Outcomes of Alcohol Septal Ablation in the Patients with Hypertrophic Obstructive Cardiomyopathy
Mei-lian Cai1,2 , Yu-ming Chen1*, Guo-qiang Zhong1*
1Department of Cardiology, the First Affiliated Hospital of Guangxi Medical University, Nanning, China
2Department of Cardiology, People's Liberation Army Joint Logistic Support Force 924th Hospital (form name: 181st Hospital of Chinese People's Liberation Army), Guilin, China
*Corresponding author: Yu-ming Chen. Department of Cardiology, the First Affiliated Hospital of Guangxi Medical University, Nanning, China.
Guo-qiang Zhong, Department of Cardiology, the First Affiliated Hospital of Guangxi Medical University, Nanning, China
Received: 14 January 2024; Accepted: 19 January 2024; Published: 12 February 2024
Article Information
Citation: Mei-lian Cai, Yu-ming Chen, Guo-qiang Zhong. Outcomes of Alcohol Septal Ablation in the Patients with Hypertrophic Obstructive Cardiomyopathy. Cardiology and Cardiovascular Medicine. 8 (2024): 52-59.
View / Download Pdf Share at FacebookAbstract
Background: Alcohol septal ablation (ASA) is a commonly used invasive procedure for reducing septum volume in patients with hypertrophic obstructive cardiomyopathy (HOCM).
Objective: This study aimed to evaluate the safety and efficacy of ASA in patients with drug-refractory symptomatic HOCM. A total of 20 patients hospitalized in the Department of Cardiology at our hospital with HOCM from July 2019 to July 2022 were collected and received ASA to compare the differences in the relevant indicators before ASA and 3 months after ASA.
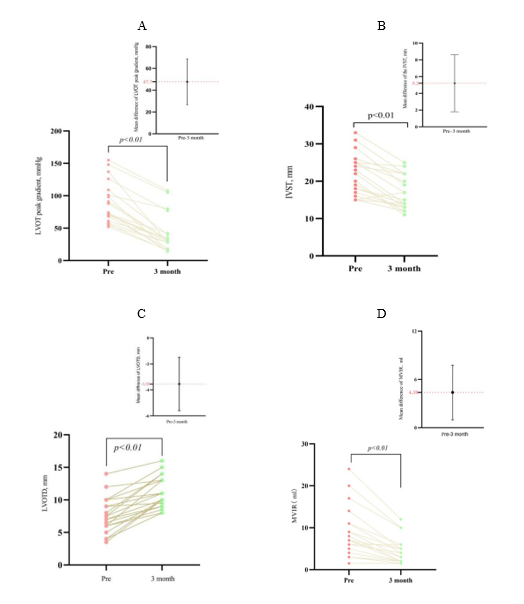
Results: At 3 months post-ASA, mean of left ventricular outflow tract (LVOT) peak gradient decreased to 55.5%±18.5%. Echocardiography derived that LVOT peak gradient decreased from 88.1±32.0 mmHg to 40.4±28.7 mmHg (p<0.001). Interventricular septum thickness (IVST) reduced from 21.8±5.4 mm to 16.6±4.5 mm (p<0.001). Left ventricular outflow tract diameter (LVOTD) increased from 7.6±2.7 mm to 11.5±2.4 mm (p<0.001). Mitral valve instantaneous regurgitation (MVIR) decreased from 8.5±6.1 mL to 4.7±3.2 mL (p<0.001). There were no significant differences in left ventricular end-diastolic diameter (LVEDD) or left ventricular ejection fraction (LVEF) (P>0.05). During ASA and up to 3 months post procedure, no serious complications were observed.
Conclusion: ASA has been a safe and effective treatment strategy for patients with drug-refractory symptomatic HOCM.
