Effectiveness of Telecardiology Interventions on Reducing Hospital Readmissions in Elderly Heart Failure: Systematic Review and Meta-Analysis
Ghazala S. Virk1, Sarah Hack2, Chandini Gundala3, Tanzeela Saeed4, Deep Patel5, Sai Prashanthi Varakala6, Yukesh Karki7, Venkata Avinash Ugripelli8, Marium Abid9, Binish Essani10, Muhammad Sohail S. Mirza11*
1Avalon University School of Medicine, Willemstad, Curacao, USA
2St. George’s University, Grenada, West Indies
3Vydehi Institute of Medical Sciences and Research Centre, Bangalore, Karnataka, India
4Services Institute of Medical Sciences, Lahore, Pakistan
5GMERS Medical College, Valsad, Gujarat, India
6Osmania Medical College, Hyderabad, Telangana, India
7Kathmandu Medical College, Bagmati province, Nepal
8Siddhartha Medical College, Andhra Pradesh, India
9Jinnah Medical & Dental College, Karachi, Pakistan
10Jinnah Medical and Dental College, Karachi, Pakistan
11Shandong University School of Medicine, Jinan, China
*Corresponding author: Muhammad Sohail S. Mirza, MBBS, Shandong University School of Medicine, Jinan, China, Email: drsohailmirza2024@gmail.com
Received: 31 July 2025; Accepted: 22 August 2025; Published: 01 September 2025
Article Information
Citation:
Ghazala S. Virk, Sarah Hack, Chandini Gundala, Tanzeela Saeed, Deep Patel, Sai Prashanthi Varakala, Yukesh Karki, Venkata Avinash Ugripelli, Marium Abid, Binish Essani, Muhammad Sohail S. Mirza. Effectiveness of Telecardiology Interventions on Reducing Hospital Readmissions in Elderly Heart Failure - Systematic Review and Meta-Analysis. Cardiology and Cardiovascular Medicine. 9 (2025): 368-379.
View / Download Pdf Share at FacebookAbstract
Heart failure becomes a chronic condition when the heart cannot pump blood properly. The cycle then repeats, hospitalizations are recorded for acute heart failure; interventions are sought to prevent further hospitalizations. Telecardiology interventions, such as remote monitoring and teleconsultation, were therefore proposed as a means to ramp up heart failure management and diminish the incidence of readmission. The systematic review and meta-analysis aimed to evaluate the impact of telecardiology interventions on two levels of outcome-reduction of hospital readmissions. An elaborate search was carried out in renowned bibliographic databases, namely, PubMed, Google Scholar, Cochrane Library, and Scopus, for randomized controlled trials (RCTs) and cohort studies published between 2000 and 2025. The included studies evaluated telemedicine interventions, which included mobile health applications, nurse-led telemonitoring, and teleconsultations. The primary outcome was the rate of hospital readmission; the secondary outcome measures included quality of life, patient satisfaction, and functional capacity. Meta-analysis on pooled data was done using a random-effects model for effect size estimation. Overall effect size was found to be 0.71 (95% CI: 0.31-1.11). It suggested a moderate reduction in readmissions with telecardiology interventions, though high heterogeneity (I² = 91.95%) was seen, which is due to differences in the designs of included studies, interventions, and populations. There was no significant publication bias as measured by the funnel plot and Egger's test. Risk of Bias showed variability across studies; some were low risk, and others moderate to high risk. Despite these limitations, results indicate that telecardiology may be effective in reducing hospital readmissions, although future research will be needed to better refine intervention models and patient-specific approaches.
Keywords
<p>Telecardiology; Heart failure; Hospital readmissions; Telemedicine interventions; Meta-analysis</p>
Article Details
1. Introduction and Background
Heart failure (HF) is a health imperative around the world, especially as it affects the elderly. Being one of the major causes of hospitalizations and deaths, HF prevalence increases with age and contributes to a high rate of readmission and a significant burden on healthcare systems globally [1]. HF is a condition that worsens the physical condition, degrades the quality of life, and increases the cost of health care in older people, simultaneously causing multiple hospitalizations [2]. To counter this situation, medical practitioners are starting to implement more telecardiology interventions wherein patients are treated using remote monitoring and digital technologies outside of conventional hospital facilities [3].
Telecardiology is the umbrella term for telemonitoring, teleconsultations, and mobile health applications, which allow clinical interventions to occur when timely interventions are needed, and as such, assist in better patient outcomes [4]. These can protect vital signs, offer training and monitoring on a continuous basis, and help identify deterioration in clinical status early, thereby decreasing readmission [5]. The increasing incidence of telecardiology in the clinical setting is still under scrutiny regarding its ability to prevent the readmission of patients and, more specifically, elderly heart failure patients [6].
Among the most vital indicators of the quality and cost-effectiveness of healthcare, specifically in heart failure management, is the rate of hospital readmission [7]. In the case of older patients with HF, readmission to the hospital occurs in roughly 25% of instances after discharge within the 30-day window, mostly due to the occurrence of further symptoms or lack of adequate post-discharge care [8]. It has been argued that heart failure patients discharged without sufficient follow-up measures could be at risk of accidents leading to rehospitalization, especially those above 65 years of age [9]. This accentuates the need for feasible intervention strategies to ensure continuity of care and prevent readmission [10].
Telecardiology may offer several advantages in this situation. In Ledvina's study (2021), for instance, telemedicine mechanisms were shown to reduce readmission rates for heart failure as well as the mortality rate by means of continuous monitoring and early intervention [11].
Likewise, telecardiology interventions such as telemonitoring can significantly reduce hospital readmissions among patients and improve their quality of life by monitoring patients with heart failure [12]. Thus, strong documentation of telemedicine's involvement in effective care management and reduced hospitalizations, especially for the very complex elderly patients, has been made [13].
