Noninvasive Ultrasound Assessment of the Normal Optic Nerve Sheath Diameter in Healthy Adults: an Islamabad-based Pakistani Population Study
Rubia Ahmada, Aeisha Begumb, Salma Umbreenb*, Ahsen Farooqc, Rabia Waseem Buttd, Kalsoom Basitd
aRadiology Department, Izzat Ali Shah Hospital, Wah Cantonment, Pakistan
bRadiology Department, Wah Medical College, Wah Cantonment, Pakistan
cRadiology Department, IIMC-PRH/Riphah International University, Rawalpindi, Pakistan
dRadiology Department, HITEC-IMS, Taxila, Pakistan
*Corresponding Author: Salma Umbreen, Radiology Department, Wah Medical College, Wah Cantonment, Pakistan
Received: 07 November 2020; Accepted: 21 November 2020; Published: 24 November 2020
Article Information
Citation: Rubia Ahmad, Aeisha Begum, Salma Umbreen, Ahsen Farooq, Rabia Waseem Butt, Kalsoom Basit. Noninvasive Ultrasound Assessment of the Normal Optic Nerve Sheath Diameter in Healthy Adults: an Islamabad-based Pakistani Population Study. Journal of Ophthalmology and Research 3 (2020): 86-95.
DOI: 10.26502/fjor.2644-00240027
View / Download Pdf Share at FacebookAbstract
Abstract
Aim: The noninvasive B-mode transocular ultrasound (TOU) measurement of the optic nerve sheath diameter (ONSD) is becoming popular to monitor intracranial pressure (ICP). Different studies report varied values for normal ONSD. Our primary aim was to find the TOU-measured normal ONSD in healthy adult Pakistanis living in Islamabad Capital Territory (ICT).
Methodology: One hundred healthy adult volunteers participated in this cross-sectional study, conducted at the Pakistan Atomic Energy Commission (P.A.E.C.) General Hospital, Islamabad. Each eye was scanned for the optic nerve (ON) via TOU using a B-mode 7-15 MHz linear probe. The investigators measured ONSD in a transverse plane three millimeters behind the retina. They recorded an average of three readings as a mean ONSD value for both eyes.
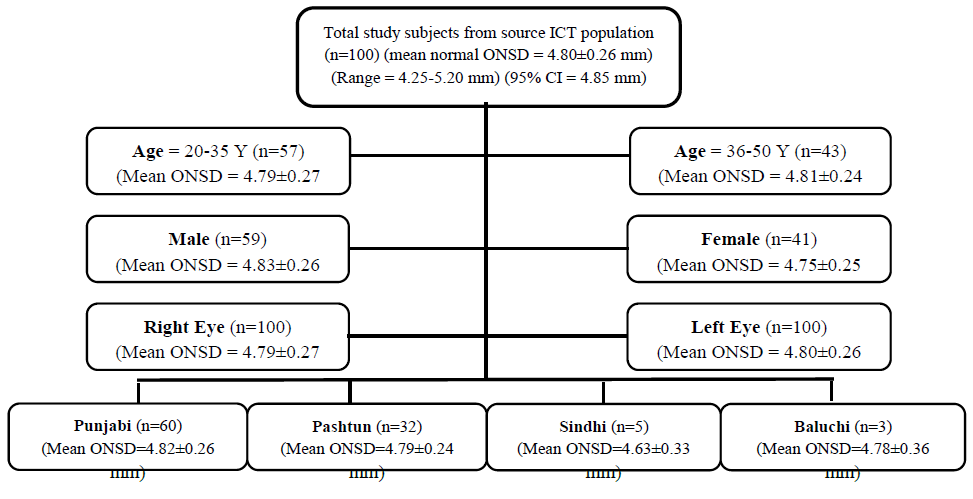
Results: The overall normal mean ONSD was 4.80±0.26 mm with a minimum of 4.25 mm and a maximum of 5.20 mm. The mean ONSD for the age group of 20-35 years was 4.79±0.27 mm and for 36-50 years, it was 4.81±0.24 mm (p = 0.7952), for the male eye it was 4.83±0.26 mm and for the female eye was 4.75±0.25 mm (p = 0.1238), and for the right eye was 4.79±0.27 mm and for the left eye was 4.80±0.26 mm with (p = 0.2434) and (r = 0.9455). There was no statistically significant difference in the mean ONSD of the four ethnic groups (p = 0.7141).
