Pseudexfoliation: Therapeutical Treatment in Ocular Hypertension Related to Pseudoexfoliation Syndrome
Felisia Gjyrdedi
European Eye Clinic, Tirana, Albania
*Corresponding author: Felisia Gjyrdedi, European Eye Clinic, Tirana, Albania.
Received: 05 August 2025; Accepted: 13 August 2025; Published: 08 September 2025.
Article Information
Citation:
Felisia Gjyrdedi. Pseudexfoliation: Therapeutical Treatment in Ocular Hypertension Related to Pseudoexfoliation Syndrome. Journal of Ophthalmology and Research. 8 (2025): 47-52.
DOI: 10.26502/fjor.2644-002400105
View / Download Pdf Share at FacebookAbstract
Glaucoma is a disease characterized by progressive damage to the optic nerve, with or without elevated intraocular pressure; and is one of the leading causes of irreversible blindness worldwide. Pseudoexfoliation has been identified as the leading cause of secondary open-angle glaucoma. It is a disease that affects over 60-70 million people. The pathophysiology of pseudoexfoliation is characterized by the deposition in the eye tissues of a fibrillar material. Intraocular deposits are found in the trabecular meshwork, cornea, lens, and iris, leading to significant ocular and visual morbidity. The prevalence of the disease varies by geographic location and ethnicity, and a number of environmental, demographic, genetic, and molecular factors have been identified as potential causes. Despite the high morbidity, there is still no definitive cure for pseudoexfoliation. Treatments are aimed at managing elevated intraocular pressure, including local, systemic, or surgical therapy.
Keywords
<p>Pseudoexfoliation, Glaucoma, Intraocular pressure.</p>
Article Details
1. Aim of the Study
The aim of our study was to asses the incidence of ocular hypertension and glaucoma in patients with pseudexfoliation syndrome, and the adequate management of elevated ocular pressure, medically and surgically.
2. Materials and Methods
This was a prospective study, conducted by evaluating the patients presented in our department at Mother Theresa Hospital Tirana, during a six months period, from May to October 2022. In the study were included all patients over 45 years old, which presented with different complaints such as decrease in visual acuity, or routine check-ups. We excluded from the study all patients who were currently under treatment for glaucoma. Each patient underwent a complete ophthalmological evaluation, including visual acuity, intraocular pressure measurement with a Goldmann tonometer, biomicroscopic evaluation of the anterior segment, gonioscopy, and the evaluation of fundus oculi and optic nerve after dilation. In patients with intraocular hypertension and/or changes in the appearance of the optic nerve, Optical Coherence Tomography (OCT) and pachymetry were performed. Patients were also asked about the presence of other systemic pathologies, especially allergies, cardiovascular and respiratory diseases.
1.The diagnosis of pseudoexfoliation was established based on the presence of pseudexfoliative material on the pupillary border, on the anterior lens capsule, and the anterior chamber angle. 2.Intraocular hypertension was considered to be an ocular pressure value above 21 mm Hg. 3.Pseudoexfoliative glaucoma was considered to be the presence of pseudoexfoliation in an eye with intraocular hypertension and glaucomatous changes in the optic nerve head, verified by OCT examination.
In the further follow up, the patients were divided into two groups:
- Patients who did not present high values of ocular pressure, and without changes in the optic nerve, were considered normal subjects (T0), and were re-evaluated after 4 months (T1).
- Patients who presented with high ocular pressure values and glaucoma, were put on drug therapy (T0). They were re-evaluated after two weeks (T1), six weeks (T2), and then ten weeks after the start of therapy (T3).
The choice of the starting therapy was based on the values of ocular pressure, the degree of glaucomatous damage of the nerve, the patients' age, the evaluation of ocular adnexa for the presence of allergies and other surface diseases, as well as the presence or absence of systemic disease that are a contraindication to the use of certain classes of drugs. The target value of intraocular pressure was individualized based on the degree of glaucomatous damage and the patients' age. As a first line treatment, B blockers and carbonic anhydrase inhibitors were proposed; as second line of treatment prostaglandin analogues, and as third line of treatment alfa agonists. In patients in whom drug therapy was insufficient to reduce the pressure to acceptable values, trabeculectomy was proposed.
The statistical study was done with SPSS25. Techniques used were: Crosstab, Chi –Square test, Median, Standart Deviation, MIN and MAX values, T Test, Paired Sample T and Binary logistic regression.
