Impact of Constraint- Induced Movement Therapy (CIMT) on Upper Limb Motor Functions of Post Stroke Survivors
Dina NA1*, Sharmin S2, Kamal T3, Sarker S4
1Department of Physical Medicine and Rehabilitation, National Healthcare Network, Dhaka, Bangladesh
2Department of Physical Medicine and Rehabilitation, Shaheed Monsur Ali Medical College, Dhaka, Bangladesh
3Department of Physical Medicine and Rehabilitation, Dhanmondi Diagnostic and Consultation Centre, Dhaka, Bangladesh
4Department of Physical Medicine and Rehabilitation, MH Samorita Hospital and Medical College, Dhaka, Bangladesh
*Corresponding Author: Naima Akhter Dina, Department of Physical Medicine and Rehabilitation, National Healthcare Network, Dhaka, Bangladesh.
Received: 05 January 2023; Accepted: 14 February 2023; Published: 17 February 2023
Article Information
Citation:
Dina NA, Sharmin S, Kamal T, Sarker S. Impact of Constraint- Induced Movement Therapy (CIMT) on Upper Limb Motor Functions of Post Stroke Survivors. Journal of Orthopedics and Sports Medicine 5 (2023): 62-66.
View / Download Pdf Share at FacebookAbstract
Background: Stroke is frequently accompanied by loss of motor function, where more than half of stroke survivors losing functional abilities in their affected upper limb. Constraint- Induced Movement Therapy (CIMT) is one of the rehabilitative interventions that can be effective for motor recovery.
Objectives: To observe the impact of Constraint- Induced Movement Therapy (CIMT) on upper limb motor functions of post stroke survivors. Methods: The study was designed as a Quasi- experimental study (Pretest and Post-test) conducted in the department of Physical Medicine and Rehabilitation, Shaheed Suhrawardy Medical College Hospital (ShSMCH), Dhaka. The patients eligible for CIMT were evaluated clinically and by standardized assessment tools at enrollment and followed up at 2 weeks and at 4 weeks after giving conventional rehabilitation and CIMT. Motor functional abilities of hemiparetic upper limb were assessed by Fugl-Meyer (FM) assessment.
Results: A total 60 patients were analyzed among them mean age was 52.77 ± 10.30 years. Most of them (72%) were male. Mean of onset stroke duration were found 34.62 ± 48.66 days. Ischemic stroke was found in 77% patients. Mean FIM score at baseline among the patients was 106.28 ± 12.61. Mean FM baseline score was 45.57 ± 7.56 where 86.7% and 13.3% patients were found in moderate and mild impairment group (p=0.000) respectively. Follow-up after two week mean FM score was found 52.25 ± 6.58 among them 68.3% in moderate impairment and 31.7% in mild impairment group (p=0.000). Follow-up after four week mean FM score was 54.42 ± 5.66 among them 60% in moderate impairment and 40% in mild impairment group (p=0.000).
Conclusion: Constraint-Induced Movement Therapy (CIMT) combined with conventi
Keywords
<p>Constraint-Induced Movement Therapy; Stroke; Motor function; Rehabilitation</p>
Article Details
1. Introduction
Stroke is one of the common and disabling health-care problems worldwide. It is the third most common cause of death in the developed world after cancer and ischemic heart disease, and is the most common cause of severe physical disability [1,2]. Every year, a significant number of stroke survivors are left with residual disabilities, varying from mild to severe form [3]. These disabilities can be reduced by proper rehabilitation [4,5]. The consequences of upper limb disability in post stroke adults influence their Activities of Daily Living (ADL) such as feeding, grooming, bathing, dressing, toileting etc. [6,7]. After stroke, when the function of one side is superior to contra lateral limb, patient may prefer to use the active limb to perform self-care. With time they use their non-involved limb to perform ADL [8,9]. Taub et al. [10,11] described this phenomenon as “learned non-use”. As upper limbs play a valuable role in performing ADL, retraining motor controls and skills to improve ADL should be an important aim of rehabilitation programs [8].
The upper limb dysfunction due to stroke is usually treated by using various rehabilitation approaches, CIMT is one of these approaches which may minimize the consequences of upper limb dysfunction and enhance stroke patients’ daily functional activities [10,12]. CIMT was developed by Dr. Edward Taub, is a therapeutic package based on two principles: (1) restraint of the less-affected limb for prolonged periods to force use of the more-affected limb and (2) supervised repetitive task practice of upper limb by shaping [13-16].
