Acute Ischemic Stroke Patients for Alteplase or Medical Care Alone or Intervention with/without Alteplase in Palestine (AIS-AMI Palestine)
Mohammed Habib* #, Majed Alshounat #, Mohammed Salama#
# Cardiology Department, Alshifa Hospital- Gaza-Palestine
*Corresponding author: Mohammed Habib, Head of Cardiology Department, Alshifa Hospital- Gaza-Palestine.
Received: 11 November 2022; Accepted: 21 November 2022; Published: 29 November 2022
Article Information
Citation: Mohammed Habib, Majed Alshounat, Mohammed Salama. Acute Ischemic Stroke Patients for Alteplase Alone or Medical Care Alone or Intervention with/without Alteplase in Palestine (AISAMI Palestine). Cardiology and Cardiovascular Medicine 6 (2022): 523-528.
View / Download Pdf Share at FacebookAbstract
Background: Stroke is the most common cause of permanent disability and the third most common cause of death in Palestine. We aimed to examine patterns of stroke presentation, causes, management, and outcomes at the largest public Mistry of health hospitals in Palestine.
Methods: Comprehensive data from all patients with acute ischemic stroke who admitted to alshifa hospital between November 2021 and July 2022 and treated with alteplase alone or endovascular intervention with or without alteplase were prospectively collected and compare with acute ischemic stroke patients who treated with medical care alone at Palestine medical complex hospital at 2018. Acute ischemic stroke presentation patterns, in-hospital evaluation and management, mortality, and morbidity were evaluated.
Results: Medical care alone group: 138 patients with acute ischemic stroke, mean age was 65 ±14 years and 49% were women. most of patients received antiplatelet therapy (98%), although none received thrombolysis. Only 17% received physical therapy evaluation. In-hospital mortality was 13%, modified ranking score 0-2 was in 44 patients (32%). Endovascular intervention with/without alteplase group: 56 patients with acute ischemic stroke. The mean age was 61 ±12 years and 41 % were women. All patients received brain computed tomography scans, although few received other investigations such as carotid Doppler (13 %). Most patients with ischemic stroke received antiplatelet therapy (99%), although 39 patients (70%) received thrombolysis. Only 61 % received physical therapy evaluation. In-hospital mortality was 7 %. the modified ranking score 0-2 was in 32 patients (57%).
Conclusions: This study conducted in Palestine showed that among patients with acute ischemic stroke, functiona
Keywords
<p>Ischemic Stroke; Endovascular Therapy; Tissue Plasminogen Activator (tPA)</p>
Article Details
1. Introduction
Stroke is one of the leading causes of death and disability worldwide. The tissue plasminogen activator (tPA) is the only therapeutic agent approved to treat patients with acute ischemic stroke [1]. According to the American Heart Association/American Stroke Association Guidelines for the Early Management of Patients With Acute Ischemic Stroke the clinical benefits of tPA manifest when the agent is administered within 4.5 hours of stroke onset [2]. However, intravenous (IV) tPA administration is associated with increased occurrence of intracranial hemorrhage [3-5]. Each year in the Palestine, approximately 5200 people have an acute ischemic stroke. About 12% mortality related to stroke [6] On average, every 75 minutes, someone in the Palestine has a stroke and every 6 hours one Palestinian died from stroke. Before modern treatments at Palestine in-hospital mortality between 1-5 days was 13% and among survivors, more than 60% on patients had moderate-to-severe neurologic deficits [7]. The introduction of intravenous alteplase in 1995 led to substantial improvement in outcomes [8]. More recently, effective mechanical thrombectomy has radically altered initial management in many patients. The thrombolytics treatment with tPA and mechanical thrombectomy was started in Gaza strip for acute ischemic stroke in November 2021.
2. Methods
2.1 Study Design and Settings
Four major healthcare providers exist in Palestine: the Palestinian Ministry of Health, Palestinian nongovernmental organizations, the United Nations Relief and the private sector. Secondary and tertiary care are mostly provided through the Ministry of Health in 12 hospitals distributed in the West Bank and in 13 hospitals in Gaza strip for old treatment strategy we purposively sampled 2 of the largest Ministry of Health hospitals in the West Bank. Palestine Medical Complex Hospital in Ramallah City is located in the Center and had 231 beds, serving a population of 338 383 residents. Al- Watani Hospital in Nablus City is located in the North and has 255 beds, serving a population of 372 621 residents.
For new treatment strategy the sampled is collected from the largest hospital in Palestine and located in Gaza city and has 600 beds, serving 722350 residents.
