Subclinical Left Ventricular Disfunction in Obese Children: Are we Late?
B Riaño-Mendez1, M Ruiz-del Campo2, P Garcia-Navas2, A Ibiricu-Lecumberri1, MY
Ruiz-del Prado3
1Pediatric cardiologist, Department of Pediatrics, San Pedro hospital, Logroño, Spain.
2Pediatric endocrinologist, Department of Pediatrics, San Pedro hospital, Logroño, Spain.
3Associate professor, University of La Rioja, Logroño, Spain.
*Corresponding author: B Riaño-Mendez, pediatric cardiologist, Department of Pediatrics, San Pedro hospital, Logroño, Spain.
Received: 18 May 2023; Accepted: 25 May 2023; Published: 05 October 2023
Article Information
Citation: B Riaño-Mendez, M Ruiz-del Campo, P Garcia-Navas, A Ibiricu-Lecumberri, MY Ruiz-del Prado. Subclinical left ventricular disfunction in obese children: are we late?. Cardiology and Cardiovascular Medicine. 7 (2023): 336-342.
View / Download Pdf Share at FacebookAbstract
Aim: Longitudinal global strain (LGS) is reduced in obese patients with preserved ejection fraction of the left ventricle (LV). TAPSE/PAPS ratio, recently described, may be a step forward a more efficient RV function evaluation. The aim of the present study was to screen left and right subclinical dysfunction in obese pediatric patients without comorbidities.
Methods: This case-control study compared 104 children aged 5-18 years between October 2017 and February 2019, 52 obese children with body mass index (BMI) > mean +2SD, and 52 matched controls. They were screened for other cardiovascular risk factors like insulin resistance or hypercholesterolemia. A complete echocardiography including standard and functional parameters was performed.
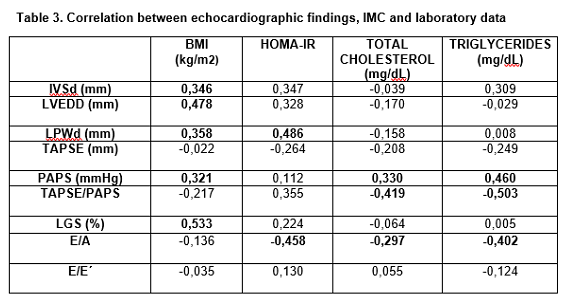
Results: Obese children presented worse longitudinal LV function (LGS -15,90% ± 3,84 SD) in comparison with non-obese children (-19,44% ± 5,75, p=0,001). LGS correlated positively with BMI. Standard echocardiography also revealed LV dilatation and hypertrophy. TAPSE/ PAPS ratio correlated negatively with total cholesterol (r -0,419, p=0,006) and triglycerides levels (r -0,503, p=0,002). HOMA-IR (r -0,458, p=0,006) correlated negatively with E/A ratio of left ventricle.
Conclusion: Remodeling of LV and sub clinic systolic dysfunction could be relatively common in asymptomatic patients with obesity and easily detected by functional echocardiography. It is necessary to perform a standardized cardiovascular evaluation in obese children for early identification of subclinical dysfunction especially in those with insulin resistance and dyslipidemia.
Keywords
<p>Obese children; BMI; Longitudinal global strain; TAPSE/ PAPS ratio; HOMA-IR; Triglycerides</p>
Article Details
1. Introduction
The prevalence of overweight among children in high income and middle/low income countries is continuing to increase [1]. Nearly 40% of pediatric population in our midst are either obese or overweight [2]. One of the major efforts in public health nowadays in the first world is obesity in children and adolescents. Obese children may be at risk for consequences, both short-term and long-term health consequences tracking of obesity to adulthood [3]. Intense correspondences between obesity and cardiovascular disease (CVD) have been shown in many studies. In fact, obesity has been considered an independent risk factor for CVD and CVD risks in obese children. Indeed, literature has described the relationship between BMI in adolescence and all-cause mortality [4]. Children exhibit early signs of cardiovascular dysfunction as a result of their excess adiposity as recent studies have shown, frequently independent of other obesity-related comorbidities such as insulin resistance, hypertension or dyslipidemia. Clinical testimony to date suggests that the cardiovascular injure seen in middle-aged adults is also happening in obese children [5], particularly in those with a central fat distribution. At present, the secondary and tertiary prevention measures are the most important points to fight against cardiovascular disease [6]. However, efforts to analyze modifiable risk factors present in children and adults over a long time have not been a priority to date 2. The major obesity-induced changes described are enlargement of left ventricular structures, left ventricular (LV) hypertrophy, systolic and diastolic dysfunction, heart failure. An appropriate detection and treatment of these cardiovascular damages in early phases is important in order to slow down and reverse the process in high-risk pediatric populations [7]. New echocardiographic procedures are developed to accomplish accurate evaluation of myocardial deformation ( both segmental and global). The newly released development is the two-dimensional speckle-tracking echocardiography (2D STE), a routine for assessing myocardial strain and measure deformation function [8]. It provides information which is not available with any of the echocardiographic parameters used at the present time. STE provides an impartial quantification of myocardial deformation and left ventricular systolic and diastolic dynamics. One of this value is that this technique is angle-independent. Results regarding the viability, exactitude and clinical application of speckle-tracking echocardiography are quickly accumulating [9]. In literature, there are still few publications in the application of this method in pediatric population.
