Migraine Management Practices in India: A Comprehensive Review of Current Approaches, Challenges, and Future Directions
Sarthak Joshi*,1, Bhavya Goyal1, Dr. Sameeksha Joshi3, Dr. Tanishq Joshi4, Dr. Manjul Joshi5, Dr. Suvan Goyal6, Dr. Arun Koul2
1MBBS, Maulana Azad Medical College
2Department of Neurology, Govind Ballabh Pant Institute of Postgraduate Medical Education & Research and Maulana Azad Medical College
3MBBS, University College of Medical Sciences
4Department of Surgery, Himalayan Institute of Medical Sciences
5MBBS, Government Medical College, Haldwani
6MBBS, King George's Medical College
*Corresponding author: Sarthak Joshi, Maulana Azad Medical College, New Delhi.
Received: 22 July 2025; Accepted: 31 July 2025; Published: 118 August 2025
Article Information
Citation: Sarthak Joshi, Bhavya Goyal, Dr. Sameeksha Joshi, Dr. Tanishq Joshi, Dr. Manjul Joshi, Suvan Goyal, Dr. Arun Koul. Migraine Management Practices in India: A Comprehensive Review of Current Approaches, Challenges, and Future Directions. Journal of Pharmacy and Pharmacology Research. 9 (2025): 96-108.
View / Download Pdf Share at FacebookAbstract
Migraine constitutes a substantial public health challenge in India, marked by high prevalence, significant disability, and considerable socio-economic impact. Despite the availability of diverse treatment modalities, migraine remains widely underdiagnosed and undertreated. This systematic review comprehensively examines India's migraine treatment landscape, detailing conventional pharmacological agents-including Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), Triptans, Tricyclic Antidepressants (TCAs), beta-blockers, and newer Calcitonin Gene-related Peptide (CGRP) inhibitors, alongside traditional Ayurvedic and Unani medicines and complementary therapies like Yoga and meditation. Emerging non-invasive neuromodulation techniques are also discussed as promising alternatives. Analysis of current prescription trends reveals the prevalent use of NSAIDs and Fixed Dose Combinations (FDCs) for acute management, and TCAs, propranolol, and flunarizine for prevention, with concerns regarding polypharmacy. Furthermore, critical gaps are identified in healthcare professional knowledge, drug information accessibility, and patient access, exacerbated by sociocultural factors and prevailing stigma. The article underscores the imperative for integrated, culturally sensitive, and policy-driven interventions to enhance patient outcomes and mitigate the national burden of this debilitating neurological disorder. It highlights the significant opportunity for combining evidence-based traditional therapies with conventional treatments to foster a more personalized and holistic treatment paradigm in India.
Keywords
<p>Migraine Management; India; Pharmacological Treatments; Traditional Medicine; Public Health</p>
Article Details
Introduction: The Burden of Migraine in India
Migraine is a widespread neurological disorder that significantly impacts public health in India. Epidemiological data indicate that approximately 15% of adults in India are affected by migraine, with a notable higher prevalence observed among women and in urban populations.[1] The country has experienced a dramatic increase in the incidence and prevalence of headache disorders, including migraine, over the past three decades. From 1990 to 2019, India witnessed a substantial 91.07% rise in migraine prevalence, primarily attributed to population growth.[2] In 2019, India bore the largest absolute burden of migraine cases and associated disability-adjusted life-years (DALYs) among the BRICS nations, accounting for approximately 17.93 million cases and 7.69 million DALYs [3]. The profound impact of migraine extends beyond individual suffering, contributing significantly to global disability and lost productivity.[3] Migraine attacks are complex neurological events that can last for hours to days, severely impeding an individual's ability to engage in daily activities, work, and social interactions.[3,4] The economic burden of migraine encompasses both direct costs, such as medical care and treatment expenses, and substantial indirect costs, including lost wages and decreased work performance. This dual burden disproportionately affects younger adults and working professionals, highlighting the considerable economic consequences of this condition.[5]
Despite its widespread occurrence and debilitating effects, migraine is frequently underdiagnosed and undertreated in India. This issue is particularly pronounced in low-resource settings, where healthcare systems grapple with fragmented infrastructure and limited awareness regarding headache disorders.[1,3,6] The pervasive nature of migraine, coupled with its frequent under-recognition and stigmatization, means that a significant portion of affected individuals often remain undetected and receive inadequate treatment.[6,7] This creates a critical disjunction: a widespread health issue with substantial societal and economic costs is not adequately addressed at a systemic level. The perception of migraine as an "invisible" illness, as highlighted by public awareness campaigns[7], often leads to its neglect by policymakers. This, in turn, results in underfunded public health systems and a lack of standardized care, perpetuating a cycle where the burden of the disease continues to grow without commensurate resource allocation or targeted national strategies.[8] Recognizing migraine as a major public health and economic challenge is therefore essential for informing effective policy and resource distribution.
2. Conventional Pharmacological Treatment Practices
Acute Migraine Management
Conventional pharmacological treatment for migraine in India primarily focuses on providing acute symptom relief during an attack. The mainstays of acute management include triptans and nonsteroidal anti-inflammatory drugs (NSAIDs).[9] Triptans, a class of serotonin receptor agonists, are highly effective for severe headaches and migraine attacks that do not respond to general analgesics or NSAIDs.[10] Commonly available triptans in India include sumatriptan, rizatriptan, zolmitriptan, eletriptan, naratriptan, and almotriptan.[10,11] Sumatriptan, particularly when administered subcutaneously, is noted as the most effective and fastest-acting treatment for acute attacks.[10] Oral triptans like eletriptan (40 mg) and rizatriptan (10 mg) are recognized as the fastest-acting oral options based on meta-analyses, while naratriptan and frovatriptan have longer half-lives.[10] If a patient does not respond to one triptan, trying another is a common strategy.[10]
Combination drugs are also frequently prescribed. Examples include Naproxen combined with Sumatriptan (e.g., Headset Tablet), Naproxen with Domperidone (e.g., Naxdom 500 Tablet, Napra D 500 Tablet), and Caffeine with Ergotamine, Paracetamol, and Prochlorperazine (e.g., Vasograin Tablet).[11] Simple analgesics such as acetylsalicylic acid (aspirin), paracetamol, and ibuprofen, often in combination with caffeine, are effective for mild to moderate migraine attacks and should be considered first-line for these cases.[10] Antiemetics are also crucial for managing associated symptoms like nausea and vomiting during a migraine attack.[10] It is important to note that opioid analgesics are generally not recommended for the treatment of acute migraine attacks.[10] The efficacy of acute migraine medications, including triptans, is enhanced when taken early in the headache phase [10].
