Management of Hypertension and Diabetes Mellitus in Patients with Target Organ Damages and/or Previous Cardiovascular Diseases in Lebanon. Where do We Stand with Respect to International Guidelines?
Jeannot Kekedjian1, Raymond Challita1, Mikael Abi Abdallah1, Mirna N Chahine1,2*, Roland Asmar1,2
1Faculty of Medical Sciences, Lebanese University, Hadath, Lebanon
2Foundation-Medical Research Institutes (F-MRI®), Beirut, Lebanon
*Corresponding Authors: Prof. Mirna Chahine, Lebanese University, Faculty of Medical Sciences, Hadath, Lebanon
Received: 22 October 2020; Accepted: 30 October 2020; Published: 09 November 2020
Article Information
Citation: Jeannot Kekedjian, Raymond Challita, Mikael Abi Abdallah, Mirna N Chahine, Roland Asmar. Management of Hypertension and Diabetes Mellitus in Patients with Target Organ Damages and/or Previous Cardiovascular Diseases in Lebanon. Where do We Stand with Respect to International Guidelines?. Cardiology and Cardiovascular Medicine 4 (2020): 679-696.
View / Download Pdf Share at FacebookAbstract
Background: Hypertension and diabetes are major health problems worldwide. They can coexist together increasing the complication rates. The increased incidence of these complications in the Lebanese population reflects a poor disease control, consequently increased risk of death. Objective: The aim of this study was to assess Lebanese physicians’ compliance to international guidelines and their control on diabetes and hypertension.
Methods: Retrospective cross-sectional study was conducted on 750 Lebanese patients randomly selected from 6 university hospitals from January 2014 to August 2015. Patients were divided according to their medical history: 252 hypertensive, 249 diabetic, 249 both hypertensive and diabetic. All patients had target organ damages and were admitted to the hospitals.
Results: Our study showed the overuse of beta blockers in hypertensive and diabetic patients, while neglecting lifestyle modifications and the drug of choice for special populations. A proportion of 7% of hypertensive patients in the Lebanese population were untreated for their hypertension. The first line treatment for diabetic patients was respected in most of the patients. However, results showed those with diabetes were not properly controlled. Aspirin was only used in half of the patients, though all of them were high-risk with target organ damages.
Discussion: Results from this study in Lebanon indicate the absence of adherence to guidelines by the Lebanese physicians, especially in the management of hypertension where beta blockers were overused, in addition to the absence of control of diabetes and hypertension, which may be due to physicians’ non adherence to guidelines or patients’ noncompliance to medications.
Keywords
<p>Hypertension; Diabetes; Lebanon; Target organ damage; Guidelines; Treatment</p>
Article Details
1. Introduction
Hypertension (HTN) and Diabetes (DM) are major health problems worldwide. They can coexist together increasing the complication rates [1]. Many studies and researches were conducted to evaluate their complications, to find the best tools for diagnosis and management, to establish international guidelines to control them, and to assess physicians’ adherence to these guidelines. A study conducted on six hundred Lebanese physicians showed that their compliance with clinical practice guidelines was not always present [2]; another one showed poor agreement between the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) guidelines and clinical practice [3]. As for DM, the International DM Management Practice Study (IDMPS) demonstrated that Lebanese patients, with glycemic control reaching 29.6% only, were not adequately controlled or followed up, and further studies are to be done to evaluate adherence to international guidelines [4].
Unfortunately, there is a perception that physicians are doing an incomplete job in treating HTN and DM despite the availability of effective well-tolerated therapy [5]. This is highly critical since the presence of any of the four markers of organ damage, that are micro albuminuria, increased pulse wave velocity, left ventricular hypertrophy (LVH) and carotid plaques, can predict cardiovascular mortality independently, and this risk increases with the number of damaged organs [6]. Moreover, the adherence to management and self-care measures is sub-optimal resulting in high complication rates [7], the most common being heart disease by 27.8% [7].
There is an alarming prevalence of DM and pre-DM in the Lebanese population [8] along with an increased risk of cardiovascular diseases [9], which is a major manifestation of target organ damages (TOD) along with kidney disease. The increased incidence of these complications in the Lebanese population may reflect a poor control of HTN and DM, and consequently increased risk of death. There is no specific study in Lebanon regarding the adherence of Lebanese physicians to the international guidelines for HTN and DM in patients with TOD and/or previous cardiovascular diseases, whether the strategy they follow is based on guidelines or not, or whether it is successful in controlling patients’ blood pressure (BP) and glycaemia and ongoing organ damage. It is still unknown if the international guidelines should be adapted to the Lebanese population or be modified in order to help Lebanese physicians achieve ultimate goals and improve patients’ management. Accordingly, we conducted a study to assess Lebanese physicians’ compliance to international guidelines and their control on DM and HTN.
2. Methods
A cross-sectional retrospective multicentric study was conducted where 750 Lebanese patients were included. Patients were randomly selected from 6 hospitals: the academic Beirut Governmental University Hospital, Sacré-Coeur Hospital, Lebanese Geitaoui Hospital, Middle East Institute of Health-Bsalim Hospital, Mount-Lebanon Hospital, and Notre Dame du Liban Hospital, from January 2014 to August 2015. Certainly, before beginning our study, a document was sent to these hospitals requesting approval to access patients’ files by the ethics committee in these hospitals. Data was then collected and patients were divided into three different groups based on the information retrieved from their previous medical history section in their medical file.
Group 1: consisted of 252 patients known to have HTN.
Group 2: consisted of 249 patients known to have DM.
Group 3: consisted of 249 patients known to have both HTN and DM.
2.1 Inclusion criteria
- Patients should be hypertensive and have one or more of the TOD and/or previous cardiovascular diseases (CVD).
- Patients should be diabetic and have one or more of TOD and/or previous CVD.
- Patients should be diabetic and hypertensive and have one or more of the TOD and/or previous CVD.
NB: The TOD are LVH, asymptomatic atherosclerosis, microalbuminuria, renal dysfunction
2.2 Exclusion criteria
Patients with no HTN and/or no DM, no TOD and no CVD were excluded from the study.
2.3 Data collection
Collection of data started in January 2014 and ended in August 2015. For each patient, a case report form was filled out including demographic parameters, treatment options, and biologic values.