Types of restraints include a sling or triangular bandage, a splint, a sling combined with a resting hand splint, a half glove, and a mitt [17]. Determination of the type of restraint used for therapy depends on the required level of safety [18]. While restraining the unaffected upper limb 90% of waking hours, training the affected limb six hours a day, for two weeks in hospital setting [15,19-21]. Shaping is a training method in which a task is gradually made more difficult with respect to patient’s motor capabilities. It is systematic, specifiable and quantified. About 120 tasks have been developed by the Constraint Induced Therapy Research Group. Among which 10 to 15 tasks are selected primarily for each patient. Each task is usually performed in a set of 10-30 seconds trials. At the end of each set of 10 trials, the task is changed. Reward should be provided visually and verbally to encourage good performance. Performance regressions are usually ignored. Rest should be given between trials as needed [11].
As patient is engaged in repetitive exercises with the affected limb, the brain grows new neural pathways referred to as cortical reorganization or neuroplasticity. Thus, possible benefits are achieved [17,18,22] Reliable and valid measurements of motor functions are required to assess physical recovery following stroke. The Fugl-Meyer assessment was developed for these purposes. Fugl-Meyer motor assessment includes items dealing with the shoulder, elbow, forearm, wrist, and hand in the upper extremity [23-26].
2. Methods
The investigator himself recruited the cases during the training period in Shaheed Suhrawardy Medical College Hospital (ShSMCH). The investigator reviewed the diagnosis of all stroke cases every day morning referred to department of Physical Medicine and Rehabilitation, ShSMCH for rehabilitative purpose and follow up. All consecutive cases were checked for eligibility criteria (inclusion and exclusion criteria) and those found eligible were approached for informed consent by the investigator. The history was obtained from patients or closest attendant. Seventy Five (75) cases of Stroke (confirmed by CT scan of Brain), met eligibility criteria were selected for the study from ShSMCH, among them sixty (60) were patients with ischemic stroke and the remaining fifteen (15) were hemorrhagic stroke. The pre-designed semi-structured questionnaire was used for all cases. A face to face interview was used for filling out the questionnaire. The cases were evaluated clinically and by standardized assessment tools at enrollment (within 6 months of stroke onset) and followed up at 2 weeks and at 4 weeks after giving CIMT. Assessments included baseline demographics, clinical findings, stroke characteristics, impairments and motor functional abilities of hemiparetic upper limb before giving CIMT and motor functional abilities of hemiparetic upper limb after giving CIMT. Motor functional abilities of hemiparetic upper limb were assessed by Fugl-Meyer assessment.
3. Results
The study was conducted to observe the impact of Constraint- Induced Movement Therapy (CIMT) on upper limb motor functions of post stroke survivors attending at the Department of Physical Medicine and Rehabilitation (PMR) of Shaheed Suhrawardy Medical College Hospital (ShSMCH). During the study period 75 stroke patients according to inclusion and exclusion criteria were selected for CIMT on upper limb. But 10 subjects did not complete their treatment and 5 subjects did not come for second follow-up for unknown reasons. Finally sixty (n= 60) patients were evaluated for data presentation and analysis. Data are presented and analyzed according to objectives. The findings are presented through tables, graphs and organized as below:
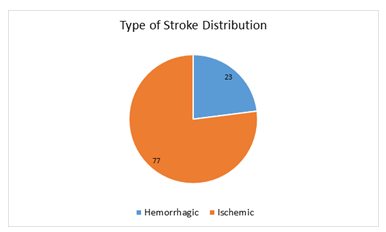
Figure 1: Type of stroke distribution (n= 60).
Among the study subjects regarding the type of stroke, most of the patients were found ischemic (77%) and rests (23%) were hemorrhagic.
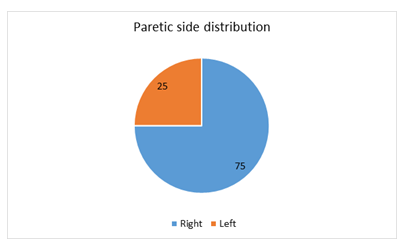
Figure 2: Paretic side distribution (n= 60).
