Macular Thickness Variation after Conventional and Short-Pulse Laser Treatment in Diabetic Patient by Optical Coherence Tomography
Golam Faruk Hossain1*, Joly Yeasmin2, Tariq Reza Ali3, Tajmeh Mehtaj4
1Assistant Professor, Department of Community Ophthalmology, Bangabandhu Sheikh Mujib Medical University
2Resident, Phase-B, Department of Ophthalmology, Bangabandhu Sheikh Mujib Medical University
3Associate Professor, Department of Ophthalmology, Bangabandhu Sheikh Mujib Medical University
4Assistant Professor, Department of Community Ophthalmology, Bangabandhu Sheikh Mujib Medical University
*Corresponding author: Golam Faruk Hossain, Assistant Professor, Department of Community Ophthalmology, Bangabandhu Sheikh Mujib Medical University.
Received: 26 December 2024; Accepted: 31 December 2024; Published: 15 January 2025;
Article Information
Citation: Golam Faruk Hossain, Joly Yeasmin, Tariq Reza Ali, Tajmeh Mehtaj. Macular Thickness Variation after Conventional and Short-Pulse Laser Treatment in Diabetic Patient by Optical Coherence Tomography. Journal of Ophthalmology and Research. 8 (2025): 01-05.
DOI: 10.26502/fjor.2644-00240098
View / Download Pdf Share at FacebookAbstract
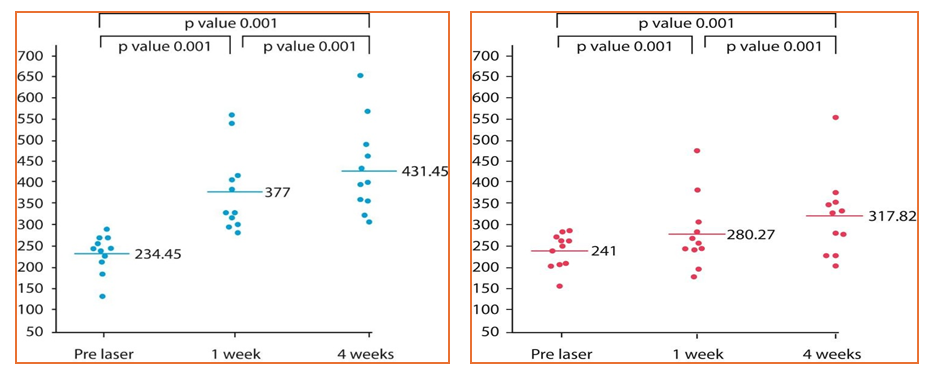
Background: Diabetic retinopathy is a leading cause of blindness, and this study evaluates the comparative impact of conventional and short pulse laser photocoagulation on macular thickness in PDR patients to optimize treatment outcomes. Aim: The aim of this study was to evaluate changes in macular thickness in patients with PDR treated with conventional single-spot laser photocoagulation versus short pulse laser photocoagulation, using Optical Coherence Tomography (OCT) measurements at baseline, 1 week, and 4 weeks post-treatment. Methodology: This prospective longitudinal study was conducted at Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka from July 2023-June 2024, total 22 PDR patients was selected by using consecutive sampling (11 eyes per group). Group I underwent single-spot laser photocoagulation in one session, and Group II received short pulse laser photocoagulation in two sessions. Inclusion criteria included PDR without macular edema (central thickness <300 \u00b5m) and diabetes mellitus, while exclusion criteria ruled out significant ocular comorbidities. Macular thickness was assessed using OCT before treatment and at 1- and 4-weeks post-treatment. All procedures were standardized, performed by a single surgeon, and data were analyzed with Statistical Package for the Social Sciences (SPSS) version 26. Result: The results showed significant increases in macular thickness in both groups, with the conventional laser group demonstrating a rise from 234.45 ± 44.91 μm pre-laser to 431.45 ± 104.12 μm at 4 weeks, and the short pulse laser group increasing from 241 ± 39.68 μm to 317.82 ± 94.82 μm. Statistically significant changes were observed at both 1-week and 4-week time points in both groups p=0.001. The study also highlighted differences in laser parameters, with the short pulse laser group using higher power, shorter pulse duration, and more spots compared to the conventional laser group. Both treatments demonstrated effectiveness in altering macular structure, with short pulse laser showing greater precision and efficiency. Conclusion: Both conventional and short pulse laser photocoagulation significantly increased macular thickness, with the short pulse laser showing greater efficacy. These results suggest that short pulse laser may offer a more efficient treatment for PDR.
