A Framework on Developing an Integrative Medicine Clinical Practice Guideline (CPG) for Systemic Lupus erythematosus (SLE) with Comorbidities Management in Hong Kong
Yuanyuan Chen1, Philip Hei Li2, Cheng Zhang1, Ning Wang1, Yibin Feng*, 1, Che-Shing Lau*, 2
1School of Chinese Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, 3 Sassoon Road, Pokfulam, Hong Kong SAR, PR of China.
2Rheumatology and Clinical Immunology, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, PR of China
*Corresponding author: Yibin Feng. School of Chinese Medicine, 3 Sassoon Road, Pokfulam, Hong Kong S.A.R., PR of China. Che-Shing Lau, Rheumatology and Clinical Immunology, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, 21 Sassoon Road, Pokfulam, Hong Kong SAR, PR of China
Received: 31 July 2023; Accepted: 08 August 2023; Published: 24 October 2023
Article Information
Citation: Yuanyuan Chen, Philip Hei Li, Cheng Zhang, Ning Wang, Yibin Feng, Che-Shing Lau. A Framework on Developing an Integrative Medicine Clinical Practice Guideline (CPG) for Systemic Lupus erythematosus (SLE) with Comorbidities Management in Hong Kong. Journal of Pharmacy and Pharmacology Research. 7 (2023): 213-219.
View / Download Pdf Share at FacebookAbstract
Background: Systemic Lupus erythematosus (SLE) is a heterogeneous autoimmune disease that affects multiple organs. In most patients with SLE, the comorbidity manifests within three years of initial diagnosis. In Hong Kong, SLE with comorbidities significantly affect patients' quality of life and contributes to mortality. Due to the complexity of comorbidities, clinicians require comprehensive suggestions across disciplines. An integrative medicine clinical practice guideline (CPG) must be developed for the management of SLE with comorbidities. Therefore, this framework is designed to address multimorbidity in SLE patients.
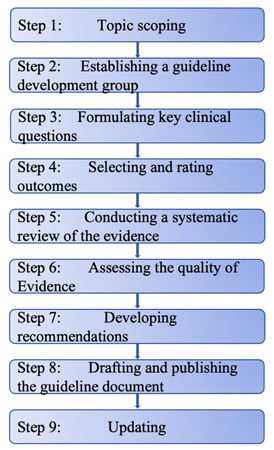
Methods & Results: The framework is based on the steps of developing CPGs outlined in the WHO handbook for guideline development, Appraisal of Guidelines for Research and Evaluation II Instrument, Guideline International Network and Reporting Items for Practice Guidelines in Healthcare. The design of CPG for SLE includes nine steps as the followings: topic scoping, establishing a guideline development group, formulating key clinical questions, selecting and rating outcomes, conducting a systematic review of the evidence, assessing the quality of evidence, developing recommendations, drafting and publishing the guideline document, and updating are conducted.
Conclusion: This CPG represents a significant advancement in establishing guidelines for multimorbidity in SLE. It will provide recommendations for the management of comorbidities in SLE. To update and adjust recommendations, further studies with large-scale clinical trials are necessary for the future.
Keywords
<p>Clinical practice guideline; Systemic Lupus erythematosus; Comorbidity; Multimorbidity; Integrative medicine; Traditional Chinese medicine</p>
Article Details
Abbreviations
: SLE, systemic lupus erythematosus; HA, hospital authority; CPG, clinical practice guideline; GDM, glucocorticoid-induced diabetes mellitus; DM, diabetes mellitus; TCM, traditional Chinese medicine; CAT, complementary and alternative therapy; CM, conventional medicine; NSAID, nonsteroidal anti-inflammatory drug; CVD, cardiovascular disease.1. Introduction
Systemic lupus erythematosus (SLE) is a heterogeneous autoimmune disease that involves multiple-organ damage including heart, lungs, liver, kidneys, joints, skin, blood vessels, and nervous system [1]. Due to its intricate pathogenetic mechanisms, SLE can affect anyone at any age. Most commonly, it affects women in their reproductive years [2]. The prevalence of SLE in mainland China is about 30–70/100,000, and the ratio of males to females is 1:10–12 [3]. It is estimated that across all Hospital Authority (HA) hospitals in Hong Kong, there were 5243 patients with SLE in 2008, 91% of whom were women [4]. The prevalence of SLE in Hong Kong was calculated to be 0.1% [4] Therapy- or disease-related comorbidities may occur in SLE patients. A study showed a high risk of comorbidity at the time of diagnosis and incident comorbidity after diagnosis in patients with SLE [5]. It has been estimated that half of SLE patients develop comorbidity within 3 years of initial diagnosis [5]. A high burden of comorbidities in SLE such as cardiovascular disease, diabetes mellitus, dyslipidemia, osteoporosis, avascular bone necrosis, infection, musculoskeletal disease, ocular disease, and malignancy may significantly affect the quality of life and contribute to mortality [6].