At the time of data collection, acute stroke was managed by internal medicine specialists and a neurologist at the Palestine Medical Complex Hospital and in Alshifa hospital. Al-Watani Hospital did not have a neurology specialist at the time of data collection and acute stroke was managed by internal medicine specialists. Data were collected between September 2017 and May 2018 from Palestine Medical Complex Hospital and between February 2018 and May 2018 from Al-Watani Hospital. And between November 2021 and July 2022 from Alshifa Hospital.
The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
The present prospective registry study involved all patient with acute ischemic stroke who admitted to alshifa hospital between November 2021 and July 2022 and treated with alteplase alone or endovascular intervention with/without alteplase were prospectively collected (new treatment strategy) And compare with acute ischemic stroke patients who treated with medical care alone at West Bank (Palestine medical complex hospital and Alwatani hospital) at 2018 (before beginning of administration of IV tPA or mechanical thrombectomy in Palestine) (old treatment strategy).
The present prospective nonrandomized study involved all patient with acute ischemic stroke who admitted to alshifa hospital between November 2021 and July 2022 and treated with alteplase alone or endovascular intervention with/without alteplase were prospectively collected (new treatment strategy) And compare with acute ischemic stroke patients who treated with medical care alone at Palestine medical complex hospital at 2018 (old treatment strategy).
2.2 The Old Treatment Strategy (Medical Care Alone) [7]
involved 138 patients , prospective hospital-based registry at hospitals in the West Bank of Palestine, the stroke management including ( antiplatlet, Statin, antihypertensive, antilipid) in the absence of thrombolytic therapy and endovascular intervention.
2.3 The New Treatment Strategy ( Endovascular Intervention with or without tPA or Tpa Alone)
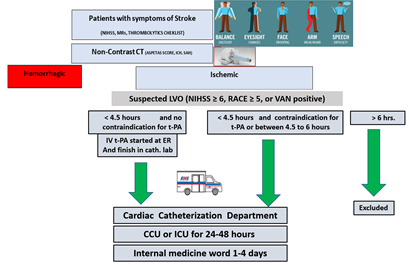
Eligibility criteria included receipt of intravenous t-PA (0.6 mg per kilogram), with 15% as a bolus and the remainder infused over a 1-hour period (maximum dose, 60 mg) within 4.5 hours after symptom onset and moderate-to-severe neurologic deficit according to the National Institutes of Health Stroke Scale (defined as an NIHSS score ≥ 6). For patients with suspicion of large vessel occlusion (NIHSS ≥ 6 or RACE score ≥ 5 or VAN positive) [8-9], the angiographic procedure had to begin before finishing the T-PA infusion and be completed within 6 hours (5-7 hours) after the onset of stroke. Or if t-pa contraindicated the patient transfer directly to cardiac catheterization laboratory. Participants who had no angiographic evidence of a treatable occlusion received no additional treatment, and those with a treatable vascular occlusion received endovascular intervention with an approach chosen by the site (i.e., thrombectomy with aspiration catheter or endovascular delivery of Intraarterial alteplase (maximum dose, 30 mg) by means of the standard microcatheter). Heparin infusion was started intravenously with a 5000-unit bolus, followed by an infusion of 1000 units per hour if endovascular therapy more than 1 hour, and was discontinued at the end of the procedure. CT was performed at baseline, at 24 hours (±6 hours), and if there was a neurologic decline. Written informed consent was obtained from the patient. (Figure 1). The primary outcome was the score on the modified Rankin scale assessed and death at the time of hospital discharge.
CCU: coronary care unit, ICU: intensive care unit, NIHSS: National Institutes of Health Stroke Scale, RACE: Rapid Arterial occlusion Evaluation (RACE) Scale for Stroke, VAN: Stroke vision, aphasia, neglect (VAN) assessment
2.4 Statistical Analysis
Continuous data are reported as means ± SD where appropriate. Categorical data are presented as absolute values and percentages. Statistical analyses were performed by X square test to comparison the primary outcome(modified Rankin scale 0-2 and death) between medical care alone and new treatment strategy involved tPA and endovascular intervention or between medical care alone and a P-value <0.05 was considered significant.
3. Results
3.1 The old Treatment Strategy [7]
All patient received head computed tomography scans, although few received other investigations such as magnetic resonance imaging (8%) or carotid Doppler (4%). Most patients with ischemic stroke received antiplatelet therapy (98%), although none received thrombolysis. Only 17% received physical therapy evaluation. In-hospital mortality was 12%, 23% of patients had at least 1 poststroke complication, and the median modified Rankin Score at discharge was 4 (interquartile range, 2–5). At discharge, the median modified Rankin Scale score 0-2 was in 44 patients (32%), moderate to severe disability were seen in 61% of patients. and 13 % of patients died during the hospital stay. We also identified several gaps in acute stroke management including absence of thrombolytic therapy and endovascular intervention, low rates of diagnostic vascular and cardiac imaging and limited rehabilitation services.
