Clinical and Ultrasound Features Associated with the Presence or Absence of Calcification in Patients with Symptomatic Shoulders
Alexandre Dumusc, Luisa Orlik, Alain Farron, Pascal Zufferey*
RHU/DAL/centre hospitalier universitaire Vaudois, av Pierre Decker 4, 1005 Lausanne, Switzerland
*Corresponding Author: Dr. Pascal Zufferey, RHU/DAL/centre hospitalier universitaire Vaudois, av Pierre Decker 4, 1005 Lausanne, Switzerland
Received: 30 December 2020; Accepted: 07 December 2020; Published: 11 December 2020
Article Information
Citation: Alexandre Dumusc, Luisa Orlik, Alain Farron, Pascal Zufferey. Clinical and Ultrasound Features Associated with the Presence or Absence of Calcification in Patients with Symptomatic Shoulders. Journal of Orthopaedics and Sports Medicine 2 (2020): 168-182.
View / Download Pdf Share at FacebookAbstract
Background: Acute and chronic shoulder symptoms can be due to calcifications but also to other lesions well detected by Ultrasound (US).
Objective: The present study’s objectives were to determine whether, some demographic, clinical and ultrasound features were associated with the presence or absence of calcifications in symptomatic shoulders patients.
Methods: As part of this retrospective, transversal, case-control study of 490 patients, the 125 patients with calcifications were compared to 125 patients without calcification randomly extracted from the cohort. Subgroups were defined according to types and durations of symptoms. The frequency and types of associated lesions in the two groups, as well as the different US appearances of the calcifications were compared according to their different clinical presentations.
Results: Calcific tendinitis was present in 26% of patients. Demographic characteristics or clinical manifestations, significantly associated with calcifications were: being a woman (p = 0.002), a shorter delay between symptoms and diagnosis (p = 0.007 and have acute symptoms. The presence of calcifications was associated with the absence of associated (42% vs. 6%, p = 0.0001) or less severe associated US lesions, particularly total rotator cuff rupture (5% vs. 18%, p = 0.001). Soft and cystic calcifications without shadowing were found more frequently in patients with hyperalgesic shoulders (p = 0.005) compared to chronic shoulders.
Conclusions: Only few demographic and clinical features were significantly more frequent in the presence of calcifications. US revealed fewer additional lesions when calcifications were present and, some US aspects of the calcification suggested the type of symptoms.
Shoulder pain articles Shoulder pain Research articles Shoulder pain review articles Shoulder pain PubMed articles Shoulder pain PubMed Central articles Shoulder pain 2023 articles Shoulder pain 2024 articles Shoulder pain Scopus articles Shoulder pain impact factor journals Shoulder pain Scopus journals Shoulder pain PubMed journals Shoulder pain medical journals Shoulder pain free journals Shoulder pain best journals Shoulder pain top journals Shoulder pain free medical journals Shoulder pain famous journals Shoulder pain Google Scholar indexed journals Rotator cuff articles Rotator cuff Research articles Rotator cuff review articles Rotator cuff PubMed articles Rotator cuff PubMed Central articles Rotator cuff 2023 articles Rotator cuff 2024 articles Rotator cuff Scopus articles Rotator cuff impact factor journals Rotator cuff Scopus journals Rotator cuff PubMed journals Rotator cuff medical journals Rotator cuff free journals Rotator cuff best journals Rotator cuff top journals Rotator cuff free medical journals Rotator cuff famous journals Rotator cuff Google Scholar indexed journals Bursitis articles Bursitis Research articles Bursitis review articles Bursitis PubMed articles Bursitis PubMed Central articles Bursitis 2023 articles Bursitis 2024 articles Bursitis Scopus articles Bursitis impact factor journals Bursitis Scopus journals Bursitis PubMed journals Bursitis medical journals Bursitis free journals Bursitis best journals Bursitis top journals Bursitis free medical journals Bursitis famous journals Bursitis Google Scholar indexed journals Rheumatologist articles Rheumatologist Research articles Rheumatologist review articles Rheumatologist PubMed articles Rheumatologist PubMed Central articles Rheumatologist 2023 articles Rheumatologist 2024 articles Rheumatologist Scopus articles Rheumatologist impact factor journals Rheumatologist Scopus journals Rheumatologist PubMed journals Rheumatologist medical journals Rheumatologist free journals Rheumatologist best journals Rheumatologist top journals Rheumatologist free medical journals Rheumatologist famous journals Rheumatologist