Refractive Status of diabetic patients at Bangladesh Medical University (BMU)
Shams Mohammed Noman1*, Rajashree Das2, Mohammad Afzal Mahfuzullah3, Mehjabin Haque4, Tajmeh Mehtaj5.
1Associate Professor Department of Ophthalmology, BMU, Dhaka, Bangladesh
2Assistant Professor, Department of Ophthalmology, BMU, Dhaka, Bangladesh
3Associate Professor, Department of Ophthalmology, BMU, Dhaka, Bangladesh
4Assistant Professor, Department of Ophthalmology, BMU, Dhaka, Bangladesh
5Assistant Professor, Department of Community Ophthalmology, BMU, Dhaka, Bangladesh
*Corresponding author: Shams Mohammed Noman, Associate Professor Department of Ophthalmology, BMU. E-mailid: drshams_noman@yahoo.com
Received: 25 June 2025; Accepted: 30 June 2025; Published: 04 July 2025.
Article Information
Citation: Shams Mohammed Noman, Rajashree Das, Mohammad Afzal Mahfuzullah, Mehjabin Haque, Tajmeh Mehtaj. Refractive Status of diabetic patients at Bangladesh Medical University (BMU) Journal of Ophthalmology and Research. 8 (2025): 34-38.
DOI: 10.26502/fjor.2644-002400103
View / Download Pdf Share at FacebookAbstract
Background: In Bangladesh, where diabetes affects millions of adults, understanding the refractive status of diabetic patients is vital for improving eye care and preventing avoidable vision loss. Aim: To assess the refractive status of diabetic patients by identifying the prevalence and types of refractive errors and evaluating their association with blood glucose levels. Additionally, it seeks to determine the impact of diabetes on visual acuity and the effectiveness of refractive correction. Methods: This cross-sectional study at BMU's Ophthalmology Department assessed refractive status in 200 adult diabetic patients (simple random sampling). Diabetic status was biochemically confirmed. Refractive errors were measured via objective and subjective techniques, followed by bestcorrected visual acuity. Diabetic control was recorded. Data was analyzed using SPSS 26, employing descriptive statistics, correlation, and linear regression. Results: Among the 200 diabetic patients studied, 53.5% were male and 46.5% female. The most frequent visual complaint, 58.5%, was blurred vision for both near and distance. Notably, 62% of participants exhibited poor glycemic control. Simple myopia was the predominant refractive error in both right 41.5% and left 42.5% eyes, followed by hyperopia 37.5% and 36.5%. A strong positive correlation was found between myopia and nuclear sclerosis r=0.73, with regression analysis indicating that 52% of nuclear sclerosis variability was explained by myopia. Significantly, 14.5% of right eyes and 13.0% of left eyes showed no visual improvement after refractive correction, suggesting co-existing diabetic ocular pathology. Conclusion: The findings of this study will help to identify high burden refractive errors in diabetic patients. Simple myopia and hypermetropia are utmost common and related with diabetic and lens changes. Numerous patients had compacted their visual acuity despite improvement, signifying basic diabetic eye complications. These findings highlight the necessity for regular refractive assessments as portion of diabetic eye care to allow early detection and recover visual outcomes in this helpless group.
Keywords
<p>Diabetes Malitus, Myopia, Hypermetropia, Retinoscopy, Astigmatism.</p>
Article Details
1. Introduction
Bangladesh faces a serious public health issue. Over 13 million people, about 10% of adults, have diabetes [1]. Diabetes changes the lens osmotically and causes refractive shifts that often go unnoticed [2]. Diabetic retinopathy and cataract are well known [3,4]. However, refractive errors like myopia, hyperopia, and astigmatism also impair vision. Assessing these errors is important to understand the refractive status of diabetic patients.
Globally, uncorrected refractive errors affect over 2 billion people. In South Asia, rates exceed 40%, especially in urban and diabetic groups [2,7]. In Bangladesh, 42.7% of adults have refractive errors: 22.1% myopia, 20.6% hyperopia, and 32.4% astigmatism [20]. In rural Sirajganj, 62% have presbyopia, and only 13% wear spectacles [21].