3. Results
A. Part One
In total, the number of patients diagnosed with pseudoexfoliation was 92 patients. A demographic breakdown of the sample was performed to better understand the association and distribution of pseudoexfoliation in different groups.
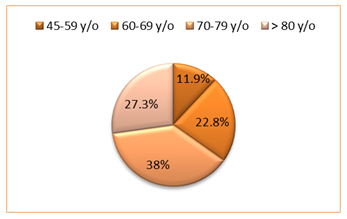
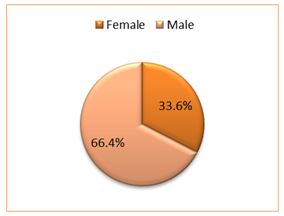
Patients were divided into age groups: 45-59 years; 60-69 years; 70-79 years; and over 80 years. In our control group, the age ranged from 50 years to 88 years, with a mean of 72 years (M=71.88, ds=9.26). Also, 61 patients were males (66.3%); while 31 were females (33.7%). To see if there were significant differences between genders in terms of mean age, we used the T-test. There were no statistically significant differences between genders, since the p-value was greater than .05. (p>.05) The result showed that the mean age among women was (M=72.48, ds=8.32) and among men (M=71.57, ds=9.75). Also, the percentage of men was higher than that of women for each age group.
|
Age group |
45-59 y/o |
60-69 y/o |
70-79 y/o |
>80 y/o |
|
Nr.of males |
9 |
13 |
23 |
16 |
|
% of males |
81.80% |
61.90% |
65.70% |
64% |
|
Nr.of females |
2 |
8 |
12 |
9 |
|
% of females |
18.20% |
38.10% |
34.30% |
36% |
|
Total |
11 |
21 |
35 |
25 |
Table 1: Crosstabulation gender-age
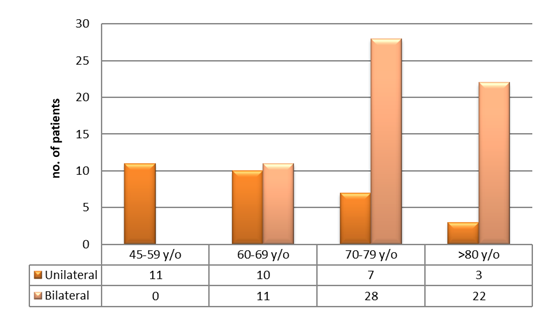
Furthermore, unilateral findings of pseudoexfoliation material was observed in 31 patients (33.7%), and bilateral in 61 patients (66.3%). In the 45-59 year old group, 11 patients (100%) had unilateral findings; in the 60-69 year old group, 10 patients (47.6%) had unilateral deposits, while 11 (52.4%) had bilateral deposits; in the 70-70 year old group, 7 patients (20%) had unilateral deposits, and 28 (80%) had bilateral deposits; in the over 80 year old group, 3 patients (12%) had unilateral deposits, and 22 or 88% had bilateral deposits.
To see if there were significant differences between laterality in terms of mean age, we used the T-test. We concluded that statistically significant differences appeared between laterality since the p value was less than .05. (p<.05). The result showed that the mean age in patients with bilateral distribution is higher (M=75.33, ds=6.76), compared to patients with unilateral distribution with the mean age (M=65.1, ds=9.84).
The main features associated with pseudoexfoliative syndrome were determined. In our study, there were a total of 154 eyes (from 92 patients).
Table 2: Clinical features of patients with pseudoexfoliation
|
Clinical features |
N (%) |
|
Material on the anterior capsule |
125 (81.1%) |
|
Material on the pupillary border |
132 (85.7%) |
|
Structural anomalies of the iris |
10 (6.4%) |
|
Poor dilation |
107 (69.4%) |
|
Cataract |
131 (85.0%) |
|
Elevated intraocular pressure |
72 (46.7%) |
|
Open angle glaucoma |
39 (25.3%) |
|
Closed angle glaucoma |
0(0%) |
B. Part Two
a. Patients without changes in intraocular pressure
In patients diagnosed with pseudoexfoliation, 51 of them (55.4%) did not present increased values of intraocular pressure or glaucomatous changes of the optic nerve head. Among them, 34 or 66.7%, belonged to the male gender; while 17, or 33.3%, were female. The distribution was bilateral in 58.9% of cases (n=30), and unilateral in 41.1% of cases (n=21).
