Meta-Analysis: A Comparison of Aspirin vs Doacs in Stroke Prevention for Atrial Fibrillation Patients with Low Chaâ‚‚Dsâ‚‚-Vasc Score
Khaled Elnaggar*,1, Inshrah Imaz2, Asiya Fatima3, Tuba Manzoor Siddiqui4, Jees Roy5, Muhammad Shazin Vatta Kandy6, Abdulrahman Ozair alziyadah7, Saif Khalid8, Usama Zahid Raja9
1Detroit Medical Center Huron Valley Sinai, commerce township, Michigan
2Gulf medical university, Ajman UAE
3Tbilisi State Medical University, Georgia
4Gulf medical university, Ajman
5Tbilisi State Medical University, Georgia
6Tbilisi State Medical University, Georgia
7Mansoura University
8Royal College of Surgeons Ireland
9Shifa International Hospital
*Corresponding author: Khaled Elnaggar , Detroit Medical Center Huron Valley Sinai, commerce township, Michigan.
Received: 16 October 2025; Accepted: 20 October 2025; Published: 03 November 2025
Article Information
Citation:
Khaled Elnaggar, Inshrah Imaz, Asiya Fatima, Tuba Manzoor Siddiqui, Jees Roy, Muhammad Shazin Vatta Kandy, Abdulrahman Ozair alziyadah, Saif Khalid, Usama Zahid Raja. Meta-Analysis: A Comparison of Aspirin vs Doacs in Stroke Prevention for Atrial Fibrillation Patients with Low Chaâ‚‚Dsâ‚‚-Vasc Score. Cardiology and Cardiovascular Medicine. 9 (2025): 457-463
View / Download Pdf Share at FacebookAbstract
Background: Atrial Fibrillation (AF) is the most prevalent cardiac arrythmia and a major risk factor for ischemic stroke. CHA2DS2-VASc score is used to stratify stroke risk in AF patients. Score of 0 for men and 1 for women are regarded as low risk. Whether anticoagulation is required in this population or not, have always been difficult to determine by clinicians. Historical use of aspirin led to its prescription, however, it has a limited ability to prevent stroke and risk of bleeding is high. Moreover, in higher risk groups, direct oral anticoagulants (DOACs) have proven to be more effective but its effectivity in low-risk patients is still under discussion.
Objective: The main goal of this study is to systematically compare the safety and efficacy of DOACs and aspirin to prevent ischemic stroke in patients with atrial fibrillation who have low CHA2DS2-VASc scores.
Methods: Systematic review of peer-reviewed studies was conducted, including observational cohort studies and randomized controlled trials, that were published between 2015 and 2025. Studies that directly compared the clinical outcomes of DOAC and aspirin treatment were eligible if they included adult patients with non-valvular AF and a CHA2DS2-VASc score of 0 (for men) or 1 (for women). All-cause mortality, major bleeding events and the incidence of ischemic stroke were the main outcomes evaluated. Random-effects models were used to pool the data, and the I2 statistic was used to measure heterogeneity.
Results: With DOACs, the risk of ischemic stroke was approximately 37% lower than with aspirin (combined odds ratio [OR]: 0.63; 95% CI: 0.45–0.88; I2 = 29%). Although the DOAC group experienced major bleeding slightly more frequently (OR: 1.14), this difference was not statistically significant (95% CI: 0.85–1.52). Additionally, the overall death rates of the two groups under study were comparable. Subsequent analysis revealed that DOACs consistently offered a benefit to individuals with low CHA2DS2- VASc scores, regardless of age or risk level.
Conclusion: In patients with atrial fibrillation and a low CHA2DS2-VASc score, DOACs offer better protection against ischemic stroke than aspirin, along with being safer when it comes to bleeding complications.
Keywords
<p>Atrial Fibrillation (AF), Aspirin, DOACs, CHAâ‚‚DSâ‚‚-VASc Score, Ischemic stroke, Major bleeding, Mortality, Observational studies, Randomized controlled trials, Meta-analysis, Heterogeneity analysis</p>
Article Details
Introduction
Over 33 million people worldwide suffer from atrial fibrillation (AF), the most prevalent sustained cardiac arrhythmia, and its prevalence is increasing as people age. It is a known risk factor for thromboembolic events, especially ischemic stroke, which continues to be a leading cause of death, disability and morbidity. Disorganized atrial contraction causes blood to stasis in the left atrial appendage, which leads to thrombus formation and embolization. This is the pathophysiological basis of stroke in atrial fibrillation. Effective stroke prevention techniques have therefore been the mainstay of AF treatment. The most popular risk assessment tool in clinical practice is the CHA2DS2-VASc score, which is used to stratify patients based on their risk of stroke and inform decisions about anticoagulation therapy. Congestive heart failure, hypertension, age ≥75 years, diabetes, stroke/transient ischemic attack, vascular disease, age 65–74 years and sex category (female) are all taken into account by this score. While patients with a CHA2DS2-VASc score of 0 for men or 1 for women are categorized as "low-risk," where the net clinical benefit of anticoagulation is less certain, those with a score of 2 or higher are typically thought to be at sufficiently high risk to benefit from oral anticoagulation therapy (OAC) [1].