2. Materials and Methods
2.1 Study design
The aim of the study was to analyze LV function using 2D speckle tracking in obese pediatric patients referred from the Endocrinology consult with BMI >mean+2 DS, and to contrast their data with non-obese patients with structurally normal hearts and same age and sex. We used preceding researches where LV Doppler-derived strain was contrasted between obese and non-obese children for sample size estimation.
A number of 45 patients in a cluster was estimated to provide a 90% power to identify the clinical outcome of interest (20% strain value difference between groups), with a significance level (alpha) of 0.05 (two-tailed) [10]. Patients were not involved in the recruitment to and conduct of the study. This case-control matched study was made between October 2017 and February 2019.
2.2 Body mass index (BMI)
Body mass index was calculated by the formula weight (kg)/height (m2).
The cutoff points used for childhood overweight or obesity were the ones proposed by the World Health Organization (WHO) [11] (overweight, specific body mass index (BMI) values agreement to age and sex, >mean +1 standard deviation (SD) in the reference population characterized by the WHO; obesity: sex-and age-specific BMI values, > mean +2 SD).
2.3 Blood pressure (BP)
Blood pressure was measured with an appropriate cuff in supine position in the Endocrinology consult. Patients with hypertension (systolic and/or diastolic BP over the 90th percentile for sex and height) were excluded off the study to avoid confounding factors with other comorbidities that may affect left ventricular function, already well documented in adults.
2.4 Laboratory findings
In all obese children a complete analytic was obtained: fasting blood glucose, glycosylated hemoglobin, homeostatic model assessment of insulin resistance (HOMA-IR), lipidic profile and calcium phosphate metabolism. Cutoff points for impaired fasting glucose have previously followed recommendations by the American Diabetes Association-ADA (100–125 mg/dL). Criteria for defining dyslipidemia are triglycerides >150 mg/dL y c-HDL <40 mg/dL in males and 50 mg/dL in female. Insulin resistance is assess by HOMA-IR: FPG (nmol/l) × FPI (microU/l)/22.5 (FPG: fasting plasma glucose, FPI: fasting plasma insulin) [12].
2.5 Cardiovascular evaluation
Including personal interview (familiar and personal cardiological backgrounds, functional class-modified Ross scale [13], recommended daily physical activity-more than 60 minutes of vigorous physical exercise [14], sleep quality-Chervin pediatric sleep questionnaire reduced version [15]), and physical examination (cardiopulmonary auscultation, pulse palpation). A functional echocardiography was performed to all patients both standard (left ventricular end diastolic diameter-LVEDD, interventricular septum thickness-IVSd, left ventricular posterior wall thickness-LVPWd, ejection fraction-EF) and functional parameters (tricuspid annulus plane systolic excursion-TAPSE; indirect estimation of pulmonary artery systolic pressure (PAPS) using the peak tricuspid regurgitation velocity for assessing the right ventricle -RV-function; longitudinal global and regional strain, pulsed-wave Doppler and tissue-Doppler for assessing the left one). This study was made by only one observer using a Philips EpiQ team provided with Premium Ultrasound System technology. TAPSE is a standard procedure to take the measurement of the distance of systolic excursion of the RV annular segment along its longitudinal plane, from a standard apical 4-chamber window, and represents longitudinal function of the RV [16]. Peak tricuspid regurgitation velocity was evaluated to calculate the RV-right atrial gradient and estimate PAPS [17]. TAPSE/PASP ratio is a substantial prognostic parameter in patients with pulmonary hypertension and is related with hemodynamic and functional class [18]. This ratio was subsequently calculated. Left ventricular determinations were executed in concordance to the recommendations of the American Society of Echocardiography [19]. Ejection fraction (EF) was assessed using the Teichholz routine. Diastolic function was analyzed by the mitral inflow, pulsed-wave Doppler (PWD) and tissue-Doppler imaging (TDI). TDI was obtained at the lateral margin of the mitral annulus and the velocity of the e´ wave was measured. Principal values of lateral e´ wave was captured and the E/e´ ratio was calculated from this mean value [20]. The images obtained from standard apical 4-chamber, 3-chamber and 2-chamber views were then processed (echoPAC) to calculate the end-systolic longitudinal global strain (LGS) according with the consensus document of the European Association of Cardiovascular Imaging [21]. The echocardiographer took two or three measurements and chose the best possible quality image for more accuracy.
