Functional Outcome of MIPO (Minimally Invasive Plate Osteosynthesis) in Distal Third Femur Fractures with Intra Articular Extension
Jantaj Singh, Rajkumar Aggarwal, Chandan Jasrotia, Aarti Dewan*
Department of Orthopedics, Sri Guru Ram Das Institute of Medical Science and Research, Sri Amritsar, Punjab, India
*Corresponding Author: Aarti Dewan, Department of Orthopedics, Sri Guru Ram Das Institute of Medical Science and Research, Sri Amritsar, Punjab, India.
Received: 28 January 2023; Accepted: 16 February 2023; Published: 20 February 2023
Article Information
Citation:
Jantaj Singh, Rajkumar Aggarwa, Chandan Jasrotia, Aarti Dewan. Functional Outcome of MIPO (Minimally Invasive Plate Osteosynthesis) in Distal Third Femur Fractures with Intra Articular Extension. Journal of Orthopedics and Sports Medicine 5 (2023): 67-71.
View / Download Pdf Share at FacebookAbstract
Distal femur fractures include fractures of the supracondylar and intercondylar region. They account for around 3-6% of femur fractures. They occur both in younger patients (as the result of high energy trauma) or in older patients (from low energy trauma as pathological fracture secondary to osteoporosis or malignancy). Despite advances in implant design, the management of distal femur fractures remain challenging. Fracture comminution and intra-articular extension with severe soft tissue injury can make it difficult to obtain an adequate reduction while preserving the soft tissue attachments to bone fragments to allow for bone healing. This study was done to study the functional of MIPO (Minimally Invasive Plate Osteosynthesis) in distal third femur fractures with intra articular extension.
Keywords
<p>MIPO (Minimaly Inavasive Plate Osteosynthesis); Distal femur fractures; Intra articular extension; Comminution</p>
Article Details
1. Introduction
Distal femur fractures include fractures of the supracondylar and intercondylar region. They account for around 3-6% of femur fractures. They occur both in younger patients (as the result of high energy trauma) or in older patients (from low energy trauma as pathological fracture secondary to osteoporosis or malignancy). These fractures have the potential to generate significant long term disability particularly when they are related to marked bone comminution, extensive articular damage and severe soft tissue injury [1]. The evaluation and management of patients with distal femur fractures continue to evolve on the basis of the improved understanding of the local anatomy, impact of treatment and biomechanics of fixation techniques.
Despite advances in implant design, the management of distal femur fractures remain challenging. Fracture comminution and intra-articular extension with severe soft tissue injury can make it difficult to obtain an adequate reduction while preserving the soft tissue attachments to bone fragments to allow for bone healing [2]. There is low osteogenic potential due to osteoporotic bone in elderly patients. Knowledge of strength and weakness of different implants is necessary for successful treatment of these fractures.
Retrograde nailing cannot be used in complex intra articular fractures (AO type B/C) or simple articular fractures with extensive comminution where standard protocol is direct reduction of the articular fragment followed by lag screw fixation and indirect reduction of the metaphyseal component [3].
The main goal is to anatomical restoration of the articular surface of the knee joint, stable internal fixation, preservation of blood supply with early postoperative rehabilitation of knee joint.
The MIPO technique embodies all the biomechanical advantages of bridge plate fixation. The absolute rigidity that was initially the aim of plate osteosynthesis is now replaced by more elastic fixation allowing micromotion at the fracture level resulting in indirect bone healing and abundant callus formation [4].
MIPO technique showed a decreased incidence of implant failure and infection and reduced the need for secondary bone grafting procedures in numerous clinical series with further elaboration, the trend of indirect reduction led to the development of Minimally Invasive Plate Osteosynthesis (MIPO).
In MIPO, fracture is usually reduced by closed reduction through the soft tissue window away from fracture site, the metadiaphyseal component reduction becomes difficult and malalignment is a more common complication compared to conventional open reduction [5].
2. Aim and Objectives
Aim: Aim of the study is to study the functional outcome of MIPO (Minimally Invasive Plate Osteosynthesis) in distal third femur fractures with intra articular extension.