2.4 Statistical analysis
Data analysis was completed using SPSS version 22. Descriptive statistics were used to calculate the frequency, mean and standard deviation (SD) of the continuous variables and the frequency and percentages of the nominal variables. Bivariate analysis was used to assess the correlation between the study Groups and all the study variables using Chi-Square Test, Fisher’s Exact Test, Student t-test and ANOVA test. Two-sided p-values were calculated in all tests, with statistical significance set at p<0.05.
3. Results
3.1 Demographic characteristics
The study included 750 people, 420 (56%) men and 330 (44%) women. The most common age group for men and women are 60-69 and 70-79 respectively (Table 1).
3.2 Non-Pharmacological treatment
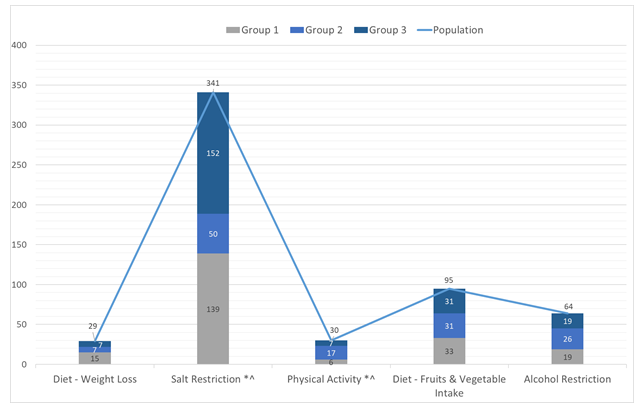
Salt restriction was the most common non-pharmacological treatment advised to patients (45.5%), followed by a diet rich in fruits and vegetables (12.7%), alcohol restriction (8.5%), physical activity (4%) and weight loss (3.9%). Salt restriction and physical activity have statistically significant differences between the diabetic group and the other groups (Figure 1). Indeed, salt restriction was significantly more advised to patients of group 1 (HTN) (40.7%, p< 0.05) and group 3 (both HTN and DM) (44.5%, p< 0.05) compared with patients of group 2 (DM) (14.6%). However, there was no statistical difference for salt restriction advised between patients of group 1 and 3. This shows that compared with DM patients, those with HTN or with both HTN and DM were highly and equally advised to restrict salt intake (Figure 1). On the contrary, physical activity was significantly more advised to patients of group 2 (56.6%) compared with patients of group 1 (20.0%) and group 3 (23.3%). However, there was no statistical difference for physical activity advised between patients of group 1 and 3. This shows that compared with patients with HTN or with both HTN and DM, those with DM were highly advised to perform a physical activity (Figure 1).
3.3 Pharmacological treatment
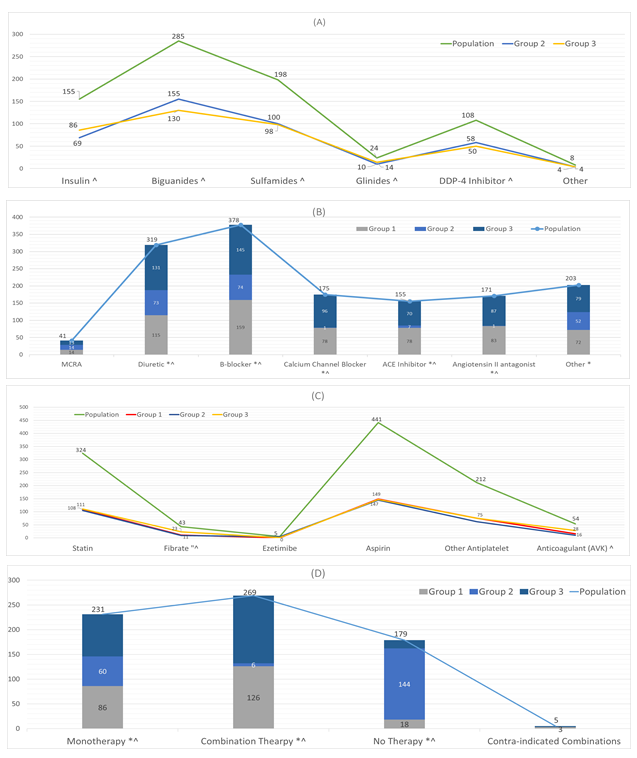
3.3.1 Anti-diabetes: The study included 498 patients with DM and with both DM and HTN (groups 2 and 3, respectively). The most commonly used anti-DM drugs were biguanides (59.2%), followed by sulfamides (39.8%), insulin (31.1%), DPP-4 inhibitors (21.7%), and glinides (4.8%). These 4 drugs showed statistically significant differences between both diabetic groups (Figure 2A). Compared with group 3 patients (DM and HTN), group 2 patients (DM) were using more significantly Biguanides (54.3%, p<0.05), Sulfamides (50.5%, p<0.05), and DDP-4 Inhibitor (53.7%, p<0.05). Compared with DM patients, those suffering from both DM and HTN were mostly prescribed to use Insulin (55.48%, p<0.05) and Glinides (58.33%, p<0.05) (Figure 2A).
3.3.2 Antihypertensive-Cardiovascular: The most common used antihypertensive and/or cardiovascular drugs were beta blockers BB (50.4%), followed by diuretics (42.5%), calcium channel blockers CCB (23.3%), angiotensin II antagonists ARB (22.8%), angiotensin converting enzyme inhibitors ACEI (20.7%), and mineralocorticoid receptor antagonists (MCRA) (5.5%). Various other drugs (e.g. peripheral vasodilators) were used in 27.1% of all patients. The following drugs have statistically significant differences between the diabetic group and other 5 drugs’ types: BB, diuretics, CCB, ARB, ACEI (Figure 2B). Apart from CCB that were used only by patients of groups 1 and 3, all other 4 drugs’ types were significantly more prescribed for patients of groups 1 and 3 compared with patients of group 2. There was no statistical significance between the use of these 4 drugs' types in patients of groups 1 & 3.