3.2 The New Treatment Strategy
Total patients from November 2021 and July 2022 who admitted to alshifa hospital and treated by intravenous tPA and/or endovascular treatment was 56 patients, with mean age was 61±12 years and 41 % were women. Cause of stroke: Cardio-embolism: 26 (46%), Intracranial atherosclerosis: 5 (9%) Ipsilateral extracranial ICA obstruction: 4 (7%),Undetermined: 21(38%), the median ASPECTA score was 7-10 [9]. Symptomatic intracranial hemorrhage within 48 hours was seen in 4 (7%), intrahospital death was seen in 4 cases (7%), 3 cases in t-PA (16%), 1 (3%)case in endovascular intervention with tPA (3%)and no mortality in intervention alone . Modified Rankin scale score of 0 to 2 at discharge in 29 patients (52%), 25 patients in intervention group and 7 in patients who received alteplase. Patients divided into 2 groups (medical care ) plus:
3.2.1 Intervention with/out tPA (38 patients 68%): total of 17 (30%) patients were assigned to undergo endovascular treatment and 21 (38 %) were assigned to receive combination therapy with intravenous alteplase and endovascular treatment.
3.2.2 Alteplase alone (18 patients , 32%): patients receive intravenous alteplase alone.
Baseline characteristics of the patients in old and new treatment strategy in acute ischemic stroke in table 1.
|
Characteristics |
New treatment strategy (N: 56 patients) |
Medical care alone (N:138 patients) |
|
Age (mean) |
61±12 years |
65±14 years |
|
Male |
33 (59%) |
72 (52%) |
|
Median NIHSS score |
Mild (NIHSS 0–6):12 ( 21%) |
Mild (NIHSS 0–6):53 ( 38%) |
|
Moderate(NIHSS 7–12): 29 (52 %) |
Moderate (NIHSS 7–12) : 41 (30%) |
|
|
Severe (NIHSS>13) :15 ( 27 %) |
Severe (NIHSS 13–20) :44 ( 32 %) |
|
|
Medical history |
||
|
Previous ischemic stroke |
11 (20%) |
54 (39%) |
|
History of atrial fibrillation |
19 (34%) |
26(19%) |
|
History of diabetes mellitus |
21 (37%) |
63 (46%) |
|
History of hypertension |
29 (52%) |
91(66%) |
Table 1: Characteristics of the Patients at Baseline.
NIHSS: National Institutes of Health Stroke Scale.
3.3 Primary Outcome (Discharge Outcomes):
Modified ranking score between 0-2 was more in new treatment strategy was seen in 32 (57%) of patients in new treatment strategy and in 44 patients (32%) in old treatment strategy (P:001) , intra-hospital death in 4 (7%) of patients in new treatment strategy and in 18(13%) of patients in old treatment strategy (P:0.2).
|
New treatment strategy |
Medical care alone |
P value |
|
|
mRS 0-2 |
32 |
44 |
0.001 |
|
Intra hospital death |
4 |
18 |
0.2 |
Table 2: Primary outcome in new and old treatment strategy.
mRS : Modified Ranking Score.
3.4 Comparison between Intervention with/out tPA and old Treatment Strategy
modified ranking score between 0-2 was seen in 25(66%) of patient who undergo endovascular intervention with or without tPA and in 44 (32%) of patient with old treatment strategy (P:0001) and intra-hospital death in one patients mortality who undergo endovascular intervention with tPA and in 18 (13%) of patients with old treatment strategy(P:0027).
|
Intervention with/out tPA |
Medical care alone |
P value |
|
|
mRS 0-2 |
25 |
44 |
0.0001 |
|
Intra hospital death |
1 |
18 |
0.0027 |
Table 3: Comparison between Intervention with/out tPA and old treatment strategy.
mRS : Modified Ranking Score, tPA: Alteplase
3.5 Comparison between tPA and medical care alone
No significant difference between mRS 0-2 or mortality at hospital discharge between two groups.
