Orbital Pseudotumor Masquerading as Orbital Cellulitis
Renis Qamo1, Esilda Trushaj2*, Ermal Simaku3
1Ophtalmology Resident, University Hospital Mother Theresa, Tirana, Albania
2Diagnostic imaging and Nuclear, Medicine Resident, University Hospital Mother Theresa, Tirana, Albania
3Ophtalmic Surgeon, University Hospital Mother Theresa, Tirana, Albania
*Corresponding author: Esilda Trushaj, Diagnostic imaging and Nuclear, Medicine Resident, University Hospital Mother Theresa, Tirana, Albania
Received: 02 February 2024; Accepted: 09 February 2024; Published: 22 February 2024
Article Information
Citation: Renis Qamo, Esilda Trushaj, Ermal Simaku. Orbital Pseudotumor Masquerading as Orbital Cellulitis. Journal of Ophthalmology and Research. 7 (2024): 25-27.
DOI: 10.26502/fjor.2644-00240091
View / Download Pdf Share at FacebookAbstract
A 55-year-old albanian male was referred to the Ophtalmology Department in Mother Theresa University Hospital Tirana, with blurried vision, painful proptosis, limitied eye movements diplopia and chemosis of the right eye for three days. Two years ago he was diagnosed with orbital cellulitis. Over the next 72 hours, he did not clinically improve as it was expected. a diffuse infiltrative mass of orbital muscles and fat on the right eye with exophtalmy of this side that suggested for infiltrative tumor. Based on the results of radiology, it was required biopsy. Histopathology revealed the presence of lymphocites, plasma cells, myofibrolastic cells and collagen, with diagnose of inflammatory chronic moderated lesion. Given the negative workup, the presentation was determined to be consistent with idiopathic orbital inflammation via a diagnosis of exclusion. Therefore, the patient was treated with intravenous steroids that produced pronounced improvement within 24 hours. The patient was discharged in improved condition with a prednisone taper and ophtalomoly follow-up. Orbital pseudotumor if often misdiagnosed as orbital cellulitis, because of the similar presentation. It is important to consider differential diagnose when the initial diagnose and treatment does not progress as we expect.
Keywords
<p>Orbital pseudotumor, Orbital cellulitis, Inflammation, Diagnosis, Steroid therapy, New treatments</p>
Article Details
1. Introuduction
Nonspecific orbital inflammation (NSOI), also known as orbital inflammatory pseudotumor, is the most common cause of painful orbitopathy in adults.It is defined as a benign, non-infectious process of the orbit without identifiable local or systemic causes. It is a clinical diagnosis of exclusion that is applied to orbital inflammation after true neoplasm, primary infection and systemic disorders have been ruled out. Most commonly involves extraocular muscles, but there may also be inflammatory changes involving retrobulbar soft tissue, the sclera, uvea, lacrimal gland. NSOI is the third most common orbital disease after thyroid eye disease and orbital lymphoma. NSOI can both radiologically and clinically mimic a malignant process [1].
The epidemiology of orbital pseudotumor is not well reported. It is considered the third most common ophthalmologic disease of the orbit after Graves disease and lymphoproliferative disorders and account for approximately 8-11% of all the orbital tumors [2].
The disease has been reported in all ethnic groups worldwide and is mostly unilateral. Is equally common in men and women. Among 1000 patients with primary orbital tumors clinically or histopathologically diagnosed at Tokyo Medical University Hospital from 1995 to 2019, OIP accounted for 27% and was the most common benign orbital tumor [3].
The ethiopatology is unknown. It is associated with other inflammatory and autoimmune disorders such are sarcoidosis, Morbus Chron, Rheumathoid Arthritis, Riedel thyroiditis etc. Many case reports and series have highlighted possible etiological factors for IOI, including autoimmune diseases and medications such as bisphosphonates, lithium and chemotherapeutics, viral infections [4].
Symptomatology mostly includes edema of the eyes and eyelids, proptosis, chemosis, diplopia, rapid usually eye pain. These manifestations are similar to orbital cellulitis, which is an inflammation of the soft tissue of the eye socket behind orbital septum. Idiopathic orbital inflammation is a diagnosis of exclusion.
Our case report aim is to discuss orbital pseudotumor manifasting as orbital cellulitis.
2. Case Describtion
A 55-year-old albanian male was referred to the Ophtalmology Department in Mother Theresa University Hospital Tirana, with blurried vision, painful proptosis, limitied eye movements diplopia and chemosis of the right eye for three days. This patient refers a repeted history two years ago with right eye pain and limitied movements . He was diagnosed in ophthalmology department with orbital cellulitis.
