From Gut to Heart: The TMAO Breakthrough Changing Southeast Asia’s Cardiac Landscape
Prof. Dasaad Mulijono1,2,3
1Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia
2Indonesian College of Lifestyle Medicine, Indonesia
3Department of Cardiology, Faculty of Medicine, Prima University, Medan, Indonesia
*Corresponding author:Prof. Dasaad Mulijono, Department of Cardiology, Faculty of Medicine, Prima University, Medan, Indonesia.
Received: June 17, 2025; Accepted: June 25, 2025; Published: July 27, 2025
Article Information
Citation: Dasaad Mulijono, From Gut to Heart: The TMAO Breakthrough Changing Southeast Asia’s Cardiac Landscape. Cardiology and Cardiovascular Medicine 9 (2025): 216-220.
View / Download Pdf Share at FacebookAbstract
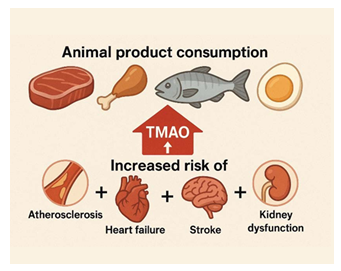
Trimethylamine N-oxide (TMAO) has emerged as a novel biomarker implicated in the pathogenesis and progression of various cardiometabolic conditions, including coronary artery disease (CAD), stroke, type 2 diabetes mellitus, obesity/metabolic syndrome, chronic kidney disease, restenosis, and heart failure. Despite increasing global recognition of its clinical relevance, TMAO testing was not available in Indonesia until Bethsaida Hospital, under the leadership of Prof. Dasaad Mulijono, successfully established a partnership with Prodia, the only private laboratory in the country willing to invest in TMAO diagnostic technology.
This article describes the implementation of TMAO testing at Bethsaida Hospital, evaluates its diagnostic and prognostic utility, and explores its role in monitoring adherence to a healthy plant-based diet (PBD).
Bethsaida Hospital is also a national pioneer in using Drug-Coated Balloon (DCB) technology for coronary interventions. Ongoing research at the institution investigates the relationship between TMAO levels and dietary adherence among cardiac patients. Individuals with lower TMAO concentrations tend to exhibit a reduced restenosis rate following DCB procedures. Furthermore, patients who demonstrate regression of coronary plaques, particularly those adhering to a PBD, consistently exhibit low TMAO levels, supporting its potential as a surrogate marker for a favourable gut microbiota composition and dietary pattern.
TMAO remains the only clinically available biomarker that indirectly reflects gut microbiota health in relation to dietary intake, particularly in individuals following a PBD. Its potential application in precision medicine holds promise for enhancing risk stratification, guiding therapeutic interventions, and improving long-term cardiovascular outcomes in patients with cardiometabolic disorders
Keywords
TMAO, Regression atherosclerosis, Restenosis, Heart failure, Plant-based diet, Gut microbiota, Bethsaida Hospital, Prof. Dasaad Mulijono, Diet adherence monitoring, Prodia Laboratory Indonesia
TMAO, Regression atherosclerosis articles, Restenosis articles, Heart failure articles, Plant-based diet articles, Gut microbiota articles, Bethsaida Hospital articles, Prof. Dasaad Mulijono articles, Diet adherence monitoring articles, Prodia Laboratory Indonesia articles.
Article Details
Introduction
Cardiovascular diseases remain the leading cause of mortality globally and in Indonesia [1-5]. Traditional biomarkers, such as low-density lipoprotein (LDL) cholesterol and C-reactive protein (CRP), have been helpful but often insufficient in capturing the complexity of cardiovascular risk, particularly concerning diet and gut microbiota. TMAO, a metabolite produced by gut microbiota from dietary choline, phosphatidylcholine, and carnitine, has been strongly associated with adverse cardiovascular outcomes [6-20]. However,despite its growing significance, access to clinical TMAO testing in Indonesia was non-existent until 2024.
Historical Background
In a determined effort to bring advanced preventive diagnostics to Indonesia, Prof. Dasaad Mulijono initiated collaboration efforts with several major private laboratories. Most declined due to a lack of market awareness and perceived low demand. Only Prodia, Indonesia’s largest private diagnostic laboratory, recognized the potential clinical and scientific value of TMAO and agreed to invest in the equipment and training necessary for high-sensitivity liquid chromatography-mass spectrometry (LC-MS/MS) testing.