Keywords
<p>Hypertrophic cardiomyopathy; Obstructive; Alcohol septal Ablation; Chemical ablation; Outflow tract pressure gradient</p>
Article Details
Abbreviations:
AF- Atial Fibrillation; ASA- Alcohol Septal Ablation; AVB- avtrioventricular block; CAG-Coronary Angiography; COVID-19- Corona Virus Disease 2019; CRT- Cardiac Resynchronization Therapy; EBU- Extra Back-Up; ECG- Electrocardiogram; HCM- Hypertrophic Cardiomyopathy; HOCM- Hypertrophic Obstructive Cardiomyopathy; ICD- Implantable Cardioverter Defibrillator; IVST- Interventricular Septum Thickness; LBBB- Left Bundle Branch Block; LV- Left Ventricular; LVH- Left Ventricular Hypertrophy; LVOT- Left Ventricular Outflow Tract; LVOTO- Left Ventricular Outflow Tract Obstruction; LVOTG- Left Ventricular Outflow Tract Gradient; LVOTD- Left Ventricular Outflow Tract Diameter; LVEDD- Left Ventricular End-diastolic Diameter; LVEF- Left Ventricular Ejection Fraction; MVIR- Mitral Valve Instantaneous Regurgitation; NYHA- New York Heart Association; OTW- Over-The-Wire; PPM- Permanent, Pacemaker; SAM- Systolic Anterior Motion; SSM- Surgical Septal Myectomy
1. Introduction
Hypertrophic cardiomyopathy (HCM) is characterized by the presence of left ventricular hypertrophy (LVH) without any underlying cardiac, systemic, syndrome, or metabolic disease, with a thickness of 15mm [1-2]. HCM presents with various clinical manifestations, including chest pain, chest tightness, syncope, palpitations, and sudden cardiac death (SCD) [3]. The most signifificant hemodynamic consequence is left ventricular outflow tract obstruction (LVOTO), with 70% of patients displaying a dynamic LV outflow tract gradient (LVOTG) of 30 mmHg (0.1mmHg=133kPa) or above [4]. Percutaneous transluminal septal myocardial ablation (PTSMA) using alcohol septal ablation (ASA) is a treatment option for hypertrophic obstructive cardiomyopathy (HOCM). This study aims to assess the safety and efficacy of ASA in patients with HOCM.
2. Materials and Methods
2.1 Study Population
This single-center, retrospective observational study was conducted in the Department of Cardiology of the First Affiliated Hospital of Guangxi Medical University from July 2019 to July 2022. All participants met the criteria in the guidelines for diagnosis and treatment of HOCM 2023 and ASA [5].
2.2 Methods
2.2.1 Coronary Angiography and LV Angiography
Preoperative coronary angiography (CAG) was performed to rule out the need for coronary bypass grafting, assess the coronary condition, and evaluate the peak systolic pressure difference between the ventricular cavity and the outflow tract using LV angiography. Base on the location of the hypertrophic myocardium in the basal or intermediate segment, the target vessel at the corresponding location was determined. CAG and LV angiography identified the suitable target vascular, specifically the first or second septal branch. Additionally, the anatomical morphology of the septal branch was confirmed to be amenable for interventional operation.
2.2.2 ASA
All procedures were conducted by three interventional cardiologists from our cardiology department. Following radial artery puncture, Extra Back- Up (EBU) 3.5 standard guide catheters were advanced to the left coronary ostium. The Runthrough NS guidewire was then directed through the target septal branch to its distal end using an over-the-wire (OTW) balloon technique, which was subsequently inflated to a pressure of 6 atm. CAG confirmed complete occlusion of the septal branch without any evidence leakage. Subsequently, the Runthrough NS guidewire was withdrawn and ethanol, at a rate of (0.1-0.3) mL per minute, was infused into the OTW balloon chamber. The total amount of ethanol infused did not exceed 3ml and the infusion last for 5 minutes. Throughout the procedure, continuous the electrocardiogram (ECG) and echocardiographic monitoring were performed. Achievement of the desired hemodynamic effect was defined as a decrease in LVOT peak gradient of ≥ 50% or a final value of <30mmHg. CAG was repeated to confirm the successful occlusion of the integrity of the left anterior descending artery without the presencs of thrombus. Following ASA, patients underwent routine monitoring including ECG, myocardial enzyme assessment, serum troponin T measurement, and echocardiography. The patients experienced improvement and were typically discharged from the hospital after 3-5 days of ASA. They were advised to continued taking β blockers, calcium channel blockers, or other prescribed medications for their underlying conditions.
2.2.3 Observed Indicators
Clinical, demographic, echocardiographic data and symptoms were recorded at baseline and during follow-up. LVOT peak gradient, IVST, left ventricular outflow tract diameter (LVOTD), mitral valve instantaneous regurgitation (MVIR), left ventricular end-diastolic diameter (LVEDD) and left ventricular ejection fraction (LVEF) were recorded and compared before ASA and 3 months after ASA. Systolic anterior motion (SAM), New York Heart Association (NYHA) functional classification were recorded and compared before ASA and after ASA. Intraoperative alcohol dose, number of target vessel branches for ablation, target vessel name for ablation, and perioperative complications were recorded.