Google Scholar indexed journals Shoulder movement articles Shoulder movement Research articles Shoulder movement review articles Shoulder movement PubMed articles Shoulder movement PubMed Central articles Shoulder movement 2023 articles Shoulder movement 2024 articles Shoulder movement Scopus articles Shoulder movement impact factor journals Shoulder movement Scopus journals Shoulder movement PubMed journals Shoulder movement medical journals Shoulder movement free journals Shoulder movement best journals Shoulder movement top journals Shoulder movement free medical journals Shoulder movement famous journals Shoulder movement Google Scholar indexed journals Chronic shoulder pain articles Chronic shoulder pain Research articles Chronic shoulder pain review articles Chronic shoulder pain PubMed articles Chronic shoulder pain PubMed Central articles Chronic shoulder pain 2023 articles Chronic shoulder pain 2024 articles Chronic shoulder pain Scopus articles Chronic shoulder pain impact factor journals Chronic shoulder pain Scopus journals Chronic shoulder pain PubMed journals Chronic shoulder pain medical journals Chronic shoulder pain free journals Chronic shoulder pain best journals Chronic shoulder pain top journals Chronic shoulder pain free medical journals Chronic shoulder pain famous journals Chronic shoulder pain Google Scholar indexed journals Acute tendinitis articles Acute tendinitis Research articles Acute tendinitis review articles Acute tendinitis PubMed articles Acute tendinitis PubMed Central articles Acute tendinitis 2023 articles Acute tendinitis 2024 articles Acute tendinitis Scopus articles Acute tendinitis impact factor journals Acute tendinitis Scopus journals Acute tendinitis PubMed journals Acute tendinitis medical journals Acute tendinitis free journals Acute tendinitis best journals Acute tendinitis top journals Acute tendinitis free medical journals Acute tendinitis famous journals Acute tendinitis Google Scholar indexed journals Osteoarthritis articles Osteoarthritis Research articles Osteoarthritis review articles Osteoarthritis PubMed articles Osteoarthritis PubMed Central articles Osteoarthritis 2023 articles Osteoarthritis 2024 articles Osteoarthritis Scopus articles Osteoarthritis impact factor journals Osteoarthritis Scopus journals Osteoarthritis PubMed journals Osteoarthritis medical journals Osteoarthritis free journals Osteoarthritis best journals Osteoarthritis top journals Osteoarthritis free medical journals Osteoarthritis famous journals Osteoarthritis Google Scholar indexed journals Joint erosions articles Joint erosions Research articles Joint erosions review articles Joint erosions PubMed articles Joint erosions PubMed Central articles Joint erosions 2023 articles Joint erosions 2024 articles Joint erosions Scopus articles Joint erosions impact factor journals Joint erosions Scopus journals Joint erosions PubMed journals Joint erosions medical journals Joint erosions free journals Joint erosions best journals Joint erosions top journals Joint erosions free medical journals Joint erosions famous journals Joint erosions Google Scholar indexed journals Traumatic lesions articles Traumatic lesions Research articles Traumatic lesions review articles Traumatic lesions PubMed articles Traumatic lesions PubMed Central articles Traumatic lesions 2023 articles Traumatic lesions 2024 articles Traumatic lesions Scopus articles Traumatic lesions impact factor journals Traumatic lesions Scopus journals Traumatic lesions PubMed journals Traumatic lesions medical journals Traumatic lesions free journals Traumatic lesions best journals Traumatic lesions top journals Traumatic lesions free medical journals Traumatic lesions famous journals Traumatic lesions Google Scholar indexed journals Acromio-clavicular joint articles Acromio-clavicular joint Research articles Acromio-clavicular joint review articles Acromio-clavicular joint PubMed articles Acromio-clavicular joint PubMed Central articles Acromio-clavicular joint 2023 articles Acromio-clavicular joint 2024 articles Acromio-clavicular joint Scopus articles Acromio-clavicular joint impact factor journals Acromio-clavicular joint Scopus journals Acromio-clavicular joint PubMed journals Acromio-clavicular joint medical journals Acromio-clavicular joint free journals Acromio-clavicular joint best journals Acromio-clavicular joint top journals Acromio-clavicular joint free medical journals Acromio-clavicular joint famous journals Acromio-clavicular joint Google Scholar indexed journals Infra-spinatus tendon articles Infra-spinatus tendon Research articles Infra-spinatus tendon review articles Infra-spinatus tendon PubMed articles Infra-spinatus tendon PubMed