Biomechanical Comparisons of Bone-Patellar Tendon-Bone Graft With or Without Suture Tape for Anterior Cruciate Ligament Reconstruction
Hong Li1,2, Lawrence Berglund1, Subin Lin1, Zhanwen Wang1, Aaron J. Krych1, Chunfeng Zhao1*
1Department of Orthopedic Surgery, Mayo Clinic, First Street SW, Rochester, MN 55905 USA
2Department of Sports medicine, Huashan Hospital, 12 Wulumuqi Rd (M), Jing'An, Shanghai, China
*Corresponding Author: Chunfeng Zhao, Department of Orthopedic Surgery, Mayo Clinic, 200 First Street SW, Rochester, MN 55905 USA.
Received: 11 November 2023; Accepted: 17 November 2023 2023; Published: 24 November 2023
Article Information
Citation: Hong Li, Lawrence Berglund, Subin Lin, Zhanwen Wang, Aaron J. Krych, Chunfeng Zhao. Biomechanical Comparisons of Bone-Patellar Tendon-Bone Graft With or Without Suture Tape for Anterior Cruciate Ligament Reconstruction. Journal of Orthopedics and Sports Medicine. 5 (2023): 428-436.
View / Download Pdf Share at FacebookAbstract
The suspensory fixations are utilized as femoral fixation for BPTB grafts with the advantages of precise position of the tunnel and high tensile strength. However, there remains a concern that BPTB grafts fixed with sutures and button might fail as a result of bone plug fracture or sutures cutting through the bone. The aim of this study was to investigate the biomechanical strength of bone-patellar tendon-bone (BPTB) graft with or without independent suture tape reinforcement in anterior cruciate ligament (ACL) reconstruction. Twenty-four knees from dogs were used, including ACL-intact knees (Intact group, n = 8), ACL reconstructed knees (BPTB group, n = 8), and ACL reconstructed knees with suture tape augmentation (BPTB- internal brace (IB) group, n = 8). Specimens were mounted on the MTS system by securing the femur and tibia within custom-made clamps. The joint was positioned in 30° of flexion. A 67 N anterior tibial loading condition was applied to test anterior tibial translation (ATT, mm). After loading, the devices and construct grafts were further displaced at 50 mm/min until failure. The failure mechanism was recorded. Cyclic displacement at 67 N (mm), ultimate failure load (N), and pullout stiffness (N/mm) were determined. Under the 67 N anterior tibial load, the ATT was 1.3 ± 0.3 mm for the intact group, 8.0 ± 5.0 mm for the BPTB group, 2.1 ± 1.0 mm for the BPTB-IB group. The ATT of the BPTB-IB group was significantly lower than that of the BPTB group (p < 0.001).
Regarding the failure mode during the failure testing, the BPTB group had all samples of sutures cutting through the bone and the BPTB-IB group failed in all samples by breakage or loosening of suture tape and then sutures cutting through the bone. The BPTB-IB group had a higher ultimate failure load than the BPTB group (668 ± 159 N vs 230 ± 87 N; p < 0.001). The mean stiffness of the BPTB-IB group was also significantly higher than that of the BPTB group (28 ±7 N/mm vs. 11 ± 3 N/mm; p < 0.001). The suture tape augmentation increased knee stability and ACL failure strength after ACL reconstruction with BPTB. Therefore, this technology could be helpful to reduce the complications of ACL reconstruction such as graft failure and promote patients back activities sooner after reconstruction, especially for the young athletic patients.
