Distribution Pattern of Community Pharmacies in Port Harcourt Metropolis, Niger Delta, Nigeria
Ifeyinwa Chijioke-Nwauche1*, Mark Ogoro2
1Department of Clinical Pharmacy and Management, Faculty of Pharmaceutical Sciences, University of Port Harcourt, Port Harcourt, Nigeria
2Department of Geography and Regional Planning, University of Port Harcourt, Port Harcourt, Nigeria
*Corresponding Author: Ifeyinwa Chijioke-Nwauche, Department of Clinical Pharmacy and Management, Faculty of Pharmaceutical Sciences, University of Port Harcourt, Port Harcourt, Nigeria
Received: 04 March 2021; Accepted: 20 March 2020; Published: 23 March 2021
Article Information
Citation: Ifeyinwa Chijioke-Nwauche, Mark Ogoro. Distribution Pattern of Community Pharmacies in Port Harcourt Metropolis, Niger Delta, Nigeria. Journal of Pharmacy and Pharmacology Research 5 (2021): 188-199.
View / Download Pdf Share at FacebookAbstract
Background: The primary importance to every society is tied to her citizen’s ability to access good healthcare services at a reasonable reach. Community pharmacies often serve as the first point of contact for persons in need of health services and therefore are the most accessible suitable platforms for accessing of healthcare services.
Aim: The study aimed at examining the distribution pattern and accessibility of community pharmacies in Port Harcourt metropolis to the populace.
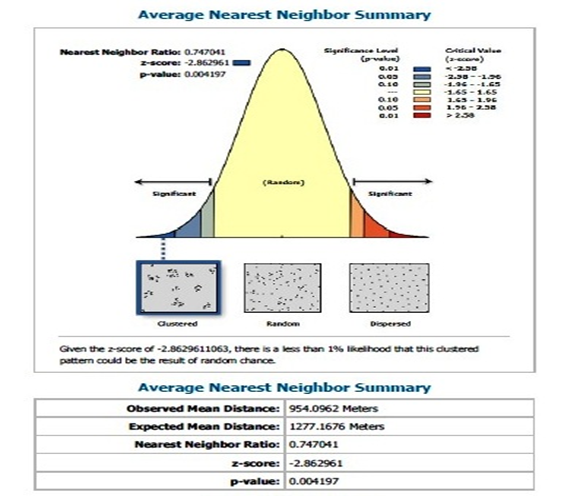
Materials and methods: High resolution Google Earth Image, Geographic Information System as well as the Global Positioning System were employed in data collection. The overlaying and buffering analysis were employed to examine the Geo-location and the compliance of pharmacies to stipulated regulation respectively. The nearest neighbour analysis tools in the spatial analysis extension of the ArcGIS 10.4 version were used to determine the spatial pattern of pharmacies across the study area.
Results: Finding revealed that, pharmacies were clustered in the heart of the metropolis (urban centers) with focus on areas of higher financial or monetary/purchasing capacity (population) and an average opening corridor of 12hours between the hours of 8am and 11 pm maximum.
Conclusion: To ensure better distribution of pharmacies and ensure comprehensive healthcare coverage, emphasis should be paid on Geo-location in the approval of operating licenses, accommodating attributes such as financial strength, age and other vulnerability of residents.
Keywords
<p>Community pharmacies; Accessibility; Distribution; Healthcare services; Port Harcourt Metropolis</p>
Article Details
Introduction
Access to healthcare which consists of coverage, services, timeliness and workforce is of primary importance to every society [1]. The institute of Medicine defines Access to healthcare as the timely use of personal health services to achieve the best health outcomes [2]. The ability to access good health services by those who need them within a reasonable reach and at conducive opening hours as well as delivery of these services when needed according to World Health Organization is termed physical accessibility [3].
