How Plants Became Cardiology’s Most Powerful Medicine in Indonesia
Prof. Dasaad Mulijono1,2,3
1Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia
2Indonesian College of Lifestyle Medicine, Indonesia
3Department of Cardiology, Faculty of Medicine, Prima University, Medan, Indonesia
*Corresponding author: Prof. Dasaad Mulijono, Department of Cardiology, Bethsaida Hospital
Received: 24 June 2025; Accepted: 02 July 2025; Published: 04 July 2025
Article Information
Citation: Dasaad Mulijono. How Plants Became Cardiology’s Most Powerful Medicine in Indonesia. Cardiology and Cardiovascular Medicine 9 (2025): 221-226.
View / Download Pdf Share at FacebookAbstract
Seven years ago, at Bethsaida Hospital in Indonesia, Professor Dasaad Mulijono pioneered the integration of a plant-based diet (PBD) into routine cardiac care—a paradigm shift that has dramatically improved outcomes for patients with chronic and cardiovascular diseases. By synergizing conventional medical therapies with intensive nutritional education and sustainable lifestyle interventions, we have witnessed clinical recoveries that were once deemed improbable.
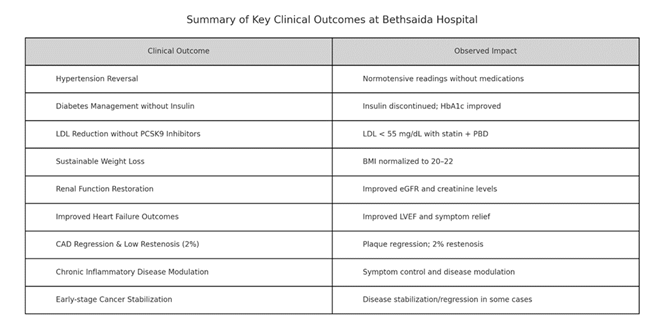
Patients have experienced remarkable reversals of hypertension, insulinindependent glycaemic control in diabetes, normalization of renal function, and substantial improvements in heart failure symptoms and ejection fraction. Atherosclerotic plaque regression is frequently observed in follow-up CT coronary angiography (CTCA) and coronary angiography. As a breakthrough achievement, our restenosis rates following drug-coated balloon (DCB) therapy are remarkably low, around 2%, compared to the 10–20% typically reported in conventional centers. Sustained weight normalization is routinely achieved, and even complex conditions such as autoimmune disorders and early-stage malignancies have shown signs of stabilization or improvement under this holistic approach.
This article presents our real-world clinical outcomes, elucidates the underlying mechanisms driving these transformations, and addresses the prevailing scepticism within the medical community. We also explore the emerging role of artificial intelligence (AI) in tailoring nutritional interventions and enhancing patient engagement. Our intention is not to seek acclaim but to inspire broader adoption of this evidence-based, patient-centered model of care—one that is not only effective but also profoundly transformative.
Keywords
Plaque Regression; Mitigating Restenosis; Plant-Based Diet; Lifestyle Medicine; Artificial Intelligence; Bethsaida Hospital; Prof. Dasaad Mulijono; Patient Education
Plaque Regression articles; Mitigating Restenosis articles; Plant-Based Diet articles; Lifestyle Medicine articles; Artificial Intelligence articles; Bethsaida Hospital articles; Prof. Dasaad Mulijono articles; Patient Education articles.
Article Details
1. Introduction
The global burden of chronic non-communicable diseases is rising, with cardiovascular diseases remaining the leading cause of death worldwide. While pharmacological management has improved outcomes, achieving long-term disease reversal and empowering patients remains a significant challenge. At Bethsaida Hospital, we have adopted an integrative approach centred around PBD. Our experience suggests that chronic disease reversal is possible when lifestyle, particularly diet, is addressed with the same intensity as pharmacotherapy.
2. Clinical Outcomes at Bethsaida Cardiac Centre
We are pleased to share the remarkable outcomes achieved at the Cardiology Centre of Bethsaida Hospital in Tangerang, Indonesia, where a PBD has been integrated into our standard cardiac care protocols for nearly seven years. This initiative represents a pioneering effort in Indonesia, marking the first systematic incorporation of evidence-based nutritional therapy into cardiovascular clinical practice.
Despite these compelling clinical outcomes, the broader medical community has largely remained unaware of our advancements due to several limiting factors. Internationally, research originating from Indonesia often receives limited attention, partly attributed to perceptions of lower research quality resulting from systemic constraints in funding and infrastructure. Additionally, locally we have encountered significant scepticism among medical peers—an issue that merits further examination in a forthcoming publication.