Preventive Migraine Therapies
Preventive medications are prescribed to reduce the frequency, severity, and duration of migraine attacks, enhance responsiveness to acute therapies, and ultimately improve the patient's quality of life.[12] Several classes of drugs are commonly employed for migraine prophylaxis in India:
- • Tricyclic Antidepressants (TCAs): Amitriptyline is a widely used TCA for migraine prophylaxis. It is considered an effective monotherapy, with a recommended initial dose of 5-10 mg and a gradual titration over six months for optimal results.[12] Amitriptyline is also deemed safe for managing catamenial migraine and can be utilized at lower doses during pregnancy.[12] While it has been a mainstay for over 35 years, its status as the first drug of choice in prophylactic therapy is debated in India, with clinical practice variations observed.[12] A systematic review and meta-analysis found that amitriptyline significantly reduced monthly migraine frequency compared to placebo. Furthermore, when compared to propranolol, amitriptyline demonstrated superiority in reducing monthly migraine frequency, duration, and severity.[2] However, no significant differences were observed between amitriptyline and flunarizine in terms of monthly migraine frequency or severity.[2]
- • Beta-blockers: Propranolol, metoprolol, and timolol are effective for migraine prevention and are frequently offered to patients to reduce attack frequency and severity.[2,9,12,13] Propranolol is one of the most regularly used beta-blockers for migraine prevention.[2]
- • Anticonvulsants: Divalproex sodium, sodium valproate, and topiramate are established as effective preventive options [2,12,13]. Divalproex sodium has shown a significant reduction in migraine headache rate. However, its use requires careful follow-up and testing due to potential risks such as pancreatitis, liver failure, and teratogenicity.[13]
- • Calcium Channel Blockers: Flunarizine is recommended in many national guidelines and holds Level A evidence supporting its use for migraine prevention.[2]
- • Other Antidepressants: Serotonin-norepinephrine reuptake inhibitors (SNRIs) and selective serotonin reuptake inhibitors (SSRIs) are also utilized in migraine management [12].
- • Angiotensin Receptor Blockers (ARBs) and ACE Inhibitors: Candesartan and Lisinopril have shown potential efficacy for migraine prevention, demonstrating reductions in headache days and hours in studies [13].
Table 1: Common Conventional Migraine Medications in India (Acute & Preventive)
|
Medication Class / Type |
Examples (Brand/Generic) in India |
Primary Use |
Notes |
|
Acute Migraine Management |
|||
|
Triptans |
Sumatriptan (e.g., Headset Tablet), Rizatriptan, Zolmitriptan, Eletriptan, Naratriptan, Almotriptan |
Severe headache relief, attacks unresponsive to analgesics/NSAIDs |
Highly effective; subcutaneous sumatriptan is fastest-acting; can be combined with naproxen [10,11] |
|
NSAIDs |
Naproxen (e.g., Naxdom 500 Tablet, Napra D 500 Tablet), Ibuprofen, Aspirin |
Mild to moderate headache relief |
Often combined with other agents [10,11] |
|
Combination Analgesics |
Caffeine + Ergotamine + Paracetamol + Prochlorperazine (e.g., Vasograin Tablet) |
Acute relief |
Ergotamine efficacy poorly documented in prospective studies [10,11] |
|
Antiemetics |
Domperidone (e.g., Grenil Tablet) |
Nausea and vomiting relief |
Effective during migraine attacks [10,11] |
|
Preventive Migraine Therapies |
|||
|
Tricyclic Antidepressants (TCAs) |
Amitriptyline |
Reduce frequency, severity, duration |
Effective monotherapy; debate on first-line status in India; superior to propranolol in some aspects [2,12] |
|
Beta-blockers |
Propranolol, Metoprolol, Timolol, Atenolol |
Reduce frequency, severity, duration |
Commonly used for prevention [2,9,12,13] |
|
Anticonvulsants |
Divalproex sodium, Sodium valproate, Topiramate |
Reduce frequency, severity, duration |
Require careful monitoring due to potential risks [2,12,13] |
|
Calcium Channel Blockers |
Flunarizine |
Reduce frequency, severity, duration |
Recommended in national guidelines (Level A evidence) [2] |
|
Angiotensin Receptor Blockers (ARBs) |
Candesartan |
Reduce frequency, severity, duration |
Possibly effective for prevention [13] |
|
ACE Inhibitors |
Lisinopril |
Reduce frequency, severity, duration |
Possibly effective for prevention [13] |
|
CGRP Inhibitors (Monoclonal Antibodies) |
Erenumab, Fremanezumab, Galcanezumab |
Prevention of episodic and chronic migraines |
Novel class, generally well-tolerated, effective [9,14,15,16,17] |
|
Gepants (Oral CGRP receptor antagonists) |
Rimegepant, Ubrogepant, Atogepant, Lasmiditan |
Acute treatment and prevention (Atogepant) |
As effective as basic painkillers for acute, Atogepant promising for prevention [18,19] |
Deficiencies in Drug Information Sources
A significant challenge in rational migraine drug usage in India stems from substantial deficiencies and variations in drug information sources. A study assessing information for acute-specific migraine drugs like ergots and triptans revealed widespread incompleteness across major reference materials.[20]
The Central Drugs Standard Control Organization (CDSCO), a government source, exhibited only 21.77% completeness in drug information. Crucially, it lacked details on contraindications, special precautions, adverse drug reactions, drug interactions, or pregnancy categories for listed triptans and ergotamine tartrate.[20] Its focus appeared to be solely on approved indications and banned drugs, rather than providing comprehensive details for end-users.[20]
The National Formulary of India (NFI) showed similar limitations with 21.1% completeness. Despite its role as a key reference, it covered only two acute migraine drugs (dihydroergotamine and sumatriptan) and provided insufficient dosage information. Critical parameters such as contraindications, special precautions, and adverse drug reactions for sumatriptan were inadequate, and drug interaction information was entirely missing for both listed drugs.[20] Furthermore, the NFI was inconsistent with updates to the National List of Essential Medicines (NLEM), still including dihydroergotamine despite its removal from NLEM 2015.[20]
Current Index of Medical Specialties (CIMS) hard copies demonstrated a mere 18.37% completeness. For drugs like ergotamine, sumatriptan, rizatriptan, and zolmitriptan, only partial information on indication and dose was available, with crucial parameters like contraindications, adverse drug reactions, and pregnancy categories entirely absent.[20] While CIMS online resources offered more complete information for some triptans, the study primarily focused on the deficiencies in hard copies.[20]
The Monthly Index of Medical Specialties (MIMS) showed a comparatively higher completeness score of 72.79%. However, it still presented insufficient dosage information for sumatriptan and, critically, omitted pregnancy category information for all listed antimigraine drugs.[20] This omission is a severe safety concern, especially given that migraine predominantly affects females in reproductive age groups.[20] The transition of MIMS to online-only resources after April 2019 suggests a shift in information dissemination, but the historical deficiencies underscore a systemic issue.[20]
These information gaps across major Indian drug information sources have significant implications. When healthcare professionals and patients lack comprehensive, consistent, and reliable drug information, it directly impedes rational prescribing practices and patient adherence. Such deficiencies can lead to irrational drug usage[20], suboptimal treatment outcomes, and an increased risk of adverse events. The absence of crucial details like pregnancy categories highlights a profound patient safety concern, particularly for a condition prevalent among women of childbearing age. The consistent call for government and commercial entities to "streamline and provide comprehensive, uniform, and reliable drug information"[20] emphasizes the urgent need for regulatory and educational reforms to ensure safe and effective pharmacological management of migraine.