2.2.4 Postoperative Efficacy Evaluation
Evaluation of operation success: intraoperative CAG showed no shadow of the target septal branch or no thrombosis of the anterior descending branch, and the patient's symptoms were relieved immediately postopration.
Effect assessment: At 3 months post-ASA, the patients underwent echocardiography examination. It was considered good if that LVOT peak gradient decreased ≥50% or a final value of <30mmHg, and poor if the LVOT peak gradient decreased <50% or a final value of >30mmHg.
2.3 Statistical Analysis
We used SPSS statistical software version 27.0 to perform data analysis. Normally distributed measurement data were expressed as x ± s and analyzed with the paired sample t-test; Count data were expressed as percentages and analyzed with the χ2 test. non-normally distributed measurement data are expressed as the median (min, max). P values < 0.05 were considered statistically significant, while P values > 0.05 were considered statistically non-significant. Categorical variables were defined as the number of observed patients (percentage). Based on the statistical results of SPSS 27.0 software, the figures were plotting using Graphpad Prism 8.0 software.
3. Results
3.1 Baseline Characteristics
Table 1 presents a summary of the baseline characteristics of the study population. All participants were Asian ethnicity and originated China. Out of the total sample, 15 (75%) were males and 5 (25%) were females. The mean age of the patients included in the study was 54.5±11.2 years.
Table 1: Baseline clinical characteristics
|
Characteristics |
No.(%) |
Characteristics |
No.(%) |
|
Clinical Characteristics |
Calcium channel blocker |
3(15) |
|
|
Age,mean(SD), y |
54.5±11.2 |
Family history of HCM |
2(10) |
|
BMI, kg/m2 |
24.4±1.7 |
Family history of SCD |
1(5) |
|
Male |
15(75) |
Past history |
|
|
Female |
5(25) |
Hypertension |
7(35) |
|
Course of disease, y |
3(0.5,50) |
Coronary heart disease |
4(20) |
|
Clinical Symptoms |
2-DM |
2(10) |
|
|
Chest pain |
9(45) |
Chronic bronchitis |
2(10) |
|
Chest tightness |
13(65) |
AF |
1(5) |
|
Palpitations |
5(25) |
Myocardial bridge |
1(5) |
|
Syncope |
3(15) |
PPM |
2(10) |
|
Shortness of breath |
2(10) |
ICD |
1(5) |
|
Dizziness |
3(15) |
CRT |
1(5) |
|
fatigue |
1(5) |
NYHA functional classification |
|
|
SAM |
18(90) |
III |
8(40) |
|
Medications |
II |
9(45) |
|
|
Β blocker |
17(45) |
I |
3(15) |
Abbreviation: BMI: body mass index; SAM: systolic anterior motion; SCD: sudden cardiac death; HCM: hypertrophic cardiomyopathy; DM: diabetes mellitus; AF: atrial fibrillation; ICD: implantable cardioverter defibrillator; PPM: permanent pacemaker; CRT: cardiac resynchronization therapy; NYHA:New York Heart Association
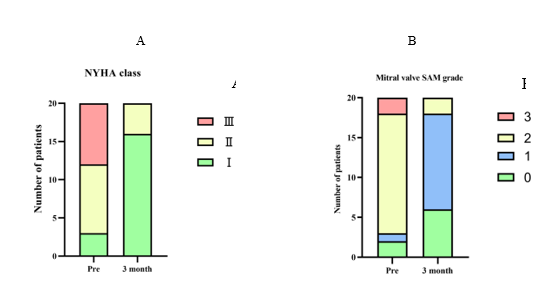
Among the 20 patients, hypertension was observed in 7 (45%) , coronary heart disease in 4 (20%) , type 2 diabetes mellitus (2-DM) in 2 (10%), chronic bronchitis in 2 (10%), atrial fibrillation (AF) in 1 (5%), and myocardial bridge in 1 (5%). The patient with AF underwent radiofrequency ablation following ASA. The 4 patients with coronary heart disease exhibited coronary artery stenosis ranging from 50% to 60%, and received secondary prevention measures for coronary artery disease. Prior to ASA, 4 (20%) patients received cardiac instrumental treatment. Of these, 2 (10%) were implanted with a permanent pacemaker (PPM). 1 (5%) received an implantable cardioverter-defibrillator (ICD) , and 1 (5%) received cardiac resynchronization therapy (CRT). Based on NYHA classification, 8 (40%) patients were categorized as NYHA III; 9 (45%) as NYHA II, and 3 (15%) as NYHA I.