Statistical analysis Descriptive analyzes of all the variables were carried out separately, using tables of absolute relative frequencies in the case of quantitative variables, and by mean ± SD, in the case of continuous quantitative variables. The Kolmogorov-Smirnov test was used to assess the normal distribution of the data. The bivariate analysis was performed using the chi-square test for the comparison of proportions and those of Student Fisher-t to compare two means. Pearson´s linear correlation coefficient analysis was used to check the positive or negative correlation between BMI, laboratory and echocardiography parameters. p<0,05 was considered statistically significant. All the statistical tests were two tailed, considering 95% confidence level. The calculations was made with the help of the statistical package SPSS 22.0.
3. Results
The study included 52 obese children (25 boys and 27 girls, mean age 10,98 ± 1,63 years) and 52 controls (32 boys and 20 girls, mean age 11,04 ± 2,91 years) referred to cardiologist by other reasons (murmur, thoracic pain or syncope) with structurally normal hearts. Demographic and anthropometric characteristics are reflected in Table 1.
Mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) in obese children was 117,64 ± 12,90 mmHg and 67,52 ± 9,85 mmHg, respectively. One patient with SBP 165 mmHg and DBP 85 mmHg confirmed by Ambulatory Measurement of Blood Pressure was excluded from the study. Fourteen obese children presented limit total cholesterol 171-199 mg/dL and only one hypercholesterolemia of 223 mg/dL. Four patients had levels of HDL fewer than 35 mg/dL. Hypertriglyceridemia >150 mg/dL was seen in five obese subjects. 14 patients (27%) presented vitamin D deficiency. The mean insulin value was 25,68 ± 12,05 μu/mL and HOMA-IR was 5,34 ± 2,39 in the obese subjects. Insulin resistance (HOMA-IR > 2,5) was identified in 30 of them (57%). All the patients were staged in functional class I (no limitations or symptoms) in modified Ross Heart Failure Classification for children. None of the obese children reached the minimum required level of physical activity, they all only practiced some kind of sport in the subject of Physical Education at school. In two patients (a 13 year old boy and a 15 year old girl) screening for obstructive sleep apnea syndrome (OSAS) was indicated due to score greater than 7 (positive answers) in sleep questionnaire. The girl presented an apnea hypopnea index 3,6 (mild OSAS). The other patient refused the realization of the polysomnography. The echocardiographic measurements between the both groups were compared in Table 2. The IVSd (p= 0,026), LPWd (p=0,018) and LVEDD (p= 0,005) were significantly greater in obese children, revealing hypertrophy and left ventricular enlargement in standard echocardiography. PAPS was significantly higher in the case group (p= 0,002). Longitudinal end-systolic global strain (LGS) was significant affected in obese children in comparison with controls, throwing a systolic subclinical dysfunction (p=0,001). Diastolic function assessed by PWD and TDI was not different between the two groups.
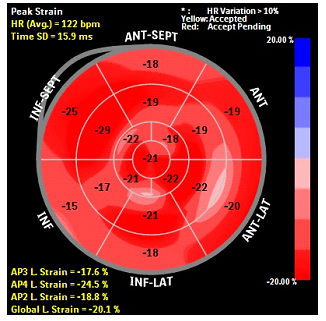
In Figure 1 is represented the global and regional strain in a control patient (“bull´s eye like”). LGS is derived from speckle tracking and analyzed by post-processing of apical images of the left ventricle (LV). Longitudinal shortening is expressed like a percentage.