3.3.3 Other drugs: The most common hypolipidemic drugs used were statin (43.2%), followed by fibrate (5.7%), and ezetimibe (0.7%). A proportion of 58.8% of patients were on aspirin during the study, 28.3% were on other antiplatelets, and 7.2% on anticoagulants. Fibrates were more significantly prescribed for patients having both HTN and DM compared with DM patients or HTN patients; AVK were more prescribed for patients having both HTN and DM compared with DM patients. (Figure 2C).
3.3.4 Overall treatment: The study included 502 patients with HTN and with both DM and HTN (groups 1 and 3). Monotherapy was used in 46% of patients suffering from HTN and both from HTN and DM. Monotherapy was significantly more used in patients with HTN (37.2%, p< 0.05) and with both DM and HTN (36.7%, p< 0.05)) compared with patients with DM (25.9%). Combination therapy consisting of diuretic + ARB, diuretic + CCB, diuretic + ACEI, ARB + CCB, CCB + ACEI or BB + CCB was used in 53.5% of patients suffering from HTN and from both HTN and DM. Combination therapy was significantly more used in patients with HTN (46.8%, p< 0.05) and with both DM and HTN (50.9%, p< 0.05)) compared with patients with DM (2.2%). A total of 35 (7%) patients received no treatment at all. Contraindicated combinations (e.g. ARB with ACEI) were seen in 5 patients (Figure 2D).
3.3.5 Treatment for selected populations: The study included 130 elderly people with isolated HTN, of which 23 (17.7%) were treated by CCB and diuretics (p< 0.05 between both hypertensive groups 1 & 3). A total of 163 (32.7%) out of 498 diabetic patients received ARB or ACEI; however, this treatment was more significantly (95.1%, p<0.05) prescribed for patients of group 3, compared with patients of group 2 (4.9%). ACEI were also used in 67 (18.8%) out of 357 patients with nephropathy or proteinuria in patients of group 1 (37.3%, p<0.05) and 3 (55.2%, p< 0.05), compared with patients of group 2 (7.5%). In addition, the study included 33 patients with stroke and SBP ranging between 140 and 159mmHg, out of which 30 (90.9%) received antihypertensive medications; patients of group 3 were prescribed more antihypertensive medications than patients of group 2 (56.7 % vs 6.7%, p< 0.05) (Table 2). A total of 57 (69.5%) out of 82 patients with both HTN and myocardial infarction were on BB, 60 (18.2%) out of 329 patients with both HTN and coronary artery disease were on BB and CCB. The study found 104 people with both DM and systolic heart failure, out of which 12 (11.5%) were on ACEI and BB. Patients with heart failure that were already on BB and ARB or ACEI received MCRA in 44.4% of cases (8 out of 18) (Table 2).
3.4 Disease control
3.4.1 Biology: Many parameters were extracted from the patients’ medical files, such as glycemia, HbA1C, Total cholesterol, LDL, HDL, triglycerides, creatinine, and microalbuminuria. The average fasting blood glucose was 159 mg/dl for the population; 103 mg/dl for the hypertensive group, 187 mg/dl for both diabetic groups (p<0.05 group 1 vs groups 2 & 3). Glycosylated hemoglobin was in average 7.4% for the population; HbA1C was significantly (p<0.05) higher in the diabetic group (8.28%) compared with the hypertensive group (5.48%) and the hypertensive and diabetic group (7.88%). There was also a statistical difference between groups 1 and 3. Total cholesterol, LDL, triglycerides and microalbuminuria in the population were 171.38 mg/dl, 102.55 mg/dl, 193.64 mg/dl, and 384.9 mg/24h respectively, with absence of statistical difference among all groups of patients. Average levels of HDL cholesterol were 37.02 mg/dl, but were significantly lower in DM patients (34.12 mg/dl, p<0.05) and DM and HTN patients (36.62 mg/dl, p< 0.05) compared with the levels of HDL in patients with HTN (40.18 mg/dl). The average person had a creatinine of 1.28 mg/dl. The highest levels of creatinine were present in patients of group 3 (1.43 mg/dl) and this was statistically significant (p<0.05) when compared with creatinine levels of group 1 (1.11 mg/dl) and group 2 (1.32 mg/dl). Patients of group 3 had also higher levels of creatinine with the ones of patients of group 2 (p<0.05). These results showed that 1) Glycemia was mostly increased in diabetic patients; 2) HDL cholesterol was significantly decreased in diabetic patients; 3) HbA1C levels were significantly increased in DM patients and those with both HTN and DM , but the co-presence of HTN with DM may decrease levels of HbA1C when compared with those of patients with DM only; 4) Creatinine levels were increased in patients with DM and HTN and even more when both conditions (DM and HTN) were present simultaneously (Table 3).
3.4.2 Outcome following guidelines: Out of 750 patients included in our study, a total of 703 (93.7%) were on treatment for their HTN and/or DM. A proportion of 97.2% of patients with HTN received treatment for their condition and/or cardiovascular problems. This percentage was significantly higher than patients with DM (93.2%, p<0.05) and those with both HTN and DM (90.8%, p<0.05). In our study, blood pressure (BP), glycemia, and overall controls were defined following the guidelines (10, 11) such as for: Patients of group 1: SBP < 140mmHg and DBP < 90 mmHg; Patients of groups 2 and 3: SBP < 140 mmHg and DBP < 85 mmHg and fasting blood sugar (FBS) < 120 mg/dl or HbA1c < 7%). Our results showed that BP was controlled in 62.8% of all patients, and 56.1% of hypertensive patients. Glycemia was controlled in 30.7% of diabetic patients. Overall control was seen in 33.6% of the population, with statistically better overall control in patients with HTN (59.5%, p<0.05), compared with DM patients (22.08%) and with both HTN and DM patients (18.9%) (Table 4).
|
Age |
30-39 |
40-49 |
50-59 |
60-69 |
70-79 |
80-89 |
90-99 |
|
Male |
4 |
36 |
79 |
115 |
110 |
69 |
7 |
|
Female |
1 |
16 |
53 |
71 |
93 |
77 |
19 |
Table 1: Age-Gender Correlation of the Population.