3.2 Association of Treatment with Outcomes
Table 2: Procedural, and 3 month parameters and clinical events
|
Characteristics |
No.(%) |
|
Procedural ablation parameters, median |
|
|
ethanol dose |
1.9±0.6 |
|
first interval branch |
18(90) |
|
first and second interval branch |
2(10) |
|
Procedure-related chest pain |
20(100) |
|
Major adverse clinical events |
2(10) |
|
Procedural and 3 month mortality |
0 |
|
Right bundle branch block |
0 |
|
Left bundle branch block |
0 |
|
second-degree type 2 AVB |
1(5) |
|
third-degree AVB |
1(5) |
|
Temporary pacemaker |
2(10) |
|
Aneurysm of septal branch |
0 |
|
Coronary thrombosis |
0 |
|
Procedure-related permanent pacemaker implantation |
0 |
|
Ventricular septal defect |
0 |
|
Pericardial effusion |
0 |
|
Bleeding |
0 |
|
Infection |
0 |
|
Hematoma at the puncture site |
0 |
|
Heart failure |
0 |
The procedural, 3 month parameters and clinical events are present in Table 2. The success rate of operation was 100% in this study. Out of the 20 patients, 14 demonstrated significant results, while 6 patients showed a poor effect. The mean ethanol dose was 2.2±0.5 mL and 1.3±0.4 mL, respectively. The overall mean ethanol dose was 1.9±0.6 mL. In terms of the ablation procedural, 18 patients underwent ablation of the first interval branch, while 2 patients underwent ablation of both the first and second interval branches. All patients experienced transient procedure-related chest pain, which was successfully treated with morphine injection, resulting in the symptoms disappearing. The perioperation and 3-month major adverse clinical event rate was 10% (n = 2). During the operation, 1 patient experienced second-degree type 2 AVB, while 1 patient experienced third-degree AVB. Temporary pacemakers were implanted for these patients; fortunately, the AVB persisted for less than 24 hours, and the temporary pacemakers were subsequently removed. There were no postoperative complications observed, including septal perforation, delayed AVB, coronary thrombosis, cardiac rupture, or death.
3.3 Procedural Outcomes
Table 3: Clinical outcomes of ASA at 3 month follow-up
|
Variable |
No.(%) |
P value |
|
|
Baseline |
3 month follow-up |
||
|
NYHA functional classification |
|||
|
I |
3(15) |
16(80) |
|
|
II |
9(45) |
4(20) |
|
|
III |
8(40) |
0(0) |
|
|
Mitral valve SAM grade |
|||
|
0 |
2(10) |
6(30) |
|
|
1 |
1(5) |
12(60) |
<0.05 |
|
2 |
15(75) |
2(10) |
<0.05 |
|
3 |
2(10) |
0(0) |
|
|
LVOT peak gradient (mmHg) |
88.1±32.0 |
40.4±28.7 |
<0.001 |
|
IVST (mm) |
21.8±5.4 |
16.6±4.5 |
<0.001 |
|
LVOTD (mm) |
7.6±2.7 |
11.5±2.4 |
<0.001 |
|
MVIR (ml) |
8.5±6.1 |
4.7±3.2 |
<0.001 |
|
LVEDD (mm) |
46.8±5.1 |
46.1±4.6 |
0.369 |
|
LVEF (%) |
67.0±9.4 |
67.9±9.2 |
0.652 |
Abbreviation: NYHA:New York Heart Association; SAM: systolic anterior motion; LVOT: left ventricular outflow tract ; LVOTD: left ventricular outflow tract diameter; IVST: interventricular septum thickness; MVIR: mitral valve instantaneous regurgitation; LVEDD: left ventricular end-diastolic diameter; LVEF: left ventricular ejection fraction.