The value of the measured pressure at time T0 was Min=12 mm Hg, Max=19 mmHg, with a mean (M=15.8, ds=2.20). The value of the measured pressure at time T1 was Min=13 mm Hg, Max=19 mm Hg, with a mean (M=16.06, ds=1.71). Through the Paired Sample Test, based on the significance p we concluded that there were no statistically significant differences (t (df=50) = 1.652, p>.05) between the results at time T0 and time T1 (M=0.25, ds=1.10) with a confidence interval CI [-.05 ; .56].
b. Patients with ocular hypertension and pseudoexfoliative glaucoma
Among the patients diagnosed with pseudoexfoliation, 41 of them (or 44.6%) presented increased values of intraocular pressure and/or glaucomatous changes of the optic nerve papilla.
Eighteen (18) of the patients presented increased values of intraocular pressure, without glaucomatous changes in the optic nerve (43.9%). Among them, 3 patients had unilateral deposits (16.6%), while 15 patients (83.4%), had bilateral deposits. Glaucomatous changes were present in 23 of the patients, or 66.1%; where 7 had unilateral findings and 16 bilateral, respectively 30.4 % and 69.6%. In total, 65.9% belonged to the male gender; while 34.1%, were female.
We used multivariate binary logistic regression analysis using three predictors (age, gender, and laterality) to predict glaucoma status. The entire model was significant (χ2 (3) = 8.843, p < 0.001). The model also showed evidence of good fit with nonsignificance of the Hosmer–Lemeshow test (χ2 (8) = 4.710, p = .788). Age and laterality were shown to be significantly associated with the presence of glaucoma in patients with PXF. Patients with bilateral involvement were 4.788 times more likely to have glaucoma (odds ratio [OR] 4.79) than patients with unilateral involvement. While older age was less associated with glaucoma (OR 0.930). Gender was not a predictor of glaucoma (p>.05).
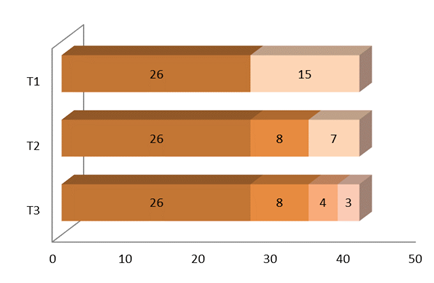
c. Follow up and target intraocular pressure
Intraocular pressure measurements after the start of therapy were performed at three different times. At time T1, 26 patients (63.4%) had reached target pressure, compared to 15 other patients (36.6%). At T2, after appropriate modifications in therapy, the pressure was at target values in 34 patients (82.9%). The pressure was still at high values in 7 patients (17.1%). At T3,3 patients (7.3%) were not yet at target values, and were considered candidates for trabeculectomy.
d. Therapy and target values
In the studied patients, 31.7% achieved the target value with the use of two medications; 43.9% with three medications, and 7.3% with one medication. Meanwhile, 4 patients, or 9.8%, underwent trabeculectomy, where 3 of them (7.3%) had a decrease in pressure to target values, and one patient was given additional drug therapy. Three of the patients in the study still have high pressure values despite maximum therapy and are candidates for trabeculectomy.
All patients who underwent, or who are candidates for trabeculectomy, presented glaucomatous optic neuropathy to a significant degree. They constituted 38.8% of the total number of patients with PXG. It was found that among the patients who needed surgical intervention, 6 had unilateral involvement and 1 had bilateral involvement. This was a statistically significant difference p<0.001.
No significant reduction in intraocular pressure was observed in patients on 3-drug therapy to whom an α agonist was added.
Table 3: Results after established treatment of choice for target pressure values
|
Type of treatment |
No. of patients |
% |
|
One type of drop |
3 |
7.30% |
|
Two types of drops |
13 |
31.70% |
|
Three types of drops |
18 |
43.90% |
|
Four Types of drops |
0 |
0% |
|
Trabeculectomy |
3 |
7.30% |
|
Trab+ drug therapy |
1 |
2.50% |
|
Candidate for trabeculectomy |
3 |
7.30% |
|
Total |
41 |
100% |
4. Discussion
Pseudoexfoliation is an important finding in the daily practice of the ophthalmologist, often presenting significant morbidity and diagnostic and therapeutic challenges. There is much debate about the prevalence of pseudoexfoliation in different populations, and these data also vary within countries [1]. Many of these variations occur either as a result of a real difference in prevalence between populations, differences in age/sex distribution within the studied population, adding various exclusion factors, or the difficulty in diagnosing early forms [2]. In our study, 92 cases of patients with pseudoexfoliation were diagnosed for the first time during the several-month period in which the study was conducted. This study though presented some limitations in assessing the prevalence of the disease, due to the small population group, the limited study time, and the inclusion in the study of only cases diagnosed for the first time with ocular hypertension and/or pseudoexfoliative glaucoma.