Conclusion: The normal mean optic nerve sheath diameter in the studied healthy adult Pakistanis, as measured through noninvasive B-mode transorbital ultrasound is 4.80±0.26 mm.
Keywords
<p>B-Mode TOU; Transocular Ultrasound; Transorbital Ultrasound; Point-of-Care Ultrasound (POCUS); Optic Nerve Sheath Diameter (ONSD); Intracranial Pressure (ICP); Intracranial Hypertension (ICH)</p>
Article Details
1. Introduction
Intracranial hypertension (ICH) is a critical complication of many neurologic and non-neurologic conditions [1]. It demands a thorough evaluation, and with early detection, continuous monitoring, and appropriate management, we can alleviate the grave consequences of secondary brain injury [1]. There are several methods, invasive and noninvasive, to assess ICP [2-5]. The gold standard is direct intraventricular ICP monitoring using an extra-ventricular drain (EVD) through a burr hole [1-5]. However, there is increasing popularity of ultrasonography being a noninvasive, low-cost, easily available, and quick imaging modality for assessing ICP indirectly via transcranial Doppler (TCD), and via B-mode transocular (or transorbital) ultrasound (TOU) [3-7]. One can perform point-of-care ultrasound (POCUS) wherever a patient is under treatment [7-10].
Literature supplies a detailed account of techniques, clinical applications, and limitations of the B-mode TOU of ONSD [4-10,11-21]. Overall, there is satisfactory reliability of the B-mode TOU to measure the ONSD [16]. Several human studies from different parts of the world report a significant correlation between the ONSD and ICP [7,8,17]. However, there is no established consensus among these studies for a normal mean ONSD, and also for an optimal upper limit of the normal [7,8,17,18]. The reasons for the varied values of TOU-measured reportedly normal ONSD and cut-off values might be attributed to equipment, technique, patients’ gender, age, ethnicity, and right or left eye [7,8,17,22]. Therefore, a knowledge of the range and mean normal human ONSD would help in finding the reliable standard reference values and delimiting an optimal cut-off value for indicating a rise in ICP and saving the patients from complications ICH.
There is a good deal of world literature on different aspects of TOU-measured ONSD, however, there are fewer studies from our country Pakistan [12,23-27]. Asghar et al. and Rehman et al. have reported measurements of ONSD in healthy subjects, but without consideration of local major ethnic groups [12,23]. The current single-center hospital-based cross-sectional study reckons the patients’ age, gender, ethnicity, and right or left eye while recording the observations. The primary objective of this study was to find the TOU-measured range and the mean normal ONSD in healthy adults in a diverse section of the local Pakistani population living in the ICT. The secondary outcome gained was an expected upper limit which could probably predict a rise in ICP to save the patient from the grave consequences of ICH.
2. Participants and Methodology
This was a single-center cross-sectional study, conducted in the Radiology Department of the tertiary-care P.A.E.C. General Hospital, Islamabad from 1st April 2017 to 30th August 2017.The Hospital Ethical Committee approved the study proposal and investigators adhered to the World Medical Association Declaration of Helsinki. An earlier Pakistani study found normal ultrasound measured ONSD in 100 healthy volunteers, but without forming age or ethnic groups [13]. Therefore, the current study also targeted one hundred healthy adult Pakistani volunteers to make a closer comparison.
2.1. Sampling and sample
Investigators used consecutive non-probability sampling with the 95% confidence interval and a standard deviation of 0.30. A strictly precise sample size calculation was not easy as it was difficult to estimate age, gender, and ethnicity related variations for ONSD in the Pakistani population. The 100 participants belonged to the four major ethnic groups (Punjabi, Sindhi, Pashtun, and Baluchi) of the Pakistani population living in the ICT. All the participants signed an informed written consent after getting an explanation about the study. The sample included hospital staff, attendants/relatives of patients. The investigators acquired a detailed history. The participants underwent a thorough medical, neurological, and ophthalmological assessment. The study excluded individuals with comorbidities such as hypertension, diabetes, malignancy, neurological or ophthalmological problems, and a previous episode of head and/or ocular trauma. It also excluded individuals with a history of acute medical illness in the past month, requiring hospital admission. The participants were divided into separate groups to correlate and compare the possible differences among them. There were two groups by age, two by gender, four groups by ethnicity, and two by the right and the left eye, as presented in the table1.
