Bilobed Flap for Post-Traumatic Angular Deformity Correction of the Fingers in Children
João Pedro Farina Brunelli*, Ricardo Kaempf, Diego Falcochio
Hospital Santa Casa de Misericórdia de Porto Alegre, Rua Professor Annes Dias, 295 - Centro Histórico, Porto Alegre - RS, Brazil
*Corresponding Author: João Pedro Farina Brunelli, Hospital Santa Casa de Misericórdia de Porto Alegre, Rua Professor Annes Dias, 295 - Centro Histórico, Porto Alegre - RS, Brazil
Received: 17 October 2023; Accepted: 25 October 2023; Published: 02 November 2023
Article Information
Citation: João Pedro Farina Brunelli, Ricardo Kaempf, Diego Falcochio. Bilobed Flap for Post- Traumatic Angular Deformity Correction of the Fingers in Children. Journal of Orthopedics and Sports Medicine. 5 (2023): 416-419.
View / Download Pdf Share at FacebookAbstract
The Fingertip injuries, usually caused by domestic accidents, such as finger crushing in doors and windows, are very common in childhood. They can cause fractures, nail bed injuries and amputations, as well as combined injuries. Initial management, with correct diagnosis and treatment, is critical for the prevention of complications, whose incidence can reach almost 50% of cases. Severe injuries or inadequate treatment can compromise bone growth, causing deformities and loss of finger alignment, impairing function and skill development in later life.
We describe a surgical treatment technique for correcting cases of posttraumatic angular deformities of the distal interphalangeal (DIP) joint using a bilobed flap associated with bone reduction. This technique allowed achieving good skin coverage after bone realignment without requiring skin grafts or more complex flaps.
The bilobed flap proved to be a good tool for correcting severe angular deformities of the fingers in the pediatric population, allowing for large correction, and providing skin coverage that is easy to apply with tissue similar to the recipient area.
Its use minimizes the risk of complications associated with more complex flaps with less surgical time and predictable results.
Keywords
<p>Bilobed flap; Angular deformity; Fingertip injury; Pediatric hand trauma</p>
Article Details
1. Introduction
Fingertip injuries, usually caused by domestic accidents, such as finger crushing in doors and windows [1], are very common in childhood. They can cause fractures, nail bed injuries, and amputations, as well as combined injuries. Initial management, with correct diagnosis and treatment, is critical for the prevention of complications, whose incidence can reach almost 50% [2]. Severe injuries or inadequate treatment can compromise bone growth, causing deformities and loss of finger alignment, impairing function and skill development in later life [3].
Post-traumatic angular deformity in children's fingers is a possible and not so rare complication, which sometimes occurs regardless of treatment. Malalignment may occur due to post-traumatic physeal closure, soft tissue contracture, or failure to reduce the physeal fracture or promote adequate bone fixation in the initial management. The greater the physeal damage or the farther the fracture is from the physis, the lower the remodeling power, leading to risks of deformities [4].
The management of large angular deformities or fingers with extensive scarring hinders primary closure of the apex of the correction, requiring the use of skin grafts or flaps and making the procedure more complex and longer and leading to morbidity in the donor area.
We describe a surgical treatment technique for correcting cases of post-traumatic angular deformities of the distal interphalangeal (DIP) joint using a bilobed flap associated with bone reduction. With this technique we achieve good skin coverage after bone realignment without the need for skin grafts or more complex flaps.
2. Anatomy
The fingertip is conceptually the area between the DIP and the most distal aspect of the finger [1]. The normal and proportional finger growth, maintaining the alignment, relies on the integrity of the structures comprising this region, such as the physis of the distal phalanx, the nail matrix, the DIP collateral ligaments, and the insertions of the flexor digitorum profundus (FDP) tendons, distal to the physis, and terminal extensor, proximal to the physis.
Trauma to this region can impair these structures, and failure to restore normal anatomy will cause fingertip asymmetric growth with possible angular and rotational deviations [5].
3. Indications
The technique is indicated for chronic post-traumatic angular fingertip deformities in children. Alignment correction with osteotomy and/or capsuloligamentous release shall be performed, which ends up hindering primary cutaneous closure after correction.