Central articles Infra-spinatus tendon 2023 articles Infra-spinatus tendon 2024 articles Infra-spinatus tendon Scopus articles Infra-spinatus tendon impact factor journals Infra-spinatus tendon Scopus journals Infra-spinatus tendon PubMed journals Infra-spinatus tendon medical journals Infra-spinatus tendon free journals Infra-spinatus tendon best journals Infra-spinatus tendon top journals Infra-spinatus tendon free medical journals Infra-spinatus tendon famous journals Infra-spinatus tendon Google Scholar indexed journals Hyperalgesic articles Hyperalgesic Research articles Hyperalgesic review articles Hyperalgesic PubMed articles Hyperalgesic PubMed Central articles Hyperalgesic 2023 articles Hyperalgesic 2024 articles Hyperalgesic Scopus articles Hyperalgesic impact factor journals Hyperalgesic Scopus journals Hyperalgesic PubMed journals Hyperalgesic medical journals Hyperalgesic free journals Hyperalgesic best journals Hyperalgesic top journals Hyperalgesic free medical journals Hyperalgesic famous journals Hyperalgesic Google Scholar indexed journals Chronic tendinopathy articles Chronic tendinopathy Research articles Chronic tendinopathy review articles Chronic tendinopathy PubMed articles Chronic tendinopathy PubMed Central articles Chronic tendinopathy 2023 articles Chronic tendinopathy 2024 articles Chronic tendinopathy Scopus articles Chronic tendinopathy impact factor journals Chronic tendinopathy Scopus journals Chronic tendinopathy PubMed journals Chronic tendinopathy medical journals Chronic tendinopathy free journals Chronic tendinopathy best journals Chronic tendinopathy top journals Chronic tendinopathy free medical journals Chronic tendinopathy famous journals Chronic tendinopathy Google Scholar indexed journals Calcific tendinitis articles Calcific tendinitis Research articles Calcific tendinitis review articles Calcific tendinitis PubMed articles Calcific tendinitis PubMed Central articles Calcific tendinitis 2023 articles Calcific tendinitis 2024 articles Calcific tendinitis Scopus articles Calcific tendinitis impact factor journals Calcific tendinitis Scopus journals Calcific tendinitis PubMed journals Calcific tendinitis medical journals Calcific tendinitis free journals Calcific tendinitis best journals Calcific tendinitis top journals Calcific tendinitis free medical journals Calcific tendinitis famous journals Calcific tendinitis Google Scholar indexed journals
Article Details
1. Introduction
Shoulder pain is a common reason for medical consultation and is most commonly linked to lesions of the rotator cuff. Rotator cuff calcification-mainly due to basic crystal deposition-is also a common finding and can give rise to chronic pain as well as acute inflammatory episodes [1]. The estimated prevalence of calcium deposits in shoulders is around 3% [2]. However, only one third of the affected shoulders seem to cause some degree of pain or discomfort at one time or another [3]. Factors associated with the development of symptoms in the presence of calcifications are still unclear, although the presence and extent of bursitis on imaging have both been shown to be associated with pain [4, 5]. Until recently, little was known about the impact of other associated rotator cuff lesions on the development of symptoms similar to those induced by calcifications themselves [6-9].
The diagnosis of periarticular shoulder calcifications relies on imaging techniques-mostly X-rays and ultrasound (US) [10, 11]. Both methods can distinguish different visual appearances of calcifications with some correlation to clinical symptoms [12, 13]. US have the advantage of also being a very effective tool for detecting any associated lesions that might also be responsible for symptoms [12]. The present study’s objective was to determine whether some clinical characteristics or US images could discriminate patients with symptomatic shoulders in the presence or absence of calcification. We particularly wanted to analyze whether any of the associated lesions visible via US were found more or less frequently when calcifications were present and whether the visual appearance of those calcifications was associated with any particular clinical manifestations.
2. Methods
This retrospective study included 490 patients with a painful shoulder referred to a rheumatologist working at a secondary care center between 1997 and 2010. Clinical data were extracted from medical reports subsequently addressed to patients’ referring general practitioners. Four clinical categories were defined according to the duration and types of symptoms (inflammatory versus mechanical pain and the presence or absence of limitations to shoulder movement) [14, 15].