Bethsaida Hospital subsequently became the first healthcare institution in Indonesia to routinely offer clinical TMAO testing as part of its integrative cardiovascular care strategy.
TMAO and Cardiovascular Disease: Scientific Evidence
Elevated plasma TMAO levels have been independently associated with:
- • 3.1 Atherosclerosis: TMAO promotes foam cell formation and endothelial dysfunction [6,10-15,18,20].
- • 3.2 Restenosis: We postulated that patients with higher TMAO levels post-percutaneous interventions are at greater risk of adverse vascular remodelling and restenosis.
- • 3.3 Heart failure: TMAO exacerbates myocardial fibrosis and ventricular dysfunction [7,17].
These pathophysiological mechanisms are thought to be mediated through pro-inflammatory pathways, disruption of cholesterol metabolism, and altered platelet reactivity [6-20].
Diagnostic Value of TMAO Testing
Sensitivity and Specificity [21-23]
• Sensitivity: ~85% for predicting major adverse cardiovascular events (MACE) in high-risk patients. Among patients with increased cardiovascular risk, 85% will show elevated TMAO.
• Specificity: ~78%, meaning that 78% of patients without increased CVD risk have normal TMAO levels. Depending on their diet, renal function, and microbiota
False Positives [21,24-26]
- • High meat, egg yolk, or fish consumption within 24–48 hours of testing.
- • Use of certain supplements (e.g., L-carnitine, choline).
- • Impaired renal
1.1 False Negatives [24,25,27]
- • Recent antibiotic use suppresses gut
- • Acute dietary changes not reflective of long-term patterns, meaning the patient fasted or recently started a PBD (short-term reduction).
- • There’s a transient drop due to medications of short-term behaviour changes.
1.2 Normal Reference Range [21,24,26]
- • ≤ 6 µmol/L in healthy individuals who usually adhere to a PBD.
- • Levels >10 µmol/L suggest increased cardiovascular risk and/or high intake of red meat or animal-based products.
Clinical Application of TMAO at Bethsaida Hospital
At Bethsaida, TMAO measurement is integrated into:
• Initial cardiovascular risk screening
- • Monitoring adherence to a PBD: Sustained TMAO levels within the normal range are used as an objective marker of dietary adherence and gut microbiota health.
- • Lifestyle intervention programs: Patients transitioning to a PBD typically exhibit a significant reduction in TMAO levels within 4–6 weeks, reinforcing behavioural
- • Research involving patients with atherosclerotic plaque regression, as documented by computed tomography coronary angiography (CTCA) and invasive coronary angiography.
- • Research involving patients post-DCB angioplasty, where TMAO is used to monitor the risk of restenosis.
Our Experiences at Bethsaida Hospital
Initial results at Bethsaida show that patients who adopted a PBD demonstrated a 60–80% reduction in TMAO within 6 weeks, correlating with improved metabolic function and lipid profile. Conversely, patients who reverted to animal- based diets experienced a re-elevation of TMAO and markers of inflammation.
Future Directions
- • Integration with AI-based dietary recommendation.
- • Longitudinal studies to track TMAO as a predictor for cardiovascular and chronic disease events in the Indonesian population.
- • Broadening role for TMAO as a marker of chronic systemic inflammation and metabolic dysfunction.
Long-Term Applications of TMAO Testing in Broader Clinical Settings
The long-term application of TMAO testing in broader clinical settings holds significant promise for reshaping preventive and therapeutic strategies across multiple specialties. As a non-invasive, metabolically informative biomarker, TMAO testing may evolve into a routine component of annual health check-ups, particularly for populations at risk of cardiometabolic diseases. In cardiology, beyond its current use in assessing restenosis and dietary adherence, TMAO testing could become integral in stratifying patients for aggressive lifestyle or pharmacologic interventions, thus optimizing resource allocation and improving patient outcomes. In nephrology, given TMAO’s accumulation in chronic kidney disease, its monitoring may offer early signals of renal dysfunction or progression risk. In endocrinology, elevated TMAO levels correlate with insulin resistance and systemic inflammation, thus supporting its use as an adjunct marker in managing type 2 diabetes mellitus and metabolic syndrome. Furthermore, in oncology, emerging research links gut dysbiosis and elevated TMAO to increased cancer risk, suggesting a future role in screening or prevention strategies. Paediatric and geriatric populations may also benefit from TMAO-guided dietary interventions, which can foster early microbiome optimization and delay age-related decline. As artificial intelligence (AI) and precision medicine platforms advance, TMAO values may be algorithmically integrated with genomics, metabolomics, and microbiome profiles to personalize diet plans, forecast disease trajectories, and monitor real-time treatment efficacy. With expanding access and decreasing testing costs, TMAO assessment could become as commonplace as lipid profiling, transforming it from a research biomarker into a standard clinical tool for proactive, nutrition-oriented, and microbiota- driven care across disciplines [28-31].