3. Traditional and Complementary Medicine Approaches
Traditional Indian systems of medicine, such as Ayurveda and Unani, alongside complementary practices like Yoga and meditation, play a significant role in migraine management, often offering holistic and culturally resonant approaches.
Ayurvedic Treatment Principles and Therapies
In Ayurveda, migraine is correlated with "Ardhavabhedaka," a condition believed to arise from the simultaneous vitiation of all three Doshas—Vata, Pitta, and Kapha—though Vata imbalance is often considered primary.[21,22,23,24] The Ayurvedic treatment philosophy for Ardhavabhedaka is comprehensive, focusing on addressing the root cause and restoring systemic balance rather than merely alleviating symptoms. Key treatment principles advocated by various Ayurvedic scholars include:
- • Avoidance of Cause (Nidana Parivarjana): Identifying and eliminating the specific causative factors that trigger Dosha vitiation, such as suppression of natural urges, excessive physical or sexual activity, increased intake of dry/rough food, excessive fasting, or exposure to cold.[21]
- • External Therapies: These include Shiroabyanga (head massage), Upanaha Sweda (application of hot poultices), and Shirobasti (a procedure involving retaining medicated oil on the head using a cap).[21]
- • Internal Oleation (Snehapana): Oral administration of medicated oils or ghee.[21]
- • Purificatory Therapies (Shodana): These detoxification procedures are central to Ayurvedic treatment and include Vamana (therapeutic emesis), Virechana (therapeutic purgation), Basti (medicated enemas), and Nasya (administration of medicated drops through nasal passages).[21,22,23] Virechana, in particular, is emphasized for removing toxins (Aam) and alleviating vitiated Vata and Pitta Doshas, thereby restoring digestive fire (Jatharagni).[22]
- • Local Applications (Lepa): External application of medicinal pastes.[21]
- • Other Specific Procedures: Rakta Mokshana (therapeutic bloodletting) and Agnikarma (therapeutic cauterization) are also mentioned.[21]
- • Dosha-Specific Treatments: Vatakaphahara Chikitsa involves treatments aimed at pacifying Vata and Kapha doshas.[21]
- • Lifestyle and Mind-Body Practices: The integration of Pranayama (breathing exercises), Yoga, and physical and mental rest is crucial for overall well-being and stress reduction.[21]
Specific Herbs and Formulations are frequently employed in Ayurvedic migraine management:
- • Triphala Churna: This traditional formulation, primarily kapha pittagna (pacifying Kapha and Pitta doshas), has a prominent anulomana (downward regulating/carminative) action. It helps in normalizing misdirected Vata dosha and clearing blockages (sanga) in the body's channels (srotas), which are often a root cause of Vata imbalance.[21] A dosage of 12 gm in divided doses with warm water post-food is suggested, as this timing is believed to optimize its action on udana vata (a subtype of Vata responsible for upward movements), thereby addressing headache symptoms.[21] Warm water (Ushnajala) serves as an adjuvant, promoting prompt drug action.[21]
- • Indigenous Drug Compound (for menstrual migraine): A specific compound is mentioned for menstrual migraine, incorporating:
- • Shatavari (Asparagus racemosus): Acts as a rejuvenator and targets the uterus and breast, making it relevant for hormonally-linked migraines.[21]
- • Brahmi (Bacopa monnieri): A renowned nootropic (medhya) herb, it effectively acts on both the head (shiras) and heart (hrdaya), the seat of intellect. Its cooling potency (sheeta dravya) helps alleviate mental distress like anxiety and irritability often associated with migraine.[21]
- • Haridra (Curcuma longa - Turmeric), Nimba (Azadirachta indica - Neem), and Tagara (Valeriana wallichi): These are hot-potency (ushna dravyas) drugs with lekhana (scraping) properties that facilitate the action of other herbs. Haridra is also a potent antitoxin (Vishagna), reducing toxins from diet and other medications.[21]
- • Ayurvedic Treatment Protocol (AyTP): A specific protocol involving five Ayurvedic medicines—Narikel Lavan, Sootshekhar Rasa, Sitopaladi Churna, Rason Vati, and Godanti Mishran—alongside regulated diet and lifestyle modifications, showed promising results. A study found complete disappearance of headache and associated symptoms in 35.2% of patients, and a marked reduction in migraine frequency and pain intensity in 70.5% of patients after 90 days of treatment.[25]
- • Ayush M-3: This polyherbal formulation is currently undergoing a prospective, randomized, double-blind, placebo-controlled, multi-centric clinical trial in India to assess its safety and efficacy in migraine patients, indicating ongoing scientific validation efforts within the Ayurvedic system.[26]
- • Other Natural Products: Ginger, butterbur, turmeric, feverfew, and ginkgo are recognized for their promising potential as natural supplements in migraine management.[9]
Efficacy Studies demonstrate the beneficial role of Ayurveda. Case studies and clinical trials suggest that Ayurvedic management can be effective as a monotherapy or as an add-on to conventional approaches, leading to observed improvements in headache frequency, intensity, and disability.[22,23,24,27] For instance, a study on anxiety-induced migraine showed significant improvement in headache duration, severity, and frequency with a protocol including Laghu Sutashekhara Rasa, Brihata Dashmoola Taila Nasya, Tablet Anzee (a combination of Tagar, Ashwagandha, Brahmi, and Shankhpushpi), and Rasayana Yoga.[24,27]
Table 2: Key Ayurvedic Treatment Principles and Herbs for Migraine
|
Category |
Principle / Herb / Formulation |
Description / Action for Migraine |
|
Treatment Principles |
Avoidance of Cause (Nidana Parivarjana) |
Eliminating triggers like suppressed urges, excessive activity, specific foods, or cold exposure [21] |
|
Shiroabyanga (Head Massage) |
Therapeutic massage of the head [21] |
|
|
Snehapana (Oleation) |
Internal administration of medicated oils or ghee [21] |
|
|
Upanaha Sweda (Hot Poultice) |
Application of hot poultices [21] |
|
|
Shirobasti |
Medicated oil retained on the head using a cap [21] |
|
|
Shodana (Purificatory Therapies) |
Detoxification via Vamana (emesis), Virechana (purgation), Basti (enema), Nasya (nasal drops) to remove toxins and balance Doshas [21,22,23] |
|
|
Lepa (Local Application) |
External application of medicinal pastes [21] |
|
|
Rakta Mokshana (Bloodletting) |
Therapeutic bloodletting [21] |
|
|
Agnikarma (Cauterization) |
Therapeutic cauterization [21] |
|
|
Vatakaphahara Chikitsa |
Treatments to pacify Vata and Kapha doshas [21] |
|
|
Pranayama, Yoga, Physical & Mental Rest |
Holistic practices for stress reduction and overall well-being [21] |
|
|
Specific Herbs / Formulations |
Triphala Churna |
Pacifies Kapha and Pitta, has downward regulating action, helps normalize misdirected Vata, clears channel blockages [21] |
|
Shatavari (Asparagus racemosus) |