A: Acute shoulder pain for ≤ 12 weeks. B: Subacute shoulder pain, mostly inflammatory (at night and at rest), for > 12 weeks but < 1 year. C: Chronic shoulder pain, mostly mechanical pain, for > 1 year. D: Hyperalgesic shoulder pain, inflammatory (at night and at rest), with impaired mobility, and a short duration of ≤ 12 weeks—.representing a subgroup of acute shoulder pain and the classic clinical presentation of an acute flare-up induced by calcification dissolution. The same rheumatologist performed all the US examinations according to a standardized protocol, using an Esaote Mylab 25 ultrasound device. The Doppler mode of this machine was at that time quite fair, that’s why mostly B mode images were recorded as described in detail in the case report sheets. The appearance of calcifications in US images was defined according to the Chiou [16] classification for hydroxyapatite calcification, to which we added one further category: linear calcification located inside the tendon, which might suggest the presence of other crystals, such as calcium pyrophosphate deposition.
The following lesions diagnosable via US were retained: (A) Acute tendinitis : defibrillation, hypo-echogenicity, increase thickness or tenosynovitis : fluid + long head tendon of biceps modifications ; (B) Chronic tendinitis: scars, traction cysts ; (C) Bursitis; fluid in the bursa; (D) Partial rupture of one or more tendons: loss of convex aspect of the tendon (“mépalt”) or non-tranfixiant rupture; (E) Complete rupture : transfixiant or complete retraction of ruptured tendon (“coiffe chauve”) of one or more tendons; (F) Capsulitis: clinical multi-direction limitations without US lesions ; (G) Synovitis/effusion in the shoulder joint; (H) Acromial conditions : acute pain on pression on the joint with or without US lesion ; (I) Other (osteoarthritis, joint erosions, traumatic lesions, etc.) [14, 17, 18].
For the case-control part, detailed clinical and US data concerning the 125 patients in the cohort who had calcification were compared to 125 patients without calcification randomly extracted from the remainder of the same cohort (125/365 patients, see Figure 1). Both groups were compared with descriptive statistics. T-test, Mann-Whitney test and Chi-squared test were performed as appropriate. We did not correct for multiple comparisons. P < 0.05 was considered significant. The variables that were significantly related to the presence of calcification were investigated using logistic regression. Results are presented as odds ratios and 95% confidence intervals. Statistical analysis was performed with STATA 16 software. The study was approved by the Human Research Ethics Committee of the Canton of Vaud (CER-VD 2018-01302).
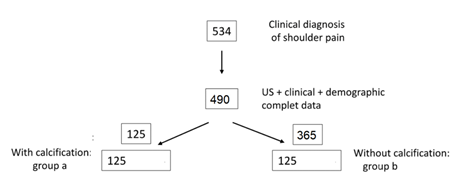
Figure 1: Patients selection for the comparison between patients with calcifications (group: a) and without calcifications (b: control group).
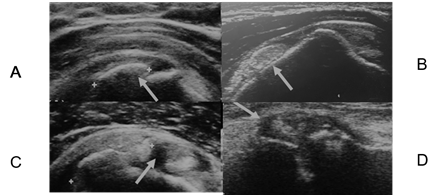
Figure 2: US appearance of calcification. A: arc shape with shadowing in supra-spinatus tendon: longitudinal view. B: soft rounded without shadowing in the bursa: longitudinal view. C: cystic and fragmented in the supraspinatus tendon: transversal view. D: linear calcification in the acromio-clavicular joint.
3. Results
Around a quarter of the patients (125/490) with shoulder symptoms had one or several calcifications. Their demographic and clinical characteristics were compared with those of the 125 patients without calcification, randomly extracted from the remainder of the cohort, and are summarized in Table 1. The locations of these calcifications were the following: supraspinatus tendon: 101, infra-scapularis tendon: 12, infra-spinatus tendon:4 ,bursa: 2 acromioclavicular joint:2 , others: 5.
When comparing the demographic data between these groups, we found no differences in terms of age at diagnosis (p = 0.2), but a significantly greater proportion of women were affected by calcifications (p = 0.002). After using a sensitivity analysis, sex remained the only significantly different demographic factor when comparing the total population of 365 patients without calcification to the 125 patients with calcification (data not shown, p = 0.04). This suggests that the extraction did not lead to any significant demographic biases and that it was representative of the entire population of patients without calcifications.