Pseudoexfoliation is considered a disease of the elderly, and these data are consistent with the results of various studies, which demonstrate that the prevalence increases with age [3,4]. The mean age in our study was 71.88 years, similar to the results of studies in Iceland (mean age 72 years) [5] and in the Framingham study (mean age 72.2 years) [6]. In the Framingham Eye Study, the prevalence of pseudoexfoliation was 1.8%. The prevalence rate increased from 0.6% for ages 52 to 64; to 2.6% for ages 65 to 74; to 5.0% for ages 75 to 85. This progressive increase in incidence was also evident in our study.
Our study showed a male predominance of 66.3%, compared with 33.7% for females. Worldwide, there are mixed reports on the prevalence of pseudoexfoliation between the sexes. Women were more affected than men in the Reykjavik Eye Study in Iceland [5], and in the Framingham Eye Study [6]. On the other hand, studies in Greece [7], Iran [8], and Turkey [9], have shown the opposite.
Statistically significant differences in laterality between age groups were observed in our study, with a linear increase in the percentage of bilateral findings of PXF deposits with increasing age. This is explained by the fact that pseudoexfoliation is a progressive disease and the deposits in the eye increase over time. Although pseudoexfoliation may be clinically present in only one eye, electron microscopy can reveal exfoliative material in the conjunctiva and iris of clinically uninvolved eyes [10].
In the second part of our study, patients without increased pressure and without changes in the optic nerve head, constituted 55.4% of the total number. No significant increase in pressure values was observed in both measured times. To date, there is no evidence to suggest that patients with pseudoexfoliation, but with normal intraocular pressure values, need monitoring or special measures to prevent the development of glaucoma [11]. However, the progressive nature of the disease raises the need for follow-up of patients, to enable timely detection and initiation of antiglaucomatous therapy in the at-risk population.
Patients with intraocular hypertension and/or glaucomatous changes accounted for 44.6% of the total number of patients. Among them, 18 patients had only high pressure, while 23 (25% of the total number) had pseudoexfoliative glaucoma. These values are relatively high, compared with the results of several other important studies that have evaluated the presence of glaucoma in patients with pseudoexfoliation (15.2% Thessaloniki Eye Study [12]; 14.2% Blue Mountains [13]; 12.0% Rejkjavik Eye Study [5]). Not all patients with high intraocular pressure will develop glaucoma in the future, but numerous studies have shown that the presence of pseudoexfoliation is an additional risk factor for the development of glaucoma, leading to the need to start antihypertensive therapy in cases with intraocular hypertension, even without optic nerve damage. Because of this, the patients in our study were put on antihypertensive therapy, regardless of whether they had glaucomatous neuropathy or not. A large hospital cohort study in Sweden compared the rate of glaucoma conversion in patients with IOP with and without pseudoexfoliation over a 5-year period. At the end of the study, the rate of glaucoma conversion was twice as high in patients with hypertension and pseudoexfoliation, as in control patients, for the same values of intraocular pressure, age, and sex. Thus, pseudoexfoliation was found to be a significant independent risk factor for glaucoma conversion in patients with intraocular hypertension [14].
Pseudoexfoliative glaucoma is characterized by high intraocular pressure and fluctuations in 24-hour pressure values. To minimize progression, the treatment should ensure a long-term target pressure and good control of 24-hour pressure. Also it is a more aggressive form of glaucoma than other types. Due to its progressive nature and the production of continuous deposition of material in the trabecular meshwork, glaucoma that has been well-managed for some time may suddenly decompensate and be associated with increased tension and further damage to the optic nerve. To achieve these goals, fixed-dose topical eye drops, or various forms of surgery, should be considered in the long-term management of the disease. Despite the aggressive and often refractory course, drug therapy has been chosen as the first line of treatment. According to the literature, initial drug management with available agents and combinations of them as needed is usually effective in reducing intraocular pressure [15-17]. Often, eyes with pseudoexfoliative glaucoma respond poorly to medical therapy and require surgical therapy [18,19]. Trabeculectomy has proven to be a successful intervention in the adequate management of the disease.