Population (N=750); Group 1: HTN (N=252); Group 2: DM (N=249); Group 3: HTN & DM (N=249). *: p < 0.05 group 1 vs group 2; “: p< 0.05 group 1 vs group 3; ^: p< 0.05 group 2 vs group 3
Population (N=750); Group 1: HTN (N=252); Group 2: DM (N=249); Group 3: HTN & DM (N=249). *: p<0.05 group 1 vs group 2; “: p< 0.05 group 1 vs group 3; ^: p< 0.05 group 2 vs group 3; Monotherapy: Diuretic, BB, ACEI or ARB; Combination therapy: Diuretic + ARB, diuretic + CCB, diuretic + ACEI, ARB + CCB, CCB + ACEI or BB + CCB; Contra-indicated combinations: ARB + ACEI.
|
CONDITION |
TREATMENT |
N |
TREATED |
|||
|
Population |
Group 1 |
Group 2 |
Group 3 |
|||
|
Elderly (age≥65) with Isolated HTN (SBP≥140 and DBP<90)" |
CCB + diuretic |
130 |
23 (17.7%) |
9 (39.1%) |
0 |
14 (60.9%) |
|
Diabetic ^ |
ACEI or ARB |
498 |
163 (32.7%) |
0 |
8 (4.9%) |
155 (95.1%) |
|
Nephropathy or Proteinuria*^ |
ACEI |
357 |
67 (18.8%) |
25 (37.3%) |
5 (7.5%) |
37 (55.2%) |
|
Stroke and SBP 140-159 ^ |
Antihypertensive medications |
33 |
30 (90.9%) |
11 (36.7%) |
2 (6.7%) |
17 (56.7%) |
|
HTN + MI |
BB |
82 |
57 (69.5%) |
31 (54.4%) |
0 |
26 (45.6%) |
|
HTN + CAD |
BB + CCB |
329 |
60 (18.2%) |
29 (48.3%) |
0 |
31 (51.7%) |
|
DM + Systolic HF (EF < 40%) |
ACEI + BB |
104 |
12 (11.5%) |
0 |
4 (33.3%) |
8 (66.7%) |
|
HF (EF < 35%) on (ARB or ACEI) and BB |
MCRA |
18 |
8 (44.4%) |
4 (50.0%) |
0 |
4 (50.0%) |
Group 1: HTN; Group 2: DM; Group 3: HTN & DM. *: p<0.05 group 1 vs group 2; “: p<0.05 group 1 vs group 3; ^: p< 0.05 group 2 vs group 3; HTN: Hypertension; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; MI: Myocardial Infarction; CAD: Coronary Artery Disease; HF: Heart Failure; EF: Ejection Fraction; Elderly: age ≥ 65; Isolated HTN: SBP ≥ 140 and DBP < 90; Systolic HF: EF <40%
Table 2: Treatment of Selected Populations.
|
Glycemia (mg/dl) *” |
Population |
Group 1 |
Group 2 |
Group 3 |
|
552 (159.60; 76.17) |
180 (103.07; 20.18) |
187 (187.35; 79.48) |
185 (186.55; 77.16) |
|
|
HBA1C (%) *”^ |
493 (7.40; 1.99) |
128 (5.48; 0.70) |
181 (8.28; 1.89) |
184 (7.88; 1.79) |
|
Total Cholesterol (mg/dl) |
327 (171.38; 58.67) |
108 (175.35; 51.11) |
99 (164.93; 46.62) |
120 (173.13; 72.39) |
|
LDL (mg/dl) |
309 (102.55; 43.81) |
103 (108.85; 44.73) |
98 (99.68; 38.64) |
108 (99.15; 46.97) |
|
HDL (mg/dl) *” |
318 (37.02; 12.67) |
105 (40.18; 12.62) |
98 (34.12; 12.06) |
115 (36.62; 12.69) |
|
Triglycerides (mg/dl) |
324 (193.64; 318.32) |
106 (147.10; 81.61) |
99 (180.35; 112.75) |
119 (246.13; 505.98) |
|
Creatinine (mg/dl) *”^ |
729 (1.28; 1.12) |
244 (1.11; 0.95) |
244 (1.32; 1.21) |
241 (1.43; 1.17) |
|
Microalbuminuria (mg/24h) |
182 (384.90; 1210.43) |
51 (505.95; 2110.69) |
59 (294.48; 542.35) |
72 (373.25; 583.10) |
Group 1: HTN; Group 2: DM; Group 3: HTN & DM. *: p < 0.05 group 1 vs group 2; “: p< 0.05 group 1 vs group 3; ^: p< 0.05 group 2 vs group 3
Table 3: Biology, N (mean; SD).
|
Guidelines |
Population (N= 750) |
Group 1 (N= 252) |
Group 2 (N= 249) |
Group 3 (N= 249) |
|
Treatment Following Guidelines |
||||
|
Receiving Treatment *” |
703 |
245 |
232 |
226 |
|
Disease Control Following Guidelines |
||||
|
BP control *^ |
471 |
150 |
190 |
131 |
|
Glycemia Control |
154 |
0 |
73 |
81 |
|
Overall Control *” |
252 |
150 |
55 |
47 |
Group 1: HTN; Group 2: DM; Group 3: HTN & DM. *: p < 0.05 group 1 vs group 2; “: p< 0.05 group 1 vs group 3; ^: p< 0.05 group 2 vs group 3; Group 1: SBP < 140 mmHg and DBP < 90 mmHg; Groups 2 and 3: SBP < 140 mmHg and DBP < 85 mmHg and (FBS < 120 mg/dl or Hba1c < 7%)
Table 4: Outcome Following Guidelines.
4. Discussion
The study included 750 patients, divided into three subgroups according to their diagnosis (HTN, DM, or both). All patients’ charts were reviewed and the following information were extracted: their non pharmacological treatment, pharmacological treatment, and disease control at the end (blood pressure and glucose readings).