Keywords
<p>Knee; ACL; BPTB; Suture tape; Biomechanical</p>
Article Details
1. Introduction
Bone-patellar tendon-bone (BPTB) graft is popular for anterior cruciate ligament (ACL) reconstruction because of their enhanced "bone-to-bone" healing in the bone tunnels compared with tendon-to-bone healing [1]. For BPTB grafts, femoral fixations are usually used with interference screws [2,3]. Interference screws have traditionally been the most common choice for fixation, but interference screws present several disadvantages, such as bone socket posterior wall blowout, difficulty with insertion, and potential graft damage during insertion. Although it is not as commonly used with BPTB grafts, suspensory fixation is used by several groups [4-10]. In some studies, the suspensory fixations, such as Endobutton or Tightrope, are utilized as femoral fixation for BPTB grafts with the advantages of precise position of the tunnel and high tensile strength [4]. Cortical suspensory fixation increases the graft-bone contact area and decreases the risk of posterior wall blowout and damage to the soft tissue portion of the graft [4]. In a randomized clinical trial, Webster et al. [5] analyzed bone tunnel enlargement between hamstring and BPTB grafts in ACL reconstructions over the course of a 2-year follow-up, and found that the hamstring group had a significantly greater femoral tunnel width than the BPTB group. In the BPTB group nine patients (32%) had femoral tunnel obliteration (on both AP and lateral views) from 4 months onwards. This study demonstrated that femoral suspensory fixation was not the principal reason of femoral tunnel enlargement. Previously, Taketomi et al. [6] investigated the efficacy of using a suspensory button for femoral fixation with BPTB graft and they demonstrated that the suspensory fixation could be considered a effective device for femoral fixation with BPTB autograft. However, there remains a concern that BPTB grafts fixed with sutures and button might fail as a result of bone plug fracture or sutures cutting through the bone [11].
Independent suture tape reinforcement has been applied for lateral ankle ligaments repair [12-14], anterior inferior tibiofibular ligament repair [15], Achilles tendon repair [16,17], deltoid ligament [18], spring ligament repair [19], ulnar collateral ligament repair [20-22], patellar tendon repair [23,24], knee medial collateral ligament repair [25,26], ACL repair [27-31]. In a canine ACL reconstruction model using internal brace, Cook et al. [29] demonstrated that the combination of a tendon allograft with internal brace (IB) was an effective load-sharing ACL construct. It prevented early failure and promoted four-zone graft-to-bone healing while avoiding problems noted with use of a pure synthetic graft, such as LARS (Ligament Advanced Reinforcement System). The independent suture tape reinforcement acted as a secondary stabilizer after reconstruction, which may allow accelerated rehabilitation and return to sports. Furthermore, it was reported that independent suture tape reinforcement for ACL reconstruction reduced graft elongation and had a higher ultimate failure load [32]. Bedi [33] suggested this independent suture tape reinforcement was a “Safety Belt” to reinforce ACL grafts. However, this concept has not been studied when a BTPB graft is used for ACL reconstruction. Therefore, the aim of this study was to investigate the biomechanical properties of BPTB graft with or without independent suture tape reinforcement in anterior cruciate ligament (ACL) reconstruction and to analyze whether bundling the independent suture tape reinforcement with BPTB graft could enhance biomechanical properties such as failure strength and stiffness. The hypothesis tested was that the independent suture tape would significantly increase graft failure strength and stiffness at time zero, and maintain graft integrity without elongation of the BPTB graft.
Article I. 2. Materials and Methods
2.1 Specimen preparation
Twenty-four fresh-frozen stifle joints were obtained from the dogs that were sacrificed from IACUC approved studies. The joints were frozen at -20°C and thawed for 24 h before use. Twenty-four knees were randomly divided into 3 groups: group 1) intact ACL (Intact), 2) BPTB reconstruction alone (BPB), and 3) BPTB reconstruction with suture tape augmentation (BPTB- IB). In the intact ACL group, after preparation of the specimens, all soft tissues were removed except the intact ACL, the femur and tibia were cut and fixed within custom-made clamps on the test machine. In the ACL reconstruction groups, the BPTB grafts were harvested from 16 knees before dissection the soft tissues, and then the knees were randomly assigned either BPTB or BPTB-IB groups.
Article II. 2.2 Surgical procedure
All surgical procedures were performed by a sports medicine surgeon (HL), who had considerable experience in ACL reconstruction surgery. For the BPTB harvest, a longitudinal incision was made from patella to tibial tuberosity. A 5-mm-wide part of the patellar tendon was isolated. Two bone blocks (10 mm in length and 5 mm in diameter) were separated and prepared.
The 2 bone blocks were reshaped and calibrated. Next, two holes were drilled in the middle of the blocks by use of a 1-mm drill. Two FiberWire sutures were passed through the holes for later fixation (Figure 1).