Objective: Objective of the study is to evaluate clinical and radiological outcome of patients of distal third femur fractures with intra articular extension treated with MIPO (Minimally Invasive Plate Osteosynthesis).
3. Material and Methods
This Interventional study was conducted from 1st April 2021 to July 2022 on patients of distal third femur fractures with intra articular extension who are skeletally mature or age of 18 years or above presented in the department of orthopedics SGRDIMSAR Amritsar in which MIPO (Minimally Invasive Plate Osteosynthesis) was included in the study to treat distal third femur fractures with intra articular extension. Patients with pathological fracture, open fracture grade 3b/3c requiring external fixation and Periprosthetic fractures were excluded from study.
4. Results
An interventional study comprising of 26 patients of distal femur fractures with intra articular extension treated with Minimally Invasive Plate Osteosynthesis (MIPO). Patients were admitted in Department of Orthopaedics at Sri Guru Ram Das Institute of medical Sciences and Research, Amritsar between 1st April 2021 to July 2022. This study was performed under the approval of our institution’s ethical review board. Informed consent was obtained from each participant. Out of 26 patients, 4 patients were lost to follow up. The final outcome of 22 cases on the basis of radiological and functional parameters was assessed and is here under:
4.1 Baseline characteristics
Maximum percentage of Age group was >50 years contributing to 65.4 % to the present study with minimum age of 18 years and maximum age of 80 years and the mean age of 54.5 ± 14.82. Out of 26 patients, 15 were female and 11 were male.
As per AO/OTA guidelines, it was observed that 10 cases were classified as 33C1 (38.5%), 15 were of 33C2 (57.7%) and one case was classified as 33C3 (3.8%).
|
Age |
Frequency |
Percent |
|
≤50 years |
9 |
34.6 |
|
>50 Years |
17 |
65.4 |
|
Gender |
||
|
Female |
15 |
57.7 |
|
Male |
11 |
42.3 |
|
AO TYPE |
||
|
33C1 |
10 |
38.5 |
|
33C2 |
15 |
57.7 |
|
33C3 |
1 |
3.8 |
Table 1: Demographic data.
5. Radiological Analysis
5.1 Coronal Plane Alignment: The normal range of anatomical lateral distal femoral angle was taken from 79 to 83 degree6. All the cases in this study had anatomical lateral distal femoral angle of uninjured side within this range with average mean of 80.86 ± 1.16. Postoperatively, anatomical lateral distal femoral angle was measured at 3rd month. There were 18 cases which had neutral alignment (there anatomical lateral distal femoral angle were within 79 to 83 degree). The average mean anatomical lateral distal femoral angle of operated side was 80.81 ± 2.55. This outcome was statistically insignificant (p value= 0.938) (Figure 1).
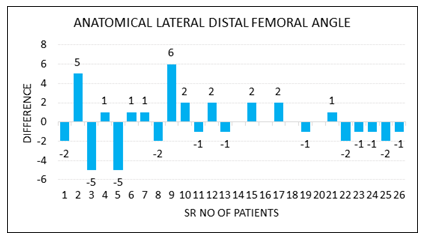
Figure 1: Anatomical lateral distal femoral angle.
There were 2 cases with valgus alignment which had valgus of 5 degree each and 2 cases had varus alignment with one case having 6 degree varus and the other case having 5 degree varus as compared to normal side of each case. (Figure 2).
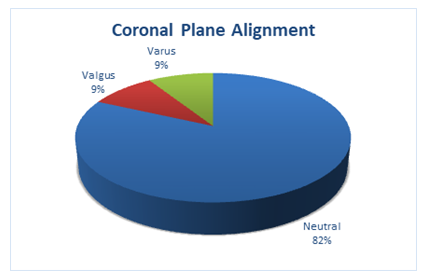
Figure 2: Coronal plane alignment.