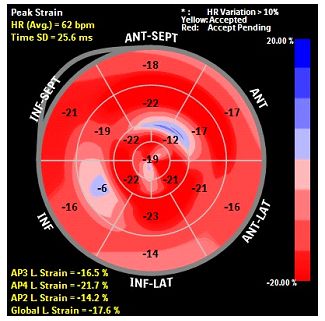
The apical image of LV in an obese patient is showed in Figure 2. Note that inferior, anterior and anteroseptal wall present the worst changes in length in proportion to baseline. Correlation between BMI and some laboratory data with echocardiographic parameters are represented in Table 3. Those marked in bold are significant at p<0,05. There was positive correlation between BMI and all standard parameters (IVSd, r 0,346, p=0,014; LVEDD, r 0,478, p=0,000; PWd, r 0,358, p=0,013), and between HOMA-IR with PWd (r 0,486, p=0,012). Pulmonary pressure correlated positively with BMI (r 0,321, p=0,017), total cholesterol (r 0,330 p=0,033) and triglycerides levels (r 0,460, p=0,005). TAPSE/PAPS ratio correlated negatively with total cholesterol (r -0,419, p=0,006) and triglycerides levels (r -0,503, p=0,002). We found significative positive relation between BMI and LGS (r 0,533, p<0,001). HOMA-IR (r -0,458, p=0,006), cholesterol (r -0,297, p=0,048) and triglycerides levels (r -0,402, p=0,011) correlated negatively with diastolic function of left ventricle estimated by E/A ratio with PWD. This correlation was not extensive to E/e´ assesed by DTI.
4. Discussion
Obesity in children has become an authentic pandemic in high income countries. There are different criteria for defining overweight and obesity, to facilize the comparison between different studies and countries, taking into account the ethnic diversity and avoiding underestimation that involves comparing with populations in which obesity already existed. The criteria most commonly approved by the international scientific society are those recommended by International Obesity Task Force (IOTF) [22] (cutoff points for childhood overweight or obesity particular to each BMI value and sex, using the reference population specified by the IOTF) and those proposed by the World Health Organization (WHO) [11]. In our study we have chosen the WHO criteria.
Enkid study (1998-2000) [23] has been the reference in obesity in children in Spain for many years, but it´s outdated.
The two most recent national studies used direct height and weight measurement: ALADINO [14] (Diet, physical Activity, Childhood Development and Obesity) study with children aged 6 to 9.9 years old; and a cross-sectional, observational study composed of children and adolescents of both sexes between 8 to 17 years old residing in family homes in mainland Spain [2]. The prevalence of overweight and obesity in this study is 26.0% and 12.6%, respectively. In our region the prevalence of obesity is quite higher (18,5%) [24]. Among obese children, based on our results, standard echocardiography did not show anomalies in the global contractility (EF>55%) [19]. However, LVEDD, interventricular septum (IVSd) and posterior wall of left ventricle (LPWd) measured in diastole were significantly higher in obese group in comparison with controls (p =0,005, p=0,026 and p=0,018, respectively). A subgroup of obese children could present LV remodeling characterized by increased volume and wall thickness. These findings are superposable to Binnetoglu et al´s [25]. In healthy children, the mean LGS value is -20,5% [26]. In our study, obese children compared with controls had lower 2D STE-derived LV LGS (-15,90 ± 3,84% vs 19,44 ± 5,75%, p=0,001). LGS in our study was not affected by sex or age. Similar observations of decreased longitudinal and circumferential strain in children with obesity were concluded by Kulkarni et al [27]. These findings are extensible to radial strain and early diastolic strain rate values [28]. Segmental analysis of the LV could provide in the future subtle markers for the emergence of future obesity-related cardiac disease [29]. Current guidelines recommend pulmonary hypertension screening in patients with severe obstructive sleep apnea. Prevalence of pulmonary hypertension in pediatric patients with obstructive sleep apnea is low and none of the patients with pulmonary hypertension had severe obstructive sleep apnea in a recent study over 163 patients [30]. According to this in our study we found significative higher pulmonary pressure in obese children, but no one had pulmonary hypertension (mPAP >25 mmHg) [31]. Normal TAPSE values including z-scores based on patient age have been established in pediatric patients [16]. The TAPSE/PASP ratio has recently been reported as an independent prognostic parameter in heart failure. When stratified by terciles, patients in the low tercile showed significantly compromised hemodynamic, functional and echocardiographic status [18]. This index may be a step forward a more efficient RV function evaluation. In our sample TAPSE/PAPS was significantly negative correlated with triglycerides (r -0,503, p=0,002) and total cholesterol levels (r -0,419, p=0,006). Diastolic function of obese participants was assessed by pulsed-wave Doppler (PWD) and TDI. We didn´t find a statistically significant difference that could indicate impaired LV filling like Gandhi et al [32]. However we found relation between HOMA-IR and triglycerides levels, correlated negatively with diastolic function of left ventricle estimated by E/A ratio with PWD. In previous studies LV diastolic disfunction in hypercholesterolemic children compared with controls is also described [33]. There wasn´t positive correlation between HOMA-IR, cholesterol, triglycerides and remodeling of left ventricle [34,35]. One reason could be that we didn´t estimate the LV mass index. And now the question is, can we take an active attitude with these patients that have already remodeling and some index of RV and LV function altered? Gores et al [36] describe an improvement in RV function assessed by TAPSE in a group of overweight patients participating in vigorous 3-month football training. We think next interventions could follow this line and select between the obese patients those that could beneficiate from personalized training and enter in a program of cardiac rehabilitation.
