Creating an Inexpensive PVC Knee Model for the Training of Ultrasound-Guided Medial Intra-Articular Knee Injections
Ryland McDermott1*, Joshua Melanson1, Skylar Davidson1, Nora Doyle2
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV
2Roseman University of Health Sciences, Henderson, NV
*Corresponding Author: Ryland McDermott, Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV
Received: 29 March 2023; Accepted: 27 April 2023; Published: 09 May 2023
Article Information
Citation:
Ryland McDermott, Joshua Melanson, Skylar Davidson, Nora Doyle. Creating an Inexpensive PVC Knee Model for the Training of Ultrasound-Guided Medial Intra-Articular Knee Injections. Journal of Orthopedics and Sports Medicine 5 (2023): 207-213.
View / Download Pdf Share at FacebookAbstract
Objectives: Ultrasound (US)-guided injections using corticosteroids or platelet-rich plasma into the knee joint is commonly used for conservative treatment of knee pathology. Practitioner skill acquisition can be challenging due to expensive simulation models and desire to limit practice on live patients. We sought to create an inexpensive, accurate educational prototype for intra-articular knee injections.
Methods: Two Polyvinyl Chloride (PVC) pipes were used for the skeletal infrastructure with a detergent pod placed in between the PVC pipes to replicate the joint space. Layers of undercooked bacon simulated the hyperechoic medial collateral ligament and hypoechoic subcutaneous tissue. The total model cost was $6.88.
Results: Our PVC model simulated anatomical landmarks and was validated through comparison to standardized educational US training videos. The model was successfully recreated 10 times. Furthermore, the PVC model was able to facilitate intra-articular knee injections by penetrating through the superficial structures of the model and injecting into the detergent pod. The model was used to facilitate injections under US guidance with 24 different medical student practitioners across 4 different educational sessions. We further validated our model with US experts.
Conclusions: Our knee model was successful in replicating medial, intra-articular knee injections under US guidance. It provided accurate injection practice as it simulated realistic bony landmarks and soft tissue. Because our model is inexpensive and easy to make, many more learners in the medical field can now safely and easily practice this procedure.
Keywords
<p>PVC model; Ultrasound guidance; Knee injections; Ultrasound education; Simulation</p>
Article Details
List of Abbreviations:
US: Ultrasound; PVC: Polyvinyl Chloride; UGI: Ultrasound-Guided Injections
1. Introduction
The knee joint is a critical weight-bearing joint that is also the largest articulating surface in the human body. Approximately 25 percent of adults will develop chronic knee joint pain at some point in their lifetime [1]. Chronic knee pain stems from a wide variety of inflammatory and degenerative causes and is associated with decreased quality of life. Not surprisingly, patients frequently seek medical attention to relieve their knee pain. Traditionally surgical interventions were the first line for knee joint issues; however, more conservative therapies have gained popularity. Ample research exists to support a trial of conservative measures prior to surgical intervention [2,3]. Intra-articular steroid injections have been reported to provide significant patient benefits by decreasing knee pain with minimal side effects as compared to surgery [4-6].
Historically, intra-articular knee injections were guided by a “feel” for anatomical landmarks that could be easily seen or palpated. With the recent technological US advancements allowing for more readily accessible, user-friendly devices with high quality imaging, Ultrasound-Guided Injections (UGI) have become the norm [7]. Studies support UGI is superior to landmark-based injections as real time images offer superior target location and accurate injection [8]. A 2021 meta-analysis comparing UGI to a blind approach found that UGI had an accuracy of >95% with all anatomical approaches while the blind injections precision ranged from 77.3% to 95.74%.8 Moreover, UGI provide a correct and cost-efficient method for injections [9-12].
Proficiency with UGI requires significant training. Rather than relying on the bedside training axiom “see one, do one, teach one,” learning through simulation has been shown to be both safer and more effective. However, teaching US guided injections into the knee joint comes with challenges of cadaver availability and model expense. Low-cost, easy to get mockups for US procedures have previously been reported [13-17]. Our aim is to create an inexpensive and accessible educational model that demonstrates the anatomical and procedural accuracy of an intra-articular knee injection through the medial approach under US guidance. Additionally, we sought to make trainees more comfortable using US-guided knee injection procedures.