Clinical presentations were similar in both groups, although the distribution of patients within the different clinical categories was significantly different (p = 0.007). More subjects were found in the acute diagnosis groups than in the chronic shoulder pain groups when calcification was present. The mean duration of symptoms, from their appearance to their clinical and US evaluations, was also significantly shorter when calcifications (p = 0.001) were present. The demographically and clinically associated factors were quite homogeneous among the different clinically defined categories (see Supplementary Table 1). We observed however that patients in the hyperalgesic group were almost always under 60 years old at diagnosis (see Supplementary Figure 1).
|
Sample status |
Without calcification n = 125 |
With calcification n = 125 |
Comparison between groups |
|
Age at diagnosis (years) |
|||
|
mean (SD) |
50.8 (14.3) |
53.1 (11.4) |
p = 0.2 |
|
data available, n (%) |
125 (100) |
123 (98) |
|
|
Sex |
|||
|
Female, n (%) |
55 (44) |
79 (63) |
p = 0.002 |
|
data available, n |
125 |
125 |
|
|
Delay (weeks) |
|||
|
mean (SD) |
70.6 (102.8) |
39.2 (66.6) |
p = 0.001 |
|
median [IQR] |
28.0 [42.0] |
17.0 [32.0] |
|
|
data available, n (%) |
96 (77) |
106 (85) |
|
|
Side affected |
|||
|
Right, n (%) |
5 (83) |
73 (62) |
p = 0.3 |
|
data available, n |
6 |
117 |
|
|
Night pain |
|||
|
Yes, n (%) |
49 (48.5) |
66 (56.4) |
p = 0.2 |
|
data available, n |
101 |
117 |
|
|
Day pain |
|||
|
Yes, n (%) |
100 (95.2) |
114 (93.4) |
p = 0.6 |
|
data available, n |
105 |
122 |
|
|
Functional disability |
|||
|
Yes, n (%) |
34 (32.4) |
52 (43.0) |
p = 0.1 |
|
data available, n |
105 |
121 |
|
|
Diagnosis category |
|||
|
Acute shoulder |
25 (26.0) |
48 (45.3) |
p = 0.007 |
|
Hyperalgesic |
9/96 (9.4) |
16/106 (15.1) |
p = 0.8 |
|
Subacute shoulder |
41 (42.7) |
40 (37.7) |
|
|
Chronic shoulder |
30 (31.3) |
18 (17.0) |
|
|
data available, n (%) |
96 (77) |
106 (85) |
|
Table 1: Comparison of clinical data between patients with and without calcification.
|
Sample status |
Without calcification n = 125 |
With calcification |
Comparison between groups |
|
No lesions Yes, n (%) data available, n US: acute tendinopathy or tenosynovitis |
8 (6.4) |
53 (42.4) |
p = 0.0001 |
|
8 (6.4) |
6 (4.8) |
p = 0.6 |
|
|
US: chronic tendinopathy |
|||
|
Yes, n (%) |
36 (28.8) |
33 (26.4) |
p = 0.7 |
|
data available, n |
125 |
125 |
|
|
US: bursitis |
|||
|
Yes, n (%) |
38 (30.4) |
19 (15.2) |
p = 0.004 |
|
data available, n |
125 |
125 |
|
|
US: partial tendon tear |
|||
|
Yes, n (%) |
22 (17.6) |
18 (14.4) |
p = 0.5 |
|
data available, n |
125 |
125 |
|
|
US: full-thickness tendon tear |
|||
|
Yes, n (%) |
22 (17.6) |
6 (4.8) |
p = 0.001 |
|
data available, n |
125 |
125 |
|
|
US: capsulitis |
|||
|
Yes, n (%) |
5 (4.0) |
3 (2.4) |
p = 0.5 |
|
data available, n |
125 |
125 |
|
|
US: synovitis or effusion |
|||
|
Yes, n (%) |
22 (17.6) |
14 (11.2) |
p = 0.15 |
|
data available, n |
125 |
125 |
|
|
US: acromioclavicular joint involved |
|||
|
Yes, n (%) |
19 (15.2) |
9 (7.2) |
p = 0.045 |
|
data available, n |
125 |
125 |
|
|
US: other |
|||
|
Yes, n (%) |
19 (15.2) |
3 (2.4) |
p = 0.0001 |
|
data available, n |
125 |
125 |
|
|
Statistical tests used: T-test, Mann–Whitney test, chi-squared test, as appropriate. |
|||
Table 2: Comparison of lesions visible via US in patients with and without calcification.