Limitations
The statistical power of the analysis is limited by the small sample size. We didn´t find relation between HOMA-IR, total cholesterol and triglycerides levels with LGS. Perhaps the view selection, defining end-systole or tracing the myocardium was not the most adequate, in obese patients there is an added difficulty due to bad transthoracic window. There were only very few patients with dyslipidemia and correlation coefficient was borderline. The correlations between echocardiographic and laboratory parameters need to be confirmed in upcoming and larger studies to know future health care implications.
5. Conclusion
Remodeling of LV and sub clinic systolic dysfunction could be relatively common in asymptomatic patients with obesity and easily detected by functional echocardiography. It is necessary to perform an standardized cardiovascular evaluation in obese children for early identification of LV changes and subclinical dysfunction especially in those with insulin resistance and dyslipidemia.
Conflict of interest disclosure
Nothing to disclose.
Funding:
No external funding was received.
Ethics committee:
Ethical Committee of Clinical Research of La Rioja.
Approval number:
CEICLAR P.I 219.
Patient and Public Involvement:
Patients were not involved in the recruitment to and conduct of the study.
Author contributions:
Authors 1 and 2 conceived the study; authors 2 and 3 enrolled the patients and supervised the data collection; authors 1 and 4 are the responsible in performing the echocardiographs; authors 1 and 2 drafted the manuscript; all authors contributed substantially to its revision.
References:
- Ogden CL, Flegal KM, Carroll MD, et al. Prevalence and trends in overweight among US children and adolescents. JAMA 288 (2002): 1728-1732.
- Sánchez-Cruz J, Jiménez-Moleón J, Fernández-Quesada F, et al. Prevalence of child and youth obesity in spain. Rev Esp Cardiol 66 (2012): 371-376.
- Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents. JAMA 307 (2012): 483-490.
- Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss. Circulation 113 (2006): 898-918.
- Cote A, Harris K, Panagiotopoulos C, et al. Childhood obesity and cardiovascular dysfunction. J Am Col Cardiol 62 (2013): 1309-1319.
- Hobbs FDR. Cardiovascular disease: different strategies for primary and secondary prevention? Heart 90 (2004): 1217-1223.
- Pascual M, Pascual DA, Soria F, et al. Effects of isolated obesity on systolic and diastolic left ventricular function. Heart 89 (2003): 1152-1156
- Leitman M, Lysyansky P, Sidenko S, et al. Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr 17 (2004): 1021-1029.
- Mondillo S, Galderisi M, Mele D, et al. Speckle-tracking echocardiography: a new technique for assessing myocardial function. J Ultrasound Med 30 (2011): 71-83.
- Barbosa JA, Mota CC, Simões-Silva AC, et al. Assessing pre-clinical ventricular dysfunction in obese children and adolescents: the value of speckle tracking imaging. Eur Heart J Cardiovasc Imaging 14 (2013): 882-889.
- De Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85 (2007): 660-667.
- Ho M, Garnett SP, Baur LA. Childhood obesity and insulin resistance: how should it be managed? Curr Treat Options Cardiovasc Med 16 (2014): 351.
- Ross RD. The Ross clasification for heart failure in children after 25 years: a review and an age-stratified revision. Pediatr Cardiol 33 (2012): 1295-1300.
- Ministry of Health, Social Services and Equality, Government of Spain. Study of the prevalence of childhood obesity. ALADINO Study (ALimentation, Physical Activity, Child Development and Obesity). NAOS Strategy (2013): 163687.
- Tomás Vila M, Miralles Torres A, Beseler Soto B. Spanish version of the Pediatric Sleep Questionnaire. A useful instrument in investigation of sleep disturbances in childhood. Reliability analysis. AN Pediatr (Barc) 66 (2007): 121-128.
- Koestenberger M, Ravekes W, Everett AD, et al. Right ventricular function in infants, children and adolescents: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 640 healthy patients and calculation of z score values. J Am Soc Echocardiogr 22 (2009): 715-719.
- Galie N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). European Heart Journal 37 (2016): 67-119.
- Tello K, Axmann J, Ghofrani HA, et al. Relevance of the TAPSE/PASP ratio in pulmonary arterial hypertension. Int Jour Cardiol 266 (2018): 229-235.
- Lang RM, Bierig M, Devereux RB, et al. American society of echocardiography’s guidelines and standards committee;European association of echocardiography recommendations for chamber quantification: a report from the American society of echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European association of echocardiography, a branch of the European society of cardiology. J Am Soc Echocardiogr 18 (2005): 1440-1463.
- Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22 (2009): 107-133.
- Voigt JU, Pedrizzetti G, Lysyansky P, et al. Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16 (2015): 1-11.
- Cole TJ, Bellizi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide international survey. BMJ 320 (2000): 1240-1243.
- Serra-Majem L, Aranceta Bartrina J, Pérez-Rodrigo C, et al. Prevalence and determinants of obesity in Spanish children and young people. Br J Nutr 96 (2006): 67-72.
- Fernández-Vallejo B, Esteban-Díez I, Bernad-Usoz JV, et al. Obesity prevalence of puberal children in La Rioja. Dietary habits and physical activity. Bol Pediatr Arag Rioj Sor 47 (2017): 104-109.
- Binnetoglu FK, Yildirim S, Topaloglu N, et al. Early detection of myocardial deformation by 2D speckle tracking echocardiography in normotensive obese children and adolescents. Anatol J Cardiol 15 (2015): 151-157.
- Levy PT, Machefsky A, Sanchez AA, et al. Reference Ranges of Left Ventricular Strain Measures by Two-Dimensional Speckle-Tracking Echocardiography in Children: A Systematic Review and Meta-Analysis. J Am Soc Echocardiogr 29 (2015): 209-225.
- Kulkarni A, Gulesserian T, Lorenzo JMMD, et al. Left ventricular remodelling and vascular adaptive changes in adolescents with obesity. Pediatr Obes 13 (2018): 541-549.
- Koopman LP, McCrindle BW, Slorach C, et al. Interaction between myocardial and vascular changes in obese children: a pilot study. J Am Soc Echocardiogr 25 (2012): 401-410.
- Kibar AE, Pac FA, Ece I, et al. Effect of obesity on left ventricular longitudinal myocardial strain by speckle tracking echocardiography in children and adolescents. Balkan Med J 32 (2015): 56-63.
- Burns AT, Hansen SL, Turner ZS, et al. Prevalence of pulmonary hypertension in pediatric patients with obstructive sleep apnea and a cardiology evaluation: a retrospective analysis. J Clin Sleep Med 15 (2019): 1081-1087
- Abman SH, Hansmann G, Archer SL, et al. Pediatric pulmonary hypertension: Guidelines from the American Heart Association and American Thoracic Society. Circulation 132 (2015): 2037-2099.
- Ghandi Y, Sharifi M, Habibi D, et al. Evaluation of left ventricular function in obese children without hypertension by a tissue Doppler imaging study. Ann Pediatr Cardiol 11 (2018): 28-33.
- Vitarelli A, Martino F, Capotosto L, et al. Early myocardial deformation changes in hypercholesterolemic and obese children and adolescents: a 2D and 3D speckle tracking echocardiography study. Medicine (Baltimore) 93 (2014): 71.
- Sanchez-Mejia AA, Levy PT, Sekarski TJ, et al. Markers of Cardiovascular Risk, Insulin Resistance, and Ventricular Dysfunction and Remodeling in Obese Adolescents. J Pediatr 166 (2015): 660-665.
- Kibar AE, Pac FA, Balli S, et al. Early subclinical left-ventricular dysfunction in obese nonhypertensive children: a tissue Doppler imaging study. Pediatr Cardiol 34 (2013): 1482-1490.
- Gores G, Ravekes W, Koestenberger M. Improvement of systolic right ventricular function in overweight children participating in a three month football training determined by tricuspid annular plane systolic excursion (TAPSE).Journal of Sports Sciences 32 (2014): 1350.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 