2.2 Imaging and measurement for ONSD
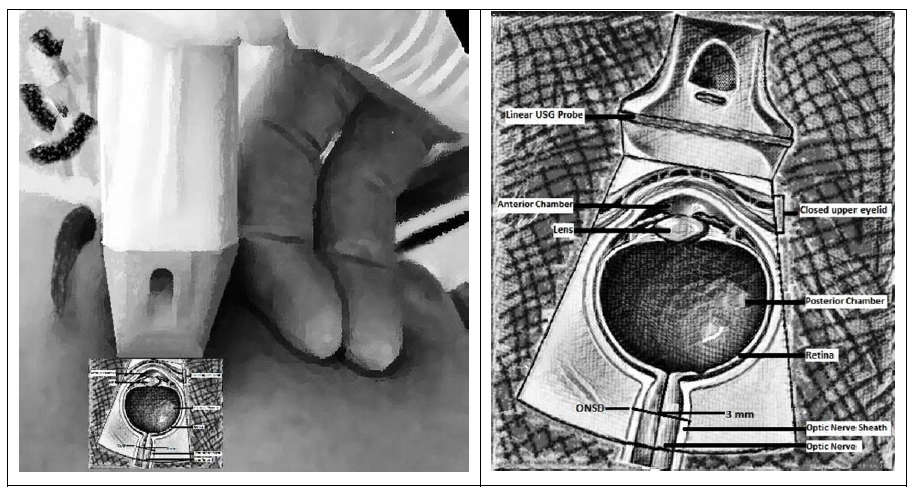
Earlier studies have explained the TOUscanning and ONSD measuring techniques and their limitationsin sufficient detail[4-15]. For this study, an investigator with less than five years of experience in radiology performed the transorbital ultrasound on GE Logiq S8 (General Electric Medical Systems, Milwaukee, WI, USA) machine using a high-resolution multi-frequency 7-15 MHz linear-array transducer. The subjects were lying relaxed, supine, and eyes closed but “looking straight” in a neutral position. The operator applied the gel and gently placed the ultrasound probe in the parasagittal and transverse planes on the temporal aspect of the closed upper eyelid with a suitable angulation orienting the ultrasound beam to image the linear hypoechoic optic nerve behind the eyeball. The operator then measured ONSD in a transverse plane as the distance between the external margins of the hyperechoic borders 3 mm behind and perpendicular to the axis of the retina at the point of entry of the optic nerve into the globe using electronic calipers in the frozen image. Figure 1 illuminates the imaging method. The operator took three values for ONSD from each eye and recorded an average of three readings as an outcome for each participant. A radiologist with more than ten years of experience supervised the examination and measurement process.
2.3 Statistical analysis
The Statistical Package for Social Sciences (SPSS) version 20.0 (IBM Corporation, New York, USA) was deployed for data analysis. The basic descriptive statistics like minimum, max, mean ± SD (standard deviation), median and quartiles, and 95% percentile for variables, i.e., age and ONSD of all volunteers were calculated. The frequencies for categorical variables, i.e., gender, age groups, and ethnicity were computed. The paired t-test compared the ONSD of the right and left eyes. An independent sample t-test compared the ONSD between two age groups and genders, but the authors applied ANOVA to compare ONSD among different ethnic groups. The tables were prepared for ONSD considering age, gender, ethnicity, and side of measurement. The p-value of < 0.05 was statistically significant. The authors have adoptedtheStrengthening the Reporting of Observational Studies in Epidemiology (STROBE)checklist to report their research [28].
3. Results
One hundred healthy adult volunteers Pakistanis living in ICT were studied. The mean age of the sample was 34.2±8.79 years with a minimum and maximum age of 20 and 50 years respectively. Males (59%) and Punjabis (60%) were in the majority.Sindhi (5%) and Baluchi (3%) subjects were in a lesser number. A bigger sampling error is likely to occur when we acquire data from a smaller sample. However, there was no statistically significant difference in mean ONSD among diverse groups. This was depicted by P-values, for the age (p = 0.7952), gender (p = 0.1238), ethnic groups (p = 0.7141), and between the right and left eye (p = 0.2434). The table1 shows the comparison of ONSD according to demographics and side of measurement. Table 2 illustrates the descriptive statistics and analysis of age and right and left eye ONSD.