According to the International Federation of Pharmacists, community pharmacy practice is the area of pharmacy practice that involves the sale of or provision of medicines and other related products to the public from a retail or commercial outlet primarily for the purpose of providing medicines [4]. It is the healthcare facility that provides pharmaceutical services to a specific community or region [5]. Pharmaceutical services are among healthcare services which have been shown to be influenced by geographic access [6]. Community pharmacists are the most accessible and widely distributed health professionals to the public and are the cornerstone of primary healthcare. This accessibility makes the community pharmacies to fit into the main goals of WHO agenda to form accessible multidisciplinary network of public health professionals. They provide personalized services, counselling and advices without prior appointments therefore community pharmacies usually serve as the first point of call for patients [7]. Their roles range from the traditional role of dispensing of prescription and non-prescription medicines to counselling, provision of effective medicine, drug information to the general public and patients that encourage quality use of medicines as well as different aspects of self-care and health promotions [8-10].
The long hours of opening which sometimes may be late into the evenings or at weekends when other healthcare workers are not available provide a convenient and less formal environment for those who cannot easily access or do not choose to access other kinds of health service. Location of community pharmacies in the heart of the community provides an avenue that is contributory to health promotion and a variety of preventive practices [11]. In England, about 1.6 million people visit a pharmacy daily [12]. Patronage of community pharmacies is very common among many Nigerians especially in seeking advice for self-care, minor ailments and treatment of common conditions such as malaria and common cold [13,14].
Accessibility which is the most important characteristic of community pharmacists is tied to its distribution. Considering this essential need of provision of these health services to every community, it is of vital importance that there be proper distribution of community pharmacies, such that there will be adequate provision of pharmaceutical services to every community. Unbalanced distribution of pharmacies with respect to population distribution would severely limit the accessibility of the populace to pharmaceutical services. Such observed limitation of services impose additional costs and inconveniences on individuals most in need of medical care and who may not be able to access healthcare beyond their immediate environment due to financial constraints or limitation of other social amenities.
Easy availability and access to a community pharmacy means that it is often the first point of contact for people in need of advice or information about medical or health care [15]. The setting in community pharmacies offers additional benefits of informal environment as well as flexibility and anonymity which are very valuable to the people. Distribution of community pharmacies has not been adequately studied in Nigeria, therefore there is a paucity of data on the subject. Pharmacy location in Port Harcourt metropolis is determined to a great extent by the decisions of individual pharmacist in response to demand for medicines, other health services and retail goods. This study sought to unveil the distribution pattern of community pharmacies across Port Harcourt metropolis and to assess their accessibility by residents. The study therefore aims to analyze the spatial location of community pharmacies using Geographic Information Systems (GIS) and providing information about their accessibility as an important tool for connections between health and the host community/environment. Additional attempt was made to establish a relationship between distribution and economic status of the populace as well as distribution and population density. The results will show the spatial pattern of community pharmacies distribution across the study area.
Materials and Method
Study area: Location and extent
The study area was limited to Port Harcourt metropolis and the design consisted of a cross-sectional observational study comprising of community pharmacies located within the metropolis. The study utilized high-resolution Google earth images to enable the delineation of the urban and its periphery extent of the study area. The information processing and digital and graphic modeling were performed by the Geographic Information System (GIS) in the ArcGIS 10.4 platform. The images and base maps were geo-referenced and digitized in the ArcGIS environment to ensure proper overlaying and analysis. The feature classes required for the analysis were digitized into their separate layers and shape files were created. The Global Position System (GPS) enabled the retrieval of the global position of all registered pharmacies to examine their locational attributes and randomness of the pharmacies across the study area. The buffering analytical tool was used in the GIS environment to identify pharmacies that are beyond 200 meters from another.
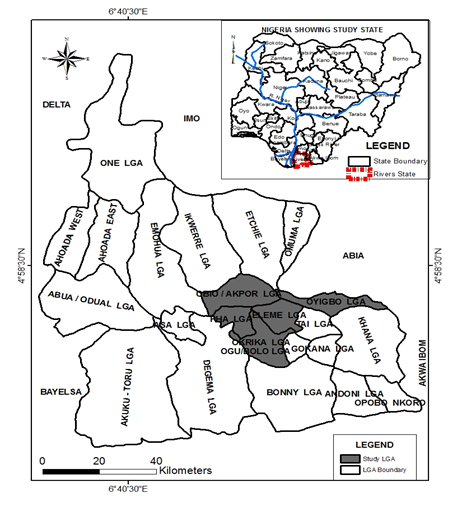
Study was carried out in Port Harcourt Metropolis. Port Harcourt has an estimated population of 1,759,739 as at 2006 [16] and as the time of the study (2018), the projected population was 2,596,000. Metropolis of Port Harcourt is positioned from Latitude 4045'N through Latitude 40 55' N, and Longitude 60 55' E through Longitude 7005' E as shown in Figure 1. The Atlantic Ocean is found at an approximate distance of 25km from it. The five local governments which the metropolis extends into are the Obio-Akpor, Eleme, Oyigbo, Okrika,and Port Harcourt local government areas (Figure 1).