Telecardiology has been discussed widely on patient engagement and self-management [14]. They have linked more patient-centered educational programs, remote consultations, and symptom tracking to increased compliance with prescribed treatments and optimal management of heart failure symptoms [15]. Telecardiology intervention aims at empowering the patient and enabling the patient to control their own health by minimizing unnecessary visits to the hospital. Thereby, it reduces some of the burden on healthcare facilities and contributes to reducing costs by limiting the number of unnecessary visits to the hospital [16].
However, telecardiology is not without challenges. The factors that would hinder the success of these interventions involve access to technology, patient health literacy, and telehealth program designs [17]. Nonetheless, telecardiology-commercialized and markedly promising technologies that would reduce the number of admissions and re-admissions per annum among elderly heart failure patients-now and still yield average results. Therefore, wider coverage is needed for a complete long-term appraisal. This systematic review and evidence synthesis through meta-analysis aims at understanding what is known so far about telecardiology effect on readmission reduction for elderly heart failure patients. It can help practitioners implement these interventions better in clinical practice.
2. Methods
2.1 Data Sources and Search Strategy
The study used a thorough literature search to determine how telecardiology interventions can be used to reduce hospital readmissions in elderly heart failure patients. Such electronic databases were searched: PubMed, Cochrane Library, Scopus, and Google Scholar (Table 1). The search period was limited to the studies published between 2000 and 2025 to make the current evidence available. The search was based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) to ensure transparency and replicability. To maximize the findings, keywords as well as MeSH (Medical Subject Headings) terms were applied. Keywords were such terms as telecardiology, telemedicine, telemonitoring, heart failure, hospital readmissions, elderly, and remote monitoring. These were joined with Boolean operators (AND, OR) in order to increase the specificity and sensitivity of the search. The present systematic review has encompassed the studies written in English that used human participants. Manual reference search of pertinent articles was carried out so as to reduce the chances of leaving out relevant studies.
|
Database |
Search Terms Used |
Filters Applied |
Truncations/Syntax |
|
PubMed |
"telecardiology" AND "heart failure" AND "hospital readmissions" AND "elderly" |
English, Human studies, 2000-2025 |
Boolean operators: AND, OR |
|
Cochrane Library |
"telemedicine" AND "telemonitoring" AND "hospital readmission" AND "elderly heart failure" |
English, Human studies, 2000-2025 |
Boolean operators: AND, OR |
|
Scopus |
"telecardiology" AND "heart failure" AND "readmission rates" AND "elderly" |
English, Human studies, 2000-2025 |
Boolean operators: AND, OR, Wildcards (*) |
|
CINAHL |
"Remote monitoring" AND "heart failure" AND "hospital readmission" AND "elderly patients" |
English, Human studies, 2000-2025 |
Wildcards () to account for plural/singular variations (e.g., "readmission" for "readmission" or "readmissions") |
|
Google Scholar |
"telecardiology" AND "elderly heart failure" AND "hospital readmission" AND "telemedicine" |
English, Human studies, 2000-2025 |
Boolean operators: AND, OR |
Table 1: Search strategy across databases.
2.2 Inclusion and Exclusion Criteria
The process of critical appraisal of the literature is usually directed within the framework of PICOS. This framework allows a systematic, rigorous process to select studies that directly answer the research questions (Table 2).
|
PICOS Element |
Inclusion Criteria |
Exclusion Criteria |
|
Population |
Elderly patients (≥50 years) diagnosed with heart failure, including both men and women. |
Patients under 50 years of age, or those without a confirmed diagnosis of heart failure. |
|
Intervention |
Telecardiology interventions, including telemonitoring, teleconsultation, remote monitoring, and mobile health apps. |
Studies not focused on telecardiology interventions (e.g., general telemedicine or non-remote healthcare). |
|
Comparator |
Usual care, including standard hospital or outpatient care for heart failure management; historical controls; non-randomized studies comparing telemedicine interventions to standard care. |
Studies without a clear comparison group (e.g., single-arm studies without control groups). |
|
Outcome |
Primary outcome: Hospital readmission rates. Secondary outcomes: Mortality, quality of life, patient satisfaction, functional capacity, physical performance (e.g., 6-minute walk test), clinical stability. |
Studies that do not report hospital readmission as a primary or secondary outcome. |
|
Study Design |
Randomized controlled trials (RCTs), pilot studies, cohort studies, and quasi-experimental studies. |
Case reports, editorials, and studies with incomplete or inadequate data for analysis. |
Table 2: PICOS Framework for Recent Study.
2.4. Data Extraction
Two independent reviewers utilized a pre-prepared standardized extraction form in order to abstract data in this systematic review. The data extracted included the author(s), the year of publication, the location of the study, and the type of study design. Demographic factors such as sample size, age, gender, and underlying comorbidities were noted so that the general applicability of the results could be assessed. The data on the telecardiology intervention were collected in detail, such as the type of intervention (telemonitoring, teleconsultations, remote devices), duration, and frequency of follow-up. The central measure was the hospital readmission rate, but secondary outcomes included mortality, quality of life, patient satisfaction, and compliance with the telecardiology interventions. The negative effects or any other unwanted outcomes of the intervention were noted. Where the two reviewers differed in their opinion in terms of data extraction, it was settled after discussion. In case the agreement was not reached, a third reviewer was contacted to achieve consistency and accuracy of the extraction process.
2.5. Quality Assessment
An appraisal of the quality of studies was done systematically, where instruments were matched with the study design. In the case of RCTs, Cochrane Risk of Bias 2 (RoB 2) was used, with a focus on random sequence generation, allocation concealment, blinding of participants and outcome assessors, missing data, and bias in selective reporting of results. The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of cohort studies by evaluating aspects of participant selection, group comparability, and outcome measures [18]. Any disagreement on the quality rating of the studies was solved by discussion; in case it appeared impossible to achieve the agreement, the opinion of the third reviewer was consulted.