The native ACL was cut from the insertion site. The femoral and tibial tunnels were made with a 5 mm-diameter drill from the ACL insertion sites. The graft with or without an suture tape (Fibertape, Arthrex, Naples FL) was pulled into the bone tunnel. The graft ends were fixed with two buttons (XTENDOBUTTON Fixation, Smith and Nephew). For the BPTB-BPTB-IB group, the Fibertape was inserted in the femoral button by passing it through the eyelets with the free ends on the tibial side (Figure 2 and Figure 3).
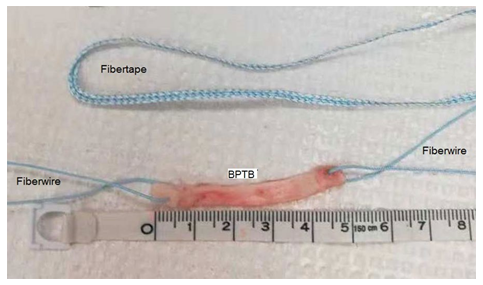
Figure 1: Bone-patellar tendon-bone tendon graft (BPBT) and Suture tape (Fibertape).
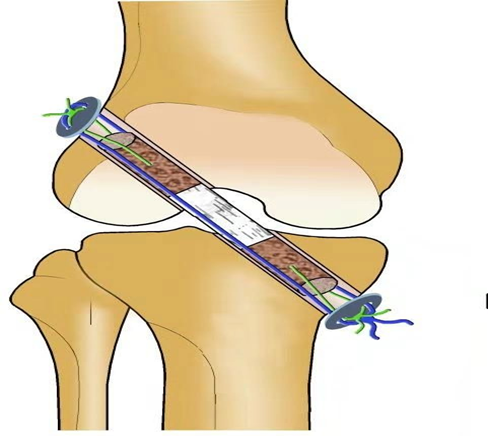
Figure 2: Schematic image showing the ACL reconstruction with Bone-patellar tendon-bone tendon graft (BPBT) and suture tape (Blue line).
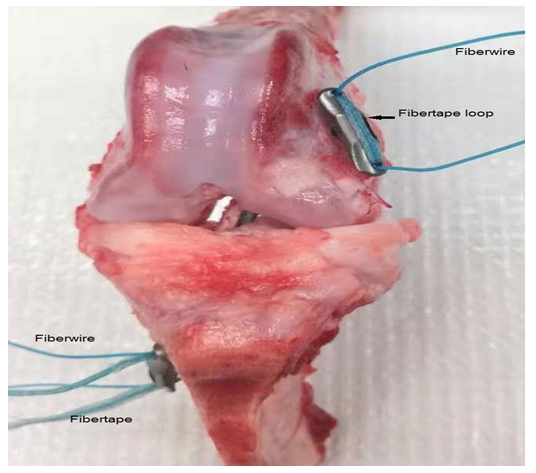
Figure 3: The reconstructed knee using Bone-patellar tendon-bone tendon graft (BPBT) and suture tape.
The knee joint was then motioned to assess anterior drawer, internal rotation, and isometry. With the knee at 30 degrees of flexion, the femoral and tibial loop sutures were tied over the button. Then, the free end of the suture tape was tied to the button at the tibial tunnel aperture
Article III. 2.3 Biomechanical testing
Specimens were mounted on the Servo-hydraulic testing machine (MTS-312, MTS Systems, Eden Prairie, Minnesota) by fixing the bones within custom-made clamps. The joint was flexed in joint flexion of 30° (Figure 4). The samples were preloaded from 10 to 50 N at 0.1 Hz for 10 cycles. A 67 N anterior tibial loading condition was used to test anterior tibial translation (ATT, mm) according to a previous study [34]. Then, the samples were displaced at 50 mm/min until failure. The failure mechanism was recorded (pullout, suture breakage, or intrasubstance tendon elongation). Cyclic displacement at 67 N (mm), ultimate failure load (N), and pullout stiffness (N/mm) were determined.
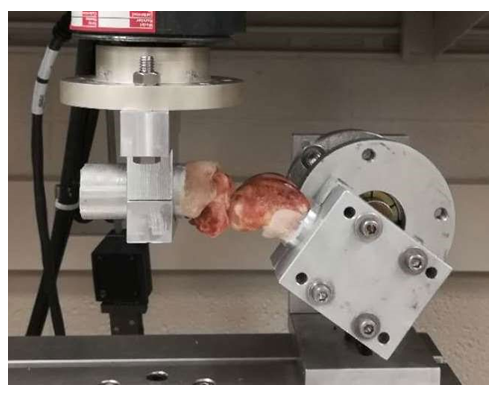
Figure 4: The knee joint will be flexed in joint flexion of 30°.
