Experience of 17 Cases of Tube Thoracostomy of COVID-19 Positive Patients During COVID-19 Pandemic Under Thoracic Surgery Unit of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
Heemel Saha
Assistant Professor, Thoracic Surgery, BSMMU, Dhaka, Bangladesh
*Corresponding author: Heemel Saha, Assistant Professor, Thoracic Surgery, BSMMU, Dhaka, Bangladesh.
Received: 16 November 2021; Accepted: 30 November 2021; Published: 09 December 2021
Article Information
Citation: Saha H. Experience of 17 Cases of Tube Thoracostomy of COVID-19 Positive Patients During COVID-19 Pandemic Under Thoracic Surgery Unit of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh. Cardiology and Cardiovascular Medicine 5 (2021): 695-703.
View / Download Pdf Share at FacebookAbstract
Background: Patients with COVID-19 are at risk of developing acute respiratory distress syndrome requiring invasive mechanical ventilation. Barotrauma in these patients often leads to clinically significant pneumothorax, which necessitates chest tube thoracostomy. However, given the mode of transmission of the severe acute respiratory syndrome coronavirus 2 virus and the aerosolizing nature of the procedure, special considerations and care must be taken to mitigate the exposure risks to health care personnel. This article discusses the risk mitigation strategies proposed and under review at the authors’ institution.
Objective To identify and diagnosis Tube thoracostomy of COVID-19 positive patients during COVID-19 pandemic under thoracic surgery unit of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh. Methods and materials A retrospective study was conducted in thoracic surgery unit of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh. Seventeen patients included in our study. We included all COVID-19 cases admitted to ICU in the period between July 2020 to August 2021, requiring thoracic surgery consultation and management. Non-COVID-19 critical cases and iatrogenic pneumothorax were excluded.
Results Total 17 patients required thoracic surgery consultation and management. Causes were pneumothorax: 05 cases (29.41%), traumatic hemothorax: 01 cases (5.88%), hydropneumothorax: 01 case (5.88%) and massive pleural effusion: 10 cases (58.82%). No complication after tube thoracostomy. 15 patient’s condition were improved in relation to oxygen demand and left hospital in good health and two patient died 3 days after tube thoracostomy who were in artificial ventilation and both patients had more than 81% lung involvement (fibrosis) diagnosed by CT scan of chest. The survival analysis showed improvement in patients who had
Keywords
<p>Barotrauma; Chest tube; COVID-19; Pneumothorax; Pleural effusion; SARS-CoV-2; Tube thoracostomy</p>
Article Details
1. Introduction
Tube thoracostomy for a traumatic hemothorax or pneumothorax is a potentially aerosol-generating procedure that is performed frequently by acute care surgeons. There are no data specific to the aerosolization of the severe acute respiratory syndrome coronavirus 2 specifically through placement of a tube thoracostomy, and the potential risk likely varies based on the indication for placement. This document provides guidance regarding special precautions to consider during the COVID-19 pandemic to minimize exposure risk to staff during tube insertion, drainage system management and tube removal. The information provided here is not intended to supersede clinical judgment. Given the limited data, the lack of any of the special equipment below should not prevent or delay the placement of a tube thoracostomy in a life-threatening situation. As the current pandemic evolves, some or all of the data and recommendations may not be applicable to future conditions. The complication rate following tube thoracostomy insertion can be up to 40% [1]. In many hospitals, tube thoracostomy is normally performed by multiple specialties, including surgery, pulmonary, radiology and emergency medicine, and the likelihood of complication is directly related to both the experience level and specialty of the proceduralist [2]. During the COVID-19 pandemic, ensuring staff safety must supersede trainee education. Accordingly, tube thoracostomy insertion for patients with known or suspected COVID-19 should occur by the most experienced provider and with the fewest number of staff members required. Optimally a thoracic procedure team would be created, composed of an attending surgeon and either a senior resident, fellow or advanced practice provider. If a thoracic procedure team is available, they would respond to all requests for tube thoracostomy in at-risk or confirmed COVID-positive patients throughout the hospital, thereby minimizing both variability in and number of proceduralists, as well as maximizing the likelihood of successful tube placement. If creation of a formal thoracic procedure team is not logistically possible, strong consideration should be given to limiting the number of both providers and specialists performing tube thoracostomy.