A funnel plot was built to explore the possibility of publication bias, and asymmetry in the plot was examined, whereas the Egger regression test was used to determine small-study effects. The trim-and-fill method was also used to re-estimate the overall effect in the cases where the bias was expected. [19,20].
3. Statistical Analysis
The random-effects model was used to synthesize results of studies that had a heterogeneous experimental design, the population of participants, protocols of interventions, and outcome variables, which were used in the systematic review. The standardized mean difference (SMD) and corresponding 95 % confidence intervals were considered the primary effect measure. They were used to study the impact of telecardiology interventions on hospital readmissions and also on the secondary outcomes, like all-cause mortality and health-related quality of life. The random-effects model is more appropriate in studies dealing with different properties in the research and is able to produce a more accurate representation in the estimation of the treatment effect through a synthesis of the heterogeneity between studies. Therefore, it was adopted as opposed to the fixed-effects model. I2 statistic was used to measure the variability of included studies; the values of 25 %, 50%, and 75 % respectively, represented low, moderate, and high heterogeneity. Subgroup analyses were also performed to investigate causes of heterogeneity, e.g., methodological differences, compliance with the protocols of telecardiology interventions, and demographic characteristics of participants, e.g., age and gender. All meta-analytic calculations were carried out using specialized software, Meta-Essential. Statistical significance was set at p < 0.05.
4. Results
4.1. Study Selection
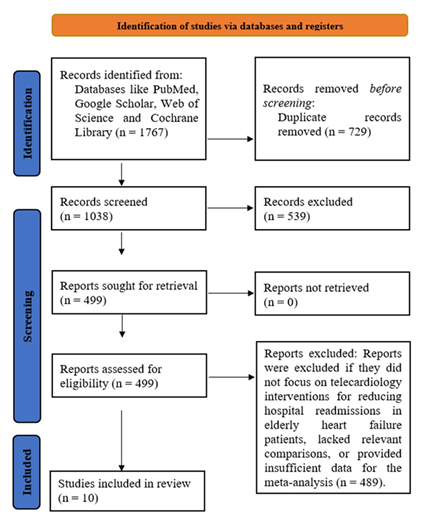
When a systematic review (meta-analysis) was conducted, the first search produced 1767 citations related to the topic, based on a variety of electronic databases and additional resources. After removing duplicates and screening for relevance, 1038 studies were assessed for eligibility. Of these, 539 were excluded because they did not specifically address telecardiology interventions or hospital readmissions in elderly heart failure patients. Following a thorough full-text review, 504 studies were further examined in detail. A total of 489 studies were excluded for not meeting the inclusion criteria, such as lacking a focus on telecardiology interventions, not reporting relevant outcomes like readmission rates, or failing to provide necessary data for meta-analysis. Ultimately, 10 clinical trials were included (Figure 1), which compared telecardiology interventions to standard care and provided sufficient data on hospital readmission rates and secondary outcomes like mortality and quality of life.
4.2 Characteristics of the included studies
The studies included in this systematic review and meta-analysis evaluate a variety of telecardiology interventions aimed at reducing hospital readmissions and improving outcomes for heart failure patients (Table 3). These studies utilize different designs, interventions, and populations, providing a comprehensive view of the effectiveness of telemedicine in heart failure management. Most studies focus on remote monitoring, teleconsultations, and telecardiology programs, with some combining additional interventions such as exercise training, education, and psychological support. The populations primarily consist of elderly or high-risk heart failure patients, often those recently hospitalized or with multiple chronic conditions. Primary outcomes across the studies include hospital readmissions, emergency department visits, and functional capacity, with secondary outcomes such as quality of life, patient satisfaction, and healthcare utilization. The study designs include RCTs, cohort studies, and non-controlled trials, whereas the follow-up covers a period of three months to over a year. The diversity of interventions and results of the studies will provide meaningful information on the role of telecardiology in the treatment of heart failure and the resulting decrease in hospital readmission.
Table 3: Summary of studies involved in the study.
4.3 Quality assessment
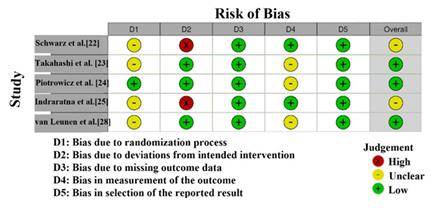
As shown in Figure 2, RoB assessment by Cochrane suggests the heterogeneity of the methodological quality of the trials used in this meta-analysis. The risk is low in most domains in both studies of Scalvini et al. [21]and Takahashi et al. [23], which implies that randomization procedures are rigorous, there is an appropriate blinding, and outcome data are reported precisely. It supports the reliability of the findings regarding the effectiveness. On the contrary, the overall risk in Piotrowicz et al. [24] is quite low, confirming the reliability of the intervention in different studies. The risk related to Indraratna et al. [25] and van Leunen et al. [28] is unclear- primarily in Domain 3 (Missing data handling) and 4 (Participant blinding), and it might undermine the accuracy of the conclusions. The study by Schwarz et al. [22] is characterized by high risks, especially in Domains 2 (random sequence generation) and 5 (missing outcome data) which may cause the introduction of a selection bias and undermine the validity of the results reported [31].