Nevertheless, the transformative impact of adopting a PBD on our patients' health outcomes has been unequivocal. In the sections that follow, we present real-world testimonials and clinical data underscoring the substantial benefits of this nutritional intervention in reversing or stabilizing chronic cardiovascular conditions. We aim to make meaningful, experience-based contributions to the global discourse on nutrition and cardiovascular care, promoting the broader adoption of this potentially life-saving approach.
3. Patient Demographics and Baseline Clinical Characteristics
Over the past seven years, more than 3,000 patients have participated in the plant-based lifestyle intervention program at Bethsaida Hospital’s Cardiology Centre. The majority (approximately 68%) were male, aged between 45 and 83 (mean age 61 ± 9.4 years). Most patients presented with established cardiovascular disease, including chronic coronary syndrome (CCS) and a history of percutaneous coronary intervention (PCI). The most prevalent comorbidities included hypertension (82%), type 2 diabetes mellitus (33%), dyslipidaemia (98%), obesity (18%), with a mean body mass index (BMI) above 30 kg/m² and overweight (68%) with BMI between 25-29.9 kg/m2. Additionally, 4% of patients had evidence of renal impairment (eGFR <60 mL/min/1.73 m²) at baseline. Many were refractory to multiple pharmacological therapies or had failed to achieve adequate metabolic control with standard medical care.
The patient cohort represents a real-world Indonesian population, predominantly from urban and peri-urban areas, with a range of socioeconomic backgrounds, including middle to lower socioeconomic levels. All participants received structured, multidisciplinary support that encompassed nutritional counselling, peer group education, and AI-assisted engagement tools. Serial laboratory evaluations, coronary CT angiography, and echocardiography were routinely employed to monitor therapeutic progress.
- Hypertension Reversal Without Medications
Numerous patients have achieved normotensive readings without antihypertensive medications. By adopting a PBD rich in potassium, magnesium, and nitric oxide (NO)- boosting greens while avoiding sodium-laden animal products, blood pressure normalization was observed within weeks to months. - Diabetes Management Without Insulin
Many type 2 diabetes mellitus (T2DM) patients have successfully discontinued insulin while maintaining glycaemic control with minimal or no oral antidiabetic medications. Haemoglobin A1c (HbA1c) values have improved significantly, and patients report increased energy and enhanced quality of life. - Low-density lipoprotein cholesterol (LDL) Reduction Without PCSK9 Inhibitors
Patients receiving high-intensity statins and ezetimibe in conjunction with a proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor have experienced profound reductions in LDL-C, eliminating the need for additional therapy. The diet’s high fibre content and absence of saturated fats contribute significantly to lipid regulation. - Sustainable Weight Loss
Overweight and obese individuals who adopt the PBD consistently reach an ideal body mass index (BMI) of 20–22 without calorie restriction. The high satiety index and nutrient density of plant foods encourage natural portion control. - Renal Function Restoration
Patients with mild to moderate chronic kidney disease (CKD) have shown significant improvement or normalization of serum creatinine and glomerular filtration rate (GFR), which prevents the need for dialysis and stabilizes kidney function. - Improved Heart Failure Outcomes
In patients with heart failure with reduced ejection fraction (HFrEF), we have observed a substantial improvement in symptoms and left ventricular ejection fraction when a PBD was incorporated alongside standard heart failure therapy. - Coronary Artery Disease (CAD) Regression and Exceptional Restenosis Rates
Our CAD patients often demonstrate angiographic regression of plaques, supported by lifestyle modification and optimal pharmacotherapy. Our DCB restenosis rate is just 2%, starkly contrasting with the 10–20% observed in other centres. - Other Chronic Inflammatory Conditions
Patients with autoimmune diseases, psoriasis, and other chronic inflammatory conditions report symptom improvement and disease modulation under a plant-based regimen. Some patients with early-stage cancers have achieved disease stabilization or regression.
4. Molecular and Physiological Mechanisms of Disease Improvement through a PBD
A growing body of scientific literature supports using a PBD as a powerful therapeutic approach for chronic diseases. Studies have consistently demonstrated its effectiveness in reversing hypertension [1-5] and T2DM [6-13], often eliminating the need for long-term pharmacological intervention. A PBD has also been shown to significantly lower LDL cholesterol levels—sometimes to ultra-low targets—contributing to the prevention and regression of atherosclerosis [14-20].