Acts on uterus, considered target-oriented for menstrual migraine [21] |
|
|
Brahmi (Bacopa monnieri) |
Nootropic, acts on head and heart, helps relieve anxiety/irritability (cold potency) [21] |
|
|
Haridra (Curcuma longa - Turmeric) |
Hot-potency, scraping property, potent anti-toxic, reduces toxins [21] |
|
|
Nimba (Azadirachta indica - Neem) |
Hot-potency, scraping property, aids action of other herbs [21] |
|
|
Tagara (Valeriana wallichi) |
Hot-potency, scraping property, balances effects of other herbs [21] |
|
|
Ayurvedic Treatment Protocol (AyTP) (Narikel Lavan, Sootshekhar Rasa, Sitopaladi Churna, Rason Vati, Godanti Mishran) |
Combination of five medicines with diet/lifestyle, showed marked reduction in frequency/intensity in 70.5% patients [25] |
|
|
Ayush M-3 |
Polyherbal formulation undergoing clinical trial for safety and efficacy [26] |
|
|
Ginger, Butterbur, Feverfew, Ginkgo |
Natural supplements with promising potential for migraine management [9] |
Unani Medicine for Migraine
In Unani medicine, migraine is referred to as "Shaqeeqa," and its pathogenesis is rooted in the imbalance of humors (blood, phlegm, yellow bile, black bile) and the accumulation of morbid matter, either vapors or humors, in vulnerable regions of the brain.[28] Unani scholars, including historical figures like Avicenna and Jurjani, classified migraines based on the nature of these humoral imbalances, distinguishing between "hot" (Shaqeeqa Haar) and "cold" (Shaqeeqa Barid) humoral conditions.[28]
Treatment principles in Unani medicine are aligned with humoral theory:
- • Acute Migraines (Shaqeeqa Haar): Associated with hot humors, these are managed through evacuation (Istifragh) and cooling therapies, provided the patient's physical condition permits.[28] Localized massage with analgesic and anti-inflammatory agents on the temporal region is beneficial, and medicated irrigation (Dalk) is also suggested.[28] Bloodletting (Fasd) from the cephalic vein on the affected side is a key procedure for intense pain, particularly in sanguineous migraines caused by hot and wet humors.[28]
- • Chronic Migraines (Shaqeeqa Barid): Involving cold humors, these necessitate long-term detoxification strategies.[28]
- • Key Therapeutic Interventions: Across both types, core interventions include purgation, bloodletting, herbal formulations, and dietary adjustments, all aimed at restoring humor balance.[28] For example, cold and dry foods are advised for sanguineous migraines, while cold and wet edibles are recommended for those caused by bilious humors.[28]
- • Holistic Approach: Unani medicine emphasizes a holistic perspective, recognizing and addressing psychological triggers such as stress and anxiety in migraine management.[28]
Specific Formulations available in India reflect these principles:
- • Hamdard Itrifal Ustukhudus: This Unani medicine, containing Triphala and Ustukhuddus (Lavandula Stoechas), is known for its potential benefits in headaches and migraine. Its primary action is on the brain and intestines, providing strength to these organs. Ustukhuddus and almond oil are believed to have MEDHYA (nootropic) effects, acting as brain tonics. Ingredients like Rosa Damascena flower, Amla, and raisins help reduce acidity, which can alleviate headaches associated with hyperacidity or gastric issues. The formulation also helps reduce gas formation, abdominal distention, and cramps.
- • Ayush Chhinkni Unani Medicine: This is a snuff powder containing eucalyptus, used for cold relief and headache. It is applied by sniffing a pea-sized amount to induce sneezes, which helps clear nasal passages and relieve symptoms.
The emphasis on holistic approaches in both Ayurveda and Unani, which address not only symptoms but also underlying systemic imbalances (Doshas, humors) and psychological factors like stress, aligns closely with the evolving understanding of migraine management in modern medicine. This continued use and ongoing research into traditional systems, such as the clinical trial for Ayush M-3[26], suggest a significant opportunity for integrative medicine in India. By combining evidence-based traditional therapies with conventional treatments, a more personalized and holistic treatment paradigm can be offered. This approach has the potential to improve patient outcomes and reduce reliance on pharmaceuticals alone, especially considering the side effects and chronic nature of migraine, while also catering to the cultural preference for traditional remedies prevalent in India [6,9].
Yoga and Meditation as Adjuvant Therapy
Yoga, an ancient Indian mind-body practice, is increasingly recognized for its beneficial effects as an adjuvant therapy in migraine management. Studies indicate that regular yoga practice can positively influence migraine measures such as headache frequency, intensity, and duration of attacks [29,30]. The therapeutic mechanisms of yoga in migraine are multifaceted. It is known to reduce stress, a major migraine trigger, and improve blood flow. Additionally, yoga practices can lower blood pressure and slow heart rate, aiding the body's recovery from stressful events like migraine episodes [30,31]. By loosening tight areas in the body, such as the neck, head, and shoulders, which often hold tension and stress, yoga can help prevent migraine onset or alleviate existing symptoms.[30]
Clinical evidence supports the efficacy of yoga. A randomized controlled trial conducted in New Delhi, India, found that yoga, when used as an add-on therapy to conventional medical management, was superior in reducing headache frequency, intensity, and Headache Impact Test (HIT)-6 scores. It also significantly improved Migraine Disability Assessment (MIDAS) scores.[29] This research suggests that integrating yoga can be a cost-effective and safe intervention for migraine management.[29,30] Specific yoga poses and practices identified as helpful include Sukshma Vyayama, Pada Sanchalanasana (cycling yoga pose), Hand stretch breathing, Shashankasana (rabbit pose), and Savasana with Yoga Nidra (deep relaxation technique).[30] Pranayama, or breathing exercises, particularly abdominal breathing and focusing on breathing from the left nostril (considered a cooling and calming nostril), are also suggested for relaxation and managing attacks [31]. The strong connection between stress and migraine, with stress being a frequently identified trigger in the Indian context [4,32], makes yoga a particularly valuable intervention. Yoga's proven efficacy in stress reduction [30,31], combined with its cost-effectiveness and accessibility, positions it as a highly beneficial complementary therapy in India. Its integration into comprehensive migraine management plans can directly address a significant trigger, potentially leading to a reduction in migraine frequency and severity, and an overall improvement in patients' quality of life, especially for those seeking alternatives or adjuncts to conventional medication due to side effects or chronic nature of the condition.