Article IV. 2.4 Statistical analysis
In order to be able to detect clinically meaningful 1.0 mm differences (SD, 0.7) in ATT among groups with 80% power, eight samples per group were needed [35]. Statistical analysis was performed with the use of STATA version 10.0 (StataCorp LLC, USA). One-way analysis of variance (ANOVA) testing was applied to detect difference between groups. P-values of <0.05 were considered significant.
3. Results
Under the 67N anterior tibial load, the ATT was 1.3 ± 0.3 mm for the intact group, 8.0 ± 5.0 mm for the BPTB group, 2.1 ± 1.0 mm for the BPTB-BPTB-IB group (Figure 5). The native ACL in intact group resulted in the shortest ATT. The ATT of the BPTB-BPTB-IB group was similar to that of the intact group (p > 0.05). BPTB grafts in the BPTB-BPTB-IB group resulted in significantly shorter displacement to failure compared with BPTB alone (p < 0.001).
Regarding the failure mode during the testing, the intact ACL failed in five cases by ligament rupture and three cases of femoral bone fracture. The BPTB-IB group failed in all samples by breakage or knot loosening of suture tape, and then sutures cutting through the bone, while the BPTB group had all samples of sutures cutting through the bone block of BPTB.
The mean failure load for the groups was 230 ± 87 N for BPTB grafts, 668 ± 159 N for BPTB- BPTB-IB group, and 1408 ± 304 N for native ACL ligaments. The mean ultimate failure load of the BPTB-BPTB-IB group was significantly higher than the BPTB group (p < 0.001). The mean ultimate failure load of the either BPTB-IB or BPTB group was still significantly lower than the intact ACL group (p < 0.001; Figure 6).
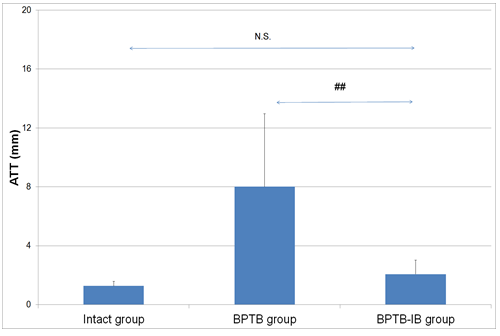
Figure 5: Anterior tibial translation (ATT) under the 67N anterior tibial load for native ACL and BPBT grafts with or without suture tape techniques. “##” indicates a significant difference between groups. “N.S.” indicates no significant difference. BPBT: Bone-patellar tendon-bone tendon graft.
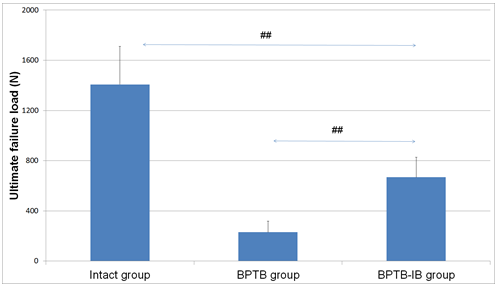
Figure 6: Maximum failure load for native ACL and BPBT grafts with or without suture tape augmentation techniques. “##” indicates a significant difference between groups. BPBT: Bone-patellar tendon-bone tendon graft.
The mean linear stiffness of the femur–ACL graft–tibial complex was 11 ± 3 N/mm for the BPTB group, 28 ± 7 N/mm for BPTB-BPTB-IB group, and 112 ± 22 N/mm for intact ACL. The mean pullout stiffness of the BPTB-BPTB-IB group was significantly higher than the BPTB group (28 ± 7 N/mm vs 11 ± 3 N/mm; p < 0.001). The mean stiffness of the BPTB and BPTB-BPTB-IB groups was still significantly lower than the intact group (p < 0.001; Figure 7,8).