2. Methods and Materials
A retrospective study was conducted in thoracic surgery unit of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh. Seventeen patients included in our study. We included all COVID-19 cases admitted to ICU in the period between July 2020 to August 2021, requiring thoracic surgery consultation and management. Non-COVID-19 critical cases and iatrogenic pneumothorax were excluded. Patients’ charts were reviewed, and demographic data, comorbidities, patterns of thoracic complications, management, length of stay, intubation, reintubation, ventilatory settings, intervention, outcome, and recovery were all analyzed. In cases of ME and SE, conservative management that included close follow-up clinically and radiologically was applied according to the clinical pathway for SE and ME [3]. Thoracostomy tubes were inserted in patients with pneumothorax that was discovered in the routine daily chest X-ray or in a chest X-ray that was performed whenever there is a clinical suspicion of pneumothorax occurrence. The study objective was to establish The American Association for Thoracic Surgery (AATS) evidence-based guidelines for the management of empyema.
3. Statistical Analysis
An excel spreadsheet was established for the entry of data. Data analysis was carried out using SPSS, Version 22. Categorical variables were summarized as frequencies and percentages. To determine the significant association of variables, the Mann–Whitney U test and Fisher exact test were used, and a significant level was considered at P <0.05. In addition, multivariate correlation and regression were done. Moreover, the Kaplan–Meier test was done for analyzing the expected duration of time of death in our sample size. Finally, a comparison between our sample and the total number of COVID-19 patients who were admitted to the ICU regarding their outcome and total length of stay in the hospital was done by using the Kruskal–Wallis test.
4. Results
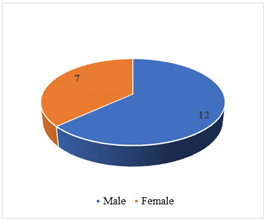
Seventeen COVID-19 patients were admitted to the ICU and twelve patients (70.58%) were males and 7 (29.42%) were females, with a male: female ratio of 1.7:1. Age range from 36 years to 77 years included in your study.
|
Occupation |
N |
% |
|
Farmer |
2 |
11.76 |
|
Job |
6 |
35.29 |
|
Business |
4 |
23.52 |
|
House hold worker |
5 |
29.41 |
|
Cause of Tube Thoracostomy: Pneumothorax: 05 cases 29.41%, Traumatic Hemothorax: 01 cases 5.88%, Hydropneumothorax: 01 cases 5.88% and Massive Pleural Effusion: 10 cases 58.82% (table-2). |
||
Table 1: Distribution of patient’s occupation.
|
Cause |
N |
% |
|
Pneumothorax |
05 cases |
29.41 |
|
Traumatic Hemothorax |
01 cases |
5.88 |
|
Hydropneumothorax |
01 cases |
5.88 |
|
Massive Pleural Effusion |
10 cases |
58.82 |
|
All are Emergency cases, no routine cases and no Pleural Biopsy and pleurodesis was done. All patients had co-morbidities. COPD: 7 cases (41.17%), DM: 4 cases (23.52%), Chronic Kidney Disease (CKD): 3 cases (17.64%), DM with IHD: 2 cases (11.76%) and History of CABG: 1 case 5.88% (table-3). |
||
Table 2: Cause of Tube Thoracostomy.
|
Co-morbidities |
N |
% |
|
COPD |
7 |
41.17 |
|
DM |
4 |
23.52 |
|
Chronic Kidney Disease (CKD) |
3 |
17.64 |
|
DM with IHD |
2 |
11.76 |
|
History of CABG |
1 |
5.88 |
|
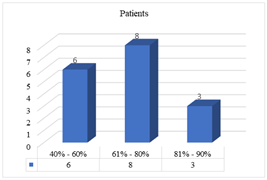
Percentage of lung involvement (fibrosis) diagnosed by CT scan of chest 40% - 60%: 6 patients, 61% - 80%: 8 patients and 81% - 90%: 3 patients (fig-2). |
||
Table 3: Distribution of Patients co-morbidities.