Conclusion
Bethsaida Hospital has pioneered the clinical use of TMAO testing in Indonesia, thanks to the visionary leadership of Prof. Dasaad Mulijono and a strategic collaboration with Prodia Laboratory. In addition to introducing TMAO testing, we are among the first in the region to adopt DCB technology as part of our advanced interventional cardiology program, with an expanding record of clinical success.
Ongoing research at our centre is focused on the relationship between TMAO levels, adherence to a PBD, and improvements in gut microbiota composition among cardiac patients. Notably, our clinical investigations have demonstrated that patients who maintain low TMAO levels, especially those adhering to a PBD, not only show reduced restenosis rates following DCB angioplasty but also exhibit regression of atherosclerotic plaques, as confirmed by CTCA and invasive coronary imaging.
TMAO offers a unique bridge between gut microbiota, dietary behaviour, and cardiovascular health, enabling a truly integrative and personalized approach to prevention and treatment. Currently, TMAO remains the only widely available clinical biomarker that indirectly assesses the health of the gut microbiota in the context of dietary intake, particularly polyphenolic dietary compounds (PBDs), making it an invaluable tool in lifestyle medicine. Its adoption may set a new paradigm for cardiovascular care in Southeast Asia, supporting long-term prevention strategies rooted in nutrition, microbiota modulation, and individualized care.
Conflict of Interest: The authors declare no conflict of interest.
References
- Di Cesare M, Perel P, Taylor S, Kabudula C, Bixby H, et al. The Heart of the World. Glob Heart 19 (2024): 11.
- Gaidai O, Cao Y, Loginov S. Global Cardiovascular Diseases Death Rate Prediction. Curr Probl Cardiol 48 (2023): 101622.
- Chong B, Jayabaskaran J, Jauhari SM, Chan SP, Goh R, et al. Global burden of cardiovascular diseases: projections from 2025 to 2050. Eur J Prev Cardiol (2024): zwae281.
- Muharram FR, Multazam CECZ, Mustofa A, Socha W, Andrianto, et al. The 30 Years of Shifting in The Indonesian Cardiovascular Burden-Analysis of The Global Burden of Disease J Epidemiol Glob Health 14 (2024): 193-212.
- Harmadha WSP, Muharram FR, Gaspar RS, Azimuth Z, Sulistya HA, et al. Explaining the increase of incidence and mortality from cardiovascular disease in Indonesia: A global burden of disease study analysis (2000-2019). PLoS One 18 (2023): e0294128.
- Amrein M, Li XS, Walter J, Wang Z, Zimmermann T, et al. Gut microbiota-dependent metabolite trimethylamine N-oxide (TMAO) and cardiovascular risk in patients with suspected functionally relevant coronary artery disease (fCAD). Clin Res Cardiol 111 (2022): 692-704.
- Zhou X, Jin M, Liu L, Yu Z, Lu X, Zhang H. Trimethylamine N-oxide and cardiovascular outcomes in patients with chronic heart failure after myocardial infarction. ESC Heart Fail 7 (2020): 188-193.
- Guasti L, Galliazzo S, Molaro M, Visconti E, Pennella B, et al. TMAO as a biomarker of cardiovascular events: a systematic review and meta-analysis. Intern Emerg Med 16 (2021): 201-207.
- ChenG,HeL,DouX,LiuT.AssociationofTrimethylamine- N-Oxide Levels with Risk of Cardiovascular Disease and Mortality among Elderly Subjects: A Systematic Review and Meta-Analysis. Cardiorenal Med 12 (2022): 39-54.
- Canyelles M, Borràs C, Rotllan N, Tondo M, Escolà-Gil JC, et Gut Microbiota-Derived TMAO: A Causal Factor Promoting Atherosclerotic Cardiovascular Disease? Int J Mol Sci 24 (2023): 1940.
- Xie G, Yan A, Lin P, Wang Y, Guo L. Trimethylamine N-oxide-a marker for atherosclerotic vascular disease. Rev Cardiovasc Med 22 (2021): 787-797.