We observed that at 3 months postoperation, the patients showed no symptoms of chest tightness, chest pain or shortness of breath. Moreover, our study revealed that the postoperative echocardiograms reviewed were better compared to preoperation (Figure 1, A, B, C, and D). The LVOT peak gradient decreased significantly from 88.1±32.0 mmHg to 40.4±28.7 mmHg (p<0.001) (A). Additionally, the mean maximum IVST reduced from 21.8±5.4 mm to 16.6±4.5 mm (p<0.001) (B). The LVOTD increased from 7.6±2.7 mm to 11.5±2.4 mm (p<0.001) (C). Furthermore, the MVIR decreased from 8.5±6.1 ml to 4.7±3.2 ml (p<0.001) (D). However, there was no significant difference in LVEDD or LVEF (P>0.05). It is worth noting that there was a significant improvement in NYHA functional classification (Figure 2, A). Specifically, NYHA functional class I increased from 3 to 16, NYHA functional class III decreased from 8 to 0. Additionally, the Mitral valve SAM grade also showed improvement (Figure 2, B). The disappearance of Mitral valve SAM increased from 2 to 6, while Mitral valve SAM grade 1 increased from 1 to 12 (P<0.05). Conversely, Mitral valve SAM grade 2 decreased from 15 to 2 (P<0.05).
Figure 1: Assessment of clinical improvement after ASA. (A) Comparison of LVOT peak gradient preoperation and 3 month follow-up. (B) Comparison of IVST preoperation and 3 month follow-up. (C) Comparison of LVOTD preoperation and 3 month follow-up. (D) Comparison of MVIR preoperation and 3 month follow-up.
4. Discussion
The echocardiography findings of this study demonstrated a decrease in LVOT peak gradient by an average of 55.5% ± 18.5% at 3 months after ASA treatment. ASA treatment is known to induce local myocardial ischemia and necrosis in the high ventricular septum, leading to an increase in the width of the LVOTD and subsequently improving LVOTO and clinical symptoms [6]. Moreover, as the severity of mitral regurgitation reduces, there is a subsequent decrease in LV end-diastolic pressure decreases, which contributes to a reduction in the size of the LV. This reduction in LV size further decreases the burden of AF and the severity of pulmonary hypertension [7]. The efficacy of the treatment is closely related to the amount of ethanol used during the procedure. Veselka et al determined that a dose of 1.5-2.5 mL of ethanol is the most suitable in terms of safety and effectiveness for periprocedural [8]. Considering long-term safety, it has been demonstrated that ASA with the standard ethanol dose of 3 mL is both safe and effective [9].
Perioperative complications of ASA mainly include AVB and right bundle branch block. The patients are prone to implant permanent dual chamber pacemaker [10]. A significant number of patients with HOCM who undergo ASA closure are at a 9% risk of requiring PPM implantation within 30 days post-ASA [11]. In this study, We did not observed any severe postoperative arrhythmia, which can be attributed to the preoperative implantation of cardiac instruments. Additionally, two patients who had temporary pacemakers implanted in the intraoperation were able to smoothly remove the temporary pacemakers without requiring PPM implantation. Notably, no deaths or severe complications occurred during the perioperative period. During the 6-month follow-up, all patients included in this study reported no symptoms of chest tightness, chest pain, palpitations, shortness of breath, syncope, delayed AVB, or any other complications leading to death. Due to the impact of corona virus disease 2019 (COVID-19) pandemic, most patients underwent echocardiography or cardiac MRI examinations at local hospitals for their 6-months postoperative evaluation. To ensure data reliability, we did not compare data obtained from external hospitals with those collected form our own institution.