Condition of the patient during tube thoracostomy on face mask with 10 lit/m O2: 7 cases, On non-rebreather mask with 16 lit/m O2: 5 cases, On high flow nasal cannula with 35-60 lit/m O2: 3 Cases and on artificial ventilation: 2 cases. The highest Condition of the patient during tube thoracostomy 7 cases 41.17% of condition purpose on face mask with 10 lit/m O2 (Table-4).
|
Condition of the patient during tube thoracostomy |
No of Cases |
% |
|
On face mask with 10 lit/m O2 |
7 |
Cause of Tube Thoracostomy: Pneumothorax: 05 cases 29.41%, Traumatic Hemothorax: 01 cases 5.88%, Hydropneumothorax: 01 cases 5.88% and Massive Pleural Effusion: 10 cases 58.82% (table-2).
41.17 |
|
On non-rebreather mask with 16 lit/m O2 |
5 |
29.41 |
|
On high flow nasal cannula with 35-60 lit/m O2 |
3 |
17.64 |
|
On artificial ventilation |
2 |
11.76 |
|
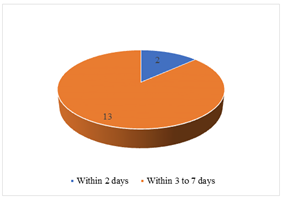
Timing of removal of Chest drain tube Within 2 days: 2 cases and Within 3 to 7 days: 13 cases (figure 3). |
||
Table 4: Condition of the patient during tube thoracostomy.
|
Outcome |
N |
% |
|
Improved |
15 |
88.23 |
|
Died |
2 |
11.77 |
Table 5: Outcome of Patient’s condition after tube thoracostomy.
No Complication after tube thoracostomy. 15 patient’s condition improved in relation to oxygen demand and left hospital in good health and two patient died 3 days after tube thoracostomy who were in artificial ventilation and both had more than 81% lung involvement (fibrosis) diagnosed by CT scan of chest (Table-5). Chest drain tube was always given in “Safety triangle”. All patients were followed guidance and recommendations from the AAST Acute Care Surgery and Critical Care Committees for tube thoracostomy during the COVID-19 pandemic. All cases were done by local anesthesia (2% lignocaine injection).
5. Discussion
In December 2019, the first case of COVID-19 was diagnosed in China. Human-to-human transmission transpired early in 2020, causing a global pandemic to ensue [4]. Since then, targeted medical strategies have been implemented at multiple levels encompassing numerous specialties. As the disease progressed, we developed an understanding of the disease components. We drew on experience gained earlier in the millennium from Severe Acute Respiratory Syndrome (SARS) and the influenza A virus subtype, H1N1 flu [4,5]. The symptoms are similar to large extent, with a cough and shortness of breath as the hallmarks. Many physicians attribute coughing and the subsequent increase in intra-alveolar pressure as contributing causes of thoracic complications in such patients. In SARS-CoV-1, ME was typically seen in combination with SE or pneumothorax, rather than as solo entities [5]. It was also seen in unintubated patients, which supports the notion that the destruction of alveoli is due to the disease process rather than a complication of mechanical ventilation. The presence of ME is actually considered a marker for an increased likelihood of intubation [6]. Moreover, it was often a precursor of increased mortality. In SARS-CoV-1, ME incidence was around 11.6%. It is usually indicated by Naclerio’s V sign, an air rim shadow on the border of the heart [6]. Unlike MERS-CoV and SARS-CoV-1, COVID-19 has a characteristic disease pattern of ground-glass opacities preferentially distributed towards the posterior segments of the lower lobes [7]. In our study, we found a significant association between the outcome, reintubation rates, and these thoracic complications. In COVID-19 patients who developed thoracic complications in general, better prognosis was seen in patients with pneumothorax who were treated with thoracostomy tube insertion. The survival analysis test showed a higher survival rate in patients who were treated with indwelling thoracostomy tubes in comparison to the conservative group. The notion was that, in patients (other than COVID-19 patients) who developed SE and ME without pneumothorax, the conservative approach is well accepted [3]. But, we elected to treat by thoracostomy tube insertion on the ipsilateral side of the SE in our group of COVID-19 patients. The peculiarity of those patients and the isolation constraints in critical care setting and monitoring dictated to practice safer and more aggressive prophylactic approach. Our study no Complication after tube thoracostomy. 