Table 1: Mean ONSD in age, gender, ethnicity, and side of measurement groups
|
Subjects |
Mean ONSD |
Standard Deviation |
P-value |
|
Age Group 1 (20-35 years) (n=57) |
4.79 |
0.27 |
0.7952 |
|
Age Group 2 (36-50 years) (n=43) |
4.81 |
0.24 |
|
|
Males (n=59) |
4.83 |
0.26 |
0.1238 |
|
Females (n=41) |
4.75 |
0.25 |
|
|
Punjabis (n=60) |
4.82 |
0.26 |
0.7141 |
|
Pashtuns (n=32) |
4.79 |
0.24 |
|
|
Sindhis (n=5) |
4.63 |
0.33 |
|
|
Baluchis (n=3) |
4.78 |
0.36 |
|
|
Left Eye (n=100) |
4.80 |
0.26 |
0.2434 |
|
Right Eye (n=100) |
4.79 |
0.27 |
Table 2: Descriptive statistics of age, and left and right eye ONSD
|
Descriptive Statistics |
Age in years |
ONSD in millimeters (mm) |
|||
|
Left |
Right |
Average |
|||
|
Minimum |
20.0 |
4.10 |
4.40 |
4.25 |
|
|
Mean |
34.2 |
4.80 |
4.79 |
4.80 |
|
|
Maximum |
50.0 |
5.20 |
5.20 |
5.20 |
|
|
Range |
30.0 |
1.10 |
0.80 |
0.95 |
|
|
Standard Deviation (SD) |
8.79 |
0.26 |
0.27 |
0.26 |
|
|
Standard Error (SE) |
0.879 |
0.026 |
0.027 |
0.029 |
|
|
Quartile 1 |
27.0 |
4.60 |
4.60 |
4.6 |
|
|
Median |
34.0 |
4.80 |
4.70 |
4.775 |
|
|
Quartile 3 |
42.0 |
5.00 |
5.00 |
5.1 |
|
|
Interquartile Range |
15.0 |
0.40 |
0.40 |
0.45 |
|
|
CI (95%) |
Lower L |
32.7 |
4.75 |
4.74 |
4.75 |
|
Upper L |
36.0 |
4.85 |
4.85 |
4.85 |
|
|
CI (99%) |
Lower L |
31.9 |
4.73 |
4.72 |
4.73 |
|
Upper L |
36.5 |
4.87 |
4.86 |
4.87 |
|
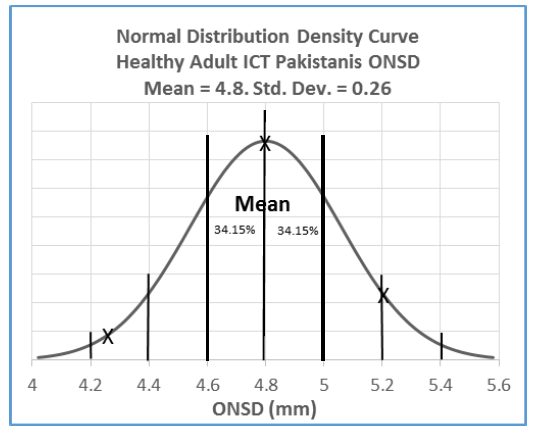
Figure 2 shows a bell-shaped unimodal curve with the symmetric distribution of ONSD data values acquired from healthy adult Pakistanis living in ICT, clustered on either side of the mean
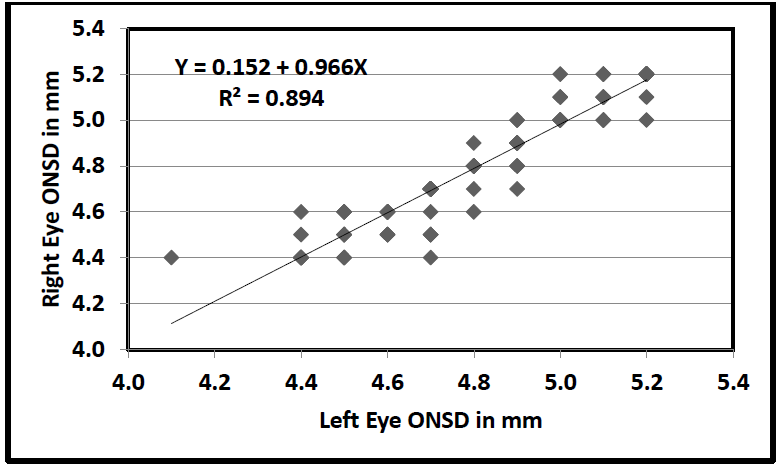
Figure 3 shows that the readings from both eyes were statistically almost the same as shown by the linear trend. The linear regression model had an R2 of 0.894, which means the model was explaining 89.4% of the variation in the dependent variable. There was a high correlation between the ONSD readings from both eyes(r =0.9455). The paired t-test showed comparable results of insignificant statistical differences bilaterally. Therefore, the authors recorded an average ONSD reading from both eyes.