4. Emerging Treatments and Clinical Trial Landscape
The landscape of migraine treatment is continually evolving, with novel pharmacological agents and non-invasive neuromodulation techniques offering new hope, particularly for patients who do not respond to conventional therapies.
Novel Pharmacological Agents
- • Calcitonin Gene-Related Peptide (CGRP) Inhibitors: This is a relatively new class of medications, primarily monoclonal antibodies (mAbs), approved for both migraine prevention and acute treatment. These drugs work by blocking the CGRP neuropeptide, which is a key mediator of vasodilation and pain in migraine pathophysiology [9,16,17]. Erenumab was the first FDA-approved mAb specifically for migraine prevention [14].
- • Efficacy and Tolerability of Erenumab in the Indian Population (EMPOwER Study): A 12-week, double-blind, randomized, placebo-controlled study (EMPOwER) evaluated erenumab in adult patients with episodic migraine from Asia, the Middle East, and Latin America, with a specific analysis focusing on the Indian sub-population.
- • Efficacy: Both 70 mg and 140 mg doses of erenumab demonstrated numerical improvement in reducing Monthly Migraine Days (MMDs) from baseline at month 3 compared to placebo.[14,33] A higher proportion of patients in both erenumab groups achieved at least a 50% reduction in MMD (59.4% for 70 mg, 58.9% for 140 mg) compared to placebo (50.8%) at month 3. Significant reductions were also observed for ≥75% reduction (45.3% for 70 mg, 43.3% for 140 mg vs. 33.1% for placebo) and 100% reduction in MMD.[14,33] The reduction in monthly acute migraine-specific medication days was numerically less in the erenumab groups compared to placebo.[14,33] Furthermore, there was a numerically higher reduction in Headache Impact Test (HIT-6™) total scores and a larger decrease in Migraine Disability Assessment (MIDAS) scores in the erenumab-treated groups, indicating improved quality of life and reduced disability.[14,33]
- • Tolerability: The incidence of treatment-emergent adverse events (TEAEs) was comparable across all groups (22.7% for erenumab 70 mg, 24.5% for 140 mg, and 25.2% for placebo), with no new safety signals reported in the Indian population.[14,33] Common TEAEs included pyrexia, nasopharyngitis, constipation, and cough.[14,33] Notably, elevated sitting systolic and diastolic blood pressures were reported in both erenumab and placebo groups in the Indian sub-population, a finding not consistently observed in earlier global studies.[14,33]
- • Other CGRP antagonists available globally include fremanezumab and galcanezumab, which have also shown efficacy in reducing monthly migraine days and improving responder rates [15,17].
- • Gepants: This is a newer class of oral small-molecule CGRP receptor antagonists, including rimegepant, ubrogepant, and lasmiditan.[18,19] While often positioned as "major breakthroughs" by pharmaceutical companies, studies suggest that these newer, more costly drugs are only as effective as basic painkillers like paracetamol and NSAIDs for acute treatment, and potentially less effective than older triptans.[18] However, atogepant, another gepant, is a promising oral medication specifically for preventive treatment. It has demonstrated significant efficacy in reducing monthly migraine days and improving functional outcomes for both episodic and chronic migraines and can also help with medication-overuse headaches. Atogepant is a prescription-only medication, typically recommended for patients who have not responded to other preventive therapies.[19]
- • PACAP Inhibitors: Research is also exploring monoclonal antibodies that target pituitary adenylate cyclase activating polypeptide (PACAP), another neuropeptide involved in vasodilation. Since PACAP acts more broadly than CGRP, blocking it could potentially benefit a wider range of migraine sufferers, including those who do not respond well to CGRP inhibitors.[16] Lu AG09222 is an example currently in Phase 2 clinical trials, showing promising results in reducing migraine days [16].
Non-Invasive Neuromodulation Techniques
Non-invasive neuromodulation techniques represent a drug-free alternative or adjunctive approach for migraine management, particularly beneficial for patients who cannot tolerate or do not respond to conventional pharmacological treatments, or for adolescents where drug-free options are preferred.
- • Remote Electrical Neuromodulation (REN): This technique involves administering an electrical stimulus at specific neural locations. It is a reversible and non-invasive process designed to alleviate head pain.
- • Transcranial Magnetic Stimulation (TMS): TMS works by stimulating brain tissues through magnetic pulses, which can reduce the frequency and severity of migraine attacks.[30]
- • Nerve Blocks: These minimally invasive procedures involve injecting a local anesthetic or anti-inflammatory medication near specific nerves responsible for transmitting pain signals. By blocking these signals, nerve blocks effectively interrupt pain pathways, providing relief from headaches and migraines. Commonly used nerve blocks for headaches include:
- • Greater Occipital Nerve (GON) Block: Targets the greater occipital nerve.[34]
- • Sphenopalatine Ganglion (SPG) Block: Targets a nerve cluster behind the nose, ideal for cluster headaches and severe migraines.
- • Trigeminal Nerve Block: Addresses the trigeminal nerve, closely linked to migraine pain.
The growing popularity of these non-pharmacological, minimally invasive options stems from their ability to offer targeted pain relief without the systemic side effects associated with oral medications. They are quick procedures, typically performed in a clinic with minimal discomfort and downtime, and can significantly reduce dependency on conventional medications. These techniques are particularly beneficial for individuals with chronic headaches, offering relief that can last for weeks or even months. The emergence and increasing adoption of these therapies are crucial for expanding the therapeutic landscape, offering hope for improved quality of life and reduced medication burden, thereby supporting a more personalized and patient-centered approach to migraine care in India.
5.Prescription Trends in Migraine Management Across India
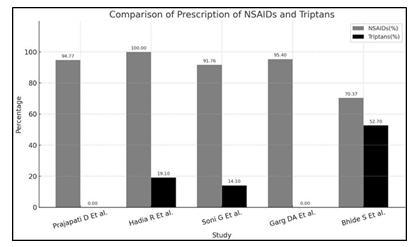
While awareness of available treatment modalities is essential, understanding the prevailing prescription trends across the nation is equally critical for effective migraine management. To this end, we analyzed data from five independent studies conducted at various centers across India, aiming to identify commonly adopted pharmacological approaches.