15 patient’s condition improved in relation to oxygen demand and left hospital in good health and two patient died 3 days after tube thoracostomy who were in artificial ventilation and both had more than 81% lung involvement (fibrosis) diagnosed by CT scan of chest. Chest drain tube was always given in “Safety triangle”. All patients were followed guidance and recommendations from the AAST Acute Care Surgery and Critical Care Committees for tube thoracostomy during the COVID-19 pandemic. All cases were done by local anesthesia (2% lignocaine injection). A significant difference was observed between the total COVID-19 patients who were admitted in the ICU without development of thoracic complications and those who had thoracic complications in the total length of hospital stay, a reflection of the magnitude of these complications and their effect on patients. It seems that the disease process plays a strong role in the degree of lung parenchyma destruction and subsequent thoracic complications.
6. Conclusion
Tube thoracostomy for a traumatic hemothorax or pneumothorax is a potentially aerosol-generating procedure that is performed frequently by acute care surgeons. There are no data specific to the aerosolization of the severe acute respiratory syndrome coronavirus 2 specifically through placement of a tube thoracostomy, and the potential risk likely varies based on the indication for placement. This document provides guidance regarding special precautions to consider during the COVID-19 pandemic to minimize exposure risk to staff during tube insertion, drainage system management and tube removal. The information provided here is not intended to supersede clinical judgment. Given the limited data, the lack of any of the special equipment below should not prevent or delay the placement of a tube thoracostomy in a life-threatening situation. As the current pandemic evolves, some or all of the data and recommendations may not be applicable to future conditions. Non-iatrogenic pneumothorax, subcutaneous emphysema, and mediastinal emphysema are well-known thoracic entities, but their presence in the context of COVID-19 disease is a harbinger for worse prognosis and outcomes. The presence of pneumothorax may be associated with better prognosis and outcome compared to surgical and mediastinal emphysema.
References
- Platnick C, Witt CE, Pieraccci FM, Robinson CK, Cohen M, Moore EE, et al. Beyond the tube: can we predict (and improve) chest tube complications in trauma patients? Oral presentation at the 2020 virtual meeting of the chest wall injury Society.
- Etoch SW, Bar-Natan MF, Miller FB, Richardson JD. Tube thoracostomy. Factors related to complications. Arch Surg 130 (1995): 521-525.
- VK Kouritas, K Papagiannopoulos, G Lazaridis, et al., “Pneumomediastinum,” Journal of Thoracic Disease 2015 (7): 44-49,.
- Ucpinar BA, Sahin C, Yanc U. Spontaneous pneumothorax and subcutaneous emphysema in COVID-19 patient: case report. Journal of Infection and Public Health 13 (2020): 887-889.
- Udupa S, Hameed T, Tom K. Pneumomediastinum and subcutaneous emphysema associated with pandemic (H1N1) influenza in three children. CMAJ 2011(183).
- Wali A, Rizzo V, Bille A, Routledge T, Chambers AJ. Pneumomediastinum following intubation in COVID-19 patients: a case series. Anaesthesia 75 (2020): 1076-1081,.
- Mohan V, Ahmed Tauseen R. Spontaneous pneumomediastinum in COVID-19. BMJ Case Reports 13 (2020): 236519.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 