US findings in patients with and without calcification are summarized in Table 2. More than 40% of patients with calcification had no other lesions visible on US images, versus only 6% among those with no calcifications present (p = 0.0001). All the lesions besides calcification, visible on US images, were numerically less frequently present in patients with calcification, but only total rupture (p = 0.001), bursitis (p = 0.004), acromioclavicular lesions (p = 0.045), and other lesions (p = 0.0001) were significantly less frequent.
When analyzing the US imaging results according to the different predefined clinical categories, no additional differences between the two groups were observed. In patients presenting with hyperalgesic shoulder pain, calcification was even less frequently associated with other lesions visible via US than in patients without calcification (8/16 vs. 8/9, p = 0.05). Rotator cuff rupture was also significantly less frequent in all the clinical categories when calcification was present and did not occur significantly more frequently among patients with chronic shoulder pain (1/18) (see Supplementary Table 2).
Multivariate logistic regression analysis showed that even after mutual adjustment, the presence of calcification was associated with female sex (adjusted OR 2.8, 95% CI 1.5 to 5.3), the absence of bursitis (aOR 2.3, 95% CI 1.0 to 5.0), the absence of complete rotator cuff ruptures (aOR 3.8, 95% CI 1.2 to 12.5) and the absence of other lesions such as osteoarthritic fracture (aOR 11.1, 95% CI 2.2 to 50). After adjustment for sex and US features, chronic shoulder was associated with reduced odds of calcification compared to acute shoulder (aOR 0.33, 95% CI 0.14 to 0.78).
When looking at associations between the visual shape of calcification in US images (Figure 1) and clinical symptoms, a significantly higher proportion of soft and cystic calcifications without shadowing was found in patients with hyperalgesic shoulder pain (p = 0.005) compared to chronic shoulder pain (See details in Table: 3).
|
Hyperalgesic shoulder pain n = 16 |
Chronic shoulder pain |
Comparison between groups |
|
|
Side affected |
|||
|
Right, n (%) |
6 (40) |
10 (63) |
p = 0.2 |
|
data available, n |
15 (94) |
16 (89) |
|
|
Location: supraspinatus |
|||
|
Yes, n (%) |
14 (88) |
14 (78) |
p = 0.5 |
|
data available, n |
16 (100) |
18 (100) |
|
|
Size (cm) |
|||
|
mean (SD) |
1.5 (0.7) |
1.2 (0.7) |
p = 0.4 |
|
median [IQR] |
2.0 [1.0] |
1.0 [0.5] |
|
|
data available, n (%) |
11 (69) |
7 (39) |
|
|
US characteristics |
p = 0.06 (all groups) |
||
|
Shape: linear |
p = 0.6 |
||
|
Yes, n (%) |
1 (8) |
2 (22) |
|
|
data available, n |
12 (75) |
9 (50) |
|
|
Shape: arc +/- shadow |
p = 0.3 |
||
|
Yes, n (%) |
2 (17) |
5 (56) |
|
|
data available, n |
12 (75) |
9 (50) |
|
|
Shape: soft or cystic |
P = 0.005 |
||
|
Yes, n (%) |
9 (75) |
2 (22) |
|
|
data available, n |
12 (75) |
9 (50) |
|
|
Statistical tests used: T-test, Mann–Whitney test, and chi-squared test, as appropriate. |
|||
Table 3: Comparison of calcification characteristics visible via US between hyperalgesic and chronic shoulder pain groups.
4. Discussion
The present study confirmed that calcific tendinitis represents around 25% of the lesions visible via US in patients with symptomatic shoulder pains examined during routine daily rheumatology practice [19]. Calcifications were also found when acute as well as chronic symptoms were the reason for referral to the rheumatologist [19, 20]. No demographic factors other than being a woman were clearly associated with the presence of calcification. Acute flare-ups linked to calcification were rare after 60 years old, supporting previous data in the literature showing that acute inflammatory flare-ups related to calcification occurred mostly in young and middle-aged women [6].