Community pharmacies in Port Harcourt metropolis are grouped into 13 Zones with each zone consisting of about 8-34 Pharmacies [14]. As at the time of the study, there were about 362 community pharmacies. Using Taro Yamane sampling frame (1967; 1973), a sample size of 189 was calculated as the minimum number of pharmacies to be sampled. From each zone, convenient sampling was done to obtain the calculated sample size of pharmacies. However, a total of 219 community pharmacies sampled represents more than half of the total community pharmacies within the study area. The study was carried out in October, 2018.
The data sources for this study were primary and secondary sources using the Global Positioning System to extract the coordinate of the pharmacies across the study area. Google imagery was used to delineate the base map where the community pharmacy location was overlaid. The distribution pattern of Community Pharmacies across the study area was analyzed using the nearest neighbor analytical tool which was used to examine the location of community pharmacies and determine the pattern of these locations whether they are clustered, random or dispersed across the study area. Also the relationship of distribution with respect to population density and poverty using Alpha version 2010, 2015 and 2020 estimates of numbers of people per pixel (ppp) and people per hectare (pph) square, with national totals adjusted to match UN population division estimates were also evaluated and analysed [17].
Results
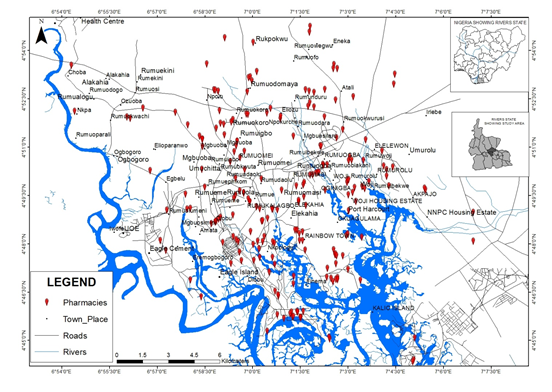
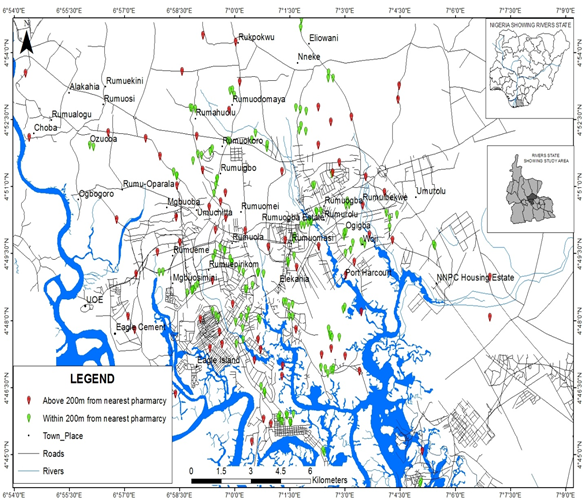
Out of the 367 community pharmacies present in Port Harcourt Metropolis as at the time of study, we captured 219 based on the minimum calculated sample of 189. The map shows the distribution pattern of community pharmacies within the study area (Figure 2). Observation shows the pharmacies are concentrated in the heart of the metropolis which is the center of urban development and human activities. The average opening hours for most of the pharmacies are 12hours usually between the hours of 8 am to 10 pm. However, a few of the pharmacies are open as late as 11 pm.
The result obtained shows that the spatial location of pharmacies in Port Harcourt Metropolis is clustered and located within developed neighborhood of the city or where persons of higher financial capacity reside (Figure 2).
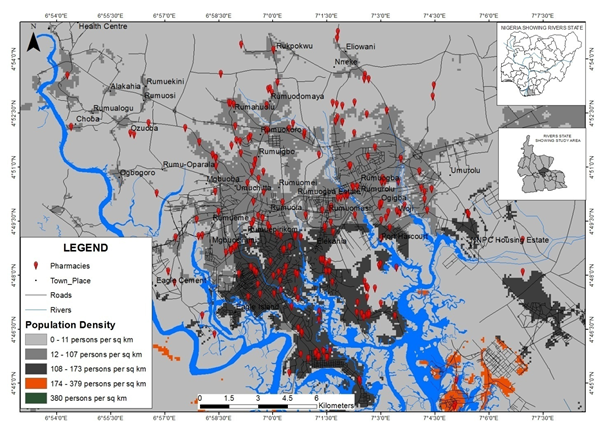
Analyzing the result in reference to population density, Figure 3 shows the population of the study area in raster form and the overlay of the location of registered pharmacies enumerated for the study. From the overlay analysis, the locational decisions of pharmacies were based largely on the availability of purchasing population/strength hence, the concentration of pharmacies in areas with higher population per square kilometers. Areas with 12 to 107 and 108 to 173 persons per square kilometers host most of the pharmacies leaving only very few located in areas of 0 to 11 persons per square kilometers.
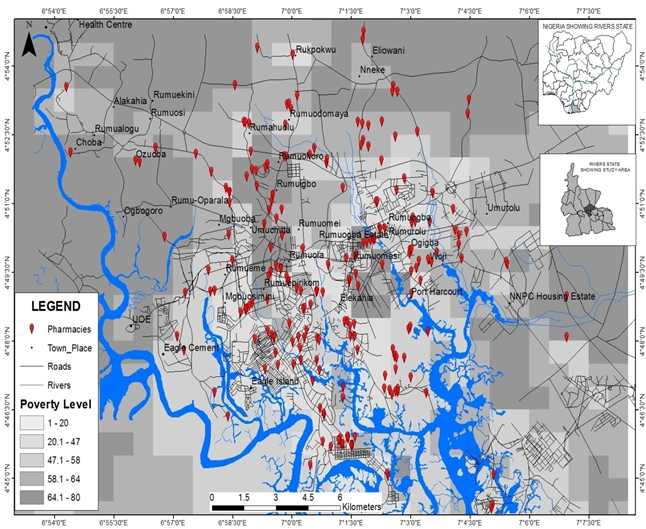
Understanding the underlying factors favoring the location of pharmacies in the study area, revealed that, areas with less than 20 percent of the population living below poverty line based on UN population division estimate, [17] favored the location of pharmacies as compared to areas of 47.1 to 80 percent of the populations living below poverty line as shown in Figure 4. From the analysis, concentrations of dense population do encourage the location of pharmacies in addition to the financial strength of the population as shown in Figure 4. This reveals that, areas with higher per capita income host more pharmacies compared to areas with population of low per capita income.
Average distance obtained between one pharmacy to the nearest neighboring pharmacy was also determined and the result is shown in Figure 5.
Figure 5 was derived from the analysis of pharmacy location across the study area. The analysis revealed that the spatial location of pharmacies is clustered with an observed main distance of 954.0962m (0.9km) between two pharmacies.
Discussion
Community pharmacy according to Kelling [18] should be highly accessible and managed by professionals that can be trusted by patients. The distribution of pharmacies is a very important determinant of access to medicines and health care services, and as stated earlier geographic access is an important influencing factor to healthcare services [6]. In Ontario, about 63.6% of residents live within a walking distance or enjoy a walking distance to pharmacy while 84.6% and 90.7% reside within 2km or 5km driving distance [19]. Hence pharmacies in Ontario were described as geographically accessible to the majority of the population.
A 2018 study shows a record of 3,768 registered community pharmacies in Nigeria with Rivers State being on the eight position in the scale of number of pharmacies [20]. Port Harcourt is the capital of Rivers State and has 367 registered community pharmacies as at the time of the study metropolis [21]. The present study was able to present distribution pattern of 221 community pharmacies. Poor accessibility to pharmacies by residents in the community implies poor access to medicines since pharmacies are first place of call for most people hence it serves a primary care arm.
Results of the study showed a concentration of the pharmacies to be mostly in the urban areas. This is in consonance with an earlier study that demonstrated a skewed distribution of pharmacies in favour of urban areas [21]. A similar pattern was shown in the Canadian where a higher concentration of community pharmacies are in urban areas of Ontario especially in areas zoned for commercial activity [19]. The implication of this is that persons residing in semi-urban or rural areas were more likely to have less access to community pharmacies and thereby less access to pharmaceutical and healthcare services. In the United States of America, residents that dwell in rural areas are faced with the challenge of poor quality roads and lack of public transportation and have to travel farther to access care in comparison to the urban dwellers [22].
This distribution of pharmacies in Port Harcourt metropolis as observed from the study emphasizes location of pharmacies in the heart of the areas of dense population thereby undermining the periphery where development is yet to be pronounced. This trend of pharmacy location will increase the distance that can be walked by the population to the nearest pharmacy in the periphery areas of the study.
Another factor that influences location of pharmacies observed from the study is the per capita income of the persons. This was shown in Figure 4 where areas with higher per capita income host more pharmacies compared to areas of with population of low per capita income.
Community pharmacies provide platforms for health promotion, preventive practices, provide medicines, healthcare products and services and assist the public to make optimal use of them. They also serve as linkage to other healthcare professionals in ensuring optimized patient outcomes in health delivery [23]. Therefore, in areas of shortage or reduced number of community pharmacies, or where there is a long distance to access community pharmacies, these services will be lacking. This was confirmed by a New Zealand study that established that patients farther from pharmacies were less likely to use their services [24]. In order to improve location of pharmacies in rural or sub-urban areas, incentives to attract pharmacists to these areas such as access to electricity, good roads and water supply should be put in place.
The average distance of 954.0962m (0.9km) between pharmacies as obtained from the study, falls within the regulations of the Pharmaceutical Council of Nigeria which prescribes that pharmaceutical premises shall be sited not less than 200m from each other [25]. From the study 138 of the pharmacies were sited within the 200m mark while 81 pharmacies were sited at more than 200m distance from the next pharmacy. This implies that less than 50% of the pharmacies in the present study were sited at more than 200m apart. This was demonstrated via the buffering analysis as depicted in Figure 6 with the red symbol identifying those pharmacies sited beyond 200m totaling 81 pharmacies and the green light showing those sited within the 200m land mark and totaled 138 Pharmacies.
Conclusion
The study has shown that the spatial distribution of community pharmacies within the study area is not uniformly or evenly distributed but is concentrated within the urban areas of the metropolis as well as in areas of higher population density. This distribution pattern makes them inaccessible to residents of the sub-urban or rural areas where few pharmacies or none at all are located. It has also shown that community pharmacies are more distributed in areas with less than 20% of population dwelling below poverty level when compared with the area with about 47.1 to 80% living below poverty line. To ensure better distribution of pharmacies and comprehensive healthcare coverage, emphasis should be paid on Geo-location in the approval of operating licenses, accommodating attributes such as financial strength, age and other vulnerability of residents.
Acknowledgements
The authors wish to acknowledge Sonia Jacobs and Ukpong Lizzy Austeen for the level of participation in data collection. Thanks also go to Amanoritsewo Omatosan Jochebed and Onyeanusi Obianuju Divine for their level of participation in the data analysis.
References
- Healthy People. Access to Health Services. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health (2020). Available at: http://www.healthypeople.gov/2020/topics-objectives/topic/Access-to- Health-Services. Accessed January, 2021.
- Institute of Medicine, Board of Health Care Services. Future directions for the National Healthcare Quality and Disparities Reports. Washington, DC: National Academies Press; 2010. https://www.ncbi.nlm.nih.gov/books/NBK220161/. Accessed February, 2021.
- World health Organization (WHO). Universal Health Coverage and Universal Access, Bulletin of the World Health Organization (2013); 91:546-546A. Available at https://www.who.int/gender-equity-rights/understanding/accessibility-definition/en/. Accessed, February, 2021.
- International Pharmaceutical Federation (FIP). Good Pharmacy Practice (GPP) in developing Countries: Recommendations for stepwise implementations. (1998).
- Smith, Y. Community Pharmacy. News-Medical, 2019. Retrieved on March 02, 2021 from https://www.news-medical.net/health/Community-Pharmacy.aspx.
- Arcury TA, Gesler WM, Preisser JS, et al. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Services Research 40 (2005): 135-156.
- World Health Organization (WHO). The legal and regulatory framework for community pharmacies in the WHO European Region, 2019. Available at https://apps.who.int/iris/bitstream/handle/10665/326394/9789289054249-eng.pdf?sequence=1&isAllowed=y. Accessed January, 2021.
- World Health Organization (WHO): The role of pharmacist in healthcare systems (1994).
- Ogbonna BO, Ejim CE, Ikebudu CC, et al. Pharmaceutical Care and Community Pharmacy Practice In Nigeria; Grappling With the Frontier. European Journal of Pharmaceutical and Medical Research (EJPMR) 2 (2015): 33-42.
- Spears T. Community Pharmacists Play Key Role in Improving Medication Safety: As trusted community health advisors, pharmacists can promote the safe use of medications and improve clinical outcomes. Pharmacy Times 76 (2010): 64.
- Chua SS, Ramachandran CD, Paraidathathu TT. Response of community pharmacists to the presentation of back pain: a simulated patient study. International Journal of Pharmacy Practice 14 (2006): 171-178.
- Pharmaceutical Services Negotiating Committee (PSNC). About community pharmacies. Available at https://psnc.org.uk/psncs-work/about-community-pharmacy/. Accessed March, 2021.
- Annual Malaria Control Programme Review: Ethiopian and Nigeria. 2012. The Carter Centre, Atlanta Georgia.
- Chijioke-Nwauche IN, Sam-Ozini P. Malaria prevalence and health-seeking behaviour in two Niger Delta communities. Sch. Acad. J Pharm 6 (2017): 191-196.
- Cunningham-Burley S. Rediscovering the role of the pharmacist. The Journal of the Royal College of General Practitioners 38 (1988): 99.
- National Bureau of Statistics Federal Republic of Nigeria, Annual Abstract of Statistics (2010).
- Alpha version 2010, 2015 and 2020 estimates of numbers of people per pixel (ppp) and people per hectare (pph) square, with national totals adjusted to match UN population division estimates. Nigeria: Population per 100 meters grid Cell Retrieved 20th January, 2018, from GeoData Institute, University of Southampton (2017).
- Kelling SE. Exploring accessibility of community pharmacy services. Innovations in Pharmacy 6 (2015).
- Law MR, Dijkstra A, Douillard JA, et al. Geographic accessibility of community pharmacies in Ontario. Healthcare Policy 6 (2011): 36.
- Ekpenyong A, Udoh A, Kpokiri E, et al. An analysis of pharmacy workforce capacity in Nigeria. Journal of Pharmaceutical Policy and Practice 11 (2018): 20.
- Oseni Y, Oseni YO. Pharmacists’ distribution in Nigeria; implication in the provision of safe medicines and pharmaceutical care. International Journal of Pharmacy and Pharmaceutical Sciences 9 (2017): 7-10.
- Ricketts TC. ‘‘Preface.’’ In Rural Health in the United States. Oxford University Press, New York (1999): pp vii–viii.
- Okoro RN. Comparative Analysis of Private Retail Community Pharmacies’ Participation in the National Health Insurance Scheme of Nigeria and Ghana: Implications for Access to Essential Medicines. Ethiopian Journal of Health Sciences 29 (2019).
- Hiscock R, Pearce J, Blakely T, et al. Is neighborhood access to health care provision associated with individual-level utilization and satisfaction?. Health Services Research 43 (2008): 2183-2200.
- Pharmacists Council of Nigeria. Procedures for the registration of Pharmacists and Pharmaceutical premises in Nigeria (2014).


 Impact Factor: * 3.3
Impact Factor: * 3.3 Acceptance Rate: 74.39%
Acceptance Rate: 74.39%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 