Among the study subjects regarding the paretic side distribution, most of the patients’ (75%) paretic sides were right and rests 25% patients’ paretic sides were left.
|
Distribution of Comorbidities |
||
|
Distribution of Comorbidities |
Frequency |
Percent (%) |
|
Hypertension (HTN) |
31 |
51.7 |
|
Both hypertension and diabetic mellitus |
18 |
30 |
|
No hypertension or diabetic mellitus |
8 |
13.3 |
|
Diabetic mellitus (DM) |
3 |
5 |
|
Total |
N=60 |
100 |
Table 1: Distribution of comorbidities (n= 60).
Among the studied patients regarding the distribution of comorbidities, only Hypertension (HTN) and only Diabetic Mellitus (DM) were found in 51.7% and 5.0% patients respectively. Both DM and HTN were found in 30.0% patient and no HTN or DM was found in 13.3% patients.
|
FIM score |
Frequency |
Percent (%) |
Mean ± SD |
|
85-100 |
19 |
31.67 |
|
|
101-116 |
22 |
36.66 |
106.28 ± 12.61 |
|
117-126 |
19 |
31.67 |
|
|
Total |
60 |
100 |
Table 2: Distribution of FIM score at baseline (n= 60).
Mean FIM score at baseline among the studied patients was 106.28 ± 12.61. The lowest and highest FIM score at baseline in this study was 88 and 126 respectively.
|
FM score |
Frequency |
|
Percent% |
Mean ± SD |
P-value |
|
|
W0 FM |
Mild (58-66) |
8 |
n=60 |
13.3 |
45.57 ± 7.56 |
0 |
|
Moderate (28-57) |
52 |
86.7 |
||||
|
Severe(0-27) |
0 |
0 |
||||
|
W2 FM |
Mild (58-66) |
19 |
31.7 |
52.25 ± 6.58 |
0 |
|
|
Moderate (28-57) |
41 |
68.3 |
||||
|
Severe (0-27) |
0 |
0 |
||||
|
W4 FM |
Mild (58-66) |
24 |
40 |
54.42 ± 5.66 |
0 |
|
|
Moderate (28-57) |
36 |
60 |
||||
|
Severe(0-27) |
0 |
0 |
Table 3: Evaluation of FM score at different follow-up: (n= 60).
Table 3 showing evaluation of FM score at different follow-up. Where significant difference between mild and moderate impairment groups were found at initial assessment, week 2 and week 4 follow-up (P<0.05) regarding FM score. The Table 3 also shows increasing percentage of mild impairment group and decreasing percentage of moderate impairment group at week 2 and week 4 follow-up. No severe impairment group was found.
4. Discussion
This study was conducted to observe the impact of Constraint-Induced Movement Therapy (CIMT) on upper limb motor functions of post stroke survivors attending at the Department of Physical Medicine and Rehabilitation (PMR) of Shaheed Suhrawardy Medical College Hospital (ShSMCH). In this present study the mean age of the patients was 52.77 ± 10.30 years. Most of the patients were found in 46-60 years age group (60%) followed by 20% in 30-45 and 61- 70 years age group each. Similar mean age also found in many studies [8,27,28] including studies of Bangladesh 38-40 where most of stroke patients were between 51-70 years of age. Most of the patients in this study were male (72%). The ratio of male-female was 2.57:1. On the other hand male-female ratio in the study of Tariah et al. [27] was 4:1, Gharib et al. [8] was 1.67:1 and Steven et al. [29] was 2.86:1. Male predominance in stroke was also observed in various studies in Bangladesh [30-33] . In this study most of the patients were retired (33.3%) followed by 28.3% housewife, 18.3% service holder, 6.7% were farmer and businessman and 3.3% were teacher and unemployment each respectively, which coincided with the study of Hossain et al. [31] Among the patients mean duration of onset stroke were found 34.62 ± 48.66 days and most of the patients 78.3% in 1-30 days group. Rests were found 10.0% in more than 90 days, 8.3% in 61-90 days and 3.3% in 31-60 days group respectively. This reflects stroke patients seek rehabilitation not only in early phase but also in chronic phase of stroke [25]. Highest 77% patient’s type of stroke was Ischemic stroke. Most of the patient’s paretic side was right (75%). Similar result was found 70% in Tariah et al. [27], 60% in Sanford et al. [34] and 72% in Mohammad et al. [30] study respectively. Among the patients most of the comorbidities were found HTN 51.7% followed by both DM and HTN 30.0%, unknown 13.3% and DM 5.0% respectively. Hayee et al. [35] found that 52.11% were hypertensive, which was 58% by Alamgir et al. [36]. Similar studies in some Asian countries also correlated with the present study [37]. Mean of FM baseline score was found 45.57 ± 7.56, where moderate impairment group was 86.7% and mild impairment group was 13.3% (p=0.000). After two week follow-up mean FM score was 52.25 ± 6.58 among them 68.3% were in moderate impairment and 31.7% were in mild impairment group (p=0.000). After four week follow-up mean FM score was 54.42 ± 5.66 among them moderate impairment group 60% and mild impairment group 40% (p=0.000). No severe impairment was found in this study. A study done by Tariah et al. [27] found the mean of FM baseline score were 46.7 ± 12.64, after two months follow-up 55.8 ± 6.46 (p=0.061) and four months follow-up 54.5 ± 9.53 (p=0.336) respectively. These statuses were not statistically significant. The Fugl-Meyer Upper Extremity Motor Performance Section Test scores showed significant improvements (P=0.004) in a study of Whitall J et al. [6].