2. Methods and Materials
2.1 Materials
Using PVC pipe and electric tape purchased at a national chain hardware store, coupled with bacon strips, rubber bands and detergent pods from the supermarket, we constructed a medial knee joint. Table 1 details the cost of each product and total model:
|
Material |
Amount |
Cost ($) |
|
PVC Pipe 1” × 24” |
1 |
1.65/pipe |
|
Detergent pod |
1 |
0.31/pod |
|
Uncooked bacon strips |
2 |
0.64/strip |
|
Rubber bands |
1 |
0.99/package |
|
5 mL Disposable syringe with a 1.5” 25 Ga needle |
1 |
0.65/syringe |
|
Electrical tape |
1 |
2.00/roll |
|
Total cost of the model |
6.88 |
Table 1: Materials used to assemble the medial knee model.
The materials were chosen specifically to best represent anatomical landmarks:
- PVC pipes: distal femur and proximal tibia
- Detergent pod: medial meniscus and synovial space
- Bacon strips: medial collateral ligament and subcutaneous tissue
- Rubber bands: insertion of medial collateral ligament to respective bones
The pipe was cut into multiple 1” × 6” pieces, which was a desired length to improve the maneuverability of the knee model. If options to cut the PVC pipe are unavailable, 2 PVC pipes can be bought and used instead.
2.2 Medial Knee Model Construction
Two cut 1” × 6” PVC pipes were laid out in a line with a space in between. The ends of the two PVC pipes represent the femur medial epicondyle and tibia medial condyle respectively. Glue was applied around the ends of the detergent pod to secure it in the desired position as needed. The detergent pod was then placed halfway into the lumens of both PVC pipes to represent the medial meniscus and synovial space. The two PVC pipes with the detergent pod in between them were bent 10 degrees to demonstrate slight knee flexion, which imitates the desired positioning for our medial knee injection. Electrical tape was used on the inferior lateral sides of the knee model to increase stability.
Once the PVC pipe and detergent pod model is in slight flexion, two strips of bacon are placed on one of the sides of the model, which will be deemed the medial side. The strips of bacon are folded in half and stacked on top of each other. Two rubber bands are used to fasten the bacon to the model. One band is wrapped around each end of the bacon and its respective PVC pipe. The model is then checked for stability and glue is applied as needed if any parts of the model are loose. Figure 1-3 displays examples of how to assemble the model:
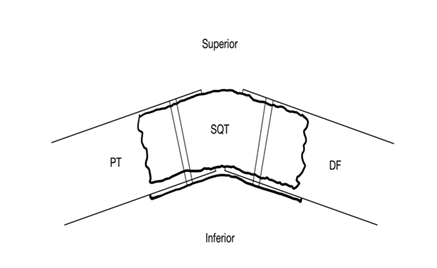
Figure 1: Sketch of a horizontal view of the medial knee model. Subcutaneous tissue (SQ), medial femoral condyle (DF, “distal femur”), proximal tibia “plateau” (PT).
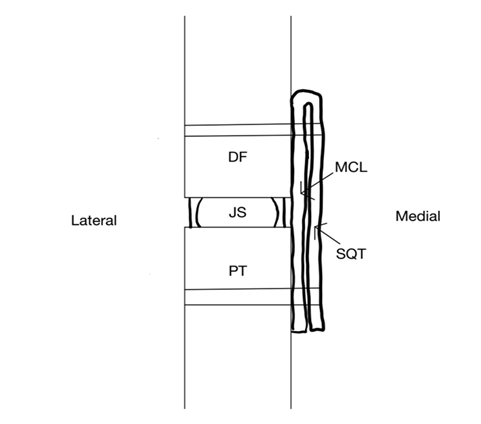
Figure 2: Sketch of a superior view of the medial knee model. Subcutaneous Tissue (SQ), Medial Collateral Ligament (MCL), medial femoral condyle (DF, “distal femur”), Joint Space (JS), Proximal Tibia “Plateau” (PT).

Figure 3: Superior view of the PVC medial knee model.