It is common for SLE patients to have multiple health conditions, but explicit guidance regarding how to make clinical decisions with those with multimorbidity is lacking for clinicians. There is a major challenge in developing a clinical practice guideline (CPG) for SLE patients with comorbidities due to the evidence base typically less focusing on a complex condition [6, 7]. The clinical management of one condition may affect the clinical management of the other condition(s) through interactions between the condition(s) and the treatment(s). For example, the likelihood of developing glucocorticoid-induced diabetes mellitus (GDM) after receiving high-dose glucocorticoids was higher in SLE patients with a family history of diabetes mellitus (DM), hypertension, or higher body mass index [8]. Therefore, using evidence from individuals with a single condition to make recommendations for more complex individuals may increase clinical uncertainty. There are two recent CPGs that address the issue of comorbidity and multimorbidity in SLE, but specific recommendations reported in these two CPGs for SLE patients remain insufficient [3, 9]. In-depth recommendations about comorbidities associated with a wide range of organ damage are needed.
Due to the complexity of comorbidities, clinicians need comprehensive suggestions across disciplines. Traditional Chinese medicine (TCM) plays a central role in Hong Kong's medical practice as one of the complementary and alternative therapies (CATs) [10]. Patients in Hong Kong continuously seek treatment from practitioners in two systems due to the popularity and acceptability of the integrative therapy of TCM and conventional medicine (CM) [11]. Clinical practices have proven the effectiveness of TCM which is based on pattern differentiation in treating SLE comorbidities. However, because of the particular restrictions in Hong Kong and the complexity of comorbidities, currently, no integrative medicine guideline for SLE comorbidities exist. An integrative CPG is crucial for supporting medical decisions regarding SLE comorbidities management. This publication presents a framework for developing an integrative medicine CPG on the basis of existing approaches. The two primary components of integrative medicine are TCM and CM In this framework.
2. Methods
The framework was based on the steps of developing CPGs outlined in the WHO handbook for guideline development, Appraisal of Guidelines for Research and Evaluation II Instrument (12), Guideline International Network and Reporting Items for Practice Guidelines in Healthcare (13). Nine steps including topic scoping, establishing a guideline development group, formulating key clinical questions, selecting and rating outcomes, conducting a systematic review of the evidence, assessing the quality of evidence, developing recommendations, drafting and publishing the guideline document, and updating were conducted (Figure 1). A systematic review to identify the integrative medicine of SLE with comorbidities by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria will be presented in an accompanying paper and is only briefly discussed here.
3. Results
3.1 Topic scoping - what are the comorbidities that the guideline attempts to address?
To properly refine the scope of the CPG around multimorbidity in SLE, the CPG developers will adopt a clear strategy. As part of the CPG, both the primary conditions of SLE, as well as related coexisting conditions or specific combinations of those conditions will be addressed. It is expected that the CPG will attempt to address comorbidities including thyroid disease, depression and anxiety, obesity, dyslipidaemia, hypertension, osteoporosis, cardiovascular diseases, allergic disorders, gastrointestinal diseases, infections, neurologic diseases, cerebrovascular diseases, kidney diseases, respiratory diseases, diabetes mellitus, malignancy, skin diseases, and hematologic disorders. According to a recent study, 51.0% of 399 SLE patients with multiple comorbidities had at least three physical disorders and 33.1% had at least two mental disorders(6). This is a large percentage showing multimorbidity across both categories. The CPG will categorize comorbid disorders by organs and domains. For example, SLE with coexisting conditions such as hypertension, dyslipidemia, and obesity can be classified as a metabolic disorder. Clinical evidence and epidemiological data will be examined during the scoping phase to determine the important coexisting conditions. The scoping phase will begin with preliminary literature searches.