Acute Treatment Patterns
NSAIDs were the most commonly prescribed drugs for acute migraine attacks[35,36,37,38,39], with some studies reporting usage in 100% of patients[36]. Naproxen emerged as the most frequently used NSAID[35,36,37], with prescription of other NSAIDs like Paracetamol, Etoricoxib, and Indomethacin being comparatively less common. The prescription of triptans was notably low across most studies[35,38], with a few exceptions[39], warranting further investigation into the underlying causes of this underutilization. Rizatriptan was found to be the most common triptan prescribed [36,39]. Fixed-dose combinations (FDCs), particularly that of Naproxen and Domperidone[35,36,37], were also widely employed as first-line treatments.
Preventive Therapy Trends
Preventive treatment strategies showed considerable variation across centers. However, tricyclic antidepressants (TCAs)[36,37,38], Propranolol [37,38], and Flunarizine [35] consistently appeared as the most commonly prescribed prophylactic agents.
Polypharmacy Concerns
A trend toward polypharmacy was observed in nearly all studies, with the average number of drugs prescribed per patient ranging from 2.59 to 3.89[35,36,37,38,39]. While this may be justified by the need to manage multiple aspects of the condition-such as acute pain, associated symptoms like nausea, long-term prevention, and comorbidities, it raises concerns regarding potential drug-drug interactions, increased risk of adverse effects, and reduced patient adherence.
6. Challenges in Migraine Diagnosis, Treatment Access, and Adherence in India
Despite the significant burden of migraine in India and the availability of various treatment options, several systemic and sociocultural challenges impede effective diagnosis, treatment access, and patient adherence.
Gaps in Healthcare Professional Knowledge, Attitude, and Practice (KAP)
Migraine remains widely underdiagnosed and undertreated in India, particularly in low-resource settings, partly due to fragmented healthcare infrastructure and limited awareness among healthcare professionals (HCPs).[1] A study conducted in Eastern India revealed significant gaps in HCPs' knowledge, attitude, and practice regarding migraine management:
- • Knowledge: While moderate (65%) knowledge was observed regarding migraine, only 65% of HCPs correctly identified the International Classification of Headache Disorders-3 (ICHD-3) criteria, and a mere 40% were aware of triptans as a first-line therapy for migraine.[1] This indicates a lack of familiarity with evidence-based guidelines and crucial acute therapies.
- • Attitude: HCPs generally held positive attitudes, with 72% acknowledging migraine as a serious condition.[1]
- • Practice: Despite positive attitudes, practice was suboptimal, with only 58% adhering to guideline-recommended practices.[1] This disconnect between attitude and practice is a global phenomenon, often attributed to factors like time constraints and patient preferences.[1]
A stark specialist vs. non-specialist divide was evident: neurologists were 3.45 times more likely to follow optimal practices compared to General Practitioners (GPs).[1] GPs showed a higher reliance on NSAIDs (70% of GPs vs. 35% of neurologists) and often lacked confidence in managing complex migraine cases, leading to underuse of prophylactic agents.[1] Furthermore, disparities between government and private sector practitioners were observed, with government HCPs showing lower awareness of ICHD-3 diagnostic criteria (48% vs. 62% for private HCPs) and being less likely to prescribe triptans (25% vs. 45% for private HCPs).[1] These findings suggest systemic inequities, possibly due to outdated drug formularies and high patient loads in public facilities.[1]
The study identified several barriers to optimal migraine management, ranked by their mean score (1-5):
- Lack of time for counseling (mean score 4.2/5).[1]
- Limited access to prophylactics (mean score 3.9/5).[1]
- Patient preference for analgesics (mean score 3.7/5).[1]
- Resource constraints, such as a lack of MRI access.[1]
- Patient non-compliance due to cost.[1]
Sociocultural Barriers and Stigma
Migraine is not only under-recognized but also heavily stigmatized in India, particularly in rural areas where its prevalence is notably high (14.1% to 25.2%).[6] This stigma has profound consequences, leading to social isolation, decreased self-esteem, and a reluctance among individuals to seek medical help, thereby exacerbating the disease burden.[6] The "invisible nature" of migraine-its episodic pattern and the common misconception that it is "just a headache"-contributes significantly to its stigmatization.[6] Cultural factors and traditional beliefs prevalent in rural settings can further amplify this stigma, directly impacting treatment-seeking behavior and overall disease management.[6]
Beyond stigma, broader socioeconomic factors contribute to health disparities. Individuals with lower socioeconomic status, lower educational levels, or those from marginalized communities often experience worse health outcomes and reduced access to care.[8,40] This creates a complex interplay where stigma, often deeply rooted in cultural perceptions and a lack of public awareness, actively deters individuals from seeking necessary medical attention. This issue is further compounded by socioeconomic barriers, such as the cost of treatment or travel to healthcare facilities, and systemic healthcare inequities, including a shortage of specialists and limited resources in rural areas.[1,8] The result is a significant portion of the population suffering from undertreated or untreated migraine, leading to increased disability and substantial economic losses at both individual and societal levels.[3,5] Therefore, effective interventions must be culturally sensitive and address both the societal perception of migraine and the structural barriers that hinder access to appropriate care.
Healthcare System Disparities
Variations within national healthcare systems significantly impact headache management, and the introduction of costly innovative drugs further widens existing gaps in access.[8] Public healthcare systems in India are frequently underfunded, resulting in a lack of standardized care, insufficient education among staff, and limited access to highly specialized centers.[8] This situation exacerbates the challenge of providing optimal migraine care, especially in a country where a large proportion of the population resides in rural areas with limited access to specialized neurological care [1]. Despite advancements in migraine treatment, such as the development of CGRP inhibitors, access to these therapies remains constrained by factors including medication availability, regulatory approval, financial coverage, and the expertise of healthcare providers.[8] This represents a critical "last mile" problem in healthcare delivery: even highly effective treatments or well-established guidelines may not reach the majority of affected individuals due to systemic underfunding, fragmented infrastructure, and a severe shortage of neurologists [1,6,8]. Telemedicine has been identified as a potential solution to improve health equity by expanding access to headache care, reducing lengthy waiting times, and eliminating extensive travel, particularly for patients in underserved areas where staff shortages are prevalent.[8] Given that India contributes the largest absolute burden of headache disorders in South Asia[3], addressing these systemic disparities through comprehensive policy reforms is paramount. Such reforms should focus on enhancing drug accessibility, strengthening primary care infrastructure, and leveraging digital health solutions to bridge geographical and socioeconomic gaps, ultimately moving towards more equitable and effective migraine care for all.
7. Recommendations and Future Research Directions
Addressing the burden of migraine in India requires concerted public health initiatives and targeted research efforts to bridge existing gaps and improve patient outcomes.