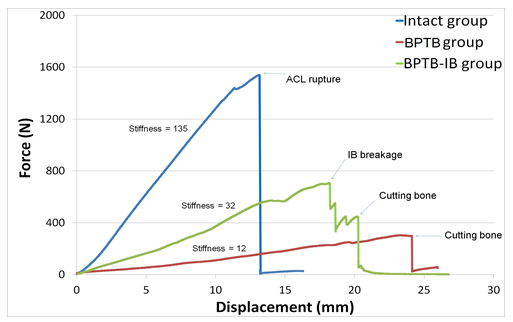
Figure 7: Force/displacement curves for the stiffness analysis between groups. BPBT: Bone-patellar tendon-bone tendon graft. IB: internal brace.
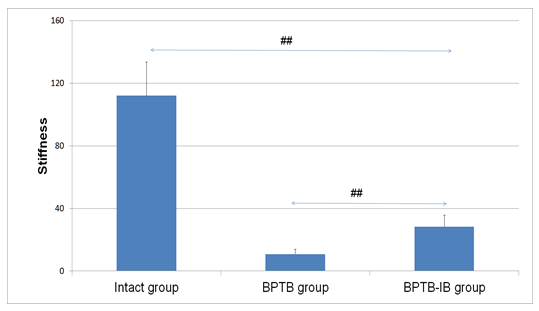
Figure 8: Linear stiffness for native ACL and BPBT grafts with or without suture tape augmentation techniques. “##” indicates a significant difference between groups.
4. Discussion
The function of the suture tape is suggested to be a dynamic safety belt in synergistic load- sharing construct with soft tissue. Previously, several investigations had revealed a higher failure rate in younger patients, although studies had reported reliable outcomes with tendon grafts [36,37]. After implantation, ACL graft undergoes a remodeling process, termed as “ligamentization” [38,39]. During this ligamentization process, the reconstructed tendon graft becomes vulnerable [40,41]. Internal bracing of a tendon graft means a promising strategy in ACL reconstruction, as it may add mechanical reinforcement of the graft, which may be helpful during the graft ligamentization process.
In the present study, the ATT was 1.3 ± 0.3 mm for the intact group, 8.0 ± 5.0 mm for the BPTB group, 2.1 ± 1.0 mm for the BPTB-IB group under the 67N anterior tibial load. This finding indicated that suture tape reinforcement could restore ATT to values similar to the ACL-intact state. Previously, Herbort et al. [42] reported that the ATT of the intact knee, ACL ruptured knee and BPBT reconstructed knee were 7.1 ± 1.2 mm, 14.0 ± 2.6 mm and 8.5 ± 2.1 mm under 134 N anterior tibial load at 30° of knee flexion using human cadaveric knees. Previously in one ACL suture repair study using goat joints, Fisher et al. [34] reported that the mean ATT of ACL intact knee, ACL suture repaired knee and ACL suture augmentation (two Fiberwire sutures) knee were 2.1 ± 0.6 mm, 11.0 ± 3.5 mm and 5.1 ± 2.2 mm respectively under 67 N anterior tibial load at 30° of knee flexion. In addition, in another suture repair study using human cadaveric knees, Hoogeslag et al. [43] analyzed the ATT of the ACL repair with the double loop Fibertape using human cadaveric knee specimens. The mean ATT of the intact ACL group, ACL deficient group and pure ACL repair group were 4.9 ± 1.2 mm, 8.8 ± 2.3 mm and 6.9 ± 2.6 mm, while the tape augmentation group (5.6 ± 2.0 mm) restored ATT to values similar to the ACL-intact state after 10 cyclic loading. Suture augmentation with Fiberwire could restore the tibial translation to within 3mm of the intact joint and may be helpful for ACL remodeling by providing the initial knee joint stability. The current results corroborate these studies. In the current study, the mean ultimate failure load of the BPTB-IB group (668 ± 159 N) was significantly higher than the BPTB group (230 ± 87 N). Previously, Bachmaier et al. [32] compared the ultimate failure load of bovine flexor tendon grafts for ACL reconstruction with and without suture tape using porcine tibia model. Collectively, the ultimate failure load of small diameter (8mm) reinforced grafts were 1592 ± 105 N, which resulted in a 64% increase compared with the controls without suture tape (968 ± 103 N). They demonstrated that independent suture tape reinforcement resulted in significantly higher ultimate failure load without stress-shielding the ACL graft. Furthermore, they reported that the ultimate failure load of pure suture tape was 865 ± 81 N. It is presumed that the fibertape and tendon graft synergistically provided the ultimate load-to-failure strength. To be noted, the tripled tendon grafts without fibertape had already about 968 N of ultimate failure load strength, which might be enough for daily activity. However, in the current study, the BPTB graft had only about 230 N of ultimate failure load, which might be not enough for daily activity if there is no “safety belt”. This indicates the great importance of suture tape reinforcement for BPTB graft. This preliminary study, for the first time, demonstrated the BPTB graft with suture tape reinforcement may be able to allow full weight-bearing at early time after surgery and promise a safer and earlier return to sports.