Keywords
<p>Macular thickness, Diabetic retinopathy, Conventional laser, Short pulse laser, Optical coherence tomography.</p>
Article Details
1. Introduction
PDR is a severe form of diabetic retinopathy that causes abnormal blood vessel growth in the retina. Macular thickness is a measure of the thickness of the macula, the central part of the retina responsible for sharp, central vision. PDR is a severe vision-threatening complication of diabetes mellitus, characterized by the abnormal growth of blood vessels in the retina. These fragile vessels are prone to bleeding and can lead to complications such as vitreous hemorrhage, tractional retinal detachment, and ultimately blindness if untreated [1]. PDR is a significant contributor to visual impairment worldwide, particularly in regions with a high prevalence of diabetes, emphasizing the urgent need for effective treatment strategies [2].
Panretinal photocoagulation (PRP) has long been the standard treatment for PDR. It works by inducing regression of neovascularization, thereby reducing the risk of severe vision loss. However, conventional PRP often results in side effects such as peripheral vision loss, macular edema, and post-treatment inflammation, which may impact the patient’s quality of life. In recent years, advancements in laser technologies, including the Pascal (Pattern Scanning Laser) system and short-pulse lasers, have shown promise in addressing these limitations.
Emerging evidence suggests that these newer laser modalities can reduce central macular thickness (CMT), preserve visual acuity (VA), and lower the risk of inflammation compared to traditional lasers. Studies have demonstrated their ability to deliver effective treatment with fewer complications and enhanced patient comfort [3].
Diabetes mellitus is a leading cause of eye-related complications in our country. With its rising prevalence, reaching 9.2% in 2022, these ocular conditions are poised to become an even greater global health threat in the near future than they are today [4]. Diabetes mellitus can lead to a range of pathological effects on the eye, ranging from index myopia, early-onset cataracts, and mild or background diabetic retinopathy to more severe conditions such as PDR or advanced diabetic eye disease, including vitreous hemorrhage or tractional retinal detachment [5]. PDR is one of the leading causes of blindness and visual loss. Panretinal Photocoagulation (PRP) reduces the risk of severe vision loss in PDR. Good visual acuity results can improve vision-related quality of life [6].
Neovascular AMD requiring frequent anti-VEGF treatment to achieve adequate suppression of choroidal neovascular activity and exudation is a common clinical scenario; suboptimal disease control can limit vision gains and contribute to vision loss over time [7].
Retinal laser photocoagulation is recognized as a standard treatment of PDR [8].
Laser light is absorbed by the retinal pigment epithelium, converting into thermal energy. This heat denatures retinal proteins, leading to cellular death and coagulative necrosis [9]. The ischemic retina is destroyed, reducing VEGF levels and subsequent neovascularization [10].
This study aims to evaluate the changes in macular thickness in patients with PDR treated with conventional single-spot laser photocoagulation versus short pulse laser photocoagulation, using OCT.
2. Methodology
This prospective longitudinal study was conducted at the Department of Ophthalmology and Community Ophthalmology, BSMMU, Dhaka, from July 2023 to June 2024. Patients diagnosed with PDR were recruited using consecutive sampling, with a calculated sample size of 11 eyes per group based on Julious’s formula. Group I received conventional single-spot laser photocoagulation in one session, and Group II underwent short pulse laser photocoagulation in two sessions. Inclusion criteria included PDR without macular edema and central macular thickness <300 µm, with type 1 or type 2 diabetes mellitus, while exclusion criteria were clinically significant macular edema, central macular thickness >300 µm, uveitis, corneal opacity, vitreous hemorrhage, epiretinal membrane, vitreomacular tension, and tractional retinal detachment. Complete clinical evaluations were performed, including history, ocular assessments (BCVA, pupillary reaction, slit-lamp examination, intraocular pressure measurement, and fundus examination). Laser procedures were conducted using a NIDEK GYC-500 laser machine and Mainstem pan fundoscopic contact lens under standardized conditions, with macular thickness measured by OCT (NIDEK RS-330) before treatment and at 1 week and 4 weeks post-treatment. Ethical clearances and written consent taken from each patient properly. All procedures were performed by a single surgeon to ensure consistency, and data on patient history, examination findings, and investigations were recorded in a structured pre-tested format. Data were analyzed using SPSS version 26. Continuous variables were shown as mean and standard deviation. Categorical variables were presented as frequency and percentage. Paired t test were applied to assess changes in macular thickness over time after conventional and short pulse laser photocoagulation.