3.2 Establishing guideline development group - who will be included in the guideline panel to provide expertise?
The synthesis and evaluation of evidence will become more complex if the scope is expanded beyond a single condition. Therefore, to address SLE with multimorbidity rather than one single condition, the CPG workgroup will need to incorporate a broader range of expertise(7). CPG workgroup for SLE with comorbidities will consist of clinicians, researchers, guideline methodologists, and experts in TCM, immunology, rheumatology, nephrology, cardiology, metabolic disease, osteology, dermatology, radiology, and evidence-based medicine. Four main groups including a steering group led by the responsible technical officer, a guideline development group made up of external experts, an external review group, and a systematic review team will be established. The steering group is primarily responsible for identifying the topic and key questions to be included in the guideline, drafting recommendations and the final guideline, as well as providing administrative support. The guideline development group aims to finalize the scope and key questions, formulate evidence-based recommendations, conduct the Grading of Recommendations Assessment, and approve the final guideline document. The external review group assists in identifying any errors or missing data and provides feedback on clarity, setting-specific issues, and implementation implications. While systematic reviews are fundamental parts of CPG development, it is the responsibility of the systematic review group to conduct systematic searches for relevant evidence, assess the quality of eligible studies, and summarize the findings. A conflict of interest in the workgroup could seriously undermine the objectiveness and independence of guidelines(14). Any conflict of interest will need to be declared and managed appropriately by the workgroup.
3.3 Formulating key clinical questions – what key clinical questions should be answered to formulate recommendations?
The formation of key clinical questions governs a systematic search of the evidence. “PICO” elements including population, intervention, comparator and outcome will be considered when forming a clinical question. It seeks to answer who will be affected (population), what action is being considered (intervention), what other options are available (comparator), and what the recommendation is trying to accomplish (outcome). In particular, the outcome is an important consideration when forming a recommendation for solving a complicated issue. The presence of comorbidities in SLE usually increases the number of potentially relevant outcomes. For example, one of the important outcomes for the management of SLE co-existing with musculoskeletal symptoms may include the progression of hypertension. It is because nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and indomethacin, which are commonly used by SLE patients co-existing with musculoskeletal symptoms, serositis, and headaches, cause significant rises in blood pressure(15, 16). The CPG will focus on integrative treatments of TCM and CM, thus key questions will relate to the effectiveness and safety of these treatments. After forming key clinical questions, they will be answered to formulate the recommendation. The following questions are examples aimed to be answered:
(1) In SLE patients, what integrative medicine of TCM and CM, compared with routine treatments shows effectiveness for managing different comorbidities?
(2) In which comorbidities of SLE do CM and TCM show the most benefit in the process of management?
(3) In SLE patients, which comorbidities of SLE should be treated by TCM/CM alone to achieve effectiveness?
Clinical practitioners' perspectives about treatment for SLE with comorbidities will be gathered through a questionnaire. The goal is to identify the most important clinical questions by conducting two rounds of the Delphi survey. The survey plans to involve 15 immunologists and 15 TCM practitioners with a minimum of five years' clinical experience managing SLE. Following the first round of the survey, all participants will rate the items that failed to reach a consensus. The key questions will be ranked based on their importance.
3.4 Selecting and rating outcomes – how to make judgements regarding the values and preferences of patients to determine the importance of outcomes?