General physical examination and vital parameters were normal, lymph nodes were not palpable. On examination of the left eye 14/20 with full visual field, normal structures, normal eye pressure and proper muscle coordination. On examination of the right eye (LE), BCVA was 2/60 with accurate projection of rays. The right eye showed abaxial proptosis, floaters, conjunctival congestion with chemosis. There was conjunctival congestion with chemosis, eye eritema and diplopia.A dilated funduscopic examination of the right eye revealed optic disc edema of one diopter elevation. The intraocular pressure of the right eye was 25 mm. The B-scan of the right eye showed lateral rectus muscle enlargement.
Initial laboratory investigation including complete blood cell count and basic metabolic panel were normal. The orl consult was normal, with absence of nasal secretions, only nasal septal deviation on rinoscopy. The cardiac pulmonary, abdominal, neurologic exams revealed no deficits and/or abnormalities.
The patient was immediately started on intravenous Ceftriaxone 1 gm 2x1 for 7 days, intravenous Vankomycin 80 mg 2x1 for 7 days, Dexamethason 20 mg, eye drop Maxitrol (0.3%) QID in the right eye. There was mild improvement during the days regarding to diplopia that now was present only on right lateral position, fundus oculi examination was without changes and was also noticed reduced exophtalmy. Our patient continued having pain and limited eye movements.
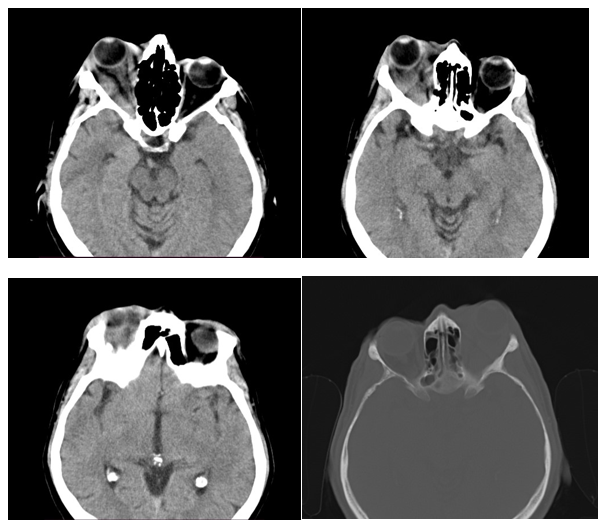
The head CT demostrated a diffuse infiltrative mass of orbital muscles and fat on the right eye with exophtalmy of this side that suggested for infiltrative tumor. Based on the results of radiology, it was required biopsy. Histopathology revealed the presence of lymphocites, plasma cells, myofibrolastic cells and collagen, with diagnose of inflammatory chronic moderated lesion.
The therapy changed in Ceftriaxone 1 mg, Vancomycn, fisiologic solution 2x1, Prednisone 5 mg 6:0:0 and Omeprazole 20 mg 1x1 p.os.
Neurosurgeon examined the patient and reported that pupils were both equal and reactive to light, extraocular movements were intact and there were no meningeal signs. The patient did not have indications for neurosurgical intervent. Surgery may be needed to remove part of the bones of the orbit to relieve pressure, but this want not the case.
The therapy prescripted by the ophthalmologist was Prednisone 5 mg
5ts-0-0 (5 days) 4ts-0-0 (5 days) 3ts-0-0(5 days)
Meocil 3.5 g 3x1 Aspirin protect 100 mg 0-1-0 and omeprazole 20 mg 1-0-0
The patient showed dramatic clinical improvement within 24 hours of steroid administration with a significant reduction in symptoms. He was subsequently discharged to complete the therapy at home with ophthalmology follow-up. .
3. Discussion
Non specific orbital inflammation (NSOI) also known as orbital inflammatory pseudotumor is a benign, noninfectious lesion of the orbit. The orbital inflammation occurs in absence of known systemic or local etiology. It is among the 3rd most common orbital diseases along with thyroid orbitopathy and lymphoproliferative disorder and accounts for 5-10% of orbital processes [2].
As in our case most of the symptoms include, eyelid swelling, proptosis, eye pain diplopia, limited eye movements. The clinic mimicks others diseases and it is important to make an accurate differential diagnosis. The most common are orbital lymphoma and orbital cellulitis.