In cardiometabolic health, a PBD supports sustainable weight loss and achieving an optimal BMI [21-30]. It has shown promise in reversing early to moderate stages of chronic kidney disease, improving renal function without additional medication burden [31-43]. Dietary intervention in patients with heart failure has been shown to improve cardiac function and provide symptom relief [44-50].
Furthermore, emerging evidence supports the role of PBD in reducing atherosclerosis [51-61] and restenosis rates following DCB angioplasty—a critical advancement in post-interventional care. Beyond cardiology, this dietary approach has also contributed to clinical improvement or stabilization in various chronic inflammatory conditions [62-64], including autoimmune disorders [65-70] and some early-stage cancers, where it may help prevent progression and keep the disease localized [71-76].
These findings underscore PBD's broad therapeutic potential and the urgent need to integrate it into mainstream medical practice as a foundational element of chronic disease management. This paper provides a brief overview of the mechanisms by which PBD exerts its benefits across the various conditions discussed.
A PBD improves hypertension by enhancing NO production, lowering sodium, and reducing inflammation. In diabetes, it improves insulin sensitivity, preserves beta-cell function, and supports gut microbiota. For lipid disorders, it lowers LDL through reduced absorption and increased clearance. In obesity, it promotes satiety and reduces inflammation. For CKD, it reduces intraglomerular pressure and renal toxins. Heart failure outcomes improve through reduced afterload and inflammation. CAD regression is driven by improved endothelial function and reduced smooth muscle proliferation. Chronic inflammatory diseases benefit from reduced cytokines and improved immune modulation. Cancer risk is mitigated by lower IGF-1 levels, inhibition of angiogenesis, and enhanced apoptosis.
5. Addressing the Reluctance in the Medical Community
Despite compelling clinical outcomes and a growing body of scientific literature supporting plant-based nutrition, many healthcare professionals remain hesitant to embrace this approach within standard medical practice. Several interrelated factors contribute to this reluctance [71-79].
- Limited Nutritional Education:
Medical training worldwide, including in Indonesia, allocates a minimal amount of time to nutrition education. As a result, most physicians graduate with little to no formal understanding of how dietary interventions can prevent, treat, or reverse chronic diseases. Without foundational knowledge, many feel unprepared to counsel patients on plant-based diets, let alone integrate them into treatment plans. - Perceived Patient Non-Compliance:
There is a widespread belief that patients will not adhere to a PBD, especially in cultures where meat, dairy, and processed foods are deeply ingrained in daily life and social rituals. This perception often leads to therapeutic nihilism, where clinicians pre-emptively dismiss the potential of lifestyle change without even attempting an intervention. - Time Constraints and Systemic Pressures:
The current structure of healthcare systems—particularly fee-for-service models—prioritizes quick consultations, pharmacologic solutions, and procedural interventions. Time-intensive counselling on nutrition and lifestyle is often undervalued, inadequately reimbursed, or not reimbursed at all. This economic model disincentivizes preventive approaches that require sustained engagement. - Lack of Familiarity with the Evidence Base:
Although the evidence supporting plant-based nutrition is robust and expanding, it remains underrepresented in mainstream medical journals and conferences. Physicians who rely on traditional sources for continuing education may not be exposed to the most current research or dismiss nutrition-based studies as inferior to pharmaceutical trials due to differences in study design and funding. - Cultural Bias and Personal Habits:
Like their patients, physicians are influenced by cultural norms and personal habits. If a clinician does not personally follow a plant-based lifestyle, it may be psychologically or ethically challenging to recommend it to patients. Some may even feel that doing so would imply criticism of their lifestyle choices. - Influence of Industry and Institutional Norms:
The pharmaceutical, medical device, and food industries have a substantial influence on medical education, hospital policies, and clinical practice guidelines. This can create a subtle (or overt) bias against interventions threatening established revenue streams. Furthermore, hospitals often serve processed foods or animal products, reinforcing the perception that diet is a secondary concern. - Fear of Legal or Professional Repercussions:
In settings where PBDs are not yet standard of care, some physicians may fear legal risk or professional criticism if they recommend a diet perceived as “alternative” or “unconventional.” They may worry about liability should a patient’s condition not improve or complications arise, despite overwhelming evidence that a well-planned PBD is safe and effective. - Scepticism and the "Too Good to Be True" Phenomenon:
When physicians encounter stories of disease reversal through diet, whether hypertension, T2DM, or even coronary artery disease, the results can seem too dramatic to be credible. There is a natural scepticism, especially among practitioners trained to rely on pharmacologic or interventional solutions. Some view lifestyle medicine as anecdotal or fringe, rather than a legitimate clinical discipline grounded in evidence. - Inertia and Comfort with Familiar Protocols:
Changing clinical practice requires new knowledge and the willingness to unlearn long-standing beliefs. For many, the comfort of familiar protocols—such as prescriptions, procedures, and clinical pathways—outweighs the perceived benefits of adopting a more proactive, nutrition-based approach. Shifting this mindset requires compelling data and strong leadership. - Emotional Burnout and Therapeutic Fatigue:
Paradoxically, some physicians experience emotional fatigue after years of treating lifestyle-related diseases with minimal long-term success. This burnout can lead to cynicism about the potential for change in themselves and their patients. Introducing a plant-based approach may feel like another idealistic solution doomed to fail for such clinicians.