5. Conclusion and Recommendations
It may be suggested that Constraint-Induced Movement Therapy (CIMT) along with conventional therapy has a beneficial impact on post stroke hemiparetic upper limb survivors who were eligible for CIMT. Further descriptive and analytical studies with larger and representative sample size for the population are warranted to observe the impact of Constraint-Induced Movement Therapy (CIMT) on upper limb motor functions of post stroke survivors.
6. Limitations of the Study
The study was conducted on a relatively small sample. The study was conducted in a referral hospital in the capital city and may not be representative of total population as the hospitalization is associated with affordability and distance from the hospital (residential address reveals most of the patients were from the urban or semi urban areas). Furthermore, the study was Quasi- experimental study (Pre-test and Post-test) study and has its inherent weakness.
References
- Allen CMC, Lueck CJ, Dennis M. Davidson’s Principles and Practice of Medicine, 21st (2010): 1180-1191.
- Bonita R, Mendis S, Truelsen T, et al. The global stroke initiative. Lancet Neurol: 3 (2004): 391-393.
- O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 376 (2010): 112-123.
- Langhorne P, Bernhardt J, Kwakkel G. Stroke Care 2: Stroke rehabilitation. Lancet 377 (2011): 1693-702.
- Langhorne P, Sandercock P, Prasad K. Evidence-based practice for stroke. LancetNeurol 8 (2009): 308-309.
- Whitall J, McCombe WS, Silver KH, et al. Repetitive bilateral arm training with rhythmic auditory cueing improves motor function in chronic hemiparetic stroke. Stroke 31 (2000): 2390-2395.
- Gowland C, deBruin H, Basmajian JV, et al. Agonist and antagonist activity during voluntary upper-limb movement in patients with stroke. PhysTher 72 (1992): 624-633.
- Gharib M, Ghorbani H, Abdolvahab M, et al. Effect of Time Constraind Induced Therapy on Function, Coordination and Movements of Upper Limb on Hemiplegic adults. Iranian Rehabilitation Journal 9 (2011): 32-36.
- Pamela S, Vegher J, Gilewski M, et al. Client centered occupational therapy using constraint-induced therapy. Stroke 14 (2005): 115-121.
- Taub E, Miller NE, Novack TA, et al. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil 74 (1993): 347-354.
- Taub E, Harger M, Grier HC, et al. Some anatomical observations following chronic dorsal rhizotomy in monkeys. Neuroscience 5 (1980): 389-401.
- Wolf SL, Winstein CJ, Miller JP, et al. Retention of upper limb function in stroke survivors who have received constraint-induced movement therapy: the EXCITE randomized trial. Lancet Neurol 7 (2008): 33-40.
- Morris DM, Taub E, Mark VW. Constraint-induced movement therapy: characterizing the intervention protocol. EuraMedicophys 42 (2006): 257-268.
- Taub E, Crago JE, Burgio LD, et al. An operant approach to rehabilitation medicine: overcoming learned nonuse by shaping. J Exp Anal Behav 61 (1994): 281-293.
- Taub E, Uswatte G, Pidikiti R. Constraint-induced movement therapy: a new family of techniques with broad application to physical rehabilitation- a clinical review. Journal of Rehabilitation Research and Development 36 (1999): 237-251.