4.1 Lifestyle modifications
Our study showed an overall low rate of lifestyle modification in all patients, with comparable results with studies in Ethiopia [12]. This low rate may be due to several reasons: in addition to incomplete documentation and patients’ noncompliance, it can also be explained by improvement in health services and treatment of older adults according to a Brazilian national survey [13]. Several studies worldwide showed the importance of lifestyle changes: a Chinese study showed that long-term lifestyle intervention can be used as adjunctive therapy to improve the BP [14]; A randomized controlled trial (SMARTER) showed improvements in both HbA1c and insulin sensitivity [15]. With the high prevalence of modifiable risk factors among Americans with a family history of DM and/or CVD [16], a systematic review showed the necessity to continue to create high-quality interventions, not only to treat current symptoms of the disease but also to help prevent cardiovascular disease [17]. While a Japanese study showed the benefit of lifestyle modifications on the cardiovascular profile [18], the Look AHEAD long-term lifestyle intervention on the other hand did not significantly lower ECG signs of LVH in overweight and obese adults with type 2 DM [19].
4.2 Diabetes treatment and consequences
4.2.1 Insulin use in patients with diabetes and hypertension: We observed that more patients with HTN and DM were on insulin, than those with DM alone. This could be attributed to several reasons:
Insulin Resistance
HTN is often present as part of the metabolic syndrome of insulin resistance [20] that predicts type 2 DM. Moreover, insulin resistance is a prothrombotic state, leading to increased risk of cardiovascular events [21]. Sowers et al showed a role of insulin resistance in the development of HTN by an increase in vascular adhesion molecule expression, oxidative stress, inflammation, and decreased vascular nitric oxide levels, which promote vascular stiffness resulting in persistent HTN [22]. Several studies showed the benefit of insulin in patients with HTN: The Epidemiology of DM Intervention and Complications (EDIC) study demonstrated that intensive insulin therapy during the DM Control and Complications Trial (DCCT) reduced the long-term risk of developing HTN by 24% [23]. On the other hand, a study by Ferrannini et al showed that exogenous insulin may lead to HTN through vasoconstriction and sodium and fluid retention [24].
Incretin Mimetics
The GLP-1R agonists (also called incretin mimetics) increase insulin and glucagon production in the liver. Three GLP-1R agonists have been found to significantly reduce the risk of atherosclerotic cardiovascular disease ASCVD in adults with T2DM who are at high ASCVD risk [25].
4.2.2 Overuse of diuretics in diabetes: Some patients who have DM without HTN were on diuretics (Figure 2B), even though data from clinical trials showed that prolonged use of thiazide diuretics were associated with an increased incidence of type 2 DM compared with placebo or drugs such as ACEI, ARB or CCB [26]. This could be due to the association of other diseases requiring the use of diuretics such as heart failure. A study by Potier et al published in 2019 showed a significant increase in the risk of lower limb edema and lower limb amputation in patients with type 2 DM treated with diuretics [27]. On the other hand, a study by Scheen et al showed that the benefit of thiazide diuretics in reducing cardiovascular events outweighs the risk of worsening glucose control in type 2 DM and of new-onset DM in non-diabetic patients [28].
4.3 Hypertension treatment
4.3.1 Overuse of Beta Blockers: Beta Blockers (BB) accounted for the most commonly used antihypertensive cardiovascular drug (Figure 2B). According to guidelines, ACEI and ARBs were recommended as a first line therapy in patients with HTN and LVH [10]. However, studies in the literature concerning BB are diverse. Some try to justify their use, while others continue to consider the superiority of ACEI and ARBs. A study by Xing F, et al. [29] involving 2566 patients with HTN and LVH showed that BB may become the first line drug to be used in those patients, especially that BB may lead to LVH regression. Other studies involving larger populations are needed to validate those findings. On the other hand, a prospective Indian study by Ramaswamy et al. [30] showed the effectiveness of ACEI and ARBs in treating patients with HTN and LVH compared to BB and CCB. In our population the overuse of BB was associated with low rates of blood pressure control and increased recurrence and complication rates.
Although BB has shown to reduce cardiovascular mortality in diabetic and hypertensive patients especially after myocardial infarction [31], modern therapy of HTN emphasizes on the importance of the initiation of ACEI or ARB [10] in patients with TOD and/or DM. Moreover, only 69.5% of patients with myocardial infarction were on BB in our study (Table 2), which means that almost one third of patients with MI were not getting optimal treatment. BB or other drugs can be used in combination with ACEI or ARB to control HTN in diabetics [32]. Actually, different studies in Europe showed the underuse of ACEI and ARB (which can be considered as new drugs) and the overuse of BB [33] (which is similar to the issue we are dealing with in our Lebanese population).
4.3.2 Untreated patients: The study included 501 patients with HTN, 7% of which were left untreated (Figure 2D). These results are promising compared to some international studies reporting the same issue: A study in Congo showed that one third of screened patients had untreated HTN [34]. Another study in Germany showed that 12.6% of 2205 patients with HTN were untreated [35]. A study involving 3 European excellence centers for HTN demonstrated that 21.7% of 14229 patients were untreated [36]. These data are alarming, considering that untreated HTN is associated with increased cardiovascular risk.
4.4 The Problematic Underuse of Cardiovascular Drugs
4.4.1 The Underuse of ACE Inhibitors
4.4.1.1 ACE Inhibitors and DM: Our study reported that only 32% of those with DM were taking ARB or ACEI. These numbers were low considering the multiple controlled trials that established the importance of ACEI in delaying the progression of diabetic nephropathy [37]. A study published by Sumida et al in 2017 showed that reducing albuminuria in those with DM was associated with improved renal and cardiovascular outcomes [38]. A 2018 update by Umanath et al proved that RAS-blocking medications are the single best evidence-based therapy for diabetic nephropathy [39]. Moreover, a Canadian study showed that practice guidelines should reflect that ACEI remain the preferred RAAS inhibitor for high risk patients [40]. In contrast, another study in Taiwan showed that ARB use reduces the risk of stroke compared to ACEI in those with HTN and DM [41].
4.4.1.2 ACE Inhibitors and Proteinuria: Out of 357 patients in the study with proteinuria, only 18.8% were on ACEI. These results were surprisingly low, considering that CKD was contributed partly to the overactivity of RAAS [42], their blockers being recommended as first line treatment in all CKD hypertensive patients regardless of the association with DM [43]. A systematic review published in 2016 concluded that early initiation of ACEI reduced the risk of microalbuminuria in those with DM and normoalbuminuria [44]. Moreover, guidelines emphasized on the use of ACEI and ARB in patients with proteinuria. Thus, major studies in the literature are in accordance with the guidelines, however our population showed increased recurrence rates and complications which can be also related to BB overuse. This supports the importance of RAAS inhibitors which was previously discussed in different studies. On the other hand, another systematic review showed that ACEI failed to reduce all- cause mortality and ARB may be preferred for diabetic patients with albuminuria [45]. Despite all these studies, more research is needed to evaluate the therapeutic index of RAS blockade in patients with advanced CKD [46].