3. Results
The study included participants from two treatment groups: conventional laser and short pulse laser. In the conventional laser group, the majority of participants, 54.5% were aged 51–60 years, while only 9.1% of participants in the short pulse laser group were in this age range. The mean age of participants in the conventional laser group was 48.64 ± 5.61 years, whereas the short pulse laser group had a slightly higher mean age of 51 ± 12.02 years. Baseline characteristics were comparable between the groups, with 63.6% male and 36.4% female participants in both groups. Treatment was administered to the right eye in 54.5% of cases in the conventional laser group and 45.5% in the short pulse laser group, while the left eye was treated in 45.5% and 54.5% of cases in the conventional and short pulse laser groups, respectively.
The comparison of laser parameters between the two groups revealed distinct differences. During the first session, the mean power in the short pulse laser group was significantly higher 662.73 ± 163.96 mW compared to the conventional laser group 321.82 ± 61.94 mW. The pulse duration was shorter in the short pulse laser group 0.03 ± 0.01 ms than in the conventional laser group 0.35 ± 0.05 ms. Additionally, the average number of laser spots was greater in the short pulse laser group, while the spot size was smaller. Notably, only the conventional laser group required a second session, during which the parameters remained consistent with those of the first session.
MT over time, assessed through OCT, showed significant increases in both groups. In the conventional laser group, the mean MT rose from 234.45 ± 44.91 µm pre-laser to 377 ± 95.75 µm at 1 week and 431.45 ± 104.12 µm at 4 weeks. The differences were statistically significant between pre-laser and 1 week p=0.001 and between 1 week and 4 weeks p=0.001. Similarly, in the short pulse laser group, the mean MT increased from 241 ± 39.68 µm pre-laser to 280.27 ± 82.1 µm at 1 week and 317.82 ± 94.82 µm at 4 weeks, with significant differences observed between pre-laser and 1 week p=0.001 and between 1 week and 4 weeks p=0.001. These findings demonstrate that both conventional and short pulse laser photocoagulation effectively induce changes in macular thickness over time. However, the short pulse laser group required higher power, shorter pulse duration, and more laser spots, suggesting it may offer a more precise and efficient approach to treating proliferative diabetic retinopathy.
Table 1: Distribution of the study patients by age (in years)
|
Age in Year |
Conventional laser |
Short pulse laser |
|
≤40 |
18.20% |
27.30% |
|
41-50 |
27.30% |
36.30% |
|
51-60 |
54.50% |
9.10% |
|
61-70 |
0% |
27.30% |
|
Mean Age |
48.64 ± 5.61 |
51 ± 12.02 |
Table 1 shows in the conventional laser group, more than half of the participants (54.5%) were aged 51–60 years, whereas in the short pulse laser group, only 9.1% fell within this age range. The mean age of participants in the conventional laser group was 48.64 ± 5.61 years, compared to 51 ± 12.02 years in the short pulse laser group.
Table 2: Baseline characteristics at the time of registration (n=22)
|
Baseline characteristics |
Conventional laser (n=11) |
Short pulse laser (n=11) |
||
|
N |
% |
N |
% |
|
|
Gender |
||||
|
Male |
7 |
63.6 |
7 |
63.6 |
|
Female |
4 |
36.4 |
4 |
36.4 |
|
Eye |
||||
|
Left eye |
5 |
45.5 |
6 |
54.5 |
|
Right eye |
6 |
54.5 |
5 |
45.5 |
Table 2 demonstrate the baseline characteristics were comparable between the groups. Both conventional and short pulse laser groups had 63.6% male and 36.4% female participants. Treatment was administered to the right eye in 54.5% and 45.5% of cases and to the left eye in 45.5% and 54.5% of cases in the conventional and short pulse laser groups, respectively.