Furthermore, one major concern that BPTB grafts fixed with sutures and button fails as the sutures cutting through the bone or the bone plug fracture. In this study, the BPTB-IB group failed in all samples by breakage or loose of suture tape reinforcement and then sutures cutting through the bone, while the BPTB group had all samples of sutures cutting through the bone.
Previously, Brown et al. [11] reported that patellar tendon grafts fixed with NO.5 Ethibond sutures and button failed as the sutures cutting through the bone, the bone plug fracture, or the sutures rupture. In a preliminary experiment, No.5 Ethibond sutures were applied to connect the bone plug and button fixations, but suture breakage occurred. As a result, we decided to use NO.2 Fiberwire and observed that all samples failed by sutures cutting through the bone block of the graft.
There are limitations to the current study. Dog knees were used as substitute material for human knee joint. As known, dog knee is smaller than humans, and the strength is lower. However, the dog is a common ACL animal model because of more consistent mechanical properties [44-46]. Moreover, the suture tape reinforcement is one synthetic non-degradable graft. The long time follow-up result after implantation is still not clear. A recent 6-month animal experiment revealed that no suture tape failure was found in ACL reconstruction using a quadriceps tendon allograft with suture tape [29]. Furthermore, the joint was flexed in joint flexion of 30°, and the results in other degrees of flexion were not analyzed. Because the knee joint was fixed in joint flexion of 30° as it does clinically, this degree represented the most stable condition. Finally, it is not certain how the suture tape may affect the biologic healing during the ligamentization process. A further in vivo study will be done in future.
In conclusion, the suture tape augmentation increased knee stability and ACL failure strength after ACL reconstruction with BPTB. Therefore, this technology could be helpful to reduce the complications of ACL reconstruction such as graft failure and promote patients back activities sooner after reconstruction, especially for the young athletic patients.
Article V. Acknowledgment
We would like to thank Zhelin Long, MD, for contributing significantly to the specimen preparation, required for the completion of this project.
Funding:
This study was funded by Mayo Clinic Orthopedic Department Research Program.
References
- Suzuki T, Shino K, Nakagawa S, et al. Early integration of a bone plug in the femoral tunnel in rectangular tunnel ACL reconstruction with a bone-patellar tendon-bone graft: a prospective computed tomography analysis. Knee Surg Sports Traumatol Arthrosc 19 (2011): 29-35.
- Tibor L, Chan PH, Funahashi TT, et al.2016 Surgical Technique Trends in Primary ACL Reconstruction from 2007 to 2014. J Bone Joint Surg Am.98:1079-1089.
- Eysturoy NH, Nissen KA, Nielsen T, et al.2018 The Influence of Graft Fixation Methods on Revision Rates After Primary Anterior Cruciate Ligament Reconstruction. Am J Sports Med 46: 524-530.
- Colombet P, Bouguennec N. Suspensory Fixation Device for Use With Bone-Patellar Tendon-Bone Grafts. Arthrosc Tech 6 (2017): e833-e838.
- Webster KE, Feller JA, Hameister KA. Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 9 (2001): 86-91.
- Taketomi S, Inui H, Nakamura K, et al. Secure fixation of femoral bone plug with a suspensory button in anatomical anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft. Joints 3 (2015): 102-108.
- Barrett GR, Noojin FK, Hartzog CW, et al. Reconstruction of the anterior cruciate ligament in females: A comparison of hamstring versus patellar tendon autograft. Arthroscopy 18 (2002): 46-54.