4.4.2 The underuse of Aspirin: Our study included 750 patients, of which 60% were on aspirin, although all of them were high-risk patients with TOD and should be on aspirin therapy. Most of the studies performed worldwide demonstrated the importance of aspirin in high risk patients: A substudy of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) showed that patients with HTN as well as those with target organ damages have a change in their platelet physiology with higher levels of P-selectin, a protein that acts as an adhesion molecule on the surface of activated endothelial cells. The trial also showed that the use of aspirin lowered the levels of the same protein [47]. A new study by Rocca et al showed that low dose aspirin may have beneficial effects by targeting multiple pathways responsible for accelerated atherosclerosis and its thrombotic complications [48]. However, the results were not the same for low risk patients: a randomized double-blind, placebo-controlled trial done in seven countries on patients with average cardiovascular risk factors and no DM showed a low rate of events [49].
4.5 Low rates of control
4.5.1 In Hypertension: According to the recommended new office BP treatment targets, the proportions of treated uncontrolled hypertensive patients substantially increased. These findings should prompt a tighter application of therapeutic recommendations and, thus, highlight the need for improving HTN management and control strategies [36]. In our population, the BB overuse may explain the low rate of blood pressure control reaching a maximum of 60% in our studied population. To note that 7% of hypertensive patients were not treated for their HTN. BB combined with diuretics are widely used in treating HTN despite the presence of new guidelines which explains the fact that only one fourth of the patients had their blood pressure controlled [50]. This low rate of control may guide physicians to change their prescription attitudes. RAAS inhibitors are associated with the greatest control rate compared to other drugs [51]. Different studies showed low rates of blood pressure control in different populations. A proportion of 37% of the Portuguese population had their BP controlled but rate of control was decreased in patients with associated medical problems especially DM and kidney disease [52]. In our study, our patients had TOD and most of them had associated medical conditions which may explain the low control rates. Studies should be performed to specify causes of poor BP control in patients with multiple comorbidities especially in patients treated according to guidelines. Low adherence to guidelines was a major problem in different studies. More than 50% of patients received inappropriate drugs and under prescription was the major problem [53]. This was also present in Bahrain where physicians did not adhere to guidelines, particularly when treating elderly patients [54]. This also applies to our studied population where ACEI and ARB were not well prescribed.
4.5.2 In Diabetes: Concerning DM, the first line treatment for diabetic patients is BG following lifestyle modification [11]. This was respected in most of the patients. However, results showed that patients with DM were not really controlled (Table 4). This was also evident in a Lebanese university health clinic study where only 28.4% and 17.8% of patients had their HbA1c and FBS controlled, respectively [55]. A recent electronic database search showed that half of the diabetic patients have an uncontrolled blood glucose level and the major problem was the prescribers tolerating a mild hyperglycemia for a long period of time [56]. Many studies tried to establish a cause for the lack of control. Improving physicians’ knowledge concerning the guidelines [57], dietary counseling [58], and patient education [57] should be addressed to improve control. Furthermore, many patients and physicians delay the initiation and underestimate the importance of early insulin initiation due to lack of physicians’ knowledge and patient understanding [59]. This was also observed in our study where insulin was not initiated in patients with TOD and uncontrolled DM.
4.6 Strength of the Study
- Our study included 750 patients from both sexes and different age groups, chosen randomly, and treated by physicians from different specialties: cardiologists, endocrinologists, primary care physicians, geriatric physicians.
- The study was multicentric, which implies that patients were from different socio-economic backgrounds.
- All included patients were admitted patients and the medications were the ones given at discharge.
- The hospitals chosen were in Beirut and Mount Lebanon region and were all university affiliated hospitals, where interns and residents are present, and a continuous medical education program is present, conferences are held routinely, and good documentation and appropriate patient history is taken.
- Patients had comparable medical histories: they all had TOD (high risk patients), had HTN and/or DM.
- Data were collected after taking the consent from the ethical committee of the enrolled hospitals.
4.7 Weaknesses of the Study
- Our study was retrospective as we collected the data from patients’ medical charts; the timing of occurrence of complications was missing for most of the time.
- Some files had missing or incomplete data, e.g. none of the patients had his waist circumference documented in medical charts. Weight and height were also missing for some patients, or were not accurate (underestimation of weight for those on hemodialysis, overestimation for those admitted with anasarca secondary to their cardiac preexisting condition).
- We were not able to follow the level of compliance of patients to their treatment, and acknowledge the factors affecting their noncompliance if present.
- We were not able to assess the social status, the degree of education, and patients’ awareness of their condition.
- All patients were admitted, so they probably had more comorbidities, which might affect the general characteristics of the general population (age, number of comorbidities upon presentation).
- Patients were treated by physicians from different specialties, which might create a discrepancy in applying the guidelines properly (e.g. an endocrinologist’s priority might be lowering the glucose level, while the cardiologist’s main focus would be decreasing the cardiovascular risk). In addition to that, different physicians have different backgrounds: while treating according to the American guidelines, while others follow the European society of cardiology.
4.8 Study Perspectives
- We need a better system of documentation in hospitals to have a more precise concept of each patient’s background (social, medical, timeline of events occurrence...)
- We need to include clinic patients in further studies, as they represent a large proportion of cardiac patients.
- As it was obviously shown, more studies are needed to be done to assess the role of BB in treating hypertensive patients.
- More retrospective and prospective studies are needed to test whether BB are better used in the prevention or reversal of TOD.
- Moreover, the widespread use of BB may raise the following question: Why are BB that popular? Why do physicians still prescribe BB even when it is not indicated?
- More studies should be done that focuses on the causes that drive Lebanese physicians to prescribe medications. Is it their experience? Is it the drug’s price? Is it the pharmaceutical company? Is it the government or just related to the patients’ social status?