SAM is a hallmark feature specific to HOCM. Its initial description dates back to the 1960s [12]. SAM has been observed in 30%-60% of HCM patients [12-14], while in this study, it was observed in 95% of patients. However, there have been reports linking SAM to certain conditions such as acute obstruction of the left coronary artery, mitral valve repair surgery, ventricular septal hypertrophy in hypertensive patients (under conditions of absolute hypovolemia), all of which can lead to LVOTO [15-16]. LVOTO in HOCM is a dynamic and unstable phenomenon that requires comprehensive evaluation [3]. The decision to repeat ASA should be based on a combination of patient symptoms and echocardiography results. Currently, there are three main invasive methods for reducing septum volume in HOCM [17]: ASA, surgical septal myectomy (SSM), and septal radiofrequency ablation. There were no significant differences in all-cause mortality, cardiovascular mortality, and SCD between SSM and ASA [18]. ASA demonstrated advantages in improving NYHA functional class, reducing LVOTG, and lowing the incidence of new AF [19]. Therefore, ASA can be considered as an alternative treatment for mildly symptomatic HOCM patients who are intolerant to SSM. However, compared to SSM, ASA is associated with a higher risk of complete heart block and the need for repeated procedures, among other factors. Researchers at Xijing Hospital introduced the Liwen technique in 2016 for the first time to treat HOCM patients. The Liwen technique is a novel intervention procedure known as percutaneous intramyocardial septal radiofrequency ablation (PIMSRA), which involves guiding a radiofrequency needle through the hypertrophic ventricular septum and using high-temperature radiofrequency (90-100°C) to induce coagulation necrosis in the hypertrophic myocardium. This intervention leads to thinning of the LV septum, thereby reducing LVOTG and improving clinical symptoms [20].
A study involving 244 patients with drug-refractory HOCM found PIMSRA resulted in a reduction of mean maximum septal thickness from 24.0±5.1 mm to 17.3±4.4 mm (P < 0.001) and a decrease in mean LVOTG from 79.0±53.0 mmHg to 24.0±14.0 mmHg (P < 0.001). The thirty-day major adverse clinical event rate was 10.5% (n = 21), with no reported bleeding events or strokes. These findings suggest that PIMSRA may be an effective procedure for relieving LVOTO and associated symptoms with an acceptable rate of complications [21]. Currently, there are two newly developed targeted drugs, namely mavacamten and aficamten, which belong to the category of small molecule cardiac myosin inhibitors. These drugs have been specifically designed for the treatment of symptomatic patients with HOCM. In terms of regulatory approval, mavacamten received its authorization in the United States during the month of April in 2022. This approval was granted specifically for the treatment of adult patients with symptomatic NYHA functional class II-III HOCM, aiming to enhance both cardiac function and alleviate clinical symptoms [22]. Subsequently, in June 2023, this drug received approval in Europe as well, thereby broadening its scope for the treatment of symptomatic HOCM in adult patients [23]. Aficamten is being used in phase III clinical trials.
5. Limitations
This study is a retrospective analysis with a small sample. Due to the impact of the COVID-19 epidemic, the most important limitation of this study is its lack of long-term follow-up, and the subsequent inability to assess the patient's prognosis.
6. Conclusion
ASA in patients with HOCM is safe and effective for relief of symptoms at short-term follow-up.
Funding
Funding information is not applicable
Author Contributions
Conceptualization: Meilian Cai, Data curation: Meilian Cai, Investigation: Meilian Cai, Resources: Yuming Chen, Supervision: Guoqiang Zhong, Writing-original draft: Yuming Chen, Guoqiang Zhong, Writing-review & editing: Meilian Cai
Institutional Review Board Statement: The study was conducted according to the guidelines of the Declaration of Helsinki, and clinical protocol was approved by the ethics committee of the First Affiliated Hospital of Guangxi Medical University (2024-E076-01).
Informed Consent Statement: Patient consent was waived due to retrospective nature of the study.
Data Availability Statement: The data presented in this study are available on request from the corresponding author.
Conflicts of Interest: The authors declare no conflict of interest.
References
- Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [J]. The Journal of thoracic and cardiovascular surgery 162 (2018): e23-e106.
- Maron B.J. Clinical course and management of hypertrophic cardiomyopathy [J]. N Engl J Med. 379 (2018): 1977.
- Cai ML, Zhong GQ. Hypertrophic Obstructive Cardiomyopathy with SAM Phenomenon: A Case Report and Literature Review [J]. Cardiology and Cardiovascular Medicine 6 (2022): 515-522.
- Albano B B, Fadreguilan E C, Chua J M. et al. Treating a Structural Heart Disease Using a Non- structural Approach: Role of Cardiac Pacing in Hypertrophic Cardiomyopathy [J]. Cardiol Res 8 (2017): 20-25.
- The Joint Committee of Cardiomyopathy Specialty Alliance, National Center for Cardiovascular Diseases/Cardiovascular Precision Medicine Branch of China International Exchange and Promotive Association for Medical and Health Care, Expert group of "Guidelines for Diagnosis and Treatment of Hypertrophic Cardiomyopathy 2023". Guideline for Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy 2023 [J]. Chinese Circulation Journal 38 (2023): 1-33.