Identified Research Gaps and Priorities
Despite the significant burden of migraine in India, there remains a notable research gap in fully understanding headache disorders in South Asia, particularly when utilizing recent comprehensive data such as the Global Burden of Disease (GBD) 2021 study.[3,41] A critical deficiency is the lack of large-scale, longitudinal studies and neuroimaging data specific to the Indian population, which hinders a complete understanding of the long-term cognitive consequences of migraines in this demographic.[42]
To address these gaps and improve migraine care in India, several research priorities have been identified:
- • Culturally Sensitive Interventions: Developing and evaluating community-based anti-stigma initiatives and support services that are culturally appropriate for diverse Indian populations.[6]
- • Accessibility Disparities: Conducting studies to explore and quantify disparities in migraine care accessibility between rural and urban areas, and among different socioeconomic groups.[1]
- • Patient Perspectives: Investigating patient perspectives on treatment barriers and preferences to inform patient-centered care models.[1]
- • Traditional and Complementary Therapies: Rigorously evaluating the efficacy and safety of natural supplements and complementary therapies, such as specific Ayurvedic formulations (e.g., Ayush M-3) and Yoga, through high-quality clinical studies [9,26].
- • Intrinsic Factors: Further research into the genetic, epigenetic, metabolic, neurological, and psychological factors contributing to migraine in the Indian context is needed to develop targeted therapies.[9]
- • Customized Healthcare Interventions: Developing and testing healthcare interventions that are specifically tailored to the unique needs and cultural context of the Indian population, rather than relying solely on research conducted in high-income countries.[42]
The consistent emphasis on the unique challenges and cultural contexts in India—such as the high prevalence in rural areas, the impact of stigma, the widespread use of traditional practices, and specific local triggers-highlights that generic global guidelines or treatment approaches may not be entirely effective or applicable.[1,6,40,42] Therefore, there is an urgent need for India-specific research-encompassing epidemiological studies, clinical trials, and qualitative research-to generate the evidence base necessary for developing effective, culturally appropriate interventions and national policies. This will lead to more effective and equitable migraine care across the country.
Policy Recommendations
Addressing the complex burden of migraine in India necessitates a multi-pronged policy approach to drive systemic change. The identified challenges, including knowledge and practice gaps among healthcare professionals, deficiencies in drug information, sociocultural stigma, and healthcare access disparities, demand coordinated policy actions.
Key policy recommendations include:
- • Education and Training: Implementing mandatory Continuing Medical Education (CME) programs for healthcare professionals, with a strong focus on the International Classification of Headache Disorders-3 (ICHD-3) criteria and evidence-based prophylactic therapies. Such programs are crucial for reducing existing knowledge gaps and improving adherence to best practices.[1]
- • Drug Accessibility: Taking proactive steps to include essential migraine medications, particularly triptans and newer CGRP inhibitors, in state essential drug lists. This measure would significantly enhance equity in access to effective treatments, especially in underserved regions where affordability and availability are major barriers.[1]
- • Digital Solutions: Leveraging mobile health (mHealth) tools for symptom tracking, patient education, and clinical decision support. Digital solutions can effectively mitigate time constraints faced by HCPs and expand access to care, particularly in rural and remote areas where physical access to specialists is limited.[1,8]
- • Integrated Care Models: Fostering stronger collaboration and establishing clear referral networks between primary care settings and tertiary specialized centers. This integration would ensure that patients receive appropriate care at different levels, improving the continuum of migraine management.[1]
- • Integration into National Health Programs: Integrating migraine management into existing national non-communicable disease (NCD) programs. This would elevate migraine's status as a significant public health issue, facilitating dedicated resource allocation, screening, and management strategies at a national level.[1]
These proposed policy recommendations form a comprehensive strategy aimed at transforming migraine management in India. Their implementation can lead to a significant paradigm shift, transitioning from fragmented and undertreated care to a more standardized, accessible, and patient-centered system. This will not only improve individual patient outcomes and quality of life but also substantially reduce the overall public health and economic burden of migraine across the nation.
8. Conclusion
Migraine poses a substantial and growing public health challenge in India, characterized by high prevalence, significant disability, and considerable socio economic impact. The current treatment landscape is diverse, encompassing conventional pharmacological approaches (acute and preventive), traditional Indian systems of medicine like Ayurveda and Unani, and crucial lifestyle and dietary modifications. While conventional therapies offer effective symptom relief and prevention, their optimal utilization is hampered by deficiencies in drug information and knowledge gaps among healthcare professionals. Traditional systems and complementary therapies, rooted in holistic principles, offer culturally resonant and effective adjuncts, particularly in stress management and personalized care. Despite these varied approaches, migraine remains widely underdiagnosed and undertreated, exacerbated by pervasive socio-cultural stigma, socioeconomic disparities, and systemic weaknesses within the healthcare infrastructure. The "invisible" nature of migraine often leads to its neglect in policy and resource allocation, perpetuating a cycle of inadequate care.
To address these multifaceted challenges and improve migraine management in India, the following recommendations are critical:
- • Strengthen Healthcare Professional Training
- • Improve Drug Information and Accessibility
- • Combat Stigma through Culturally Sensitive Awareness
- • Prioritize India-Specific Research
- • Promote Integrative Care Models
- • Leverage Digital Health Solutions
By adopting these comprehensive and integrated strategies, India can move towards a more robust, equitable, and patient-centered approach to migraine management, significantly alleviating the burden of this debilitating condition nationwide.
References
- Kumar C, Rana A, et al. Assessment of knowledge, attitude, and practice towards migraine among healthcare professionals in Eastern India. Healthcare Bulletin (2025): 3324.
- Srinivasan AV, Bhanu K. A Comparative Systematic Review and Meta-analysis of Amitriptyline with Propranolol and Flunarizine for the Prophylaxis of Migraine Headache. J Assoc Physicians India 73 (2025): e1.
- Satapathy P, Chauhan S et al. Trends in migraine and tension-type headaches in South Asia: findings from the Global Burden of Disease Study 2021 (1990–2021). Front Neurol 15 (2025): 1514712.
- Patel A, Pathak M, et al. Migraine - Recent Developments and Future Opportunities. ResearchGate (2024).
- Krishnan A, Chowdhury D, Duggal A, et al. Headache-attributed burden and a health-care needs assessment in Delhi and National Capital Region of India: estimates from a cross-sectional population-based study. J Headache Pain 26 (2025): 106.
- Shukla S, Joshi DA, et al. Prevalence and consequences of stigma associated with migraine in a rural Indian headache clinic. Rural Neuropractice (2025).
- Migraine and Headache Awareness Month. American Migraine Foundation (2025).
- Raffaelli B, Rubio-Beltrán E, Cho SJ, et al. Health equity, care access and quality in headache – part 2. J Headache Pain 24, 167 (2023).
- Abo-Elghiet F, Elosaily H, Hussein DK, et al. Bridging Gaps in Migraine Management: A Comprehensive Review of Conventional Treatments, Natural Supplements, Complementary Therapies, and Lifestyle Modifications. Pharmaceuticals 18 (2025): 139.