- Although continuous medical education is present in these hospitals why are physicians reluctant to adhere to guidelines? This should be addressed in further studies and multiple programs are to be done to help physicians abide by guidelines.
- Finally, our population included patients with advanced cases and multiple comorbidities. Studies are to be performed to assess the reason behind poor control in patients with multiple comorbidities and how these comorbidities affect control, and measures to be done to improve control.
5. Conclusion
This study in Lebanon indicated the absence of adherence to guidelines by the Lebanese physicians, especially in the management of hypertension where beta blockers were overused, in addition to the absence of control of diabetes and hypertension, which may be due to physicians’ non adherence to guidelines or patients’ noncompliance to medications.
Acknowledgements
We are extremely grateful for the following hospitals for allowing us to go through their patients’ medical files in order to conduct our study: the academic Beirut Governmental University Hospital, Sacré-Coeur Hospital, Geitawi Hospital, Middle East Institute of Health- Bsalim Hospital, Mount-Lebanon Hospital and Notre Dame du Liban Hospital.
References
- Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in southeast asian and African regions: need for effective strategies for prevention and control in primary care health settings. International journal of hypertension 14 (2013): 1-14.
- Farhat F, Jazra C, Ali M, et al. Profile of the care of arterial hypertension: questionnaire addressed toLebanese physicians. J Med Liban 45 (1997): 240.
- Mallat SG, Samra SA, Younes F, et al. Identifying predictors of blood pressure control in the Lebanese population-a national, multicentric survey – I-PREDICT. BMC Public Health 14 (2014): 1142.
- Azar ST, Malha LP, Zantout MS, et al. Management and control of patients with type 2 diabetes mellitus in Lebanon: results from the International Diabetes Management Practices Study (IDMPS). J Med Liban 61 (2013): 127-131.
- Moser M. Physician or Clinical Inertia: What Is It? Is It Really a Problem? And What Can Be Done About It? JCH 11 (2009): 1-4.
- Mancia G, Fagard R, Narkiewicz K, et al. Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) 31 (2013): 1281-357.
- Costanian C, Bennett K, Hwalla N, et al. Prevalence, correlates and management of type 2 diabetes mellitus in Lebanon: findings from a national population-based study. Diabetes Res Clin Pract 105 (2014): 408-415.
- Ghassibe-Sabbagh M, Deeb M, Salloum AK, et al. Multivariate epidemiologic analysis of type 2 diabetes mellitus risks in the Lebanese population. Diabetol Metab Syndr 6 (2014): 89.
- Nasreddine L, Naja FA, Sibai AM, et al. Trends in nutritional intakes and nutrition-related cardiovascular disease risk factors in Lebanon: the need for immediate action. J Med Liban 62 (2014): 83-91.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 39 (2018): 3021-3104.
- ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD The Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). European Heart Journal 34 (2013): 3035-3087.
- Tibebu A, Mengistu D, Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer Adherence 11 (2017): 323-330.
- Nascimento Cde M, Mambrini JV, de Oliveira CM, et al. Diabetes, hypertension and mobility among Brazilian older adults: findings from the Brazilian National Household Sample Survey (1998, 2003 and 2008). BMC Public Health 15 (2015): 591.
- Li M, Liu L, Song S, et al. Effect of long-term lifestyle intervention on mild cognitive impairment in hypertensive occupational population in China. Medicine (Baltimore) 97 (2018): e11975.
- Dasgupta K, Rosenberg E, Joseph L, et al. Physician step prescription and monitoring to improve ARTERial health (SMARTER): A randomized controlled trial in patients with type 2 diabetes and hypertension. Diabetes Obes Metab 19 (2017): 695-704.
- Akhuemonkhan E, Lazo M. Association between family history of diabetes and cardiovascular disease and lifestyle risk factors in the United States population: The 2009-2012 National Health and Nutrition Examination Survey. Prev Med 96 (2017): 129-134.
- Gorina M, Limonero JT, Álvarez M. Effectiveness of primary healthcare educational interventions undertaken by nurses to improve chronic disease management in patients with diabetes mellitus, hypertension and hypercholesterolemia: A systematic review. Int J Nurs Stud 86 (2018): 139-150.
- Yamamoto-Kabasawa K, Hosojima M, Yata Y, et al. Benefits of a 12-week lifestyle modification program including diet and combined aerobic and resistance exercise on albuminuria in diabetic and non-diabetic Japanese populations. Clin Exp Nephrol 19 (2015): 1079-1089.
- Brinkley TE, Anderson A, Soliman EZ, et al. Long-Term Effects of an Intensive Lifestyle Intervention on Electrocardiographic Criteria for Left Ventricular Hypertrophy: The Look AHEAD Trial. Am J Hypertens 31 (2018): 541-548.
- American Diabetes Association. Treatment of hypertension in adults with diabetes (Position Statement). Diabetes Care 25 (2002): S71-73.
- Grundy SM, Brewer HB, Jr, Cleeman JI, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 109 (2004): 433-438.
- Sowers JR. Diabetes mellitus and vascular disease. Hypertension 61 (2013): 943-947.
- de Boer IH, Kestenbaum B, Rue TC, et al. Insulin therapy, hyperglycemia, and hypertension in type 1 diabetes mellitus. Arch Intern Med 168 (2008): 1867-1873.
- Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet 380 (2012): 601-610.
- Hernandez AF, Green JB, Janmohamed S, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet 392 (2018): 1519-1529.
- Elliott WJ, Meyer PM. Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet 369 (2007): 201-207.
- Potier L, Roussel R, Velho G, et al. Lower limb events in individuals with type 2 diabetes: evidence for an increased risk associated with diuretic use. Diabetologia 62 (2019): 939-947.
- Scheen AJ. Type 2 Diabetes and Thiazide Diuretics. Curr Diab Rep 18 (2018): 6.
- Xing F, Chen J, Zhao B, et al. Real role of β-blockers in regression of left ventricular mass in hypertension patients: Bayesian network meta-analysis. Medicine (Baltimore) 96 (2017): e6290.
- Ramaswamy PK, Bhanukumar M, Hathur B, et al. Factors Contributing to Development and Reversal of LVH: A Pilot Study. J Clin Diagn Res (2016).