5.2 Sagittal plane alignment: The normal range of angle between blumensaat line and anatomic axis of shaft of femur was taken as 35.4 ± 3 degrees [7]. The average mean angle of operated side was 35.22 ± 2.11. This outcome was statistically insignificant (p value = 0.097). Postoperatively, there were 20 cases which had neutral alignment (there angle was within this range). There was one case with 4 degree extension and one case of 4 degree flexion (Figure 3).
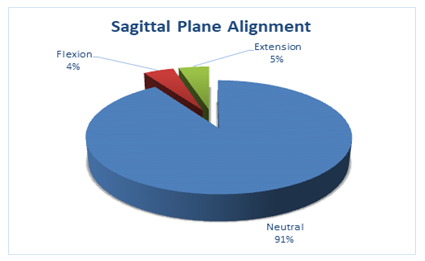
Figure 3: Sagittal plane alignment.
5.3 Total femoral length: There was an average decrease in total femoral length at 3rd month of 7.68 mm (p≤0.001) as compared to uninjured side. This outcome was statistically significant (Figure 4).
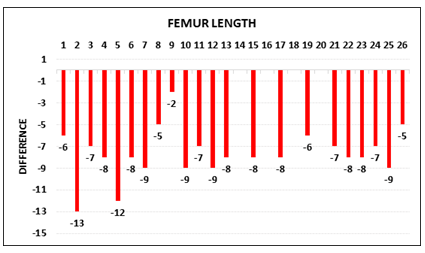
Figure 4: Difference in femoral length.
5.4 Rotational alignment: There was an average trend toward neutral alignment of the operated limb as compared to the uninjured limb. 19 patients had neutral rotational alignment. There were 3 cases of malrotation. 2 cases had external malrotation and 1 case with internal malrotation.
5.5 Union: Radiological union at 3 months was achieved in 19 cases in total. 3 cases had delayed radiological union (Figure 5).
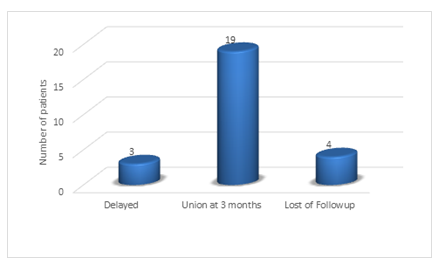
Figure 5: Radiological union of patients.
6. Functional Outcome:
Functional outcome at 3rd month was assessed using oxford knee score showed a mean score of 40 ± 1.83 with most cases having satisfactory outcome ≥40 score (14 cases). The mean range of motion achieved at 3 months was 96.14 ± 22.88 degrees (Table 2).
There were 2 cases with restriction of movement with both patients achieving 45 degree flexion. The flexion deformity (inability to achieve full extension) was present in 4 cases.
|
Mean ± SD |
Minimum |
Maximum |
|
|
Oxford Knee at 3 Months |
40 ± 1.83 |
36.00 |
43.00 |
|
Range of Motion |
96.14 ± 22.88 |
45.00 |
120.00 |
Table 2: Functional outcome of patients.
7. Discussion
Distal femur fractures include fractures of supracondylar and intercondylar region and have always been difficult to treat. They tend to occur in elderly population but incidences in younger age group have also been increasing due to increasing road traffic accidents. The goals for treatment are the anatomical restoration of articular surface, length, alignment and rotation with early mobilisation of joint. Various fixation methods for distal femur fractures have been described. it can be categorized into retrograde intramedullary nailing and plating. Plating can be further categorized into open anatomical reduction and fixation with plate or Minimally Invasive Plate Osteosynthesis (MIPO).
Our study comprised of 26 patients of distal femur fractures with intra articular extension (Ao type C) which were treated with Minimally Invasive Plate Osteosynthesis (MIPO). Out of the 26 patients, 4 patients were lost to follow up. The patients were treated with distal femur locking plate with direct articular reduction using lateral parapatellar approach and indirect reduction of metaphyseal component by Minimally Invasive Plate Osteosynthesis (MIPO). The functional outcome depends on adequacy of reduction and rigid fixation of articular fragment and maintenance of length, alignment and rotation in all the planes with early union of the fracture.