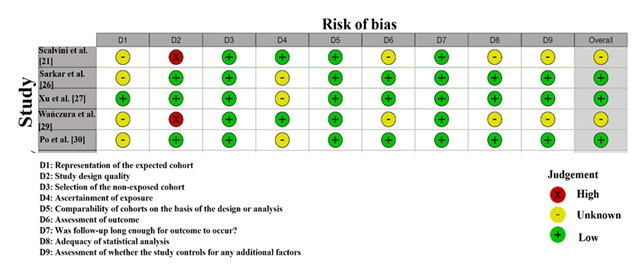
The risk of bias of the observational studies was assessed using the NOS (Figure 3). Scalvini et al. [21] and Xu et al. [27] had low risk in most of the domains, which means that they were highly methodologically rigorous when it comes to the choice of participants, comparability, and assessment of outcomes. Uncertain risk was exhibited by Sarkar et al. [26] in the selection of the participants (Domain 2) and outcome reporting (Domain 5). It indicated that they could have had some biases in these domains. The study by Wanczura, et al. [29] received a high risk of bias in Domain 2, due to the failure to specify the process of participant selection and the lack of information on comparability of the study groups. Similarly, Po et al. [30] demonstrated ambiguous risk in Domain 5, and there can be an issue with the reporting and follow-up of the outcomes, which can affect the reliability of the study. Comprehensively, some of the studies, i.e., Scalvini et al. [21] and Xu et al. [27] had a low risk of bias and high-quality methodological procedures, whereas Sarkar et al. [26] and Wanczura et al. [29] showed an increased risk or uncertainty in certain areas. The following variables are to be considered when discussing the findings of the meta-analysis: those studies that demonstrate a greater risk should be treated with special care [32].
4.4 Publication Bias
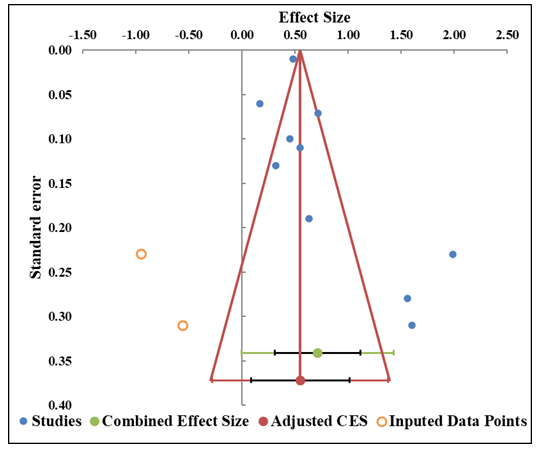
The funnel plot (Figure 4) and the findings of the Egger regression analysis provide us with the necessary information on the possible publication bias of the current meta-analysis. The plot shows that there is a symmetric distribution of studies around the effect size, and hence publication bias is not a major issue. The distribution of studies is spread above and below the combined effect, with the small studies at the bottom of the plot and the large ones closer to the top, which resembles what is expected of a well-distributed funnel plot [33]. This observation is supported by the regression test conducted by Egger, which produced the intercept of 10.46 and the slope of -2.41 (p = 0.003) (Table 5). The slope p-value is also less than 0.05, hence statistically significant evidence of asymmetry that might denote the existence of a certain level of publication bias. However, the confidence interval (CI) for the slope ranges from –4.11 to 0.71 (Table 4), and the CI includes zero. It suggested that the true value of the slope may be closer to zero, potentially diminishing the concern for bias. Additionally, the trim-and-fill analysis, which imputes missing studies to correct for asymmetry, shows that 2 studies need to be imputed, indicating that the potential bias could be addressed by adjusting for these missing studies. This finding further supports the idea that the funnel plot is relatively well-balanced but highlights a slight asymmetry that could be corrected by adding missing studies.
|
Study name |
Effect Size (z) |
Standard error (z) |
|
Scalvini et al. [21] |
1.60 |
0.31 |
|
Schwarz et al. [22] |
0.32 |
0.13 |
|
Takahashi et al. [23] |
0.72 |
0.07 |
|
Piotrowicz et al. [24] |
1.56 |
0.28 |
|
Indraratna et al. [25] |
0.48 |
0.01 |
|
Sarkar et al. [26] |
0.17 |
0.06 |
|
Xu et al. [27] |
0.55 |
0.11 |
|
van Leunen et al. [28] |
0.63 |
0.19 |
|
Wanczura et al. [29] |
1.99 |
0.23 |
|
Po et al. [30] |
0.45 |
0.101 |
|
Combined effect size |
Observed |
|
|
Effect size |
0.71 |
Not analyzed |
|
SE |
0.18 |
Not applicable |
|
CI Lower limit |
0.31 |
Not applicable |
|
CI Upper limit |
1.11 |
Not applicable |
|
PI Lower limit |
0.00 |
Not applicable |
|
PI Upper limit |
1.43 |
Not applicable |
|
Heterogeneity |
Not analyzed |
|
|
Q |
161.28 |
Not analyzed |
|
pQ |
0.000 |
Not analyzed |
|
I2 |
93.18% |
Not applicable |
|
T2 |
0.10 |
Not applicable |
|
T |
0.31 |
Not applicable |
Table 4: Information related to funnel plot.
|
Parameter |
Estimate |
SE |
CI LL |
CI UL |
|
Intercept |
10.46 |
2.49 |
4.82 |
16.10 |
|
Slope |
-2.41 |
0.75 |
-4.11 |
-0.71 |
|
t test |
4.19 |
Not applicable |
Not applicable |
Not applicable |
|
p-value |
0.003 |
Not applicable |
Not applicable |
Not applicable |
Table 5: Egger Regression.