Refractive errors in diabetic populations show distinct patterns. Indian research reports a 60% prevalence of refractive errors in Type 2 diabetics over 40, with astigmatism (47.4%), hyperopia (39.7%), and myopia (19.4%). Higher glycemic levels were strongly associated with myopia (OR 4.15) and astigmatism (OR 2.01) [22].
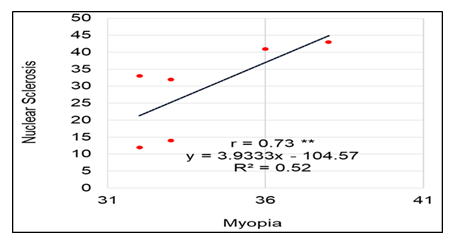
Lens opacity, especially nuclear sclerosis, is closely linked to myopic shifts. Our findings support this, showing a strong positive correlation between myopia and nuclear sclerosis (r=0.73, R²=0.52). Myopia may offer some protective effect, possibly due to biomechanical properties of the eye. This indicates a complex refractive and structural interplay in diabetic eye health [23].
In our study at BMU, we examined 200 diabetic patients. About 41–42% had simple myopia, 36–38% had hyperopia, and over 50% had both near and distance vision impairment. Poor glycemic control was seen in 62%, and 14–15% of eyes failed to improve with refractive correction, suggesting underlying ocular pathology. These findings highlight the need for thorough refractive and structural assessments, supporting our study aim [1,6].
Diabetes mellitus (DM) is a global health crisis with a rapidly rising prevalence [8]. The International Diabetes Federation (IDF) estimated that over 537 million adults had diabetes in 2021, a number projected to grow substantially [9]. Much of this burden lies in low- and middle-income countries, especially across Asia, where the Indian subcontinent is a major epicenter [9]. Bangladesh, a densely populated South Asian country, faces a rapid increase in diabetes prevalence, emphasizing the urgent need for effective prevention and management [11].
Diabetic retinopathy (DR) is a leading cause of preventable blindness in working-age adults worldwide [12]. Diabetes also accelerates cataract formation, especially nuclear cataracts, which further impairs vision [13]. Poor glycemic control and long diabetes duration are key risk factors for these complications [14].
While DR and cataract receive most attention, refractive changes are also common in diabetic patients and can signal early ocular involvement [15]. Blood glucose fluctuations alter the lens’s refractive index, causing transient myopic shifts during hyperglycemia or hypermetropic shifts after rapid glucose reduction [16]. Chronic hyperglycemia can lead to permanent refractive changes, including myopia, hypermetropia, astigmatism, and earlier presbyopia [17]. Identifying and correcting these errors is vital for improving vision and quality of life in diabetic patients [18].
In the Indian subcontinent, where diabetes is highly prevalent, studies on refractive status and its links with systemic diabetic parameters are still limited [19]. Existing research often focuses on diabetic retinopathy or cataract, leaving gaps in understanding refractive changes, their relationship with glycemic control and diabetes duration, and the effectiveness of refractive correction in Bangladeshi patients, especially at BMU [24]. Localized data like these can enhance clinical practice, improve screening, and support better ocular management in this region.
This study aims to assess the refractive status of diabetic patients at BMU by determining the prevalence and types of refractive errors and their associations with blood glucose levels. It will also evaluate the impact of diabetes on visual acuity and the effectiveness of refractive correction. The findings will provide valuable insight into diabetic ocular manifestations in Bangladesh and help inform better clinical care.
2. Methodology
This cross-sectional study was conducted at the Ophthalmology Department of BMU to assess the refractive status of adult diabetic patients. We recruited 200 diabetic patients of both genders who required refractive error correction, selected through simple random sampling. Diabetic status was confirmed using biochemical tests and clinical examination. Patients were excluded if they had significant ocular pathology unrelated to diabetes, a history of ocular trauma, or previous eye surgery affecting their vision. We used a structured, pretested data collection form to record demographic information, duration of diabetes, glycemic control status, and detailed refractive measurements. Glycemic control was determined by each patient’s most recent fasting blood glucose levels, with uncontrolled diabetes defined according to national guidelines. Refractive errors were measured using standard objective and subjective refraction techniques, followed by best-corrected visual acuity testing. Comprehensive slit-lamp and dilated fundus examinations were performed to detect diabetic eye complications and other anterior or posterior segment issues. Data was analyzed using Statistical Package for the Social Sciences (SPSS) version 26. We used descriptive statistics (frequencies, percentages, means, and standard deviations) to summarize sociodemographic, clinical, and refractive data. Correlation and linear regression analyses assessed the relationship between myopia and nuclear sclerosis.