In the current study, the overall normal mean ONSD was 4.80±0.26 mm with a minimum of 4.25 mm and a maximum of 5.20 mm. There was no statistically significant difference in the mean ONSD among diverse groups. The data values were evenly distributed around the mean. The 95% confidence interval (CI) was between 4.7 mm to 4.85 mm. As the estimated upper limit of 95% CI was 4.85 mm, ultrasound measurements of ONSD above this limit lead to the 95% probability of ONSD being abnormal. The estimated upper limit of 99% CI was 4.87 mm, and ultrasound measurements of ONSD above this limit lead to the 99% probability of ONSD being abnormal. Therefore, further investigations into the effects of raised intracranial pressure should be recommended to patients with suspicion of ICH having the ONSD measuring above confidence intervals. Figure 3 shows a summary of the study, according to the STROBE statement checklist.
4. Discussion
As already described, there is no convincing agreement among the researchers, both outside and within Pakistan, for a normal mean ONSD, and also for the best possible upper limit of the normal ONSD which can indicate a rise in ICP and predict ICH confidently.The authors have primarily found the range and the mean normal ONSD in 100 healthy adults from a section of the Pakistani population comprising the four major ethnic groups living in the ICT. The secondary outcome of the study was an expected upper limit of ONSD. The Sindhi and Baluchi subjects were less. A bigger sampling error is likely to occur when we acquire data from a smaller sample. However, the findings were generally independent of age, gender, ethnicity, and left or right eye. The results of the current study show an overall mean normal ONSD of 4.80±0.26 mm with a range of 4.25 to 5.20 mm. The expected upper limit of 4.85 mm can possibly predict raised ICP in the Pakistanis. Therefore, any measurement above this level warrants other investigations for patients suspected of ICH.
Schroeder et al. [17] carried out a systematic review and meta-analysis of (final) 39 studies with cumulatively 2,927 healthy subjects, and 5,854 eyes, and reported a pooled mean ONSD measurement of 4.78 mm (95% CI, 4.63-4.94 mm), with no significant differences in the various geographic regions, in 34 studies.The mean ONSD in the current study is closer to that, however, with a slightly wider range.
A study from Turkey [9] reported an ONSD of 4.1±0.5 mm for the group of 50 adults with a normal head CT, and the cut-off value was 4.5 mm in the presence of intracranial pathology. A study of healthy adult Nepalese [13] had a range of 3.1 to 4.6 mm and a median value of 4.1 mm for normal ONSD. The Bangladeshi study [29] reported a median ONSD of 4.41 mm, 95% of values falling between 4.25 to 4.75 mm, in 136 healthy children (12.5% <16 years), and adults. A study of 500 healthy subjects of South India [30] showed a mean ONSD for males 4.5-5.1 mm (4.8±0.3 mm) and females 4.7-5.1 mm (4.9±0.2 mm). A Chinese study [12] reported a mean ONSD of 5.1 ± 0.5 mm and the 95th percentile of 5.9 mm in 519 healthy volunteers. In comparison to these regional studies, the values for the normal ONSD in the current study were similar to those reported from India [30].
Asghar et al. [12] studied 100 healthy volunteers in Karachi without forming age groups. They described that 95% of the study sample had an ONSD <4.82 mm. Rehman et al. [23] studied 52 subjects in Rawalpindi and compared the mean ONSD in patients with idiopathic intracranial hypertension (IIH) to ONSD in a normal control group. They reported a mean ONSD of 4.33±0.38 mm in the normal group. A study of 26 tumor patients in Karachi [24] to decide the pre-anesthetic status of ICP by ONSD, reported 5.0 mm as an upper limit of ONSD. In another study of 100 mass-effect-stroke intensive care unit (ICU) patients in Islamabad,[25] the authors expressedan ONSD >5.8 mm as the cut-off limit. In a study of 60 traumatic brain injury (TBI) patients conducted in Rawalpindi, [26] described an ONSD >5.0 mm as a cut-off value. In another Karachi study, [27] of 48 pediatric patients authors reported a threshold of ONSD in infants >4.0 mm, in children of 1-10 years >4.71 mm, in adolescent >10 years >5.43 mm for raised ICP.Among these Pakistani studies, the normal ONSD values in the current study are comparable to those reported by Asghar et al [12].