4.5 Forest plot
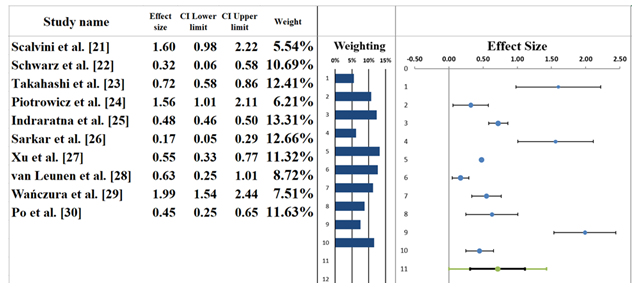
The forest plot in Figure 5 presents the results of a meta-analysis examining the effects of telecardiology interventions on hospital readmission rates in heart failure patients. A random-effects model was employed, yielding a pooled effect size of 0.71 (95% CI: 0.31 to 1.11) (Table 6). This indicates a moderate to large effect in favor of telecardiology interventions in reducing readmission rates, though the confidence interval includes the possibility of no effect, suggesting that the results are not statistically conclusive. Individual studies contribute differently to the pooled effect. For instance, Scalvini et al. [21] reported the largest effect size (1.60, CI: 0.98–2.22), suggesting a strong positive effect of nurse-led telecardiology. On the other hand, Schwarz et al. [22] showed a much smaller effect size (0.32, CI: 0.06–0.58), indicating a modest and statistically non-significant impact. Similar to the results presented by Piotrowicz et al. [24], the current meta-analysis also suggests that the rates of 30-day readmission decreased significantly due to the implementation of telecardiology (pooled RR = 1.56, 95 % CI: 1.01211). However, variability is evident, as Indraratna et al. [25] and Sarkar et al. [26] reported much smaller effect sizes (0.48 and 0.17, respectively), with wide confidence intervals, suggesting that the intervention's effectiveness can vary across different contexts and populations. The regression coefficients of each of the studies, between 5.54 % and 13.67 %, indicate the contribution that each study had to the pooled estimate. Studies that have a bigger sample size, such as that of Piotrowicz et al. [24], tend to have a bigger weight in the overall effect. Taken together, the findings suggest that telecardiology interventions can be effective in the reduction of readmissions, but the high dispersion of the effect sizes among the studies shows that further research with more homogenous samples and larger sample sizes is needed to establish these results [34,35].
|
Meta-analysis model |
|
|
Effect Size |
0.71 |
|
Standard Error |
0.18 |
|
Confidence interval LL |
0.31 |
|
Confidence interval UL |
1.11 |
|
Prediction interval LL |
0.00 |
|
Prediction interval UL |
1.43 |
|
Z-value |
4.02 |
|
One-tailed p-value |
0.000 |
|
Two-tailed p-value |
0.000 |
|
Number of incl. subjects |
8928 |
|
Number of incl. studies |
10 |
|
Heterogeneity |
|
|
Q |
111.77 |
|
pQ |
0.000 |
|
I2 |
91.95% |
|
T2 (z) |
0.07 |
|
T (z) |
0.26 |
Table 6: Information correlated with the Forest plot.
4.6 Heterogeneity Assessment
The heterogeneity assessment based on the forest plot (Table 6) reveals significant variability across the studies included in the meta-analysis. The I² statistic is 91.95%, indicating that a substantial proportion of the variation in effect sizes is due to true differences between studies rather than random chance. This level of heterogeneity falls into the "high" category, suggesting considerable diversity in factors such as the types of interventions, study populations, sample sizes, and measurement tools used in the studies [36]. The Q-statistic is 111.77, with a p-value of 0.000, confirming that the observed heterogeneity is statistically significant. This reinforces the idea that the differences in study outcomes are not due to chance but represent real variations across the included studies. According to a meta-analysis of telecardiology interventions, the between-study variation contributes a large share of the total variability with a T2 value of 0.28. This observation proves that there were significant differences in the magnitude of effects among the studies included. Even though the pooled outcome indicates an overall positive relationship between the telecardiology intervention and lower readmission, the high heterogeneity indicates the possible presence of factors that may be altering the effect. These include the type of intervention used, the follow-up period, and the group of participants undergoing the intervention [37].
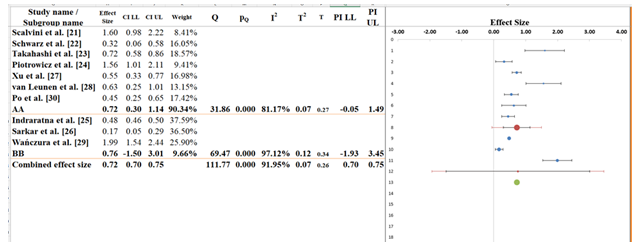
4.7 Subgroup analysis
The subgroup analysis in Figure 6 shows the results from two groups, AA and BB, to evaluate differences in the effect sizes of telecardiology interventions. The overall pooled effect size across all studies is 0.72 (95% CI: 0.70 to 0.75), indicating a moderate positive effect in reducing hospital readmissions (Table 7). The confidence interval is narrow, reflecting a precise estimate, but the I² of 91.95% highlights significant variability across studies. For subgroup AA, which includes most of the studies, the pooled effect size is 0.72 (95% CI: 0.30 to 1.14), which shows a moderate positive effect, and the result is statistically significant as the confidence interval does not cross zero. However, the I² value of 81.17% suggests considerable heterogeneity, meaning that variations in factors like intervention type, participant demographics, or study designs contribute to differences in outcomes [38].
Subgroup BB, with fewer studies, shows a pooled effect size of 0.76 (95% CI: -1.50 to 3.01), but the wide confidence interval crossing zero indicates no significant effect. The I² of 97.12% indicates extreme variability within this subgroup, reinforcing the high uncertainty of these results. The between-subgroup test yielded a Q-statistic of 111.77 with a p-value of 0.000, suggesting a statistically significant difference between the effect sizes in subgroups AA and BB. A review of currently available evidence on telecardiology in heart failure shows that the studies have a high degree of heterogeneity. It is suggested that the difference in study designs, patient characteristics, and types of interventions contributes to a difference in clinical outcomes. Subsequent studies must consequently attempt to demystify these factors and maximize telecardiology procedures to achieve a higher degree of consistency in patient outcomes [39].