We believe that data-driven results, compelling patient testimonials, extensive publications, and institutional leadership can begin to shift this mindset. As more centres demonstrate consistent, reproducible outcomes using plant-based interventions, scepticism will fade, replaced by curiosity and conviction. By addressing these barriers openly and systematically, we aim to foster a more patient-centered, preventive, and evidence-based model of care.
6. The Role of AI in PBD Nutrition Education
AI has played a crucial role in our program by supporting patients through:
- • Personalized plant-based recipe generation
• Nutritional education tailored to individual health conditions
• Real-time Q&A support for diet-related inquiries
AI offers a powerful counterbalance in an era when social media platforms like YouTube and TikTok are saturated with influencers promoting unbalanced and often unhealthy animal-based dietary advice. Thanks to advances in AI technology, patients now have access to accurate, personalized, and evidence-based nutrition education, bridging the knowledge gap and empowering patients and clinicians to make informed dietary decisions. We envision AI as an indispensable tool in the future of preventive and lifestyle medicine [80–82].
7. Conclusion
The clinical transformation observed at Bethsaida Hospital challenges the traditional paradigm that chronic cardiometabolic diseases are irreversible and destined for lifelong pharmacotherapy. Our experience reaffirms a growing body of scientific evidence that a well-structured PBD can manage and often reverse diseases once considered progressive. When implemented within a multidisciplinary framework alongside evidence-based medical therapy, nutrition becomes a powerful therapeutic tool capable of restoring physiological function across multiple organ systems.
Despite these outcomes, resistance within the medical community persists, often rooted in outdated education, perceived patient non-compliance, or systemic inertia. We contend that such reluctance must be addressed through scientific discourse, updated curricula, and practical implementation models. Moreover, the advent of AI presents a unique opportunity to democratize access to evidence-based nutrition education, personalize patient engagement, and scale interventions beyond institutional boundaries.
This paper is not a proclamation of singular success, but a call to the global medical community: to investigate, replicate, and refine this model of care. Chronic disease reversal through lifestyle medicine is not theoretical—it is happening. And it deserves its rightful place at the forefront of 21st-century healthcare.
8. Conflict of Interest: The authors declare no conflict of interest.
9. References
- Alexander S, Ostfeld RJ, Allen K, Williams KA. A plant-based diet and hypertension. J Geriatr Cardiol 14 (2017): 327-330.
- Tomé-Carneiro J, Visioli F. Plant-Based Diets Reduce Blood Pressure: A Systematic Review of Recent Evidence. Curr Hypertens Rep 25 (2023): 127-150.
- Joshi S, Ettinger L, Liebman SE. Plant-Based Diets and Hypertension. Am J Lifestyle Med 14 (2019): 397-405.
- Charles JA, Habibullah NK, Bautista S, Davis B, Joshi S, Hull SC. Planting the Seed for Blood Pressure Control: The Role of Plant-Based Nutrition in the Management of Hypertension. Curr Cardiol Rep 26 (2024): 121-134.
- Gibbs J, Gaskin E, Ji C, Miller MA, Cappuccio FP. The effect of plant-based dietary patterns on blood pressure: a systematic review and meta-analysis of controlled intervention trials. J Hypertens 39 (2021): 23-37.
- McMacken M, Shah S. A plant-based diet for the prevention and treatment of type 2 diabetes. J Geriatr Cardiol 14 (2017): 342-354.