Table 3: Comparison of Laser Parameters Between Conventional and Short Pulse Laser Photocoagulation (n=22)
|
Conventional laser |
Short pulse laser |
|
|
(n=11) |
(n=11) |
|
|
Mean±SD |
Mean±SD |
|
|
1st session |
||
|
Power (mW) |
321.82±61.94 |
662.73±163.96 |
|
Range(min-max) |
250-490 |
490-950 |
|
Pulse duration (ms) |
0.35±0.05 |
0.03±0.01 |
|
Range(min-max) |
0.3-0.4 |
0.02-0.03 |
|
Number of spots |
1272.7±119.09 |
2593.8±527.58 |
|
Range(min-max) |
1000-1400 |
2000-3800 |
|
Spot size (nm) |
167.27±31.33 |
131.82±17.22 |
|
Range(min-max) |
140-200 |
100-150 |
|
2nd session |
||
|
Power (mW) |
317.27±34.38 |
- |
|
Range(min-max) |
250-350 |
- |
|
Pulse duration (ms) |
0.35±0.05 |
- |
|
Range(min-max) |
0.3-0.4 |
- |
|
Number of spots |
1236.4±112.01 |
- |
|
Range(min-max) |
1000-1400 |
- |
|
Spot size (nm) |
167.27±31.33 |
- |
|
Range(min-max) |
140-200 |
- |
Table 3 compares laser parameters between conventional and short pulse laser photocoagulation. The mean power for the first session was 321.82 ± 61.94 mW in the conventional laser group and 662.73 ± 163.96 mW in the short pulse laser group. Pulse duration was 0.35 ± 0.05 ms and 0.03 ± 0.01 ms, respectively. The average number of spots was 1272.7 ± 119.09 for conventional lasers and 2593.8 ± 527.58 for short pulse lasers, with spot sizes of 167.27 ± 31.33 nm and 131.82 ± 17.22 nm, respectively. For the second session, only the conventional laser group underwent treatment, with a mean power of 317.27 ± 34.38 mW, pulse duration of 0.35 ± 0.05 ms, 1236.4 ± 112.01 spots, and spot size of 167.27 ± 31.33 nm. The short pulse laser group did not require a second session.
Figure 1 illustrates the changes in MT assessed by OCT in patients treated with conventional laser photocoagulation (left panel) and short pulse laser photocoagulation (right panel) at three time points: pre-laser, 1-week post-laser, and 4 weeks post-laser. In the conventional laser group, the mean MT was 234.45±44.91 µm pre-laser, 377±95.75 µm at 1 week, and 431.45±104.12 µm at 4 weeks. Significant increases in MT were observed between pre-laser vs. 1 week p=0.001 and 1 week vs. 4 weeks p=0. 001.In the short pulse laser group, the mean MT was 241±39.68 µm pre-laser, 280.27±82.1 µm at 1 week, and 317.82±94.82 µm at 4 weeks. Similarly, significant changes were noted between pre-laser vs. 1 week p=0.001 and 1 week vs. 4 weeks p=0.001.
4. Discussion
This study investigated the changes in macular thickness following conventional and short pulse laser in Bangladeshi patients. Both treatment groups experienced a significant increase in MT at one- and four-weeks post-treatment, as measured by OCT. However, the short pulse laser group required higher power, shorter pulse duration, and a greater number of laser spots compared to the conventional laser group.
The observed increase in MT following laser treatment is consistent with previous studies [11, 13]. This initial rise is likely due to a combination of factors, including post-laser inflammation and retinal edema. These findings suggest that both conventional and short pulse laser photocoagulation can effectively induce changes in macular thickness over time.
Interestingly, the short pulse laser group required a different treatment approach compared to the conventional laser group. The higher power, shorter pulse duration, and increased number of laser spots suggest a more targeted and potentially less damaging approach for the short pulse laser. This is supported by prior research which suggests that short pulse lasers may cause less inflammation and macular thickening compared to conventional lasers [12].
Future studies with larger sample sizes are needed to confirm these findings in a Bangladeshi context. Additionally, studies comparing the long-term effects of conventional and short pulse laser therapy on visual acuity and macular thickness in this population would be valuable.