More acute symptoms and a shorter delay between symptoms and diagnosis were the only clinical manifestations in our cohort significantly associated with calcifications, confirming that it remains difficult to detect patients with shoulder calcifications based on clinical manifestations alone [21]. Imaging, particularly US imaging, remains necessary for diagnosis. The pathophysiology of calcification is still not well understood, and the relationship between calcifications and other shoulder lesions remains unclear [22]. Among our patients with calcifications, almost half had no other lesions visible in US imaging and all other lesion types were less frequently prevalent. These results support previous data in the literature suggesting that the formation of calcifications is an independent process, mostly due to disorders in the metabolism of the tendon [22] leading to basic crystal phosphate formation and deposit.
The relation between calcific tendinitis and cuff ruptures is also not sell settled. They can have very similar clinical features at presentation and can be seen together in the same patient [3]. Whether or not either might play a role in the etiopathogenesis of the other remains unclear. Two recent, non-surgical, case-control studies of patients with shoulder pain used MRI to look at the frequency of cuff rupture in patients with and without calcific tendinitis and at the relationship between these lesions [7, 23]. Both studies showed fewer complete rotator cuff ruptures in the calcific groups. Moreover, those ruptures were rarely located at the site of the tendons (3% and 4% of cases, respectively). Our study confirmed these observations, with US images showing significantly fewer rotator cuff ruptures in the group with calcification. Our results also suggest that calcific tendinitis does not precede and lead to rotator cuff rupture since we did not find a significantly higher proportion of such ruptures in patients with chronic shoulder pain [24]. Our study design was transversal, however (at rheumatological consultation), and, to the best of our knowledge, no prospective, longitudinal studies have evaluated the long-term clinical and radiographic evolution of calcific tendinitis [25] in non-surgical cohorts. Some post-treatment studies—notably using US-guided percutaneous needling—have nevertheless shown that in most cases, the clinical evolution was favorable after up to ten years of follow-up [8].
As in previous studies, some of the shapes of calcification imaged via US suggested the type of symptoms induced by that calcification [20, 26]. Nodular, soft, homogeneous calcifications without shadowing and heterogeneous cystic calcifications were essentially associated with acute inflammatory symptoms, suggesting that the calcification was already in the process of dissolution. Our study had some limitations. As mentioned above, the study was retrospective and transversal, not longitudinal. Some data were missing, particularly in the descriptions of the lesions imaged via US, some clinical categories only contained a limited number of patients, and we did not analyze either group’s comorbidities in detail, although no specific comorbidities were found in the group with calcification. Finally, the fact that the same rheumatologist, aware of the clinical presentations, performed all the US examinations, might have influenced the US findings.
In conclusion, although some demographic and clinical features were associated with calcifications, it remains difficult to detect patients with shoulder calcifications based on their clinical manifestations alone. US evaluation suggests that calcifications are associated with significantly fewer other lesions, particularly total rupture. Some US calcification patterns were associated with the clinical presentation.
References
- McCarty DJ, Jr, Gatter RA. Recurrent acute inflammation associated with focal apatite crystal deposition. Arthritis Rheum 9 (1966): 804-819.
- Speed CA, Hazleman BL. Calcific tendinitis of the shoulder. N Engl J Med 340 (1999): 1582-1584.
- Louwerens JK, Sierevelt IN, van Hove RP, et al. Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: clinical and radiologic analysis of 1219 patients. J Shoulder Elbow Surg 24 (2015): 1588-1593.
- Darrieutort-Laffite C, Blanchard F, Le Goff B. Calcific tendonitis of the rotator cuff: From formation to resorption. Joint Bone Spine 85 (2018): 687-692.
- Brinkman JC, Zaw TM, Fox MG, et al. Calcific Tendonitis of the Shoulder: Protector or Predictor of Cuff Pathology? A Magnetic Resonance Imaging-Based Study. Arthroscopy 36 (2020): 983-990.
- Louwerens JKG, Alkaduhimi H, van den Bekerom MPJ. Association Between Rotator Cuff Tears and Calcific Tendinopathy. Arthroscopy 36 (2020): 625-626.
- Beckmann NM, Tran MQ, Cai C. Incidence of rotator cuff tears in the setting of calcific tendinopathy on MRI: a case controlled comparison. Skeletal Radiol 48 (2019): 245-250.
- Serafini G, Sconfienza LM, Lacelli F, et al. Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two-needle us-guided percutaneous treatment--nonrandomized controlled trial. Radiology 252 (2009): 157-164.