A desirable outcome is the goal of the recommendation. To produce a useful recommendation, it is essential to select the most important outcome. Each outcome will be scored from 1 to 9. There are three levels of importance for a decision: critical if the outcome is 7–9, significant if it is 4–6, and not significant if it is 1–3. Based on the average score, the relative importance of outcomes will be identified and ranked in the CPG. When multimorbidity exists, certain outcomes may lose their relative significance because competing risks are present. For example, Gergianaki found that psychiatric disorders often coexisted with the gastrointestinal disorder in SLE patients(6). In these cases, SLE patients who have psychiatric disorders such as bipolar disorder, suicidal ideation, or schizophrenia may consider improvements in outcomes from gastrointestinal disorders relatively unimportant. Similarly, in the case of SLE patients with multimorbidity, the outcome of a comorbidity which is in a serious medical emergency, such as a heart attack or stroke, will be considered of relatively high importance. Moreover, for comorbidity in SLE that is categorised as severe and incurable, palliative care for symptomatic relief may become relatively important to reduce the treatment burden(7). Therefore, considering that patients with different manifestations place different values on a given outcome, an investigation into the preferences and values of SLE patients with different comorbidities is needed. The CPG workgroup will conduct a literature review and produce recommendations based on judgements regarding values and preferences.
3.5 Conducting a systematic review of the evidence – how to generate a comprehensive search?
Based on the clinical questions, the systematic review team will conduct a comprehensive search of nine electronic databases, including PubMed, ISI Web of Science, EMBASE, CINAHL Plus, AMED, Cochrane Library, China National Knowledge Infrastructure (CNKI) and WanFang Data to source eligible studies of SLE comorbidities, by the end of October 2022. Systematic reviews, meta-analyses, network meta-analyses, and original studies such as randomized controlled trials, cohort studies, case-control studies, case series studies and epidemiological surveys, etc. will be retrieved through the above-mentioned databases. Furthermore, SLE-related guidelines will be reviewed as references from official websites, such as the Scottish Intercollegiate Guidelines Network (SIGN), the National Institute for Health and Clinical Excellence (NICE), the Asia-Pacific Alliance Against Rheumatism (APLAR) and the American College of Rheumatology (ACR).
3.6 Assessing Quality of Evidence – what approaches should be used to estimate the quality of evidence across all important outcomes?
For grading recommendations, GRADE (Grading of Recommendations, Assessment, Development and Evaluations) will be used(17, 18). Each outcome will be rated based on the quality of evidence, which is categorized into four levels: very low, low, moderate, and high. Several factors including study design and execution, degree of directness, precision, consistency, and publication bias can affect the quality of the evidence for outcomes. The degree of directness refers to how well the evidence from studies corresponds to the population, the intervention, the comparator, and the outcome. Evidence should be rated lower if it applies to a population different from the guideline's target population. The directness of evidence may be compromised by the burden of multimorbidity, since patients with the same comorbidities may not be included in sufficient numbers. Additionally, insufficient participants may also result in imprecision in results. Evidence-based RCTs are rated as high quality while evidence from nonrandomized trials or observational studies is rated as low quality. Complex combinations of conditions in SLE may not have been investigated using RCTs, which results in a lower quality body of evidence for outcomes from the outset. As a result of the complex nature of multimorbidity, comorbidities associated with SLE may be primarily evidenced by observational studies. The quality of evidence from observational studies may be improved by examining three factors, including dose-response gradients, plausible biases, and magnitudes of effects. Since the presence of multimorbidity complicates decision-making, it is essential to estimate the overall quality of evidence across all important outcomes(7).
3.7 Developing recommendations - what should be taken into consideration to develop comprehensive recommendations?
Based on the summary of domestic and oversea evidence provided by the Evidence Evaluation Group, The CPG workgroup will generate recommendations that consider the advantages and disadvantages of interventions in the Hong Kong region. Rather than assessing a single condition, the CPG workgroup will consider the complexity of multimorbidity in SLE patients. This CPG will focus on the effectiveness of the combined therapy of TCM and CM. TCM theory defines syndrome differentiation as the basis of diagnosis and the guide to treatment. TCM recommendations will be presented from the TCM's perspective of diagnosis and treatment. It is expected that recommendations will be classified based on the coexisting conditions and their severity by the CPG workgroup. The CPG workgroup will also highlight key recommendations and evaluate how coexisting conditions affect their priority. Conditions will be identified when a recommendation should not be or no longer be followed. Recommendations will be drafted by the steering group and finalized by the guideline development group. Two-round Delphi surveys will be conducted to reach an agreement through an expert consensus method.