3. Results
In the results segment we point the demographic features of the study population, the prevalence and forms of refractive errors detected, and their relations with diabetic control and diabetic duration. Important results are presented in the manuscript, added by data tables and figures for complete design and deeper understanding.
Table 1: Distribution of participants by type of vision decreases complaint and diabetes conditions (N=200).
|
Gender |
Frequency |
Percentage |
|
Male |
107 |
53.5 |
|
Female |
93 |
46.5 |
|
Vision Decrease |
||
|
Decrease near and distance vision in both eyes |
117 |
58.5 |
|
Decrease near vision in both eyes |
59 |
29.5 |
|
Decrease distance vision in both eyes |
24 |
12 |
|
Diabetes Conditions |
||
|
Controlled |
76 |
38 |
|
Uncontrolled |
124 |
62 |
Table 1 shows among the 200 diabetic patients, 53.5% were male and 46.5% were female, indicating a slightly higher male predominance. In terms of visual complaints, the majority 58.5% experienced both near and distance vision reduction, followed by 29.5% with only near vision loss and 12% with distance vision loss alone. Regarding glycemic control, 62% of the participants had uncontrolled diabetes, while only 38% maintained controlled blood glucose levels.
Table 2: Distribution of Duration of suffering in diabetes among the participants.
|
Age |
Frequency |
Percentage |
|
≤ 1 Years |
7 |
3.5 |
|
1-5 Years |
69 |
34.5 |
|
6-10 Years |
65 |
32.5 |
|
11- 15 Years |
34 |
17 |
|
16-20 Years |
16 |
8 |
|
≥20 Years |
9 |
4.5 |
Table 2 expresses the largest proportion of diabetic patients had been living with the condition for 1-5 years 34.5%, followed closely by those with 6-10 years of diabetes 32.5%. Only a small fraction 3.5% was newly diagnosed ≤1 year, and long-standing diabetes ≥20 years was present in just 4.5% of the cohort.
Table 3: Distribution of Refractive Condition in Right and Left eye of the patients suffering in diabetes
Conditions.
|
Conditions |
(a) Right Eye |
(b) Left Eye |
||
|
Frequency |
Percentage |
Frequency |
Percentage |
|
|
Myopia |
83 |
41.5 |
85 |
42.5 |
|
Hypermetopia |
75 |
37.5 |
73 |
36.5 |
|
Mixed astigramtism |
5 |
2.5 |
7 |
3.5 |
|
Vision was not improved after refraction |
29 |
14.5 |
26 |
13 |
|
Only Presbyopia |
8 |
4 |
9 |
4.5 |
|
Mayopic astigmatism with presbyopia |
||||
|
Compound myopic astigmatism |
19 |
9.5 |
19 |
9.5 |
|
Myopia astigmatism with presbyopia |
32 |
16 |
33 |
16.5 |
|
Simple myopia with presbyopia |
32 |
16 |
33 |
16.5 |
|
Hyperopic astigmatism with presbyopia |
||||
|
Compound hyperopic astigmatism with presbyopia |
38 |
19 |
36 |
18 |
|
Hyperopic astigmatism with presbyopia |
7 |
3.5 |
10 |
5 |
|
Simple Hyperopic with presbyopia |
30 |
15 |
27 |
13.5 |
Table 3 illustrates the most common refractive errors among diabetic patients were simple myopia (right eye: 41.5%, left eye: 42.5%) and hypermetropia (right eye: 37.5%, left eye: 36.5%). Compound and mixed forms of astigmatism with presbyopia were also frequently observed, particularly compound hyperopic astigmatism with presbyopia (right eye: 19.0%, left eye: 18.0%). A notable percentage of patients (14.5% in the right eye, 13.0% in the left eye) did not experience vision improvement after refraction, indicating possible underlying diabetic ocular complications beyond refractive error.