- Ibrahim SA, Al-Kussary IM, Al-Misfer AR, et al. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy 21 (2005): 412-417.
- Taylor DC, DeBerardino TM, Nelson BJ, et al. Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: a randomized controlled trial using similar femoral and tibial fixation methods. Am J Sports Med 37 (2009): 1946-1957.
- Mohtadi N, Chan D, Barber R, et al. Reruptures, Reinjuries, and Revisions at a Minimum 2-Year Follow-up: A Randomized Clinical Trial Comparing 3 Graft Types for ACL Reconstruction. Clin J Sport Med 26 (2016): 96-107.
- Brown CH, Jr., Wilson DR, Hecker AT, et al. Graft-bone motion and tensile properties of hamstring and patellar tendon anterior cruciate ligament femoral graft fixation under cyclic loading. Arthroscopy 20 (2004): 922-935.
- Cho BK, Park KJ, Kim SW, et al. Minimal Invasive Suture-Tape Augmentation for Chronic Ankle Instability. Foot Ankle Int 36 (2015): 1330-1338.
- Schuh R, Benca E, Willegger M, et al. 2016 Comparison of Brostrom technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc 24 (2015): 1101-1107.
- Yoo JS, Yang EA. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol 17 (2016): 353-360.
- Teramoto A, Shoji H, Sakakibara Y, et al. Suture-Button Fixation and Mini-Open Anterior Inferior Tibiofibular Ligament Augmentation Using Suture Tape for Tibiofibular Syndesmosis Injuries. J Foot Ankle Surg 57 (2018): 159-161.
- McWilliam JR, Mackay G. The Internal Brace for Midsubstance Achilles Ruptures. Foot Ankle Int 37 (2016): 794-800.
- Chida S, Suzuki H, Kobayashi M, et al. Reconstruction of a chronically ruptured Achilles tendon using an internal brace: a case report. J Med Case Rep 12 (2018): 54.
- Nery C, Lemos A, Raduan F, et al. Combined Spring and Deltoid Ligament Repair in Adult-Acquired Flatfoot. Foot Ankle Int 39 (2018): 903-907.
- Acevedo J, Vora A. Anatomical reconstruction of the spring ligament complex: "internal brace" augmentation. Foot Ankle Spec 6 (2013): 441-445.
- Dugas JR, Walters BL, Beason DP, et al. Biomechanical Comparison of Ulnar Collateral Ligament Repair With Internal Bracing Versus Modified Jobe Reconstruction. Am J Sports Med 44 (2016): 735-741.
- Clark NJ, Desai VS, Dines JD, et al. Nonreconstruction Options for Treating Medial Ulnar Collateral Ligament Injuries of the Elbow in Overhead Athletes. Curr Rev Musculoskelet Med 11 (2018): 48-54.
- Jones CM, Beason DP, Dugas JR. Ulnar Collateral Ligament Reconstruction versus Repair with Internal Bracing: Comparison of Cyclic Fatigue Mechanics. Orthop J Sports Med 6 (2018): 2325967118755991
- Sanchez G, Ferrari MB, Sanchez A, et al. Proximal Patellar Tendon Repair: Internal Brace Technique With Unicortical Buttons and Suture Tape. Arthrosc Tech 6 (2017): e491-e497.
- Rothfeld A, Pawlak A, Liebler SAH, et al. Patellar Tendon Repair Augmentation With a Knotless Suture Anchor Internal Brace: A Biomechanical Cadaveric Study. Am J Sports Med 46 (2018): 1199-1204.
- Lubowitz JH, MacKay G, Gilmer B. Knee medial collateral ligament and posteromedial corner anatomic repair with internal bracing. Arthrosc Tech 3 (2014): e505-508.
- Gilmer BB, Crall T, DeLong J, et al. Biomechanical Analysis of Internal Bracing for Treatment of Medial Knee Injuries. Orthopedics 39 (2016): e532-537.
- Smith JO, Yasen SK, Palmer HC, et al. Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc 24 (2016): 1845-1851.
- Wilson WT, Hopper GP, Byrne PA, et al. Anterior Cruciate Ligament Repair with Internal Brace Ligament Augmentation. Surg Technol Int 29 (2016): 273-278.