5. Conclusion
Pseudoexfoliation is an age related disease, often detected incidentally, in a patient who usually presents with decreased vision, sometimes caused by other age-related ocular diseases. The most typical finding is the presence of white fibrillar material on the anterior lens capsule, or on the pupillary margin. These findings may be asymptomatic, but are often associated with other complications such as ocular hypertension, glaucoma, cataract with zonular instability and phacodonesis, posterior synechiae, etc. Pseudoexfoliative glaucoma is the leading cause of vision loss in patients with pseudoexfoliation . It is characterized by high values of tension, frequent fluctuations during 24 hours and faster progression of optic nerve damage. These patients need more aggressive combined therapy to keep the ocular tension under control. Also, antiglaucomatous surgeries are performed more frequently in these patients. Due to the chronic and progressive nature of the production and deposition of pseudoexfoliative material in the ocular structures, a well-controlled glaucoma can later decompensate. Therefore, these patients need regular routine check-ups to monitor the therapy and the progression of the optic neuropathy, in order to enable adequate drug or surgical treatment.
Acknowledgement
None
Disclosures
None.
References
- Konstas AGP, Ringvold A. Epidemiology of exfoliation syndrome. J Glaucoma 27 (2018): S4–11.
- Ritch R. Exfoliation syndrome. Curr Opin Ophthalmol 12 (2001): 124–130.
- Cashwell LF, Shields MB. Exfoliation syndrome in the southeastern United States I.Prevalence in open –angle glaucoma and non- glaucoma Populations. Acta Ophthalmol 184 (1988): 99–102.
- McCarty CA, Taylor HR. Pseudoexfoliation syndrome in Australian Adults. Am J Ophthalmol 129 (2000): 629–633.
- Hiller R, Sperduto RD, Krueger DE. Pseudoexfoliation, intraocular pressure, and senile lens changes in a population-based survey. Arch Ophthalmol 100 (1982):1080–1082.
- Kozobolis VP, Papatzanaki ME, Vlachonikolis IG, et al. Epidemiology of pseudoexfoliation in the island of Crete (Greece). Acta Ophthalmol Scand 75 (1997): 726–729.
- Nouri-Mahdavi N, Sahebghalam R, Jahanmard M. Pseudoexfoliation syndrome in central Iran: a population-based survey. Acta Ophthalmol Scand 77 (1999): 581–584.
- Yalaz M, Othman I, Nas K, et al. The frequency of pseudoexfoliation syndrome in the Eastern Mediterranean area of Turkey. Acta Ophthalmol 70 (1992): 209–213.
- Kivwlä T, Hietanen J, Uusitalo M. Autopsy analysis of clinically unilateral exfoliation syndrome. Invest Ophthalmol Vis Sci 38 (1997): 2008–2015.
- Anastasopoulos E, Founti P, Topouzis F. Update on pseudoexfoliation syndrome pathogenesis and associations with intraocular pressure, glaucoma and systemic diseases. Curr Opin Ophthalmol 26 (2015): 82–89.
- Topouzis F, Harris A, Wilson MR, et al. Increased likelihood of glaucoma at the same screening intraocular pressure in subjects with pseudoexfoliation: the Thessaloniki Eye Study. Am J Ophthalmol (2009).
- Mitchell P, Wang JJ, Hourihan F. The relationship between glaucoma and pseudoexfoliation: the Blue Mountains Eye Study. Arch Ophthalmol 117 (1999): 1319-1324.
- Grødum K, Heijl A, Bengtsson B. Risk of glaucoma in ocular hypertension with and without pseudoexfoliation. Ophthalmology 112 (2005): 386-390.
- Desai MA, Lee RK. The medical and surgical management of pseudoexfoliation glaucoma. Int Ophthalmol Clin 48 (2008): 95–113.
- Konstas AGP, Mylopoulos N, Karabatsas CH, et al. Diurnal intraocular pressure reduction with latanoprost 0.005% compared to timolol maleate 0.5% as monotherapy in subjects with exfoliation glaucoma. Eye 18 (2004): 893–899.
- Parmaksiz S, Yüksel N, Karabas VL, et al. A comparison of travoprost, latanoprost, and the fixed combination of dorzolamide and timolol in patients ëith pseudoexfoliation glaucoma. Eur J Ophthalmol 16 (2006): 73-80.
- Konstas AG, Allan D. Pseudoexfoliation glaucoma in Greece. Eye 3 (1989): 74–753.
- Klemetti A. Intraocular pressure in exfoliation syndrome. Acta Ophthalmol Suppl 184 (1988): 54–58.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