Figure 1: Correlation and regression between the Myopia and nuclear sclerosis. Here, ** represents 1% level of significance.
Figure 1 shows the analysis revealed a strong, positive, and statistically significant correlation between myopia and nuclear sclerosis (r = 0.73). The linear regression equation (y = 3.9333x – 104.57) indicates that as the severity of myopia increases, the grade of nuclear sclerosis also rises, with each one-unit increase in myopia corresponding to an average 3.93-unit increase in nuclear sclerosis. The coefficient of determination (R² = 0.52) suggests that approximately 52% of the variability in nuclear sclerosis can be explained by variations in myopia.
4. Discussion
This study provides a detailed assessment of refractive errors and their associations with diabetes control among diabetic patients attending BMU. Our findings highlight a substantial burden of refractive errors in this cohort, with simple myopia and hypermetropia being the most common types in both eyes. Nearly 42% of patients had myopia and 37% had hypermetropia, and compound astigmatism with presbyopia was also prevalent. These findings align with global patterns, where refractive errors remain a leading cause of visual impairment¹ and are notably higher in diabetic populations [2].
The demographic profile showed a slight male predominance 53.5%, and most patients experienced both near and distance visual complaints, supporting the idea that diabetic lens changes and metabolic instability contribute to significant refractive fluctuations [1, 5, 16]. This was further supported by our observation that 62% of the patients had uncontrolled diabetes, suggesting that hyperglycemia plays a critical role in refractive instability and visual complaints [11, 14]. Poor glycemic control has been consistently linked with increased risk of refractive changes and progression of diabetic ocular complications in prior research [18] especially as osmotic changes in the lens during hyperglycemia can cause transient myopic shifts [16, 22].
The present findings also revealed that a notable proportion of patients 14.5% right eye; 13.0% left eye did not show visual improvement with refractive correction. This indicates the presence of other diabetic ocular pathologies such as diabetic maculopathy or early lens opacity beyond refractive errors alone. Similar observations have been reported by Golubovik et al. [23] and Ivanescu et al. [12], who described a substantial overlap between diabetic retinopathy, cataract formation, and unpredictable refractive status. Moreover, the strong positive correlation between myopia and nuclear sclerosis (r=0.73, R²=0.52) supports the well-documented pathophysiological link between lens opacification and myopic shift [13, 15]. This agrees with findings by Gurav et al. [22] who noted that hyperglycemia and lens opacity contribute to increased myopia in diabetic patients, while Tang et al. [7] and Morgan & Rose [23] also observed similar age and diabetes-related refractive patterns.
In our cohort, most patients had a history of diabetes between 1 and 10 years, with only 4.5% having diabetes for ≥20 years. This relatively shorter duration might explain the lower rates of advanced diabetic retinopathy and its direct impact on refractive status. Nevertheless, the findings still highlight the progressive nature of diabetic ocular complications and the need for early intervention. Our results are consistent with prior observations that refractive errors worsen with both increasing diabetes duration and poor glycemic control [20, 21].
This study underscores the importance of comprehensive ocular assessments in diabetic care that include careful refraction, and fundoscopic evaluation. Accurate refractive correction is a vital, often overlooked part of preventing vision impairment and improving the quality of life in diabetic patients [18]. Early detection of refractive errors, especially myopic shifts and presbyopic changes, is a practical and cost-effective way to enhance vision, facilitate timely referral, and prevent further complications [15, 17].
Our findings add to the regional evidence base, filling a knowledge gap for diabetic patients in Bangladesh [11]. They support the broader literature on diabetic eye health in South Asia and suggest that tailored screening protocols including refraction checks should be integrated into routine diabetic care across the region [8, 9]. Future research could explore longitudinal refractive changes and evaluate the effectiveness of glycemic control interventions in mitigating visual impairment in diabetic populations.