- Cook JL, Smith P, Stannard JP, et al. A Canine Arthroscopic Anterior Cruciate Ligament Reconstruction Model for Study of Synthetic Augmentation of Tendon Allografts. J Knee Surg 30 (2017): 704-711.
- Smith PA, Bley JA. Allograft Anterior Cruciate Ligament Reconstruction Utilizing Internal Brace Augmentation. Arthrosc Tech 5 (2016): e1143-e1147.
- Smith PA, Bley JA. Anterior Cruciate Ligament Primary Repair With Independent Tensioning of the Anteromedial and Posterolateral Bundles. Arthrosc Tech 6 (2017): e2123-e2128.
- Bachmaier S, Smith PA, Bley J, et al. Independent Suture Tape Reinforcement of Small and Standard Diameter Grafts for Anterior Cruciate Ligament Reconstruction: A Biomechanical Full Construct Model. Arthroscopy 34 (2018): 490-499.
- Bedi A. Editorial Commentary: Buckle Up Surgeons: "Safety Belt" Reinforcement of Knee Anterior Cruciate Ligament Reconstruction Grafts. Arthroscopy 34 (2018): 500-501.
- Fisher MB, Jung HJ, McMahon PJ, et al. Suture augmentation following ACL injury to restore the function of the ACL, MCL, and medial meniscus in the goat stifle joint. J Biomech 44 (2011): 1530-1535.
- Jin C, Paluvadi SV, Lee S, et al. Biomechanical comparisons of current suspensory fixation devices for anterior cruciate ligament reconstruction. Int Orthop 42 (2018): 1291-1296.
- Samuelsen BT, Webster KE, Johnson NR, et al. Hamstring Autograft versus Patellar Tendon Autograft for ACL Reconstruction: Is There a Difference in Graft Failure Rate? A Meta-analysis of 47,613 Patients. Clin Orthop Relat Res 475 (2017): 2459-2468.
- Pennock AT, Ho B, Parvanta K, et al. Does Allograft Augmentation of Small-Diameter Hamstring Autograft ACL Grafts Reduce the Incidence of Graft Retear? Am J Sports Med 45 (2017): 334-338.
- Claes S, Verdonk P, Forsyth R, et al. The "ligamentization" process in anterior cruciate ligament reconstruction: what happens to the human graft? A systematic review of the literature Am J Sports Med 39 (2011): 2476-2483.
- Pauzenberger L, Syre S, Schurz M. "Ligamentization" in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy 29 (2013): 1712-1721.
- Sanchez M, Anitua E, Azofra J, et al. Ligamentization of tendon grafts treated with an endogenous preparation rich in growth factors: gross morphology and histology. Arthroscopy 26 (2010): 470-480.
- Muramatsu K, Hachiya Y, Izawa H. Serial evaluation of human anterior cruciate ligament grafts by contrast-enhanced magnetic resonance imaging: comparison of allografts and autografts. Arthroscopy 24 (2008): 1038-1044.
- Herbort M, Tecklenburg K, Zantop T, et al. Single-bundle anterior cruciate ligament reconstruction: a biomechanical cadaveric study of a rectangular quadriceps and bone—patellar tendon--bone graft configuration versus a round hamstring graft. Arthroscopy 29 (2013): 1981-1990.
- Hoogeslag RAG, Brouwer RW, Huis In’t Veld R, et al. Dynamic augmentation restores anterior tibial translation in ACL suture repair: a biomechanical comparison of non-, static and dynamic augmentation techniques. Knee Surg Sports Traumatol Arthrosc 26 (2018): 2986-2996.
- Qi L, Chang C, Jian L, et al. Effect of varying the length of soft-tissue grafts in the tibial tunnel in a canine anterior cruciate ligament reconstruction model. Arthroscopy 27 (2011): 825-833.
- Cook JL, Smith PA, Stannard JP, et al. A canine hybrid double-bundle model for study of arthroscopic ACL reconstruction. J Orthop Res 33 (2015): 1171-1179.
- Smith PA, Stannard JP, Pfeiffer FM, et al. Suspensory Versus Interference Screw Fixation for Arthroscopic Anterior Cruciate Ligament Reconstruction in a Translational Large-Animal Model. Arthroscopy 32 (2016): 1086-1097.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 