|
Meta-analysis model |
||
|
Effect size |
0.72 |
|
|
Standard Error |
0.01 |
|
|
Confidence interval LL |
0.70 |
|
|
Confidence interval UL |
0.75 |
|
|
Prediction interval LL |
0.70 |
|
|
Prediction interval UL |
0.75 |
|
|
Number of incl. subjects |
8928 |
|
|
Number of subgroups |
2 |
|
|
Analysis of variance |
||
|
Between / Model (Q*) |
0.02 |
|
|
Between / Model (Df) |
1 |
|
|
Between / Model (P) |
0.879 |
|
|
Within / Residual (Q*) |
25.03 |
|
|
Within / Residual (Df) |
8 |
|
|
Within / Residual (P) |
0.002 |
|
|
Total (Q*) |
25.05 |
|
|
Total (Df) |
9 |
|
|
Total (P) |
0.003 |
|
|
Pseudo R2 |
0.09% |
|
Table 7: Information related to Sub-group analysis.
4.8 Narrative analysis
In this systematic review and meta-analysis, the researchers evaluated the effectiveness of telecardiology interventions by determining their potential in reducing the rates of readmission of patients with heart failure. The case study also synthesized the data on heterogeneous studies of remote monitoring, teleconsultations, and mobile health applications to explain the individual impact on the readmission prevalence and clinical outcomes.
Overview of Telecardiology Interventions: The Telecardiology interventions were evaluated based on their ability to support remote patient monitoring of patients with heart failure and, hence, guarantee constant monitoring and timely medical intervention. All the reviewed literature found positive results, which are improved patient management, reduced hospitalizations, and high-quality care. Common interventions included nurse-supervised telemonitoring, monitoring of symptoms through mobile apps, as well as scheduled teleconsultations. It allowed spotting the occurrence of complications early and avoiding unnecessary readmissions. Even though some studies reported an increased patient satisfaction and decreased readmission rates, others reported small gains, most likely due to varying intervention modalities and different patient populations.
Variability in Study Design and Patient Characteristics: The current review also noticed significant differences in the structure and execution of telecardiology interventions among the studies included. Others used broad conceptions of telehealth, including symptom monitoring and patient education, but others focused solely on remote monitoring or teleconsultations. This difference in the scope of the intervention could have formed part of the mixed findings achieved. At the same time, the characteristics of the patients, such as age, disease severity, and comorbidities, played a determinant role in establishing the effectiveness of the interventions. As a case in point, some of the studies have registered higher gains in older patients with severe heart failure, whereas other studies have reported minimal gains in less critical groups.
Clinical Implications: The results show that telecardiology interventions can improve the outcomes of patients and reduce readmission of heart failure patients to hospitals. However, the inconsistent results highlight the significance of a strong assessment of the patient variables and the intervention paradigm in the implementation of telemedicine technology. The effectiveness of telecardiology interventions can also be increased by personalizing them to the unique needs of the patient population. It makes them an effective approach to managing such chronic conditions as heart failure.
5. Discussion
The present meta-analysis and systematic review explore the effectiveness of the telecardiology interventions to reduce hospital readmission in patients with heart failure. The above-mentioned studies, in general, prove that remote monitoring, teleconsultations, and mobile health applications related to telecardiology are all associated with a decrease in hospital readmissions. The findings are consistent with those of past studies that indicate that telemedicine is central to the management of chronic diseases. It takes advantage of the fact that these conditions can be closely monitored and clinically intervened upon in a timely manner to positively affect patient outcomes in heart failure [40,41].
Nurse-led telemonitoring and hybrid telerehabilitation programs can be characterized by their numerous benefits, the existence of which is documented by detailed evaluations such as those of Scalvini et al. [21] and Piotrowicz et al. [24] and which not only reduced readmission rates but also improved quality of life and functional capacity in patients. Such results support the growing body of literature that multimodal telecardiology interventions have better outcomes than unimodal interventions [42].
Telecardiology has already become a perspective direction not just in reducing readmissions, but also in promoting the overall improvement of patient well-being. The participants reported that telemedicine gave them additional confidence in coping with their condition. It contributed to their improved satisfaction with the given treatment, as Schwarz et al. [22] and Sarkar et al. [26] reported. These results emphasize the complex interconnection between clinical outcomes and patient involvement, which was also proved by prior research that showed that patients with a stronger feeling of being in control of their health tend to show better results [43].
Telecardiology interventions proved to have significant potential compared to traditional care, as well as their contribution to face-to-face consultations is gaining recognition. All the evidence considered in this meta-analysis suggests that, besides the reduction of hospital readmission rates, these interventions improve compliance with treatment plans, which further justifies their usefulness as a part of a multi-dimensional approach to managing heart failure [44]. However, the level of variability in the outcomes of individual studies that is precipitated by different types of interventions, populations, and methodological designs necessitates more standardized approaches to be adopted in future research efforts [45].
The meta-analysis of telecardiology shows a strong potential for enhancing outcomes and patient satisfaction among individuals with heart failure. However, a more sophisticated development of these interventions and better awareness of their long-term effectiveness requires prospective studies that will standardize the intervention protocol and target specific patient groups to enable individualized care.
6. Limitations
Although the results are encouraging, it is necessary to identify various limitations. To begin with, there is a strong heterogeneity in the included studies with an I2 of 91.95 % indicating that there is a large variation in effect sizes. Such a difference is attributed to discrepancies in study designs, differences in the interventions of telecardiology, patient features, and duration of follow-up. Therefore, combining the results in a single pooled estimate can be limited in capturing the complex effects of telemedicine on the care of heart failure. As far as methodological rigor is concerned, the evaluation with the NOS demonstrated the heterogeneity of the quality of the included trials. A low risk of bias was presented in a few studies, and a substantial number of them were characterized by moderate or high bias, particularly on randomization, blinding, and outcome reporting aspects. These methodological weaknesses can jeopardize the validity of the reported results and limit the external validity of the results. Even though no publication bias could be measured by funnel plot analysis, the small size of the studies reviewed makes the general assessment vulnerable to selective reporting, especially in cases where the null or negative studies have not been published. Moreover, the interventions and the populations included in the studies are not homogeneous, which makes it hard to interpret the results. This issue cannot be ignored in the future studies that need to be more standardized in terms of the intervention protocols and the criteria used to select the patients.