In our case the patient was hosted at hospital with the same symptoms and was diagnosed with orbital cellulitis. Orbital cellulitis can arise from direct extension of sinusitis or orbital infection via hematogenous spread; or from complications of eye surgery, sinus surgery, or dental work [5]. Based on the anamnesis of our patient there was no evidence that he had one of these conditions. We did not have a satisfactory improvement after the cure of antibiotics.
This lead our doctors to consider another differential diagnose. On radiological imaging, they both can appear as a diffuse inflammatory process, further adding to the confusion [6]
A ct scan was required which is an important diagnostic tool. On the head CT there was a diffuse infiltrative mass of orbital muscles and fat on the right eye with exophtalmy of this side that suggested for infiltrative tumor.
The studies have shown that orbital pseudotumor should be considered as a possible differential diagnosis when radiological studies reveal lesions extending from the orbit to intracranial structures [7]
We may consider our case as chronic orbital pseudotumor. In subacute and chronic forms, the diagnosis is more difficult and a biopsy may be necessary to rule out neoplasm. Histopathology revealed the presence of lymphocites, plasma cells, myofibrolastic cells and collagen, with diagnose inflammatory chronic moderated lesion.
According to a study on the role of biopsy, thirty-nine patients suspected of orbital pseudotumor, underwent biopsy as the next step. Nine patients underwent a therapeutic trial of corticosteroids of which one was subsequently subjected to biopsy. This valuates the role of biopsy when imaging is not very conclusive [8].
To control the inflammatory response, the patient was initiated on oral corticosteroids with a tapering schedule for corticosteroid reduction. Day after day improvement was seen. It is important to take in consideration the long term . Other studies have shown that response to steroid therapy was generally favorable initially, but persistent and recurrent cases accounted for a significant portion of the treatment failures [9]. This means that the long-term efficacy is not satisfactory. Immunosuppressants, infliximab, rituximab, adalimumab, curcumin, plasma exchange, surgical debulking, or resection may be used in patients unresponsive to systemic glucocorticoids. In addition, the disease has a certain proportion of relapses, and some patients have multiple relapses [10].This need to be seen in long term of time and further exploration and studies need to be taken.
4. Conclusion
Orbital pseudotumor if often misdiagnosed as orbital cellulitis, because of the similar presentation. It is important to consider differential diagnose when the initial diagnose and treatment does not progress as we expect.
Acknowledements
We would like to acknowledge and thank A.Sh, the patient presented in this case, for providing us with permission to use images to help educate future clinicians.
Human Ethics
Consent was obtained by the patient in this study.
Conflicts of Interests
There are no conflicts of interest.
References
- Jirawuthiworavong GV, Chundury RV, Lee AG, et al. Nonspecific Orbital Inflammation (Idiopathic Orbital Inflammation, Orbital Inflammatory Syndrome, Orbital Pseudotumor) (2024).
- Chaudhry IA, Shamsi FA, Arat YO, et al. Orbital pseudotumor: distinct diagnostic features and management. Middle East Afr J Ophthalmol 15 (2008): 17-27.
- Fang Y, Shen B, Dai Q, et al. Orbital inflammatory pseudotumor: new advances in diagnosis, pathogenesis, and treatment. Eur J Med Res 28 (2023): 395.
- Bijlsma WR, van Gils CH, Paridaens D, et al. Risk factors for idiopathic orbital inflammation: a case-control study. Br J Ophthalmol 95 (2011): 360-364.
- Hayes L, Garibaldi D, Kim A. Orbital Pseudotumor Disguised as Orbital Cellulitis and Sinusitis (2012).
- Kapur R, Sepahdari AR, Mafee MF, et al. Setabutr American Journal of Neuroradiology 30 (2009): 64-70.
- Bencherif B, Zouaoui A, Chedid G, et al. Intracranial extension of an idiopathic orbital inflammatory pseudotumor. AJNR Am J Neuroradiol 14 (1993): 181-184.
- Bijlsma WR, Elbert NJ, Kalmann R. The role of biopsy in diagnosing patients suspected of idiopathic orbital inflammation. Curr Eye Res 37 (2012): 251-253.
- Yuen SJA, Rubin PAD. Idiopathic Orbital Inflammation: Distribution, Clinical Features, and Treatment Outcome. Arch Ophthalmol 121 (2003): 491–499.
- Fang Y, Shen B, Dai Q, et al. Orbital inflammatory pseudotumor: new advances in diagnosis, pathogenesis, and treatment. Eur J Med Res 28 (2023): 395.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