5. Conclusion
Diabetic patients attending BMU exhibit a high burden of refractive errors, with significant associations between refractive status and diabetis. Addressing these refractive errors alongside diabetic retinopathy and cataract could significantly reduce visual disability in diabetic patients and improve overall diabetic eye care in Bangladesh.
Declaration of Interest Statement:
The authors declare no competing interests.
Conflict of Interest: No Conflict of Interest.
Authors Contributions:
Dr Shams Md Noman conceptualized the study and designed the methodology. Rajashree Das and Mehjabin Haque contributed data management and Tajmeh Mehtaj contributed to statistical analysis. Mohammad Afzal Mahfuzullah assisted in manuscript drafting and critical revisions. Dr Shams Md Noman supervised the research and provided final manuscript approval. All authors reviewed and approved the final version.
References
- GBD 2019 Eye Conditions Collaborators. Global burden of refractive disorders. BMC Public Health 21 (2021): 11648.
- Bhutia KL. Refractive errors in East Sikkim. Indian J Ophthalmol 69 (2021): 2018–2020.
- Wikipedia contributors. Diabetes in Bangladesh (2025). en.wikipedia.org/wiki/Diabetes_in_Bangladesh
- Wikipedia contributors. Health in Bangladesh (2025). en.wikipedia.org/wiki/Health_in_Bangladesh
- Wikipedia contributors. Myopia (2025). en.wikipedia.org/wiki/Myopia
- Wikipedia contributors. Visual Impairment (2025). en.wikipedia.org/wiki/Visual_impairment
- Tang Y. Age-related refractive disorder patterns in China. BMC Public Health 21 (2021): 22440.
- Magliano DJ, Boyko EJ; IDF Diabetes Atlas 10th edition scientific committee . IDF DIABETES ATLAS [Internet]. 10th edition. Brussels: International Diabetes Federation; (2021).
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 43 (2020): S14-S31.
- Pradeepa R, Deepa R, Mohan V. Epidemiology of diabetes in India--current perspective and future projections. J Indian Med Assoc 100 (2002): 144-148.
- Akhtar S, Nasir JA, Sarwar A, et al. Prevalence of diabetes and pre-diabetes in Bangladesh: a systematic review and meta-analysis. BMJ Open 10 (2020): e036086.
- American Diabetes Association. Microvascular complications and foot care: Standards of medical care in diabetes 2023. Diabetes Care 46 (2023): S197-S208.
- Ivanescu A, Popescu S, Gaita L, et al. Risk Factors for Cataracts in Patients with Diabetes Mellitus. J Clin Med 13 (2024): 7005.
- Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and the development of long-term complications in type 1 diabetes mellitus. New England J Med 384 (2021): 1324-1335.
- Al-Hadidy A, Al-Ani H, & Al-Qaysi M. Refractive error changes in diabetic patients. Oman Med J 37 (2022): e316.
- Arora T, Bansal R, Gupta P. Correlation of blood glucose levels with refractive error in diabetic patients. International J Contemporary Med Res 8 (2021): A1-A4.
- Refractive error patterns in patients with type 2 diabetes mellitus in a Nigerian tertiary hospital. Nigerian J Ophthalmology 29 (2020): 79-84.
- World Health Organization. World report on vision. Geneva: World Health Organization (2021).
- Khandekar R, Al-Bdour M, & Al-Amri Prevalence of diabetes and diabetic retinopathy in Oman: A population-based study. Oman J Ophthalmology 13 (2020): 79-86.
- Bourne RRA. National Blindness & Low Vision Survey, Bangladesh. Ophthalmology 111 (2004): 1150–1160.
- Kuper H. Rapid assessment of refractive error in Sirajganj. Ophthalmic Epidemiol 25 (2018): 338–346.
- Gurav YK. Refractive errors in Type 2 DM (SN-DREAMS report 18). Ophthalmology 117 (2010): 2078–2084.
- Morgan I, & Rose K. Epidemiology of myopia. The Lancet 379 (2014): 1497–1500.
- Golubovik M. Retinal complications in diabetes mellitus: importance of screening and management. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 35 (2014): 167-173.


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