4. Discussion
In this prospective hospital-based registry at public hospitals in the West Bank and Gaza of Palestine, we observed high rates of discharge disability and mortality. We also identified several gaps in acute stroke management including absence of thrombolytic therapy, low rates of diagnostic vascular and cardiac imaging, and limited rehabilitation services at 2018 in west bank public hospitals. But at 2022 and after starting with intravenous alteplase and endovascular intervention in alshifa hospital in Gaza of Palestine we observed improvement of disability and significant reduction of intra-hospital death when we treatment acute ischemic stroke by combination of alteplase and endovascular treatment. The benefit of intravenous alteplase is time-dependent. In a meta-analysis of nine randomized, controlled trials [10], 32.9% of the patients in the alteplase group, as compared with 23.1% of the patients in the control group, had a favorable 3-month outcome (defined as a modified Rankin scale score of 0 or 1) when treatment was administered within 3 hours after the onset of stroke, the corresponding rates were 35.3% and 30.1% when treatment was administered between 3 and 4.5 hours after onset. Large intracerebral hemorrhage occurred in 6.8% of the patients in the alteplase group and in 1.3% of those in the control group. The overall outcomes, as assessed by the modified Rankin scale, among the patients in the alteplase group reflected the deleterious effects of hemorrhage along with the beneficial effect on ischemic stroke recovery. In our study only 18 patients had received alteplase alone, and totally 3 patient died, 2 patients of these died because of large intracerebral hemorrhage and one died because of administration of alteplase in large ischemic stroke with NIHSS score was 26. Pooled data from five randomized, controlled trials showed that the percentage of patients who had a modified Rankin scale score of 0 to 2 at 90 days was higher among those who underwent mechanical thrombectomy than among those who did not (46.0% vs. 26.5%) [11]. A randomized, controlled noninferiority trial that compared mechanical thrombectomy alone with the combination of intravenous alteplase and mechanical thrombectomy in patients eligible for both interventions met its large prespecified noninferiority margin (the modified Rankin scale score with thrombectomy alone at 90 days was less than 20% worse than that with combined therapy); the adjusted odds ratio was 1.07 [12] the Direct aspiration as a first approach for thrombectomy has been shown to be noninferior to stent retrievers [13]. In our trial Intervention with/out tPA was administrated in 38 patients, 17 patients were assigned to undergo endovascular treatment alone and 21 were assigned to receive combination therapy with intravenous alteplase and endovascular treatment. One patient was died after tPA because of tandem stroke and modified Rankin scale score of 0 to 2 was in 25 patient. Our results provide insight on the management and outcomes of patients with stroke in Palestine can be improve if we support new treatment strategy with intravenous tPA within 4.5 hours and endovascular intervention with 6 hours of symptoms. These results highlight 4 areas to focus on to improve acute stroke care in public hospitals: (1) develop an organized stroke unit within a geographically defined location in each hospital and identify a multidisciplinary stroke team comprising medical, nursing, physiotherapy, occupational therapy, speech therapy, and social work staff. Given the limited resources, a stroke unit may comprise a set number of beds within an already established medical unit or intensive care unit; (2) support acute thrombolysis with intravenous tissue-type plasminogen activator and endovascular intervention (3) raise awareness in the community about recognition of stroke symptoms (4) implement a pathway for early discharge planning in the hospital. Early discharge planning strategies include early assessment of discharge needs, identification of realistic rehabilitation recovery goals, involving the patient and their family in the recovery process, and early rehabilitation at home or in the community.
5. Conclusions
We describe stroke presentation, management, and outcomes in public hospitals in Palestine. Results indicate poor clinical outcomes at discharge including high mortality rates and severe disability in medical care alone, and improvement of disability and mortality by treatment of combination of intravenous alteplase and endovascular intervention.
References
- National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333 (1995):1581-1587.
- Powers WJ, FAHA MD, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 50 (2019): e344-e418
- Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 384 (2014):1929-1935.
- Lees KR, Emberson J, Blackwell L, et al. Effects of alteplase for acute stroke on the distribution of functional outcomes: a pooled analysis of 9 trials. Stroke 47 (2016): 2373-2379.
- Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after largevessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387 (2016): 1723-1731.
- Palestinian Ministry of Health. Health Annual Report Palestine 2020, obtained from the Ministry of Health's (2020).
- Khatib R, Jawaadah AM, Khammash U. Presentation, Management, and Outcomes of Acute Stroke in Palestine. J Am Heart Assoc 7 (2018): e010778.
- de la Ossa NP, Carrera D. Design and Validation of a Prehospital Stroke Scale to Predict Large Arterial OcclusionThe Rapid Arterial Occlusion Evaluation Scale. Stroke 45 (2014): 87-91.
- Teleb MS, Ver Hage A, Carte J. Stroke vision, aphasia, neglect (VAN) assessment—a novel emergent large vessel occlusion screening tool: pilot study and comparison with current clinical severity indices. J NeuroIntervent Surg 9 (2017): 122-126.
- Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-guided thrombolysis for stroke
with unknown time of onset. N Engl J Med 379 (2018): 611-622. - Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after
large-vessel ischaemic stroke: a meta-analysis of individual patient data from
five randomised trials. Lancet 387 (2016): 1723-1731. - Yang P, Zhang Y, Zhang L, et al. Endovascular thrombectomy with or without
intravenous alteplase in acute stroke. N Engl J Med 382 (2020): 1981-1993. - Turk AS III, Siddiqui A, Fifi JT, et al. Aspiration thrombectomy versus stent re-triever thrombectomy as first-line approachfor large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet 393 (2019): 998-1008.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 