Telemed J E Health 8 (2002): 79–94.
- Schmeida M, McNeal R, Mossberger K. Policy determinants affect telehealth implementation. Telemed J E Health 13 (2007): 100–107.
- May C, Harrison R, Finch T, MacFarlane A, Mair F, Wallace P. Telemedicine Adoption Study Group. Understanding the normalization of telemedicine services through qualitative evaluation. J Am Med Inform Assoc 10 (2003): 596-604.
- Ishfaq R. and Raja U. Bridging the Healthcare Access Divide: A Strategic Planning Model for Rural Telemedicine Network. Decision Sciences 46 (2015): 755-790.
- Delivering quality health services: a global imperative for universal health coverage. Geneva: World Health Organization, Organisation for Economic Co-operation and Development, and The World Bank (2018).
- Ng M, Fullman N, Dieleman JL, Flaxman AD, Murray CJ, Lim SS. Effective coverage: a metric for monitoring Universal Health Coverage. PLoS Med 11 (2014): e1001730.
- Salisbury C, Thomas C, O’Cathain A, et al. Telehealth in Chronic disease: mixed-methods study to develop the TECH conceptual model for intervention design and evaluation. BMJ Open 5 (2015): e006448.
- Tanahashi T. Health service coverage and its evaluation. Bulletin of the World Health Organization56 (1978): 295 - 303.


 Impact Factor: * 3.0
Impact Factor: * 3.0 Acceptance Rate: 76.32%
Acceptance Rate: 76.32%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