- Yang X, Li Y, Wang C, Mao Z, Chen Y, et al. Association of plant-based diet and type 2 diabetes mellitus in Chinese rural adults: The Henan Rural Cohort Study. J Diabetes Investig 12 (2021): 1569-1576.
- Pollakova D, Andreadi A, Pacifici F, Della-Morte D, Lauro D, et al. The Impact of Vegan Diet in the Prevention and Treatment of Type 2 Diabetes: A Systematic Review. Nutrients 13 (2021): 2123.
- Jardine MA, Kahleova H, Levin SM, Ali Z, Trapp CB, et al. Plant-Based Eating Pattern for Type 2 Diabetes Prevention and Treatment: Efficacy, Mechanisms, and Practical Considerations. Adv Nutr 12 (2021): 2045-2055.
- Ansari P, Khan JT, Chowdhury S, Reberio AD, Kumar S, et al. Plant-Based Diets and Phytochemicals in the Management of Diabetes Mellitus and Prevention of Its Complications: A Review. Nutrients 16 (2024): 3709.
- Barnard ND, Cohen J, Jenkins DJ, Turner-McGrievy G, Gloede L, et al. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. Am J Clin Nutr 89 (2009): 1588S-1596S.
- Guest NS, Raj S, Landry MJ, Mangels AR, Pawlak R, et al. Vegetarian and Vegan Dietary Patterns to Treat Adult Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv Nutr 15 (2024): 100294.
- Panigrahi G, Goodwin SM, Staffier KL, Karlsen M. Remission of Type 2 Diabetes After Treatment With a High-Fiber, Low-Fat, Plant-Predominant Diet Intervention: A Case Series. Am J Lifestyle Med 17 (2023): 839-846.
- Polesel J, Di Maso M, Esposito G, Vitale S, Palumbo E, et al. A Plant-Based Cholesterol-Lowering Diet Score Correlates with Serum LDL-Cholesterol Levels. Nutrients 16 (2024): 495.
- Koch CA, Kjeldsen EW, Frikke-Schmidt R. Vegetarian or vegan diets and blood lipids: a meta-analysis of randomized trials. Eur Heart J 44 (2023): 2609-2622.
- Thomas MS, Calle M, Fernandez ML. Healthy plant-based diets improve dyslipidemias, insulin resistance, and inflammation in metabolic syndrome. A narrative review. Adv Nutr 14 (2023): 44-54.
- Koutentakis M, Surma S, Rogula S, Filipiak KJ, Gasecka A. The Effect of a Vegan Diet on the Cardiovascular System. J Cardiovasc Dev Dis 10 (2023): 94.
- Wang T, Masedunskas A, Willett WC, Fontana L. Vegetarian and vegan diets: benefits and drawbacks. Eur Heart J 44 (2023): 3423-3439.
- Diab A, Dastmalchi LN, Gulati M, Michos ED. A Heart-Healthy Diet for Cardiovascular Disease Prevention: Where Are We Now? Vasc Health Risk Manag 19 (2023): 237-253.
- Trautwein EA, McKay S. The Role of Specific Components of a Plant-Based Diet in Management of Dyslipidemia and the Impact on Cardiovascular Risk. Nutrients 12 (2020): 2671.
- Najjar RS, Feresin RG. Plant-Based Diets in the Reduction of Body Fat: Physiological Effects and Biochemical Insights. Nutrients 11 (2019): 2712.
- Greger M. A Whole Food Plant-Based Diet Is Effective for Weight Loss: The Evidence. Am J Lifestyle Med 14 (2020): 500-510.
- Ahmad SR. Plant-based diet for obesity treatment. Front Nutr 9 (2022): 952553.
- Remde A, DeTurk SN, Almardini A, Steiner L, Wojda T. Plant-predominant eating patterns—how effective are they for treating obesity and related cardiometabolic health outcomes? A systematic review. Nutr Rev 80 (2022): 1094-1104.
- Bassin SR, Ferreira De Carvalho J, Gulati M. A review of plant-based diets for obesity management. Endocr Pract 30 (2024): 779-789.
- Jakše B, Jakše B, Pinter S, Pajek J, Fidler Mis N. Whole-food plant-based lifestyle program and decreased obesity. Am J Lifestyle Med 16 (2020): 260-270.
- Ivanova S, Delattre C, Karcheva-Bahchevanska D, Benbasat N, Nalbantova V, et al. Plant-based diet as a strategy for weight control. Foods 10 (2021): 3052.