Besides the presence of angulation, the existence of scar tissue with reduced elasticity also makes the treatment of these children more difficult. Fibrotic tissue compromises the reduction and hinders primary cutaneous closure, even in cases of minor deviations, and shall be removed and replaced by healthy tissue using a cutaneous flap.
The bilobed flap is a double transposition random pattern flap that allows primary closure of the defect without requiring grafting of the donor area, traditionally used for the nasal region due to the low mobility of the skin in the region. It is also used due to the poor aesthetic quality resulting from skin grafts and other local and pedicled flaps that have the potential to cause significant anatomical distortions [6].
Over time, good results led to the expansion of its indications to other regions of the face, such as the lips and the ear region [7]. In the hand, this flap has already been used in the treatment of congenital deformities causing abnormal angulation of the fingers, such as clinodactyly [8], and in the treatment of tumors, such as mucous cysts [9].
A contraindication of the technique is the poor quality of the skin in the donor area, which in general will be on the opposite side of the correction area, contralateral to the apex of the deformity.
4. Technique
The procedure is performed under general anesthesia, using a pneumatic tourniquet. The first step is to define the primary cause of the deformity, whether it is a bone (malunion or asymmetric growth) or capsuloligamentous (injury to DIP collaterals and secondary stabilizers) one. Once the cause has been identified, the region at the apex of the deformity must be imagined as if it were circular, and the radius of this circle will be the basis for designing the flaps (Figure 1) [6,10].
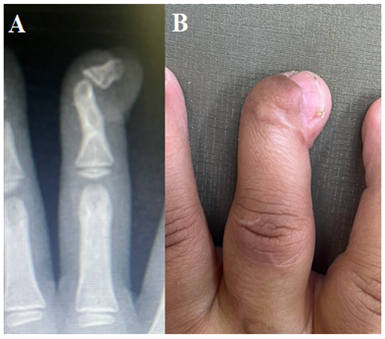
Figure 1: Radiographic (A) and clinical (B) appearance of a severe angular deformity in the coronal plane of the DIP of the third finger of a 6-year-old child, sequel to inadequate treatment of crushing in a window.
The use of the 180° model of rotation by Esser or the 90° modification by Zitelli depends on the region of greatest laxity and on skin quality. After designing the flaps, the apex region is incised transversely or circularly with resection of all scar tissue that could prevent correction, and realignment of the finger is performed through osteotomy and capsuloligamentous release, fixing the DIP aligned with one 1.0 mm or 1.2 mm Kirschner wire. Covering the primary defect with one of the lobes of the flap allows the correction to be completely performed at that moment, with no need for more complex axial flaps or skin grafts, providing coverage with tissue similar to the original, maximizing the cosmetic result. The Kirschner wire is removed after 6 to 8 weeks, and family members are instructed about home rehabilitation exercises (Figure 2).
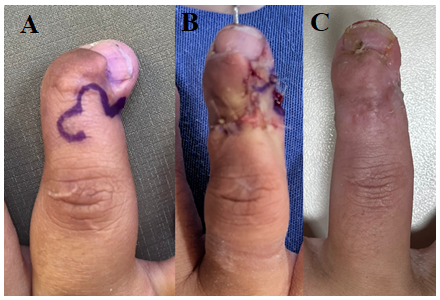
Figure 2: Surgical planning. Bilobed flap designed to transpose the skin on the dorsum of the finger and the region contralateral to the surgical site. The defect is imagined as if it were circular to draw the lobes; however, the incision of the correction area is carried out transversely (radius of the circle) from the flap pivot point (A). Final transoperative appearance demonstrating good alignment of the finger and good perfusion of the flaps (B). Clinical appearance 6 weeks after the surgery, after removal of the Kirschner wire and skin healing (C).
5. Expected Results
At the end of the healing period, good alignment of the finger is expected with adequate skin coverage, similar to the original tissue, and an almost imperceptible scar. The advantage of this technique is that it provides sufficient skin coverage to promote large corrections without requiring complex flaps, making the procedure performance shorter and easier, with similar or better results.
6. Complications
Partial or total necrosis of the lobes, injury to the extensor mechanism during flap elevation, insufficient coverage of the correction area, and infection are possible complications.