This was a cross-sectional study of B-modetransocularultrasound measurements of normal optic nerve sheath diameter in healthy adults. Thevolunteers belonged to four major ethnic groups of the Pakistani population living in ICT. The investigator’s experience of fewer than 5 years fits the anticipated expertise of a non-radiologist. This was a significant study because the local standard of the mean reference value of normal ONSD will help in early detection and saving patients from complications of intracranial hypertension.
5. Limitations
The same investigator took and recorded all readings; therefore, we could not assess the interobserver variability. We have not compared our results with studies using MRI or CT scans, which because of higher spatial resolution may provide a better image and measurement of ONSD. A comparison of directly measured ICP can better validate the correlation between TOU-measured ONSD and ICP. A-scan was not considered. The available sample age range of 20-50 years was narrow. We tried to include the four major ethnic groups of the Pakistani population, however, a comparable number of subjects from all ethnic groups were not available for this small study.
6. Recommendations
We would recommend the use of TOU-measured ONSD as a POCUS screening tool for all patients suspected of a raised ICP. We would also recommend using the ONSD values of the current study as the baseline for future reference in large multi-center human studies, especially in our country, to validate the use of TOU of ONSD in ICH patients.
7. Conclusion
The TOU-measured ONSD in 100 healthy adults form a section of the Pakistani population comprising the four major ethnic groups living in the ICT shows a mean value of 4.80±0.26 mm, a range of 4.25 to 5.2 mm, and an expected upper limit of 4.85 mm. There is no statistically significant difference in ONSD for the patient's age, gender, ethnicity, and right or left eye. Measurements beyond the upper limit warrant additional investigations to findraised ICP in patients suspected of ICH, and to avoid potential brain injury.
Acknowledgment
We thank all the volunteers who consented to take part in this study, and everybody who supported in any respect to make it possible.
Conflict of interest
The authors declare no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Financial Disclosure
The authors have no proprietary or commercial interest in any of the materials discussed in this article.
Funding: This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability statement
The de-identified participant primary data (spreadsheet, etc.) that support the findings of this study are available from the corresponding author (Salma Umbreen https://orcid.org/0000-0002-1682-6099 & drsalma.umbreen@gmail.com) upon reasonable request.
References:
- Sharma S, Hashmi MF, Kumar A. Intracranial Hypertension. InStatPearls [Internet] (2019).
- Raboel PH, Bartek J, Andresen M, et al. Intracranial pressure monitoring: invasive versus non-invasive methods—a review. Critical Care Research and Practice 2012 (2012).
- Abraham M, Singhal V. Intracranial pressure monitoring. Journal of Neuroanaesthesiology and Critical Care 2 (2015): 193-203.
- Robba C, Bacigaluppi S, Cardim D, et al. Non-invasive assessment of intracranial pressure. Acta Neurologica Scandinavica 134 (2016): 4-21.
- Sahu S, Swain A. Optic nerve sheath diameter: a novel way to monitor the brain. Journal of Neuroanaesthesiology and Critical Care 4 (2017): S13-S18.
- Richards E, Mathew D. Optic Nerve Sheath Ultrasound. InStatPearls [Internet] (2020).
- Damiani D, Damiani D. Non-Invasive Intracranial Pressure Evaluation in an Emergency Room–Point-of-Care Ultrasonography. Arquivos Brasileiros de Neurocirurgia: Brazilian Neurosurgery 38 (2019): 279-283.
- Koziarz A, Sne N, Kegel F, et al. Bedside optic nerve ultrasonography for diagnosing increased intracranial pressure: a systematic review and meta-analysis. Annals of Internal Medicine 171 (2019): 896-905.
- Komut E, Kozaci N, Sönmez BM, et al. Bedside sonographic measurement of optic nerve sheath diameter as a predictor of intracranial pressure in ED. The American Journal of Emergency Medicine 34 (2016): 963-967.