- Campbell EK, Fidahusain M, Campbell TM II. Evaluation of an eight-week whole-food plant-based lifestyle modification program. Nutrients 11 (2019): 2068.
- Bolori P, Setaysh L, Rasaei N, Jarrahi F, Yekaninejad MS, Mirzaei K. Adherence to a healthy plant diet may reduce inflammatory factors in obese and overweight women—a cross-sectional study. Diabetes Metab Syndr 13 (2019): 2795-2802.
- Chen Z, Schoufour JD, Rivadeneira F, Lamballais S, Ikram MA, et al. Plant-based diet and adiposity over time in a middle-aged and elderly population: the Rotterdam study. Epidemiology 30 (2019): 303-310.
- Joshi S, McMacken M, Kalantar-Zadeh K. Plant-based diets for kidney disease: a guide for clinicians. Am J Kidney Dis 77 (2021): 287-296.
- Zarantonello D, Brunori G. The role of plant-based diets in preventing and mitigating chronic kidney disease: more light than shadows. J Clin Med 12 (2023): 6137.
- Adair KE, Bowden RG. Ameliorating chronic kidney disease using a whole food plant-based diet. Nutrients 12 (2020): 1007.
- Torreggiani M, Fois A, Lippi F, Attini R, Longhitano E, et al. Plant-based diets for CKD patients: fascinating, trendy, but feasible? A green nephrology perspective. Clin Kidney J 16 (2022): 647-661.
- Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Grams ME, et al. Plant-based diets and incident CKD and kidney function. Clin J Am Soc Nephrol 14 (2019): 682-691.
- Stanford J, Stefoska-Needham A, Lambert K, Batterham MJ, Charlton K. Association between plant-based diet quality and chronic kidney disease in Australian adults. Public Health Nutr 27 (1): e142.
- Heo S, Han M, Ryu H, Kang E, Kim M, et al. Compliance with a healthful plant-based diet is associated with kidney function in patients with autosomal dominant polycystic kidney disease. Nutrients 16 (2024): 2749.
- Swiatek L, Jeske J, Miedziaszczyk M. The impact of a vegetarian diet on chronic kidney disease (CKD) progression—a systematic review. BMC Nephrol 24 (2023): 168.
- Khan MA, Kassianos AJ, Hoy WE, Alam AK, Healy HG, et al. Promoting plant-based therapies for chronic kidney disease. J Evid Based Integr Med 27 (2022): 2515690X221079688.
- Goraya N, Wesson DE. Plant-based diets across the spectrum of kidney disease. Clin J Am Soc Nephrol 2025.
- Cases A, Cigarrán-Guldrís S, Mas S, Gonzalez-Parra E. Vegetable-based diets for chronic kidney disease? It is time to reconsider. Nutrients 11 (2019): 1263.
- Liebman SE, Baran A, Barnett TD, Campbell TM, Chen L, et al. The effects of a whole-food plant-based nutrition education program on blood pressure and potassium in chronic kidney disease: a proof-of-concept study. Nutrients 17 (2025): 779.
- Campbell TM, Liebman SE. Plant-based dietary approach to stage 3 chronic kidney disease with hyperphosphataemia. BMJ Case Rep 12 (2019): e232080.
- Kerley CP. A review of plant-based diets to prevent and treat heart failure. Card Fail Rev 4 (2018): 54-61.
- Choi EY, Allen K, McDonnough M, Massera D, Ostfeld RJ. A plant-based diet and heart failure: case report and literature review. J Geriatr Cardiol 14 (2017): 375-378.
- Allen KE, Gumber D, Ostfeld RJ. Heart failure and a plant-based diet: a case-report and literature review. Front Nutr 6 (2019): 82.
- Alasmre FA, Alotaibi HA. Plant-based diet: a potential intervention for heart failure. Cureus 12 (2020): e8282.
- Najjar RS, Montgomery BD. A defined, plant-based diet as a potential therapeutic approach in the treatment of heart failure: a clinical case series. Complement Ther Med 45 (2019): 211-214.
- Najjar RS, Gewirtz AT. Plant-based diets: a path to ending CVD as we know it? Nutrients 15 (2023): 3608.
- Kahleova H, Levin S, Barnard ND. Vegetarian dietary patterns and cardiovascular disease. Prog Cardiovasc Dis 61 (2018): 54-61.
- Braunwald E. The war against heart failure: the Lancet lecture. Lancet 385 (2014): 812-824.



 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 