3.8 Drafting and publishing the guideline document - in what format should a full guideline documentary be drafted, and where should it be published?
The full-text guideline will be drafted with sections of introduction, guideline development methods, recommendations, discussion, and limitations included. A separate document detailing the grades of recommendations and evidence quality will be prepared for guideline users to facilitate their application. The guideline will be published in relevant professional journals and on special guideline websites. A series of academic conferences will be held to promote the implementation of guidelines.
3.9 Updating – how often should the guideline be updated?
A review of the guideline will take place every five years, and recommendations will be adjusted based on updated evidence and feedback from medical professionals. The guideline development group will collect clinical practitioners' suggestions, and the systematic review group will update the evidence.
4. Discussion
As compared to guidelines based solely on CM evidence, a comprehensive set of recommendations that can reduce the disease burden for SLE patients in Hong Kong can be provided by integrative medicine guidelines. According to a report, Asian populations are more likely to suffer from SLE than non-Asian populations as Asian patients have a higher disease activity and higher incidence of comorbidities compared with non-Asian with SLE(19). Across Asia, Hong Kong has the second-highest mean annual total cost of care per SLE patient(19). Treatment of SLE in Hong Kong is consistently associated with a high economic burden, especially when multimorbidity is present(19). For example, SLE patients with cardiovascular disease (CVD), seizures, and neuropsychiatric SLE incurred significantly higher disease costs compared with the general SLE patient population(19). Compared to the general SLE population, the presence of comorbidities increased annual healthcare costs by 44–114%, constituting the overall burden of healthcare utilization(19). TCM which is most known for its use of acupuncture and Chinese herbal medicine has been practised for more than 2000 years. Nowadays, TCM is being scientifically studied for its therapeutic effectiveness in a wide range of diseases(20). SLE patients with certain comorbidities can benefit from the integration of TCM and CM(21-23). As a result, hospital stays and hospital expenditures can be decreased, thereby reducing Hong Kong's economic burden in the management of SLE with comorbidities. Besides, compared to CM, TCM has the advantage of having a lower cost in general. Therefore, TCM should play a role in managing SLE with comorbidities in Hong Kong.
Under the TCM theory of "treatment based on syndrome differentiation", TCM has advantages over CM because it treats a broad spectrum of symptoms instead of a single symptom, which makes it appropriate to treat multimorbidity in SLE. Several clinical studies demonstrated that oral herbal medicine in TCM is an alternative medicine that can target comorbidities. A12-year population-based retrospective cohort study in Taiwan addressed the evidence that the risk of CVD in SLE patients can be reduced by the combined therapy of CM and TCM. Ten frequently used TCM pattern prescriptions were investigated, and among them, Shu-Jing-Huo-Xue-Tang was found to have a significant protective effect against CVD in SLE patients(21). An RCT conducted by Ye with 42 participants indicated that secondary osteoporosis, one of the most common comorbidities of SLE, can be improved by combining TCM formula Bu-Shen-Qiang-Shen Pill with CM including hormone therapy and calcium carbonate tablets with calcitriol capsules(22). Infection is also a major comorbidity of SLE. It is induced by the involvement of infectious agents in the pathogenesis of SLE when the immune defence capacity declines(24). TCM views yin deficiency and blood heat as essential pathological mechanisms underlying infection coexisting with SLE(25). A study showed that Xijiao Dihuang decoction contains yin-nourishing and heat-clearing herbs such as Rehmannia glutinosa (Gaertn.) DC., Paeonia lactiflora Pall. and Paeonia suffruticosa Andrews have immunosuppressive, antibacterial, anti-inflammatory, and antiviral effects in the management of SLE(26). External use of TCM has also been reported to have beneficial effects among SLE patients with bacterial ulcers of limb skin(27).