- Lee Y, Nemet I, Wang Z, Lai HTM, de Oliveira Otto MC, et al. Longitudinal Plasma Measures of Trimethylamine N-Oxide and Risk of Atherosclerotic Cardiovascular Disease Events in Community-Based Older J Am Heart Assoc 10 (2021): e020646.
- Wang B, Qiu J, Lian J, Yang X, Zhou J. Gut Metabolite Trimethylamine-N-Oxide in Atherosclerosis: From Mechanism to Therapy. Front Cardiovasc Med 8 (2021):
- Wang M, Li XS, Wang Z, de Oliveira Otto MC, Lemaitre RN, et al. Trimethylamine N-oxide is associated with long-term mortality risk: the multi-ethnic study of atherosclerosis. Eur Heart J 44 (2023): 1608-1618.
- Spasova N, Somleva D, Krastev B, Ilieva R, Borizanova A, et al. Association of the trimethylamine N-oxide with cardiovascular risk and vascular alterations in middle- aged patients with risk factors for cardiovascular Biosci Rep 44 (2024): BSR20232090.
- Latif F, Mubbashir A, Khan MS, Shaikh Z, Memon A, et al. Trimethylamine N-oxide in cardiovascular disease: Pathophysiology and the potential role of Life Sci 361 (2025): 123304.
- Jarmukhanov Z, Mukhanbetzhanov N, Kozhakhmetov S, Nurgaziyev M, Sailybayeva A, et al. The association between the gut microbiota metabolite trimethylamine N-oxide and heart failure. Front Microbiol 15 (2024): 1440241.
- Yu X, Wang Y, Yang R, Wang Z, Wang X, et al. Trimethylamine N-oxide predicts cardiovascular events in coronary artery disease patients with diabetes mellitus: a prospective cohort study. Front Endocrinol (Lausanne) 15 (2024): 1360861.
- Hou CY, Chen YW, Hazeena SH, Tain YL, Hsieh CW, et Cardiovascular risk of dietary trimethylamine oxide precursors and the therapeutic potential of resveratrol and its derivatives. FEBS Open Bio 14 (2024): 358-379.
- Sun Y, Lin X, Liu Z, Hu L, Sun P, et al. Association between plasma trimethylamine N-oxide and coronary heart disease: new insights on sex and age differences. Front Cardiovasc Med 11 (2024): 1397023.
- Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, et Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 368 (2013): 1575- 1584.
- Senthong V, Wang Z, Li XS, Fan Y, Wu Y, et Intestinal Microbiota-Generated Metabolite Trimethylamine-N- Oxide and 5-Year Mortality Risk in Stable Coronary Artery Disease: The Contributory Role of Intestinal Microbiota in a COURAGE-Like Patient Cohort. J Am Heart Assoc 5 (2016): e002816.
- Cardona A, O'Brien A, Bernier MC, Somogyi A, Wysocki VH, et Trimethylamine N-oxide and incident atherosclerotic events in high-risk individuals with diabetes: an ACCORD trial post hoc analysis. BMJ Open Diabetes Res Care 7 (2019): e000718.
- Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med 19 (2013): 576-585.
- Cho CE, Caudill MA. Trimethylamine-N-Oxide: Friend, Foe, or Simply Caught in the Cross-Fire? Trends Endocrinol Metab 28 (2017): 121-130.
- Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472 (2011): 57-63.
- Velasquez MT, Ramezani A, Manal A, Raj DS. Trimethylamine N-Oxide: The Good, the Bad and the Unknown. Toxins 8 (2016): 326.
- Gatarek P, Kaluzna-Czaplinska J. Trimethylamine-N- oxide (TMAO) in human health. EXCLI J 20 (2021): 301-319.
- Jaworska K, Kopacz W, Koper M, Ufnal Microbiome- Derived Trimethylamine N-Oxide (TMAO) as a Multifaceted Biomarker in Cardiovascular Disease:Challenges and Opportunities. Int J Mol Sci 25 (2024): 12511.
- Liu J, Ge P, Luo Y, Sun Z, Luo X, et Decoding TMAO in the Gut-Organ Axis: From Biomarkers and Cell Death Mechanisms to Therapeutic Horizons. Drug Des Devel Ther 19 (2025): 3363-3393.
- Caradonna E, Abate F, Schiano E, Paparella F, Ferrara F, et Trimethylamine-N-Oxide (TMAO) as a Rising-Star Metabolite: Implications for Human Health. Metabolites 15 (2025): 220.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 