- Stevenson T, Thalman L, Christie H, et al. Constraint-Induced Movement Therapy Compared to Dose-Matched Interventions for Upper-Limb Dysfunction in Adult Survivors of Stroke: A Systematic Review with Meta- analysis. Physiotherapy Canada 64 (2012): 397- 413.
- Schaechter JD, Kraft E, Hilliard TS, et al. Motor recovery and cortical reorganization after constraint- induced movement therapy in stroke patients: a preliminary study. Neurorehabilitation Neural Repair 16 (2002): 326-338.
- Wittenberg GF, Chen R, Ishii K, et al. Constraint- induced therapy in stroke: Magnetic-stimulation motor maps and cerebral activation. Neurorehabilitation and Neural Repair 17 (2003): 48-57.
- Dromerick AW, Edwards DF, Hahn M. Does the application of constraint-induced movement therapy during acute rehabilitation reduce arm impairment after ischemic stroke? Stroke 31 (2000): 2984-2988.
- Alberts JL, Butler AJ, Wolf SL. The effects of constraint-induced therapy on precision grip: A preliminary study. Neurorehabilitation Neural Repair 18 (2004): 250-258.
- Winstein CJ, Miller JP, Blanton S, et al. Methods for a multisite randomized trial to investigate the effect of constraint-induced movement therapy in improving upper extremity function among adults recovering from a cerebrovascular stroke. Neurorehabilitation and neural repair 17 (2003): 137-152.
- Liepert J, Bauder B, Miltner HR, et al. Treatment-Induced Cortical Reorganization After Stroke in Humans. Stroke. 31 (2000): 1210-1216.
- Sanford J, Moreland J, Swanson LR, et al. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. PhysTher 73 (1993): 447-454.
- Fugl-Meyer AR, Jaasko L, Leyman I, et al. Thepost-stroke hemiplegic patient, I: a method forevaluation of physical performance. Scand J Rehabil Med 7 (1975): 13-31.
- Kim H, Her J, Ko J, et al. Reliability, concurrent validity and responsiveness of the Fugl-Meyer Assessment (FMA) of hemiplegic patient. J PhysTherSci 24 (2012): 893-899.
- Pang MYC, Harris JE, Eng JJ. A community-based group upper extremity exercise program improves motor function and performance of functional activities in chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil 87 (2006): 1-9.
- Tariah HA, Almalty AM, Sbeih Z, Oraib SA. Constraint induced movement therapy for stroke survivors in Jordon: a home-based model. International Journal of Therapy and Rehabilitation 17 (2010): 638-646.
- Taub E, Uswatte G, King DK, et al. A PlaceboControlled Trial of Constraint-Induced Movement Therapy for Upper Extremity after Stroke. Stroke 37 (2006): 1045-1049.
- Steven L, Wolf CJ, Winstein J, et al. Effect of Constraint-Induced Movement Therapy on Upper Extremity Function 3 to 9 Months After Stroke: The EXCITE Randomized Clinical Trial. JAMA 296 (2006): 2095-2104.
- Mohammad QD, Habib M, Mondal BA, et al. Stroke in Bangladeshi patients and risk factor. Mymensingh Med J 23 (2014): 520-529.
- Hossain AM, Ahmed NU, Rahman M, et al. Analysis of Sociodemographic and Clinical Factors Associated with Hospitalized Stroke Patients of Bangladesh. Faridpur Med Coll J 6 (2011): 19-23.
- Miah AH, Sutradhar SR, Ahmed S, et al. Seasonal variation in types of stroke and its common risk factors. Mymensingh Med J 21 (2012): 13-20.
- Islam MN, Moniruzzaman M, Khalil MI, et al. Burden of stroke in Bangladesh. Int J Stroke 8 (2013): 211-213.
- Sanford J, Moreland J, Swanson LR, et al. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. PhysTher 73 (1993): 447-454.
- Hayee A, Haque A, Anwarullah AKM, et al. Analysis of Risk factors of Stroke in 472 Cases. Bangladesh Journal of Neuroscience 14 (1999): 41-54.
- Alamgir SM, Mannan MA. Cerebrovascular disease: A report of 53 cases. Bangladesh Med Res Coun Bull 1 (1995): 45-50.
- Wasay M, Khatri IA, Kaul S. Stroke in South Asian countries. Nat Rev Neurol 10 (2014): 135-143.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 