The first Chinese Medicine Hospital (CMH) in Hong Kong is scheduled to commence service within three years. Both inpatient and outpatient services will be provided by the CMH where TCM plays a dominant role. This will result in the integration of TCM-CM medicine becoming increasingly important in Hong Kong's medical system. Currently, TCM practitioners in Hong Kong rely on their knowledge and experiences in medicine when treating SLE patients with comorbidities. A guideline on integrative medicine in managing SLE with comorbidities is thus crucial to guide TCM and CM clinics and hospitals in Hong Kong in the future. Although some studies have reported beneficial effects of the combined use of TCM and CM on patients with SLE with a variety of comorbidities, there is still a lack of clinical studies examining the effects of integrative medicine on certain comorbidities among SLE patients of high quality or quantity. When there are insufficient high-quality studies incorporated into the guideline, it may be difficult to evaluate the TCM research evidence on SLE with comorbidities objectively. Therefore, TCM applications in treating conditions related to various systems in the general population may also be considered as evidence in the development of the guideline if sufficient evidence on TCM's efficacy and safety on the immune system, especially in SLE, is reviewed.
5. Conclusion
The burden of SLE is not limited to the life-threatening condition itself, but also to the comorbidities that often accompany it. Multimorbidity brings heavy burdens of disease on individuals and society. For this reason, comprehensive recommendations for improving the management of SLE patients with comorbidities should be provided. The purpose of this project is to develop an integrative medicine CPG for managing SLE with comorbidities in Hong Kong. A total of nine steps were recommended in this framework, attempting to make complex judgments. This CPG marks an important step toward establishing guidelines regarding multimorbidity in SLE, despite the lack of high-quality evidence in the CPG. It is necessary to conduct further studies with large-scale clinical trials to update and adjust recommendations in the future. Furthermore, this framework also provides methods for conducting integrative medicine guidelines that address multimorbidity in other diseases.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
All authors declare no conflict of interest.
Funding
The work was supported by Wong’s Donation (Project Code: 200006276), the Gaia Family Trust (Project Code: 200007008), Research Grant Council, HKSAR (Project Code RGC/GRF 17121419), the Health and Medical Research Fund (Project Codes 15162961, 16172751, 17181101 and 18192141) and the Chinese Medicine Development Fund (Project Code 19SB2/002A).
Authors’ contributions
YF and CSL conceived and designed the study. YC and PHL developed the search terms and drafted the manuscript. CZ and NW reviewed the protocol and revised the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgements
Not applicable.
References
- Cojocaru M, Cojocaru IM, Silosi I, Vrabie CD. Manifestations of systemic lupus erythematosus. Maedica (Bucur) 6 (2011): 330-6.
- Borchers AT, Naguwa SM, Shoenfeld Y, Gershwin ME. The geoepidemiology of systemic lupus erythematosus. Autoimmun Rev 9 (2010): A277-87.
- Li M, Zhao Y, Zhang Z, Huang C, Liu Y, Gu J, et al. Chinese guidelines for the diagnosis and treatment of systemic lupus erythematosus. Rheumatology and Immunology Research 59 (2020): 172-85.
- Mok CC. Epidemiology and survival of systemic lupus erythematosus in Hong Kong Chinese. Lupus 20 (2011): 767-71.
- Kuo CF, Chou IJ, Rees F, Grainge MJ, Lanyon P, Davenport G, et al. Temporal relationships between systemic lupus erythematosus and comorbidities. Rheumatology (Oxford) 58 (2019): 840-8.
- Gergianaki I, Garantziotis P, Adamichou C, Saridakis I, Spyrou G, Sidiropoulos P, et al. High Comorbidity Burden in Patients with SLE: Data from the Community-Based Lupus Registry of Crete. J Clin Med 10 (2021).
- Uhlig K, Leff B, Kent D, Dy S, Brunnhuber K, Burgers JS, et al. A framework for crafting clinical practice guidelines that are relevant to the care and management of people with multimorbidity. J Gen Intern Med 29 (2014): 670-9.
- Ha Y, Lee KH, Jung S, Lee SW, Lee SK, Park YB. Glucocorticoid-induced diabetes mellitus in patients with systemic lupus erythematosus treated with high-dose glucocorticoid therapy. Lupus 20 (2011): 1027-34.
- Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis JN, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 78 (2019): 736-45.
- Lam TP. Strengths and weaknesses of traditional Chinese medicine and Western medicine in the eyes of some Hong Kong Chinese. J Epidemiol Community Health 55 (2001): 762-5.
- Wong WC, Lee A, Wong SY, Wu SC, Robinson N. Strengths, weaknesses, and development of Traditional Chinese Medicine in the health system of Hong Kong: through the eyes of future Western doctors. J Altern Complement Med 12 (2006): 185-9.
- Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. Development of the AGREE II, part 1: performance, usefulness and areas for improvement. Cmaj 182 (2010): 1045-52.
- Chen Y, Yang K, Marušic A, Qaseem A, Meerpohl JJ, Flottorp S, et al. A Reporting Tool for Practice Guidelines in Health Care: The RIGHT Statement. Ann Intern Med 166 (2017): 128-32.
- Guyatt G, Akl EA, Hirsh J, Kearon C, Crowther M, Gutterman D, et al. The vexing problem of guidelines and conflict of interest: a potential solution. Ann Intern Med 152 (2010): 738-41.
- Ostensen M, Villiger PM. Nonsteroidal anti-inflammatory drugs in systemic lupus erythematosus. Lupus 9 (2000): 566-72.
- Morrison A, Ramey DR, van Adelsberg J, Watson DJ. Systematic review of trials of the effect of continued use of oral non-selective NSAIDs on blood pressure and hypertension. Curr Med Res Opin 23 (2007): 2395-404.
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64 (2011): 383-94.
- Guyatt GH, Oxman AD, Kunz R, Atkins D, Brozek J, Vist G, et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol 64 (2011): 395-400.
- Zhu TY, Tam LS, Lee VW, Lee KK, Li EK. Systemic lupus erythematosus with neuropsychiatric manifestation incurs high disease costs: a cost-of-illness study in Hong Kong. Rheumatology (Oxford) 48 (2009): 564-8.
- Liu B, Zhang Y, Hu J, He L, Zhou X. Thinking and practice of accelerating transformation of traditional Chinese medicine from experience medicine to evidence-based medicine. Front Med 5 (2011): 163-70.
- Yu HH, Hsieh CJ. Integrative Therapy Combining Chinese Herbal Medicines With Conventional Treatment Reduces the Risk of Cardiovascular Disease Among Patients With Systemic Lupus Erythematosus: A Retrospective Population-Based Cohort Study. Front Pharmacol 12 (2021): 737105.
- YE XB. Clinical Observation of Therapy of Tonifying Kidney and Strengthening Bone for Treatment of Glucocorticoid-induced Osteoporosis in Systemic Lupus Erythematosus. Journal of Guangzhou University of Traditional Chinese Medicine 31 (2014).
- Chen JM, Qian X. Clinical study on combined traditional Chinese and western medicine in the treatment of systemic lupus erythematosus with secondary osteoporosis. Jiangsu Journal of Traditional Chinese Medicine 3 (2010): 14-6.
- Illescas-Montes R, Corona-Castro CC, Melguizo-Rodríguez L, Ruiz C, Costela-Ruiz VJ. Infectious processes and systemic lupus erythematosus. Immunology 158 (2019): 153-60.
- Shen PA. Clinical study of lupus erythematosus with traditional Chinese medicine. China: People's Medical Publishing House 221 (1997).
- Wei F, Song Y, Gong A, Pan C, Zhuang Y, Zhang X, et al. Investigating the Molecular Mechanism of Xijiao Dihuang Decoction for the Treatment of SLE Based on Network Pharmacology and Molecular Docking Analysis. Biomed Res Int (2022): 5882346.
- Ke L, Deng HQ. Treatment of systemic lupus erythematosus complicated with skin bacterial ulcer with traditional Chinese medicine. Guangdong Medical Journal 29 (2008).


 Impact Factor: * 3.3
Impact Factor: * 3.3 Acceptance Rate: 74.39%
Acceptance Rate: 74.39%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 