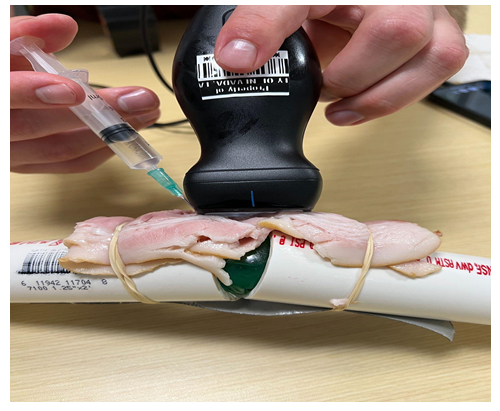
Figure 4: US-guided medial knee injection of the PVC knee model.
2.3 Procedure: Ultrasound-Guided Medial Knee Injection
Once the model was assembled, either a handheld US probe (Butterfly IQ) or a portable US probe (Mindray TE7) was obtained. The US probe was placed longitudinally with the probe’s notch pointing towards the top of the model. The representative anatomic structures were visualized under US, and a 25-gauge needle with 5 cc of room-temperature tap water was obtained. The needle was injected into the model adjacent to the US probe’s notch, and then the needle was located under US guidance. Tilting and sliding of the US probe were done as needed to achieve the ideal needle visualization. The needle was then advanced in between the PVC pipes and into the detergent pod. Once the needle was in the desired position, the 5 cc of solution was administered into the detergent pod to stimulate a medial knee injection. The injection procedure was observed under US guidance to ensure proper injection location throughout the duration of the procedure. Figure 4 demonstrates performing the injection:
3. Results
The PVC model was successfully assembled and recreated 10 times. Furthermore, the model was able to facilitate intra-articular knee injections by penetrating through the superficial structures of the model and injecting into the detergent pod. This model and injection procedure were further validated with US experts and sports medicine physicians as well as through comparison to standardized educational US training videos. The model was utilized at 4 different educational US workshops, where 24 medical students used it to practice UGIs. The materials used are shown in Table 1. The appearance of the model under sonography is shown with its representative structures labeled in Figure 5, and the medial knee injection under US-guidance is displayed in Figure 6:
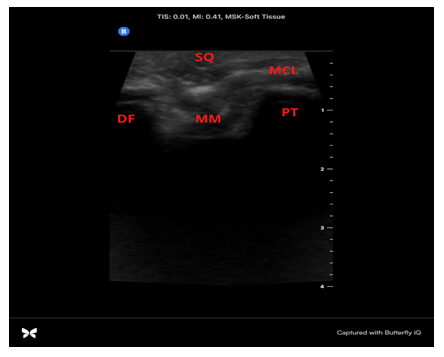
Figure 5: US image of the PVC medial knee model’s anatomical structures using a handheld US probe (Butterfly IQ). Subcutaneous tissue (SQ), medial collateral ligament (MCL), medial femoral condyle (DF, “distal femur”), medial meniscus (MM), proximal tibia “plateau” (PT).
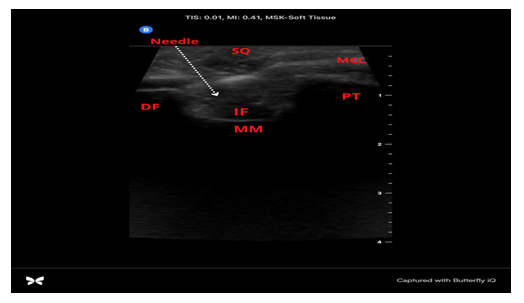
Figure 6: US image of US-guided injection into the PVC medial knee model using a handheld US probe (Butterfly IQ). 1.5-inch 25 Gauge Needle (Needle), Injected Fluid (IF), Subcutaneous Tissue (SQ), Medial Collateral Ligament (MCL), Medial Femoral Condyle (DF, “distal femur”), Medial Meniscus (MM), Proximal Tibia “plateau” (PT).
4. Discussion
The knee is one of the largest and most complex joints in the body. A variety of reasons including trauma, arthritis, and every day wear and tear result in knee joint injuries being one of the most common reasons to see an orthopedic physician.1 In fact, a study found the prevalence of total knee replacements in one calendar year in the US came out to be 4.7 million [18]. Recently non-surgical treatments such as cortisone injections, hyaluronic injections, or PRP (platelet-rich plasma) injections have been shown to both delay and prevent the need for knee surgery. This is especially helpful for patients who are not surgical candidates [19]. These office-based procedures are well-tolerated and cost effective [9-12].
Barriers to training practitioners in non-surgical US injection therapies include cadaver access and cost prohibitive simulation models [20]. For example, popular existing knee US models can cost up to $4,000 or more. This was our inspiration for designing a low-cost, easily reproducible simulation model using materials from the grocery and hardware stores. Although expensive knee models can also be a great tool for training, our model is easy to assemble and costs less than $7.00 [21]. We have shown our simulation US images create normal anatomical US images and excellent simulation training. Model building was simple and did not require additional tools or space. The entire process took the authors 5 – 10 minutes once materials were assembled. The non-perishable parts of the model can be stored and reused for future training sessions. Our model design allows for other users to customize the building process or materials based on their needs or accessible resources.
When creating any simulation model, it is important to provide a learning experience that accurately represents the true clinical situation. A model that facilitates UGIs should allow the user to appreciate anatomic structures, the needle, an articular space to inject into, and materials that replicate the feel of an actual knee. Our model accomplishes all these goals [22]. When using our model, the user is able to visualize a joint space and articulate bones because of the use of PVC pipe which provides a similar echogenicity to that of bone. The marbling of the bacon provided variable echogenicity to simulate skin and subcutaneous tissue as well as provide striations that would be seen in normal anatomy. Additionally, using a detergent pod as the joint space provides a target for injections which can be removed to assess accuracy post-injection [23].
As with any experiment, we encountered limitations. Our PVC knee joint model focused primarily on a medial approach of the knee joint and thus all other approaches were not included. The model also lacked external anatomy to visually represent the knee joint [24]. External anatomy could aid in estimating the injection site as well as provide a more thorough simulation of the actual clinical experience. Additionally, while inexpensive, the meat product and detergent pod used in the model are perishable and should be replaced as needed.
5. Conclusion
We have developed an inexpensive and easily reproducible model which facilitates US structure visualization and US-guided needle injections of the medial aspect of a knee joint. The materials used provided an accurate representation of soft tissue and bony landmarks that practitioners will encounter when doing medial knee injections. We did not find other inexpensive knee joint models reported, which speaks to the novelty of our model in terms of US visualization and guidance of medial knee injections. We hope our report contributes to making US training more accessible and effective for other clinicians. This model can be incorporated into both undergraduate and graduate medical education to further assess its capacity as a learning tool. Further studies are needed to create an inexpensive and easily reproducible total knee model that has the capacity for multiple injection approaches such as suprapatellar and anterolateral approaches.
Declarations
Ethics approval and consent to participate:
Not applicable
Consent for publication:
Not applicable
Availability of data and materials:
All data generated during this study are included in this published article.
Competing interests:
The authors declare that they have no competing interests.
Funding:
The authors declare that they have no sources of funding for this project.
Authors’ Contributions:
RM created the study design, built the model, and wrote the manuscript. JM created the study design, built the model, and wrote the manuscript. SD created the study design, built the model, and wrote the manuscript. ND created the study design. All authors also read, revised, and approved the final manuscript.
Acknowledgements:
Not applicable.
Disclaimer
This study was performed at Kirk Kerkorian School of Medicine at UNLV and did not require IRB approval.
Acknowledgements
The authors have no acknowledgments for this study.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
References
- Nguyen U, Zhang Y, Zhu Y, et al. Increasing Prevalence of Knee Pain and Symptomatic Knee Osteoarthritis: Survey and Cohort Data. Annals of Internal Medicine 155 (2011): 725-732.
- Kise NJ, Risberg MA, Stensrud S, et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomized controlled trial with two year follow-up. BMJ 354 (2016): i3740.
- Giuffrida A, Di Bari A, Falzone E, et al. Conservative vs. surgical approach for degenerative meniscal injuries: a systematic review of clinical evidence. Eur Rev Med Pharmacol Sci 24 (2020): 2874-2885.
- Wilderman I, Berkovich R, Meaney C, et al. Meniscus Targeted Injections for Chronic Knee Pain Due to Meniscal Tears or Degenerative Fraying: A Retrospective Study. Journal of Ultrasound in Medicine 38 (2019): 2853-2859.
- Byrne C, Alkhayat A, Bowden D, et al. Degenerative tears of the posterior horn of the medial meniscus: correlation between MRI findings and outcome following intra-articular steroid/bupivacaine injection of the knee. Clin Radiol 74 (2019;): 488.e1-488.e8.
- Vermesan D, Prejbeanu R, Laitin S, et al. Arthroscopic debridement compared to intra-articular steroids in treating degenerative medial meniscal tears. Eur Rev Med Pharmacol Sci 17 (2013): 3192-3196.
- Wilson DJ, Scully WF, Rawlings JM. Evolving Role of Ultrasound in Therapeutic Injections of the Upper Extremity. Orthopedics 38 (2015): e1017-e1024.
- Fang WH, Chen XT, Vangsness CT Jr. Ultrasound-Guided Knee Injections are More Accurate than Blind Injections: A Systematic Review of Randomized Controlled Trials. Arthrosc Sports Med Rehabil 3 (2021): e1177-e1187.
- Berkoff DJ, Miller LE, Block JE. Clinical utility of ultrasound guidance for intra-articular knee injections: a review. Clin Interv Aging 7 (2012): 89-95.
- Curtiss HM, Finnoff JT, Peck E, et al. Accuracy of ultrasound-guided and palpation-guided knee injections by an experienced and less-experienced injector using a superolateral approach: a cadaveric study. PM R 3 (2011): 507-515.
- Mortazavi SJ, Nabian MH. Point-of-Care Ultrasonography in Orthopedics: A Helpful Tool to Improve Patient Care. Arch Bone Jt Surg 8 (2020): 323-324.
- Cunnington J, Marshall N, Hide G, et al. A randomized, double-blind, controlled study of ultrasound-guided corticosteroid injection into the joint of patients with inflammatory arthritis. Arthritis Rheum 62 (2010): 1862-1869.
- Naraghi L, Lin J, Odashima K, et al. Ultrasound-guided regional anesthesia simulation: use of meat glue in inexpensive and realistic nerve block models. BMC Medical Education 19 (2019): 145-145.
- Risler Z, Magee MA, Mazza JM, et al. A Three-dimensional Printed Low-cost Anterior Shoulder Dislocation Model for Ultrasound-guided Injection Training. Cureus 10 (2018): e3536-e3536.
- Sullivan A, Khait L, Favot M. A Novel Low-Cost Ultrasound-Guided Pericardiocentesis Simulation Model: Demonstration of Feasibility. J Ultrasound Med 37 (2018): 493-500.
- Shin KC, Ha YR, Lee SJ, et al. Review of simulation model for education of point-of-care ultrasound using easy-to-make tools. World J Clin Cases 8 (2020): 4286-4302.
- Samuel J, Kerr E, Young D, et al. The use of joints of meat as phantoms for ultrasound-guided needling skills: a prospective blinded study. Ultrasound J 14 (2022): 14.
- Maradit KH, Larson DR, Crowson CS, et al. Prevalence of Total Hip and Knee Replacement in the United States. J Bone Joint Surg Am 97 (2015): 1386-1397.
- Bose S, Talmor D. Who is a high-risk surgical patient? Curr Opin Crit Care 24 (2018): 547-553.
- Peck E, Lai JK, Pawlina W, et al. Accuracy of ultrasound-guided versus palpation-guided acromioclavicular joint injections: a cadaveric study. PM R 2 (2010): 817-821.
- Wisniewski SJ, Smith J, Patterson DG, et al. Ultrasound-guided versus non-guided tibiotalar joint and sinus tarsi injections: a cadaveric study. PM R 2 (2010): 277-281.
- Smith J, Brault JS, Rizzo M, et al. Accuracy of sonographically guided and palpation guided scaphotrapeziotrapezoid joint injections. J Ultrasound Med 30 (2011): 1509-1515.
- Liu Y, Glass NL, Glover CD, et al. Comparison of the development of performance skills in ultrasound-guided regional anesthesia simulations with different phantom models. Simul Healthc 8 (2013): 368-375.
- Kim TE, Tsui BCH. Simulation-based ultrasound-guided regional anesthesia curriculum for anesthesiology residents. Korean J Anesthesiol 72 (2019): 13-23.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 