5. Conclusion
This study evaluated the changes in macular thickness in patients treated with conventional single-spot laser photocoagulation versus short pulse laser photocoagulation, utilizing OCT. Both treatment modalities resulted in significant increases in macular thickness over time, with the conventional laser group showing greater increases compared to the short pulse laser group. The findings suggest that short pulse laser photocoagulation, with its higher power, shorter pulse duration, and more laser spots, may offer a more precise and efficient treatment approach, potentially reducing the risk of complications and improving patient outcomes. However, further studies with larger sample sizes and longer follow-up periods are needed to confirm these findings and evaluate the long-term effects of these two laser treatments on retinal health in diabetic patients.
Declaration of Interest Statement:
The authors report no conflict of interest.
Data availability statement:
The data that support the findings of this study are available from the corresponding author
Funding:
There were no sources of funding or financial support for this project.
Contributions:
Dr. Md. Golam Faruk Hossain conceptualized and designed the study, supervised data collection, and contributed to the manuscript drafting. Dr. Md. Golam Faruk Hossain was responsible for data collection and analysis, providing valuable insights on the interpretation of the findings. Mst. Joly Yeasmin, Dr. Tariq Reza Ali contributed to the literature review and helped in the methodology design, ensuring the study adhered to ethical standards and Dr. Tajmeh Mehtaj provided statistical support, contributed to data analysis, and reviewed the manuscript critically for important intellectual content. All authors approved the final manuscript for publication.
References
- Panchapakesan A. Numerical analysis on impedance characteristics of dual wavelength quantum cascade lasers. J Optical Commun 14 (2024).
- Ogle GD, James S, Dabelea D, et al. Global estimates of incidence of type 1 diabetes in children and adolescents: Results from the International Diabetes Federation Atlas. Diabetes Res Clin Pract 183 (2022): 109083.
- Jain A, Blumenkranz MS, Paulus Y, Wiltberger MW, et al. Effect of pulse duration on size and character of the lesion in retinal photocoagulation. Arch Ophthalmol 126 (2008): 78-85.
- Nentwich MM, Ulbig MW. Diabetic retinopathy-ocular complications of diabetes mellitus. World J Diabetes 6 (2015): 489.
- Solomon SD, Chew E, Duh EJ, et al. Diabetic retinopathy: a position statement by the American Diabetes Association. Diabetes Care 40 (2017): 412.
- Caesarita DP, Wildan A, Kurniawan AH, et al. The Effect of Panretinal Photocoagulation Treatment on Vision-Related Quality of Life of Patients with Proliferative Diabetic Retinopathy at Kariadi Hospital. Ophthalmologica Indonesiana 48 (2022): 41-47.
- Pandit SA, Momenaei, Wakabayashi T, et al. Clinical Outcomes of Faricimab in Patients with Previously Treated Neovascular Age-Related Macular Degeneration, Ophthalmol Retina 8 (2024): 360-366.
- Takamura Y, Arimura S, Miyake S, et al. Panretinal photocoagulation using short-pulse laser induces less inflammation and macular thickening in patients with diabetic retinopathy. J Ophthalmol 2017 (2017): 8530261.
- Hassanpoor N, Ahoor M, Latifi A, et al. Conventional and pattern scanning pan-retinal photocoagulation laser in diabetic patients’ visual field. J Lasers Med Sci 13 (2022).
- Solomon SD, Chew E, Duh EJ, et al. Diabetic retinopathy: a position statement by the American Diabetes Association. Diabetes Care 40 (2017): 412.
- Soman M, Ganekal S, Nair U, et al. Effect of panretinal photocoagulation on macular morphology and thickness in eyes with proliferative diabetic retinopathy without clinically significant macular edema. Clin Ophthalmol 10 (2022): 2013-2017.
- Takamura Y, Arimura S, Miyake S, et al. Panretinal photocoagulation using short-pulse laser induces less inflammation and macular thickening in patients with diabetic retinopathy. J Ophthalmol 1 (2017): 8530261.
- Watanachai N, Choovuthayakorn J, Patikulsila D, et al. Changes in central macular thickness following single session multispot panretinal photocoagulation. J Ophthalmol 1 (2015): 529529.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