- Tran G, Cowling P, Smith T, et al. What Imaging-Detected Pathologies Are Associated With Shoulder Symptoms and Their Persistence? A Systematic Literature Review. Arthritis Care Res (Hoboken) 70 (2018): 1169-1184.
- Rosenthal AK. Basic calcium phosphate crystal-associated musculoskeletal syndromes: an update. Curr Opin Rheumatol 30 (2018): 168-172.
- Le Goff B, Berthelot JM, Guillot P, et al. Assessment of calcific tendonitis of rotator cuff by ultrasonography: comparison between symptomatic and asymptomatic shoulders. Joint Bone Spine 77 (2010): 258-263.
- Roy JS, Braen C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med 49 (2015): 1316-1328.
- Chiou HJ, Hung SC, Lin SY, et al. Correlations among mineral components, progressive calcification process and clinical symptoms of calcific tendonitis. Rheumatology (Oxford) 49 (2010): 548-555.
- Allen GM. Shoulder ultrasound imaging-integrating anatomy, biomechanics and disease processes. Eur J Radiol 68 (2008): 137-146.
- van der Heijden GJ. Shoulder disorders: a state-of-the-art review. Baillieres Best Pract Res Clin Rheumatol 13 (1999): 287-309.
- Chiou HJ, Chou YH, Wu JJ, et al. Evaluation of calcific tendonitis of the rotator cuff: role of color Doppler ultrasonography. J Ultrasound Med 21 (2002): 289-295.
- Naredo E, Iagnocco A, Valesini G, et al. Ultrasonographic study of painful shoulder. Ann Rheum Dis 62 (2003): 1026-1027.
- Petranova T, Vlad V, Porta F, et al. Ultrasound of the shoulder. Med Ultrason 14 (2012): 133-140.
- Ottenheijm RP, van't Klooster IG, Starmans LM, et al. Ultrasound-diagnosed disorders in shoulder patients in daily general practice: a retrospective observational study. BMC Fam Pract 15 (2014): 115.
- Sansone V, Maiorano E, Galluzzo A, et al. Calcific tendinopathy of the shoulder: clinical perspectives into the mechanisms, pathogenesis, and treatment. Orthop Res Rev 10 (2018): 63-72.
- Lewis J. Rotator cuff related shoulder pain: Assessment, management and uncertainties. Man Ther 23 (2016): 57-68.
- Darrieutort-Laffite C, Blanchard F, Le Goff B. Calcific tendonitis of the rotator cuff: From formation to resorption. Joint Bone Spine (2017).
- Sucuoglu H, Asan A. Relationship between calcific tendinopathy and rotator cuff tear on shoulder magnetic resonance imaging: case-controlled comparison. Pol J Radiol 85 (2020): e8-e13.
- Yamamoto A, Takagishi K, Kobayashi T, et al. Factors involved in the presence of symptoms associated with rotator cuff tears: a comparison of asymptomatic and symptomatic rotator cuff tears in the general population. J Shoulder Elbow Surg 20 (2011): 1133-1137.
- Tangrood ZJ, Gisselman AS, Sole G, et al. Clinical course of pain and disability in patients with subacromial shoulder pain: a systematic review protocol. BMJ Open 8 (2018): e019393.
- Yang TP, Chiou HL, Maa MC, et al. Mithramycin inhibits human epithelial carcinoma cell proliferation and migration involving downregulation of Eps8 expression. Chem Biol Interact 183 (2010): 181-186.
Supplementary Files
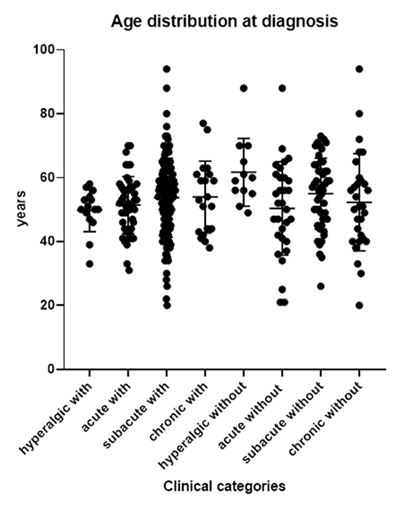
Figure 1: Age distribution of the different clinical categories.
Table 1: Demographic and clinical comparison by diagnosis category and calcification status.
Table 2: Comparison of lesions visible via US by diagnosis category and calcification status.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 