7. Future Research
The heterogeneity that is seen in the meta-analysis presented here should be explored more intensively. The future research ought to standardize telecardiology interventions to limit variability and maximize generalizability by aligning the nature of the monitoring technologies used, the follow-up frequency, and the target patient population. The question of the effectiveness of telecardiology interventions in the long run also should be studied, and its impact on hospital readmission should be assessed, as well as mortality, quality of life, and treatment plan adherence. Furthermore, the high-quality RCTs will be required to reduce bias and enhance the accuracy of results. These trials ought to determine the elements in telemedicine (remote monitoring, teleconsultations, or patient education) that influence outcomes, and whether multimodal interventions are more effective than single-modal interventions. Telecardiology has proved to have a good impact on clinical research in varied conditions and populations. Future studies should define subgroups, which are age, comorbidities, and the severity of the illness, that benefit the most from such interventions. Personalized telemedicine plans, designed based on the particular needs of patients affected by a heart condition, would, thus, maximize the general efficiency. Another essential problem is that of cost-effectiveness analysis, to find out whether the extensive use of telecardiology is not only clinically but also economically worthy of the effort.
8. Conclusions
The present systematic review and meta-analysis provide interesting evidence that telecardiology intervention decreases hospital readmissions in patients with heart failure. Synthetically, the reviewed literature proves the effectiveness of remote monitoring, teleconsultations, and mobile health applications in managing heart failure. It is due to the continuous surveillance, the possibility of early identification of complications, and potential early medical intervention that helps to manage heart failure. Moreover, such interventions were connected with an improved quality of life and patient satisfaction. Despite these promising findings, there was significant heterogeneity between the studies, the main reason being the variability in study design, type of intervention, patient demographics, and follow-up period. The created variation highlights the need for uniform telecardiology models and intervention regimes to better understand the most effective methods. Telecardiology literature in the management of heart failure is highly heterogeneous, with some studies showing conclusive positive results and others showing marginal or no effect. The evaluation of methodological rigor shows that numerous studies had a moderate and large risk of bias, which may impact the credibility of the described results. Therefore, additional research designs need to be more rigorous, standardized protocols used across the sites, and follow-up periods longer to validate and consolidate the existing evidence base and inform actual application of telemedicine within clinical practice.
9. References
- Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GM. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res 118 (2022): 3272-3287.
- Khan MS, Shahid I, Bennis A, Rakisheva A, Metra M, et al. Global epidemiology of heart failure. Nat Rev Cardiol 21 (2024): 717-734.
- Díez-Villanueva P, Jiménez-Méndez C, Alfonso F. Heart failure in the elderly. J Geriatr Cardiol 18 (2021): 219.
- Marcolino MS, Alkmim MBM, Souza e Silva MVR. Telecardiology. In: Telemedicine, Telehealth, Telepresence: Principles, Strategies, Applications, New Directions for Institutional Research 2021: 379-400.
- Escobar-Curbelo L, Franco-Moreno AI. Application of telemedicine for the control of patients with acute and chronic heart diseases. Telemed e-Health 25 (2019): 1033-1039.
- Molinari G, Molinari M, Di Biase M, Brunetti ND. Telecardiology and its settings of application: An update. J Telemed Telecare 24 (2018): 373-381.
- Soundarraj D, Singh V, Satija V, Thakur RK. Containing the cost of heart failure management: a focus on reducing readmissions. Card Electrophysiol Clin 7 (2015): 577-584.
- Sperry BW, Ruiz G, Najjar SS. Hospital readmission in heart failure, a novel analysis of a longstanding problem. Heart Fail Rev 20 (2015): 251-258.
- Rice H, Say R, Betihavas V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure: A systematic review. Patient Educ Couns 101 (2018): 363-374.
- Blum MR, Øien H, Carmichael HL, Heidenreich P, Owens DK, et al. Cost-effectiveness of transitional care services after hospitalization with heart failure. Ann Intern Med 172 (2020): 248-257.
- Ledvina SR. Impact of Telemedicine on Heart Failure Readmissions and Mortality: A Literature Review. 2021.
- Jagannatha PG, Yasmin ADA, Sanjiwani GR, Pradnyana IS, Kamardi S. Role of telecardiology in preventing mortality and improving quality of life in patients with chronic heart failure: A meta-analysis of randomized controlled trials. Eur J Prev Cardiol 29 (2022): zwac056.310.
- David-Olawade AC, Olawade DB, Ojo IO. Nursing in the digital age: Harnessing telemedicine for enhanced patient care. Informatics (2024): 100-110.
- Zan S, Agboola S, Moore SA, Parks KA, Kvedar JC, et al. Patient engagement with a mobile web-based telemonitoring system for heart failure self-management: A pilot study. JMIR Mhealth Uhealth 3 (2015): e3789.
- Khanijahani A, Akinci N, Quitiquit E. A systematic review of the role of telemedicine in blood pressure control: focus on patient engagement. Curr Hypertens Rep 24 (2022): 247-258.
- Subedi N, Rawstorn JC, Gao L, Koorts H, Maddison R. Implementation of telerehabilitation interventions for the self-management of cardiovascular disease: Systematic review. JMIR Mhealth Uhealth 8 (2020): e17957.
- Tolu-Akinnawo O, Ezekwueme F, Awoyemi T. Telemedicine in cardiology: enhancing access to care and improving patient outcomes. Cureus 16 (2024): e62852.