There were 18 cases in our study which had neutral coronal alignment (there anatomical lateral distal femoral angle were within 79 to 83 degree) 6 with 2 cases of varus alignment and 2 cases of valgus alignment, whereas Ajeet et al. [8] in 2018 had 5 patients who had varus deformity more than 10 degree.
Functional result in our study at 3rd month was assessed using oxford knee score showed an mean score of 40 ± 1.83 with most cases having satisfactory outcome ≥40 score (14 cases) and The mean range of motion achieved at 3 months was 96.14 ± 22.88 degrees. There were 2 cases with restriction of movement with both patients achieving 45 degree flexion, whereas Jati S et al. [9] in 2021 evaluated according to NEER’s scoring system 38 cases had excellent results and 8 cases had satisfactory results according to NEER’s scoring system with a mean NEER’s score of 90.133 (range 74 to 96) at a mean follow-up of 1 year and Knee stiffness was seen in 4 cases. This study had 4 cases of superficial infection, whereas there was one case of infection in our study which was treated with thorough debridement with retention of implant. This study had 2 cases of rotational mal-alignment whereas we had 3 cases of rotational malalignment.
8. Conclusion
At the end we can concluded that good functional and radiological outcome can be achieved in distal femur fractures with intraarticular extension by direct open reduction of the articular block and indirect reduction of the metaphyseal component via Minimally Invasive Plate Osteosynthesis (MIPO) (Figure 6).
According to standard teaching, the screw should be placed parallel to the knee joint in order to restore the anatomical lateral distal femoral angle. This depends on the native anatomical lateral distal femoral angle and also on the angle of the shaft of plate to the central locking screw. We have studied there is a variation in the normal anatomical lateral distal femoral angle and variation in the angle between shaft of plate and central locking screw of plates manufactured by different vendors. So we should template the uninjured side first in order to assess whether the screw should be put parallel or away from the knee joint in order to restore the native anatomical lateral distal femoral angle.

Figure 6: Showing method of templating.
Limitation of Study
The limitation of the present study was that we did not use single standard plate for fixation in all the cases of our study. We used different plates in our study which had variation in angle between shaft of plate and central locking screw.
Acknowledgement
We would like to thank all the patients who participated in the study . We acknowledge the help extended by department of orthopedics.
Funding Source
None
Conflicts of interest
There is no conflict of interest.
References
- Coon MS, Best BJ. Distal Femur Fractures. NCBI Bookshelf. National Institutes of Health. Treasure Island. Stat Pearls (2020): 1-14.
- von Keudell A, Shoji K, Nasr M, et al. Treatment Options for Distal Femur Fractures. J Orthop Trauma 30 (2016): S25-S27.
- Krishna C, Shankar RV. Current concept of management of supracondylar femur fracture: retrograde femoral nail or distal femoral locking plate. Int Surg J 3 (2016): 1356-1359.
- Nikolaou VS, Efstathopoulos N, Papakostidis C, et al. Minimally invasive plate osteosynthesis–an update. Curr Orthop 22 (2008): 202-207.
- Buckley R, Mohanty K, Malish D. Lower limb malrotation following MIPO technique of distal femoral and proximal tibial fractures. Injury 42 (2011): 194-199.
- Nam DJ, Kim MS, Kim TH, et al. Fractures of the distal femur in elderly patients: retrospective analysis of a case series treated with single or double plate. J Orthop Surg Res 17 (2022): 55.
- Yazdi H, Akbari Aghdam H, Motaghi P, et al. Using Blumensaat's line to determine the sagittal alignment of the distal femur. Eur J Orthop Surg Traumatol (2022).
- Singh A, Kumar R, Ranjan R, et al. Association of aLDFA with functional outcome of distal femur fracture treated with locking plate. Int J Res Orthop 4 (2018): 767-70.
- Jati S, Bansal H, Bohra T, et al. Functional outcome of distal end femur fractures treated by minimally invasive plate osteo-synthesis using locking compression plate: a prospective study in 50 adults. Ortho JMPC 27 (2021): 64-69.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 