- Jensen MK, Prinz C, Horstkotte D, et al. Alcohol Septal Ablation in Patientswith Hypertrophic Obstructive Cardiomyopathy:Low Incidence of Sudden Cardiac Death and Reduced Risk Profile [J]. Heart 99 (2013): 1012-1017.
- Hypertrophic Cardiomyopathy[M], Springer Science and Business Media LLC (2019).
- Veselka J, Jensen MK, Liebregts M, et al. Long-term clinical outcome after alcohol septal ablation for obstructive hypertrophic cardiomyopathy: results from the Euro-ASA registry [J]. Eur Heart J 37 (2016): 1517-1523.
- Kashtanov MG, Rzhannikova AD, Chernyshev SD, et al. Outcomes of hypertrophic obstructive cardiomyopathy patients undergoing alcohol septal ablation with a standard 3 mL dose of ethanol: Focus on long-term safety [J]. Catheter Cardiovasc Interv 95 (2020): 1212- 1218.
- Liebregts M, Faber L, Jensen MK, et al. Outcomes of Alcohol Septal Ablation in Younger Patients With Obstructive Hypertrophic Cardiomyopathy [J]. JACC Cardiovasc Interv 10 (2017): 1134-1143.
- Veselka J, Liebregts M, Cooper R, et al. Outcomes of Patients With Hypertrophic Obstructive Cardiomyopathy and Pacemaker Implanted After Alcohol Septal Ablation [J]. JACC Cardiovasc Interv 15 (2022): 1910-1917.
- Luckie M, Khattar RS. Systolic anterior motion of the mitral valve--beyond hyperthrophic cardiomyopathy [J]. Heart 94 (2008): 1383-1385.
- Luckner G, Margreiter J, Jochberger S, et al. Systolic anterior motion of the mitral valve with left ventricular outflow tract obstruction: three cases of acute perioperative Hypotension in noncardiac surgery [J]. Anesth Analg 100 (2005): 1594-1598.
- Ibrahim M, Rao C, Ashrafian H, et al. Modern management of systolic anterior motion of the mitral valve. Euro J Cardio-Thoracic Surgery 41 (2012): 1260-1270.
- Sobczyk D. Dynamic left ventricular outflow tract obstruction: underestimated cause of hypotension and hemodynamic instability [J]. J Ultrason 14 (2014): 421-427.
- Maslow AD, Regan MM, Hearing J M, et al. Echocardiographic predictors of left ventricular outflow tract obstruction and systolic anterior motion of the mitral valve after mitral valve reconstruction for myxomatous valve disease [J]. J Am Coll Cardiol 34 (1999): 2096-2104.
- Fifer M A. Septal reduction therapy for hypertrophic obstructive cardiomyopathy [J]. J Am Coll Cardiol 72 (2018): 3095–3097.
- Osman M, Kheiri B, Osman K, et al. Alcohol septal ablation vs myectomy for symptomatic hypertrophic obstructive cardiomyopathy: Systematic review and meta-analysis [J]. Clin Cardiol 42 (2019): 190-197.
- Li p, Xue y, Sun J, et al. Outcome of alcohol septal ablation in mildly symptomatic patients with hypertrophic obstructive cardiomyopathy: A comparison with medical therapy [J]. Clin Cardiol 44 (2021): 1409-1415.
- Liu LW, Liu B, Li J, et al. Percutaneous intramyocardial septal radiofrequency ablation of hypertrophic obstructive cardiomyopathy: a novel minimally invasive treatment for reduction of outflow tract obstruction [J]. Euro Intervention 13 (2022): e2112-2113.
- Zhou M, Ta S, Hahn RT, et al. Percutaneous Intramyocardial Septal Radiofrequency Ablation in Patients With Drug-Refractory Hypertrophic Obstructive Cardiomyopathy [J]. JAMA Cardiol 7 (2022): 529-538.
- Keam SJ, Mavacamten: First Approval [J]. Drugs 82 (2022): 1127-1135.
- Scholtz, S, Rudolph, V, Reil, J C. Alcohol Septal Ablation or Mavacamten for Obstructive Hypertrophic Cardiomyopathy [J]. Journal of clinical medicine 12 (2023): 6628.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 