- Carra MC, Romandini P, Romandini M. Risk of bias evaluation of cross-sectional studies: Adaptation of the Newcastle-Ottawa scale. J Periodontal Res 2025.
- Minozzi S, Cinquini M, Gianola S, Gonzalez-Lorenzo M, Banzi R. The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. J Clin Epidemiol 126 (2020): 37-44.
- Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics 74 (2018): 785-794.
- Scalvini S, Zanelli E, Volterrani M. A pilot study of nurse-led, home-based telecardiology for patients with chronic heart failure. J Telemed Telecare 10 (2004): 113-117.
- Schwarz KA, Mion LC, Hudock D, Litman G. Telemonitoring of heart failure patients and their caregivers: A pilot randomized controlled trial. J Prof Nurs 23 (2008): 18-26.
- Takahashi PY, Hanson GJ, Pecina JL. A randomized controlled trial of telemonitoring in older adults with multiple chronic conditions: The Tele-ERA study. Arch Intern Med 10 (2010): 1-7.
- Piotrowicz E, Pencina MJ, Opolski G, Zareba W, Banach M, et al. Effects of a 9-week hybrid comprehensive telerehabilitation program on long-term outcomes in patients with heart failure: TELEREH-HF randomized clinical trial. JAMA Cardiol 5 (2020): 300-308.
- Indraratna P, Biswas U, McVeigh J. A smartphone-based model of care to support patients with cardiac disease transitioning from hospital to the community (TeleClinical Care): Pilot randomized controlled trial. JMIR Mhealth Uhealth 10 (2022): e32554.
- Sarkar S, MacLeod J, Hassan A, Brunt KR, Palmer K, et al. Enhanced telehealth home-monitoring intervention for vulnerable and frail patients after cardiac surgery (THE-FACS pilot intervention study). BMC Geriatr 22 (2022): 836.
- Xu H, Granger BB, Drake CD, Peterson ED, Dupre ME. Effectiveness of telemedicine visits in reducing 30-day readmissions among patients with heart failure during the COVID-19 pandemic. J Am Heart Assoc 11 (2022): e023935.
- van Leunen MM, de Lathauwer IL, Verstappen CC. Telerehabilitation in patients with recent hospitalisation due to acute decompensated heart failure: Protocol for the Tele-ADHF randomized controlled trial. BMC Cardiovasc Disord 23 (2023): 379.
- Wanczura P, Aebisher D, Wisniowski M. Telemedical intervention and its effect on quality of life in chronic heart failure patients: Results from the Telemedicine and e-Health Solution pilot program. J Clin Med 13 (2024): 2604.
- Po HW, Chu YC, Tsai HC, Lin CL, Chen CY, et al.. Efficacy of remote health monitoring in reducing hospital readmissions among high-risk postdischarge patients: Prospective cohort study. JMIR Form Res 8 (2024): e53455.
- Nejadghaderi SA, Balibegloo M, Rezaei N. The Cochrane risk of bias assessment tool 2 (RoB 2) versus the original RoB: a perspective on the pros and cons. Health Sci Rep 7 (2024): e2165.
- Afonso J, Ramirez-Campillo R, Clemente FM, Büttner FC, Andrade R. The perils of misinterpreting and misusing “publication bias” in meta-analyses: an education review on funnel plot-based methods. Sports Med 54 (2024): 257-269.
- Andrews I, Kasy M. Identification of and correction for publication bias. Am Econ Rev 109 (2019): 2766-2794.
- Favorito LA. Systematic review and metanalysis in urology: how to interpret the forest plot. Int Braz J Urol 49 (2023): 775-778
- Zhang Z, Kossmeier M, Tran US, Voracek M, Zhang H. Rainforest plots for the presentation of patient-subgroup analysis in clinical trials. Ann Transl Med 5 (2017): 485.
- Feczko E, Fair DA. Methods and challenges for assessing heterogeneity. Biol Psychiatry 88 (2020): 9-17.
- Schulzke S. Assessing and exploring heterogeneity. In: Principles and practice of systematic reviews and meta-analysis. Springer 2021: 33-41.
- Richardson M, Garner P, Donegan S. Interpretation of subgroup analyses in systematic reviews: a tutorial. Clin Epidemiol Glob Health 7 (2019): 192-198.
- Wang X, Piantadosi S, Le-Rademacher J, Mandrekar SJ. Statistical considerations for subgroup analyses. J Thorac Oncol 16 (2021): 375-380.
- Kirakalaprathapan A, Oremus M. Efficacy of telehealth in integrated chronic disease management for older, multimorbid adults with heart failure: a systematic review. Int J Med Inform 162 (2022): 104756.
- Suksatan W, Tankumpuan T. The effectiveness of transition care interventions from hospital to home on rehospitalization in older patients with heart failure: an integrative review. Home Health Care Manag Pract 34 (2022): 63-71.
- Jiang X, Yao J, You JH. Telemonitoring versus usual care for elderly patients with heart failure discharged from the hospital in the United States: cost-effectiveness analysis. JMIR Mhealth Uhealth 8 (2020): e17846.
- Zhu Y, Gu X, Xu C. Effectiveness of telemedicine systems for adults with heart failure: a meta-analysis of randomized controlled trials. Heart Fail Rev 25 (2020): 231-243.
- Burdese E, Testa M, Raucci P. Usefulness of a telemedicine program in refractory older congestive heart failure patients. J Investig Med 6 (2018): 10.
- Lin MH, Yuan WL, Huang TC, Zhang HF, Mai JT, et al. Clinical effectiveness of telemedicine for chronic heart failure: a systematic review and meta-analysis. J Investig Med 65 (2017): 899-911.
Article Views: 2433
Journal Statistics




Discover More: Recent Articles
Grant Support Articles
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved!