Study on Ocular Surface Changes in Patients with Unilateral Pterygium Compared to their Normal Eye
Nirupama Damarla, Hymavathi Bommisetti, Madhavi Chevuturi, Sanjay Reddy Tadisina, Satyanarayana Reddy, Likitha P
Apollo Hospitals Educational & Research Foundation, Hyderabad
*Corresponding author: Nirupama Damarla, Apollo Hospitals Educational & Research Foundation, Hyderabad
Received: 11 September 2025; Accepted: 19 September 2025; Published: 26 September 2025.
Article Information
Citation: Nirupama Damarla, Hymavathi Bommisetti, Madhavi Chevuturi, Sanjay Reddy Tadisina, Satyanarayana Reddy, Likitha P. Study on Ocular Surface Changes in Patients with Unilateral Pterygium Compared to their Normal Eye. Journal of Ophthalmology and Research. 8 (2025): 53-57.
DOI: 10.26502/fjor.2644-002400106
View / Download Pdf Share at FacebookAbstract
Background: The purpose of our study was to estimate the variations between TBUT (Tear film breakup time) Schirmers test (ST)value and MGD(Meibomian gland dysfunction) between a normal eye and an eye with pterygium. Methods: 50 patients with unilateral pterygium were enrolled in our study. TBUT, ST measurements, MGD and conjunctival congestion were evaluated. The results were compared between eyes with pterygium (Cases)and normal eyes of the same patient (controls). Pterygium was graded based on the length of limbal invasion into 3 grades. We have also evaluated the relationship between grades of pterygium and TBUT and Schirmer I test . Results: The mean TBUT in cases(eyes with pterygium) was 5.16±1.89 seconds and the mean TBUT in controls(eyes without pterygium) was 7.00±1.47 seconds . The mean wetting length of Schirmer’s strip was 10.96±3.51mm in cases and 13.90±4.5 mm in controls. Schirmer’s test was statistically significant between the eyes with pterygium and eyes without pterygium with P < 0.0001. In patients with pterygium 36% had MGD (Meibomian gland dysfunction) of varying severity whereas 26.5% of eyes without pterygium had MGD. There was no association of MGD between eyes with pterygium and the eyes without pterygium. Conclusion: Our study has shown that TBUT and Schirmers test values have an association with pterygium.
Keywords
<p>Unilateral Pterygium, TBUT, Schirmers test, Meibomian gland dysfunction.</p>
Article Details
1. Introduction
Pterygium is one of the most common ocular surface disorders. Pterygium is mostly observed on the nasal aspect in the interpalpebral area. Pathologically pterygium is an elastotic degeneration of the subconjunctival tissue. Destruction of Bowman layer by fibrovascular ingrowth is typically seen when pterygium encroaches on to the cornea. There is a wide variation of prevalence of pterygium world wide.It ranges between 0.3 to 29% [1].The prevalence of pterygium in India ranges between 9.5 to 13% [2].The prevalence varies in different countries ranging from 10.1% in Singapore to 30.8% in Japan [3,4,5].
Several risk factors are attributed to pterygium such as age, male gender, illiteracy, greater outdoor activity, rural residence, dark complexion of skin and smoking. The prevalence of pterygium more commonly seen(10 times more than other areas) in regions 40° latitude around the equator [6]. This supports the role of ultraviolet(UV) radiation in the pathogenesis of pterygium. The limbal stem cells are damaged by the UV rays that cause conjunctivalization of the cornea. Mutations may occur in the p53 tumor suppressor gene due to UV rays. This can cause abnormal conjunctival epithelium resulting in pterygium [7,8]. Pterygium could also be an area where there is deficiency of limbal stem cells, that results in a invasion of conjunctival epithelium into the cornea [9].
Though UV rays exposure is equal in both the eyes we often see unilateral pterygium in patients. This suggests that factors other than UV light might also have a role in etiology of pterygium. In a study done by Li et al. there were decrease in conjunctival goblet cell population, disturbances in quality and quantity of tear film in population with pterygium [10].
Need for study: This study compares ocular surface changes in an eye with pterygium to a normal eye (without pterygium) in the same patient for the first time. This helps the ophthalmologists to tailor their treatment based on the changes of ocular surface. Our study aimed to assess ocular surface changes in patients with unilateral pterygium.
2. Materials and Methods
This was a non- interventional, observational study on 50 patients. Approval was obtained from ethics committee. Informed consent was taken from the study group after explaining the procedure and the requirement for the study . The sample size was calculated based on previous studies.
Patients coming to the Department of Ophthalmology with unilateral pterygium during the period of study were taken into the study. Patients who were using contact lenses, those who underwent ocular surgery in the last 6 months, those using artificial tear supplements, patients with corneal abnormalities , patients with allergic conjunctivitis and any condition causing dry eye due to systemic disease were excluded from the study. In the study group after taking readings from automated refractometer (AR) refraction was done wherever necessary. The type and the amount of astigmatism was recorded. A thorough slit lamp evaluation was done for the patients. Pterygium was graded based on the length of limbal invasion into 3 grades. Grade 1: length of limbal invasion between 0-2mm.Grade 2: length of limbal invasion between 2-4mm.Grade 3: length of limbal invasion more than 4mm [11]. CCT (Central corneal thickness) measurement was done using pachymetry.
Tear film was evaluated by measuring TBUT and Schirmer test.
TBUT: A fluorescein strip was moistened with saline. The surface of the eye was then stained with fluorescein. The patient is instructed to blink gently and open their eyes. The initial dry spot on the corneal surface is observed under a cobalt blue filter of the slit lamp. TBUT is the time, in seconds, between the last blink and the appearance of dry spots.
Schirmer test: The test is done using Schirmer test strips
(Whatman filter strips). Each strip is bent at 90°. The patient is asked to look up.The strip is placed between lateral 1/3rd and medial 2/3rd of the lower lid.
After placing both the strips , the patient is instructed to close both eyes for five minutes. Then after 5 minutes the Whatman filter schirmer’s strips were removed.
The length of the strips moistened by the tears of the patient in millimeters is taken as the test score.
Keratometer was used to measure the anterior corneal curvature (K1 and K2)and the axis and extent of astigmatism. Meibomian glands were examined to rule out Meibomian Gland Dysfunction (MGD) . In both the eyes, Meibomian glands obstruction and quality of secretions were evaluated under slitlamp. Mild pressure was applied on the central five meibomian glands of the lower eyelid . If there was no obstruction to the Meibomian glands ,it was classified as No Obstruction, if 1–2 glands were obstructed-Mild MGD, 3–4 glands obstructed- Moderate MGD and if all the 5 glands were obstructed -Severe MGD [12].
Statistical analysis: The data was then represented as the means ± standard deviation.t-Test was performed to compare the mean values of TBUT ansd Schirmers test across the groups.ANOVA with post hoc test of least significance difference(LAD)method was applied across the gredes.Statistical analyses were performed using SPSS Windows version 24.0. A p-value of less than 0.05 was considered statistically significant.
3. Results
This study was done on 50 patients who had pterygium unilaterally. Of them 27 were males (54%) and 23 were females (46%) .(Table.1)
Table 1: showing gender distribution.
|
Gender |
Number |
Percentage |
|
Females |
23 |
46% |
|
Males |
27 |
54% |
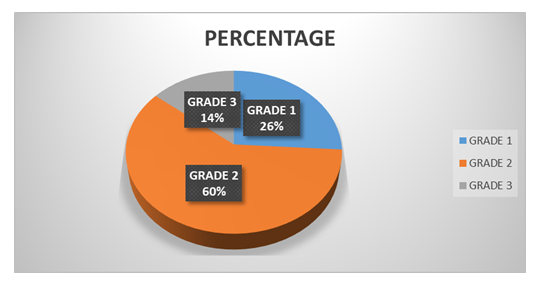
26% of the patients had Grade 1 pterygium, 60% patients had pterygium of Grade 2 and 14% patients had Grade 3 pterygium. (Figure.1).
A discriminate function analysis was done. The order and the best set of variable that were differentiated between cases and controls were TBUT and Schirmer’s test.
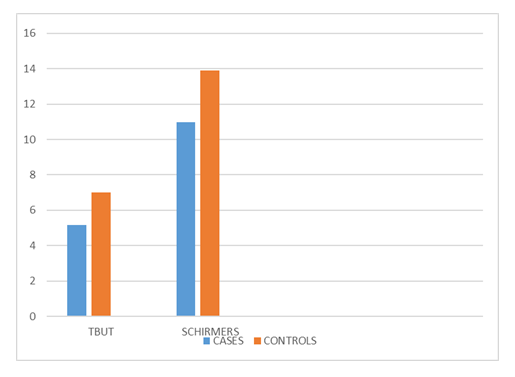
The mean TBUT in cases (eyes with pterygium) was 5.16±1.89 seconds and the mean TBUT in controls(eyes without pterygium) was 7.00±1.47 seconds . (Table.2).
Table 2: Comparison of TBUT and Schrimers test between eyes with Pterygium and eyes without Pterygium.
|
Test |
Cases |
Controls |
P value |
|
TBUT |
5.16±1.89 SEC |
7.00±1.47 SEC |
<0.001 |
|
Schrimers |
10.96±3.51 MM |
13.90±4.52 MM |
< 0.001 |
TBUT was statistically significant between cases i.e., the eyes with pterygium and eyes without pterygium i.e., controls with P < 0.0001. Mean TBUT value in Grade 1 pterygium was 6.2±3.21 seconds ,while it was 8.0±3.31 seconds and 5.1± 2.85 seconds in Grade 2 and Grade 3 Pterygium.(Table.3)
Table 3: TBUT and Schrimers test values based on the grades of Pterygium.
|
Grades of Pterygium |
TBUT |
Schirmers |
|
Control Eye |
9.2a±3.14 sec |
11.8a±4.88 mm |
|
Grade 1 |
6.2bc±3.21 sec |
9.3abc±3.48 mm |
|
Grade 2 |
8.0ab±3.31 sec |
9.1bc±4.53 mm |
|
Grade 3 |
5.1c±2.85 sec |
7.0c±3.42 mm |
(Variations in superscripts indicate significance (p<0.05) mean differences across grades.)
The mean wetting length of Schirmer’s strip was 10.96±3.51mm in cases and 13.90±4.5 mm in controls. (Figure 2).
Schirmer’s test was statistically significant between the eyes with pterygium and eyes without pterygium with P < 0.0001.
Mean Schirmer’s test value in Grade 1 pterygium was 9.3±3.38 mm, while it was 9.1±4.53 mm and 7.0±3.42mm in Grade 2 and Grade 3 Pterygium. Inferences were similar in non parametric test of Kruskal-Wallis-H test.(Table.2).
In patients with pterygium 36% had MGD (Meibomian gland dysfunction) of varying severity whereas 26.5% of eyes without pterygium had MGD. There was no association of MGD between eyes with pterygium and the eyes without pterygium.
The mean CCT in cases was 525±32 µm and in controls it was 529±29 µm.The average keratometry readings in cases were 43.67±1.53 K1 and 43.78± 1.31 K2. The average keratometry readings in controls were 43.72±1.38 K1 and 43.74± 1.40 K2.
4. Discussion
Pterygium is one of the most common ocular disease encountered in patients especially in those people living near equator. Though exposure to ultraviolet radiation is hypothesised as an important factor in etiopathogenesis of pterygium. But not all people living in the same environment develop pterygium. Also, pterygium is sometimes unilateral presenting only in one eye of an individual. This suggests that there could be other etiological factors in the development of pterygium.
The study focused on patients diagnosed with unilateral pterygium. The eyes that had pterygium was considered as ‘Case’ and the normal eye was taken as ‘Control’.
Most of the patients had Grade 2 pterygium .The symptoms of grittiness ,foreign body sensation were complained more frequently in patients with grade 2 and grade 3 pterygium when compared to grade 1 pterygium.
The eyes with pterygium had lower Schirmer test value and TBUT value when compared to the normal fellow eye with mean TBUT value of 5.16±1.89 seconds in cases and 7.00±1.47 seconds in controls with P value < 0.0001. The mean wetting length of Schrimers strip was 10.96±3.51mm in cases and 13.90±4.5 mm in controls with P value < 0.001.
In a study done by Ishioka et al., [13] and Ozsutcu et al.on evaluation of dry eye in unilateral pterygium patients T-BUT values were lower in eyes with pterygium which was similar to the findings of our study. Another study was done by Adriano et al., [14]. In their study there was a significant association of corneal staining with fluorescein in patients with pterygium.
A study done by Kiyat P et al., showed that in eyes with pterygium the Schirmer-1 test measurements were less than that of the normal eyes. But, the values were not significant statistically (p=0.308) [15].
In our study we did not find any association of MGD between eyes with pterygium and the eyes without pterygium. This was in contrary to a study done by Fen Ye et al [16]. They did a study to determine abnormalities in meibomian gland and tear function in patients with pterygium. In their study there was a statistically significant association between pterygium and degree of meibomian gland loss when compared to the study population without pterygium. But, relationship between pterygium and Schirmer’s test was not clearly defined in their study.
The association between pterygium and Dry Eye Disease is not yet clear and has a lot of research scope in this domain. Few studies have shown evidences that several inflammatory markers such as matrix metalloproteinases (MMPs), growth factors, and interleukins (ILs), are associated with pathogenesis of pterygium [17,18,19]. Research has demonstrated that IL-6 and IL-8 expression levels are significantly elevated in the epithelium of pterygium compared to those in the normal cornea, conjunctiva, and limbus.
The lower TBUT and Schirmers test values observed in eyes with pterygium compared to normal eyes in the same individual indicate a potential association between ocular surface changes and pterygium. This in turn can cause dry eye symptoms in such patients.
There are patients who have significant ocular discomfort but they do not have any significant signs clinically, and also those with severe dry eye signs clinically but with only mild symptoms [20,21,22]. Though surgery is the mainstay of treatment for pterygium causing visual disturbances, medical management includes lubricating the ocular surface with artificial tear drops .This provides short-term comfort.[23] Treatment might also be needed to address the inflammatory component of the pterygium and dry eye.
Limitations of the study: The sample size is limited and there is no follow up assessment of the ocular surface changes. This might make it difficult to detect subtle changes. Pterygium varies in size, location, and activity (inflamed vs. atrophic). These variations can affect the degree of ocular surface impact, which was not taken into account.
5. Conclusion
In our study there was a statistically significant change in TBUT values and Schirmers test values in eyes with pterygium indicating a possible association of dry eye with pterygium. More studies need to be done to establish the relationship between DED and pterygium. This might also change the medical management of pterygium towards anti-inflammatory agents along with lubrication with artificial tear drops.
Acknowledgement
None
Disclosures
None.
References
- Farhad Rezvan, Mehdi Khabazkhoob, Elham Hooshmand, et al. Prevalence and risk factors of pterygium: a systematic review and meta-analysis. Survey Ophthalmol Volume 63 (2018) : 719-735.
- Ang LP, Chua JL, Tan DT. Current concepts and techniques in pterygium treatment. Curr Opin Ophthalmol 18 (2007): 308-313.
- Ang M, Li X, Wong W, et al. Prevalence of and racial differences in pterygium: a multiethnic population study in Asians. Ophthalmol 119 (2012): 1509-1515.
- Shiroma H, Higa A, Sawaguchi S, et al. Prevalence and risk factors of pterygium in a southwestern island of Japan: the Kumejima Study. Am J Ophthalmol 148 (2009): 766-771.
- Lu P, Chen X, Kang Y, et al. Pterygium in Tibetans: a population-based study in China. Clin Exp Ophthalmol 35 (2007): 828-833.
- Coroneo MT. Pterygium as an early indicator of ultraviolet insolation: a hypothesis. Br J Ophthalmol 77 (1933): 734–739.
- Di Girolamo N, Chui J, Coroneo MT, et al. Pathogenesis of pterygia: role of cytokines, growth factors, and matrix metalloproteinases. Prog Retin Eye Res 23 (2004): 195-228.
- Hamed-Azzam S, Edison N, Briscoe D, et al. Identification of human papillomavirus in pterygium. Acta Ophthalmol 94 (2016): e195-197.
- Di Girolamo N, McCluskey P, Lloyd A, et al. Expression of MMPs and TIMPs in human pterygia and cultured pterygium epithelial cells. Invest Ophthalmol Vis Sci 41 (2000): 671-679.
- Li M et al (2007) Tear function and goblet cell density after pterygium excision. Eye (Lond) 21(2007): 224–228.
- Liu Y, Xu C, Wang S, et al. Accurate detection and grading of pterygium through smartphone by a fusion training model. British J Ophthalmol 108 (2024): 336-342.
- Daniel E, Maguire MG, Pistilli M, et al. Dry Eye Assessment and Management (DREAM) Study Research Group. Grading and baseline characteristics of meibomian glands in meibography images and their clinical associations in the Dry Eye Assessment and Management (DREAM) study. Ocul Surf 17 (2019): 491-501.
- Ishioka M, Shimmura S, Yagi Y, et al. Pterygium and dry eye. Ophthalmologica 5 (2001): 209-211.
- Adriano L, Persona ELS, Persona IGS, et al. Correlation between the presumed pterygium with dry eye and with systemic and ocular risk factors. Arq Bras Oftalmol 85 (2021): 136-143.
- Kiyat P, Karti O. Evaluation of dry eye in eyes with unilateral pterygim. Eur Eye Res 3 (2023): 12-15.
- Fen Y, Zhou F, Yuan X, et al. Evaluation of meibomian gland and tear film changes in patients with pterygium. Indian J Ophthalmol 65 (2017): 233-237.
- Livezeanu C, Craitoiu MM, Manescu R, et al. Angiogenesis in the pathogenesis of pterygium. Rev Roum Morphol Embryol 52 (2011): 837-844.
- Young CH, Chiu YT, Shih TS, et al. E-cadherin promoter hypermethylation may contribute to protein inactivation in pterygia. Mol Vis 16 (2010): 1047-1053.
- Kim KW, Park SH, Kim JC. Fibroblast biology in pterygia. Exp Eye Res 142 (2016): 32-39.
- Wanzeler ACV, Barbosa IAF, Duarte B, et al. Mechanisms and biomarker candidates in pterygium development. Arq Bras Oftalmol 82 (2019): 528–536.
- Management and therapy of dry eye disease: report of the Management and Therapy Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf 5 (2007): 163–178.
- Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol 92 (2014): 161–166.
- Sarkar P, Tripathy K. Pterygium. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2025).


 Impact Factor: * 1.2
Impact Factor: * 1.2 Acceptance Rate: 79.45%
Acceptance Rate: 79.45%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