- Lochner P, Czosnyka M, Naldi A, et al. Optic nerve sheath diameter: present and future perspectives for neurologists and critical care physicians. Neurological Sciences (2019): 1-1.
- Chen H, Ding GS, Zhao YC, et al. Ultrasound measurement of optic nerve diameter and optic nerve sheath diameter in healthy Chinese adults. BMC Neurology 15 (2015): 1-6.
- Asghar A, Hashmi M, Hussain A. Optic nerve sheath diameter evaluated by transorbital sonography in healthy volunteers from Pakistan. Anaesthesia, Pain & Intensive Care (2019): 282-286.
- Shrestha GS. Transorbital sonographic evaluation of normal optic nerve sheath diameter in healthy Nepalese adults. Journal of Neuroanaesthesiology and Critical Care 3 (2016): 115-118.
- Bates A, Goett HJ. Ocular Ultrasound. InStatPearls [Internet] (2019).
- Bloria SD, Bloria P, Luthra A. Is it the time to standardize the procedure of ultrasound guided optic nerve sheath diameter measurement?. Saudi Journal of Anaesthesia 13 (2019): 255.
- Bäuerle J, Lochner P, Kaps M, et al. Intra-and interobsever reliability of sonographic assessment of the optic nerve sheath diameter in healthy adults. Journal of Neuroimaging 22 (2012): 42-45.
- Schroeder C, Katsanos AH, Richter D, et al. Quantification of Optic Nerve and Sheath Diameter by Transorbital Sonography: A Systematic Review and Metanalysis. Journal of Neuroimaging 30 (2020): 165-174.
- Kishk NA, Ebraheim AM, Ashour AS, et al. Optic nerve sonographic examination to predict raised intracranial pressure in idiopathic intracranial hypertension: the cut-off points. The Neuroradiology Journal 31 (2018): 490-495.
- De Bernardo M, Vitiello L, Cornetta P, et al. Ocular ultrasound evaluation of optic nerve sheath diameter in military environments. Military Medical Research 6 (2019): 16.
- Du Toit GJ, Hurter D, Nel M. How accurate is ultrasound of the optic nerve sheath diameter performed by inexperienced operators to exclude raised intracranial pressure?. SA Journal of Radiology 19 (2015): 1-5.
- Ogle KY, Lewiss RE. Optic Nerve Sheath Ultrasonography: Should We Be Using It for Bedside Diagnosis of Increased Intracranial Pressure?. Annals of Internal Medicine 171 (2019): 935-936.
- Shevlin C. Optic nerve sheath ultrasound for the bedside diagnosis of intracranial hypertension: pitfalls and potential. Critical Care Horizons 1 (2015): 22-30.
- Normal II. Optic nerve sheath diameter on sonography in idiopathic intracranial hypertension versus normal. Journal of the College of Physicians and Surgeons Pakistan 26 (2016): 758-760.
- Shafiq F, Ali MA, Khan FA. Pre-anaesthetic assessment of intracranial pressure using optic nerve sheath diameter in patients scheduled for elective tumour craniotomy. Journal of Ayub Medical College Abbottabad 30 (2018): 151-154.
- Munawar K, Khan MT, Hussain SW, et al. Optic nerve sheath diameter correlation with elevated intracranial pressure determined via ultrasound. Cureus 11 (2019).
- Ghauri MA, Burqi AM, Sultan A, et al. Role Of Transocular Ultrasound In Identifying Raised Intracranial Pressure And Predicting Intracranial Bleed In Traumatic Brain Injuries. Pakistan Armed Forces Medical Journal 69 (2019): 589-594.
- Haque A, Abbas Q, Jurair H, et al. Ultrasonographic optic nerve sheath diameter measurement for raised intracranial pressure in a tertiary care centre of a developing country. Journal of Ayub Medical College Abbottabad 30 (2018): 495-500.
- Vandenbroucke JP, Von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 4 (2007): e297.
- Maude RR, Hossain MA, Hassan MU, et al. Transorbital sonographic evaluation of normal optic nerve sheath diameter in healthy volunteers in Bangladesh. PloS one 8 (2013): e81013.
- Khasage UK, Kumar V, Shamanur NS, et al. Bedside transorbital sonographic evaluation of optic nerve sheath diameter in healthy south Indian population. J. Evid. Based Med. Health 3 (2016): 5573-5576.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