- Sawicki PT, Siebenhofer A. Betablocker treatment in diabetes mellitus. J Intern Med 250 (2001): 11-17.
- Ruilope LM. How to treat the diabetic hypertensive individual appropriately. J Hypertens Suppl 16 (1998): 91-93.
- Battegay E. Modern therapy of hypertension. Praxis 92 (2003): 2153-2157.
- Ellenga Mbolla BF, Ossou-Nguiet PM, Ikama SM, et al. Rates of untreated, treated, and controlled hypertension and relationships between blood pressure with other cardiovascular risk factors in Brazzaville (Republic of the Congo): May Measurement Month 2017-Sub-Saharan Africa. European Heart Journal Supplements 21 (2019): 44-46.
- Sarganas G, Neuhauser HK. Untreated, uncontrolled, and apparent resistant hypertension: results of the German Health Examination Survey 2008-2011. The Journal of Clinical Hypertension 18 (2016): 1146-1154.
- Tocci G, Presta V, Ferri C, et al. Blood Pressure Targets Achievement According to 2018 ESC/ESH Guidelines in Three European Excellence Centers for Hypertension. High Blood Press Cardiovasc Prev 27 (2020): 51-59.
- Remonti LR, Dias S, Leitão CB, et al. Classes of antihypertensive agents and mortality in hypertensive patients with type 2 diabetes-Network meta-analysis of randomized trials. J Diabetes Complications 30 (2016): 1192-1200.
- Sumida K, Molnar MZ, Potukuchi PK, et al. Changes in albuminuria and subsequent risk of incident kidney disease. Clin J Am Soc Nephrol 12 (2017): 1941-1949.
- Umanath K, Lewis JB. Update on Diabetic Nephropathy: Core Curriculum 2018. Am J Kidney Dis 71 (2018): 884-895.
- Strauss MH, Hall AS. The Divergent Cardiovascular Effects of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Type 1 Receptor Blockers in Adult Patients With Type 2 Diabetes Mellitus. Can J Diabetes 42 (2018): 124-129.
- Pai PY, Muo CH, Sung FC, et al. Angiotensin receptor blockers (ARB) outperform angiotensin-converting enzyme (ACE) inhibitors on ischemic stroke prevention in patients with hypertension and diabetes - A real-world population study in Taiwan. Int J Cardiol 215 (2016): 114-119.
- Zhang F, Liu H, Liu D, et al. Effects of RAAS Inhibitors in Patients with Kidney Disease. Curr Hypertens Rep 19 (2017): 72.
- Del Vecchio L, Teatini U, Locatelli F. Use of ACE inhibition and blood pressure management in deferring dialysis initiation. Panminerva Med 59 (2017): 166-172.
- Persson F, Lindhardt M, Rossing P, et al. Prevention of microalbuminuria using early intervention with renin-angiotensin system inhibitors in patients with type 2 diabetes: A systematic review. J Renin Angiotensin Aldosterone Syst 17 (2016): 1470320316652047.
- Wang K, Hu J, Luo T, et al. Effects of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers on All-Cause Mortality and Renal Outcomes in Patients with Diabetes and Albuminuria: a Systematic Review and Meta-Analysis. Kidney Blood Press Res 43 (2018): 768-779.
- Weir MR, Lakkis JI, Jaar B, et al. Use of Renin-Angiotensin System Blockade in Advanced CKD: An NKF-KDOQI Controversies Report. Am J Kidney Dis 72 (2018): 873-884.
- Nadar SK, Blann AD, Kamath S, et al. Platelet indexes in relation to target organ damage in high-risk hypertensive patients: a substudy of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT). J Am Coll Cardiol 44 (2004): 415-422.
- Rocca B, Patrono C. Aspirin in the primary prevention of cardiovascular disease in diabetes mellitus: A new perspective. Diabetes Research and Clinical Practice 8 (2020): 108008.
- Gaziano JM, Brotons C, Coppolecchia R, et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet 392 (2018): 1036-1046.
- Zak-Golab A, Holecki M, Smertka M, et al. Do primary care physicians follow the current recommendations for hypertensive pharmacotherapy? Pol Arch Med Wewn 123 (2013): 206-214.
- Gharaibeh KA, Turner ST, Hamadah AM, et al. Comparison of Blood Pressure Control Rates Among Recommended Drug Selection Strategies for Initial Therapy of Hypertension. Am J Hypertens 29 (2016): 1186-1194.
- Morgado MP, Rolo SA, Pereira L, et al. Blood pressure control and antihypertensive pharmacotherapy patterns in a hypertensive population of Eastern Central Region of Portugal. BMC Health Serv Res 10 (2010): 349.
- Márquez PHP, Torres OH, San-José A, et al. Potentially Inappropriate Prescription in Older Patients in Spain (PIPOPS) Investigators’ Project. Potentially Inappropriate Antihypertensive Prescriptions to Elderly Patients: Results of a Prospective, Observational Study. Drugs Aging 34 (2017): 453-466.
- Al Khaja KA, Sequeira RP, Damanhori AH. Pharmacotherapy and blood pressure control in elderly hypertensives in a primary care setting in Bahrain. Aging Clin Exp Res 16 (2004): 319-325.
- Akel M, Hamadeh G. Quality of diabetes care in a university health center in Lebanon. Int J Qual Health Care 11 (1999): 517-521.
- Blonde L, Aschner P, Bailey C, et al. Global Partnership for Effective Diabetes Management. Gaps and barriers in the control of blood glucose in people with type 2 diabetes. Diab Vasc Dis Res 14 (2017): 172-183.
- Azar ST, Malha LP, Zantout MS, et al. Management and control of patients with type 2 diabetes mellitus in Lebanon: results from the International Diabetes Management Practices Study (IDMPS). J Med Liban 61 (2013): 127-131.
- Alameddine M, Nasreddine L, Hwalla N, et al. Factors associated with consulting a dietitian for diabetes management: a cross-sectional study. BMC Health Serv Res 13 (2013): 504.
- Khunti K, Millar-Jones D. Clinical inertia to insulin initiation and intensification in the UK: A focused literature review. Prim Care Diabetes 11 (2017): 3-12.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 