7. Discussion
Fingertip injuries, when underdiagnosed and inadequately treated, are often the cause of nail and angular deformities of the fingers [11,12], with sometimes severe aesthetic and functional impairment, as demonstrated in the case described in the technique description. Angular correction, when performed early, allows adequate development of hand function in the most important phases of manual skill formation.
Typically, fractures associated with fingertip crush injuries in children are Salter type I and II physeal fractures with flexion deformity [11] due to insertion distal to the physis of the flexor tendon and proximal to the physis of the extensor tendon [3]. On the other hand, these injuries frequently combine capsuloligamentous, cutaneous, and tendinous components, and may cause deformities in all planes. Deformities in the coronal plane of the fingers are associated with severe aesthetic and functional impairment and must be corrected early.
The bilobed flap, originally described by Esser and modified and popularized by Zitelli, is a good alternative for skin coverage of areas with little skin mobility, such as the nose, and is more often used in facial plastic surgery, rather than simple skin grafting, which does not provide such a satisfactory aesthetic result, and the creation of axial flaps, in which the complexity and morbidity of the procedure can be greater, leading to greater morbidity and surgical time [6]. Its use has also expanded over time to other areas of the face, such as the ear, chin and lips, mainly for circular defects after tumor removal [7,10].
In hand surgery, this flap has already been described for covering defects secondary to the removal of tumors, such as DIP mucous cysts [9]. Of the fingers and for the angular correction of congenital deformities [8]. It is a good tool whenever large angular correction is required that hinders primary closure of the correction area.
8. Conclusion
The bilobed flap proved to be a good tool for correcting severe angular deformities of the fingers in the pediatric population, allowing for large correction, and providing skin coverage that is easy to apply with tissue similar to the recipient area.
Its use allows minimizing the risk of complications associated with more complex flaps and with less surgical time and predictable results.
References
- Weir Y. Fingertip injuries in children: A review of the literature. Emergency Nurse. RCN Publishing Company Ltd. 26 (2018).
- Lankachandra M, Wells CR, Cheng CJ, et al. Complications of Distal Phalanx Fractures in Children. Journal of Hand Surgery 42 (2017): 574.e1-574.e6.
- Papadonikolakis A, Li Z, Smith BP, et al. Fractures of the phalanges and interphalangeal joints in children. Hand Clinics 22 (2006): 11-18.
- Hennrikus WL, Cohen MR. Complete remodelling of displaced fractures of the neck of the phalanx. Journal of Bone and Joint Surgery - Series B 85 (2003): 273-274.
- Kreutz-Rodrigues L, Gibreel W, Moran SL, et al. Frequency, Pattern, and Treatment of Hand Fractures in Children and Adolescents: A 27-Year Review of 4356 Pediatric Hand Fractures Hand. SAGE Publications Inc. 17 (2022): 92-97.
- Cook JL. Reconstructive Utility of the Bilobed Flap: Lessons from Flap Successes and Failures (2005).
- Ricks M, Cook J. Extranasal Applications of the Bilobed Flap (2005).
- Kaempf R, Brunelli JPF, Aita MA, et al. Bilobed Flap in Hand Clinodactyly Reconstruction: Technique Description and Result Appraisal. Rev Bras Ortop (Sao Paulo) 57 (2022): 642-648.
- Jiménez I, Delgado PJ, Kaempf de Oliveira R. The Zitelli Bilobed Flap on Skin Coverage After Mucous Cyst Excision: A Retrospective Cohort of 33 Cases. Journal of Hand Surgery 42 (2017): 506-510.
- Steele RB, Jellinek NJ, Foy A, et al. Use of Extranasal Bilobed Transposition Flaps in Cutaneous Reconstructive Surgery at 2 Institutions. Dermatol Surg 46 (2020): 1279-1285.
- Gibreel W, Charafeddine A, Carlsen BT, et al. Salter-harris fractures of the distal phalanx: Treatment algorithm and surgical outcomes. Plast Reconstr Surg 142 (2018): 720-729.
- Jerome JTJ, Prabu GR. Closed wedge osteotomy for middle phalanx physeal injuries associated with angulation deformities in children. European Journal of Trauma and Emergency Surgery 48 (2022): 3765-3775.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 