- Diener H-C, Förderreuther S, Kropp P, et al. Treatment of migraine attacks und preventive treatment of migraine, S 1 guideline, 2022, DGN and DMKG, in: Deutsche Gesellschaft für Neurologie (Pub.), Guidelines for diagnosis and treatment in neurology (2022).
- Tata 1mg. Migraine Drugs. 1mg.com.
- Singh S, Srinivasan AV, Banerjee TK, et al. Indian Consensus on the Role of Amitriptyline in Migraine Prophylaxis. Cureus 16 (2024): e54270.
- Silberstein SD, Holland S, Freitag F, et al. Evidence-based guideline update: Pharmacologic treatment for episodic migraine prevention in adults: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 78 (2012): 1337-1345.
- Chowdhury D, Chaudhuri JR, Ghosh P, et al. Efficacy and Tolerability of Erenumab for Prevention of Episodic Migraine in India. Ann Indian Acad Neurol 25 (2022): 433-440.
- Indian Health Service. National Pharmacy and Therapeutics Committee Formulary Brief: Migraine Prevention. IHS.gov. (2019).
- Ashina M, Dolezil D, Bonner JH, et al. A phase 2, randomized, double-blind, placebo-controlled trial of AMG 301, a pituitary adenylate cyclase-activating polypeptide PAC1 receptor monoclonal antibody for migraine prevention. Cephalalgia 41 (2020): 33-44.
- Haridas MP, Tripathy A, Maiti R, Srinivasan A. Efficacy and Safety of Anti-CGRP Monoclonal Antibodies in Prevention of Chronic Migraine: A Bayesian Network Meta-analysis. Clin Psychopharmacol Neurosci 22 (2024): 23-32.
- Karlsson WK, Ostinelli EG, Zhuang ZA, et al. Comparative effects of drug interventions for the acute management of migraine episodes in adults: systematic review and network meta-analysis. BMJ 386 (2024): e080107.
- Pozo-Rosich P, Ailani J, Ashina M, et al. Atogepant for the preventive treatment of chronic migraine (PROGRESS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 402 (2023): 775-785.
- Thangaraju P, Mahesh K, Venkatesan S. Information on migraine drugs in commonly available Indian drug information sources - Whether we satisfied the community needs? Indian J Pharmacol 54 (2022): 216-220.
- Naram S, Gawali K, Parekh H. A Case Study of Successful Ayurveda Management in the Patient of Migraine (Ardhavabhedaka) and Motion Sickness. Int J Ayurveda Pharma Res 11 (2023): 35-41.
- Patil G, Patil S, Hosur P. Ayurveda management of migraine - a case report. J Ayurveda Integr Med 15 (2024): 100983.
- Soman A, Venkatram S, Chikkanna U, et al. Ayurveda for management of migraine: A narrative review of clinical evidence. J Family Med Prim Care 11 (2022): 4228-4235.
- Bhatt P, Vaghela DB. Efficacy of Ayurvedic Medication on Anxiety-induced Migraine: A Case Study. J Ayurveda Integr Med Sci 9 (2024): 3553.
- Vaidya PB, Vaidya BS, Vaidya SK. Response to Ayurvedic therapy in the treatment of migraine without aura. Int J Ayurveda Res 1 (2010): 30-6.
- Chaudhary S, Khanduri S, Mata S, et al. Randomized double-blind placebo controlled multicentric clinical trial of Ayush M-3 in the management of migraine- A study protocol. J Ayurveda Integr Med 16 (2025): 101054.
- Bhatt P, DB Vaghela, Efficacy of Ayurvedic Medication on Anxiety-induced Migraine: A Case Study. J Ayu Int Med Sci 9 (2024): 282-286.
- Khan MM, Khan S, et al. Unani insights on migraine: psychological and holistic care. ResearchGate (2025).
- Singh S, Singh R, Singh S, et al. Effect of yoga as add-on therapy in migraine (CONTAIN): A randomized clinical trial. Neurology 94 (2020): e2397-e2406.
- Kachhadia MP, Khalil ZM, Shah S, et al. Role of Yoga as Adjunctive Therapy for Migraines: A Narrative Review of the Literature. Cureus 15 (2023): e48434.
- Nayar D, Mahapatro M, Nayar P. Role of Yoga as an Adjunct in the Management of Migraine Headache-Current Status and Future Indications. Int J Yoga 15 (2022): 12-18.
- Ramasamy B, Karri M, Venkat S, GA. Clinical profile and triggers of migraine: an Indian perspective. Int J Res Med Sci 7 (2019): 1050-1054.
- Chowdhury D, Singh S, Singh R, et al. Efficacy and tolerability of erenumab for prevention of episodic migraine in India. ResearchGate (2022).
- Wahab S, Kataria S, Woolley P, et al. Literature Review: Pericranial Nerve Blocks for Chronic Migraines. Health Psychol Res 11 (2023): 74259.
- Prajapati D, Patel M, Dharamsi A, et al. Assessment of prescription trends, quality of life, and adverse drug reactions in migraine management: A cross-sectional study at a tertiary care teaching hospital. J Popul Ther Clin Pharmacol 31 (2024): 471-481.
- Hadia R, Kapadi V, Parekh K, et al. A cross sectional observational study to assess clinical characteristics, prescription pattern and health related quality of life in migraine patients at tertiary care teaching hospital. J Young Pharm 14 (2022): 314-321.
- Soni G, Vohra A, Jain S, et al. Current trends in prescribing pattern of anti-migraine drugs in patients of migraine at a tertiary care teaching hospital. Int J Med Med Res 7 (2021): 5-14.
- Garg DA, Patra RC, Mishra A. A retrospective study on prescription pattern of migraine management: An institutional experience. Int J Eng Sci Invent Res Dev 10 (2023): 1-4.
- Bhide S, Verma P, Ravat S, et al. A study of drug prescription patterns, disease-therapy awareness and of quality of life among patients with migraine visiting a tertiary care hospital in Mumbai, India. Int J Basic Clin Pharmacol 12 (2023): 855-860.
- Armand CE, Pace A, et al. Update on Underrepresented Populations in Headache Medicine: What Is Known and Care Considerations. Practical Neurology 22 (2023): 32002.
- Xu R, Zhang R, Dong L, et al. An analysis of the burden of migraine and tension-type headache across the global, China, the United States, India and Japan. Front Pain Res (Lausanne) 6 (2025): 1539344.
- Choudhary AK. The Relationship between Migraine and Cognition: A Narrative Review in Indian Context. Med Res Arch 12 (2024): 6011.


 Impact Factor: * 3.3
Impact Factor: * 3.3 Acceptance Rate: 74.39%
Acceptance Rate: 74.39%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 