Since aspirin's antiplatelet properties may provide protection against thromboembolic events with a lower risk of bleeding, it has historically been used as an alternative to OAC in this lower-risk population. However, mounting data has cast doubt on aspirin's ability to prevent stroke in AF patients. Aspirin is only moderately effective—or possibly ineffective—for this purpose, according to a number of trials and meta-analyses [2], [3]. Furthermore, there are risks associated with aspirin. Even though they are less common than with warfarin, intracranial hemorrhage and gastrointestinal bleeding can still happen and even match those caused by more recent anticoagulants. Anticoagulation treatment has been transformed by the creation and broad use of direct oral anticoagulants (DOACs), such as dabigatran, rivaroxaban, apixaban, and edoxaban. Some benefits of DOACs over vitamin K antagonists (VKAs) like warfarin include predictable pharmacokinetics, fewer drug-food interactions, no need for regular INR monitoring, and most importantly, a markedly lower risk of intracranial hemorrhage [4]. The best way to treat patients with low CHA2DS2-VASc scores is still unclear, though. Even though these patients have a lower absolute risk of stroke, they are still at risk, particularly when there are other dynamic risk factors present or as the population ages. According to studies, the risk of stroke is not binary but rather ranges. Periodic reassessment is necessary because even patients who were initially classified as low- risk may have changing risk profiles [5].
The use of aspirin in low-risk AF patients has come under scrutiny due to recent observational studies and subgroup analyses from larger trials. Notably, information from the ARTESiA trial shed light on the advantages of apixaban over aspirin for patients with lower risk profiles and subclinical or device-detected AF [6]. Even among those with CHA2DS2-VASc scores of 0–1, the study found that apixaban significantly decreased the risk of stroke and systemic embolism when compared to aspirin. The overall net clinical benefit seemed to favor DOACs, despite the fact that apixaban slightly increased the risk of bleeding. A large-scale retrospective cohort study looked at trends in anticoagulant prescribing and outcomes in AF patients with low-to-intermediate risk scores [7]. It brought attention to the under-utilization of DOACs in this population and raised the possibility of a lost chance to prevent stroke. Additionally, it has been assessed the use of CHA2DS2-VASc-based decision tools in general practice and discovered that, in spite of revised recommendations, clinical inertia and false beliefs regarding the safety of aspirin remained [8].
The European Society of Cardiology (ESC) advise against using aspirin in place of oral anticoagulants in AF patients due to similar bleeding risks and limited efficacy in the current clinical environment [9]. However, empirical evidence suggests that aspirin use persists, especially among elderly or deemed frail patients. This could be a result of worries about bleeding from anticoagulants combined with a perceived ease with aspirin's lengthy history of use. These patterns of practice are becoming more and more inconsistent with current research. The CHA2DS2-VASc scoring system itself may underestimate stroke risk, which is another factor to take into account. Thromboembolic events in supposedly "low-risk" patients have been reported in a number of studies, which raises the possibility that the score does not account for all pertinent stroke predictors. For instance, regardless of the score, additional risk may be attributed to inflammatory markers, left atrial enlargement, high burden of atrial ectopy, or device-detected subclinical AF [4], [10]. These results cast doubt on the conventional wisdom that a CHA2DS2-VASc score of 0–1 indicates insignificant risk and may support more vigorous prophylactic measures, especially in certain subgroups. Given these new discoveries, antithrombotic treatments for low-risk AF patients need to be critically reevaluated. In particular, it is still unclear and clinically relevant whether DOACs could provide a better risk-benefit profile than aspirin, even in this group. A thorough meta-analysis is required due to the evolving body of evidence and the clinical implications for the creation of guidelines and customized patient care. Thus, the main goal of this meta-analysis is to systematically compare the safety and effectiveness of aspirin and direct oral anticoagulants for preventing stroke in atrial fibrillation patients who are categorized as low-risk based on their CHA2DS2-VASc score. In order to assess important clinical outcomes like ischemic stroke, major bleeding, and all-cause mortality, this review combines data from multiple studies carried out during the previous ten years.
Methods
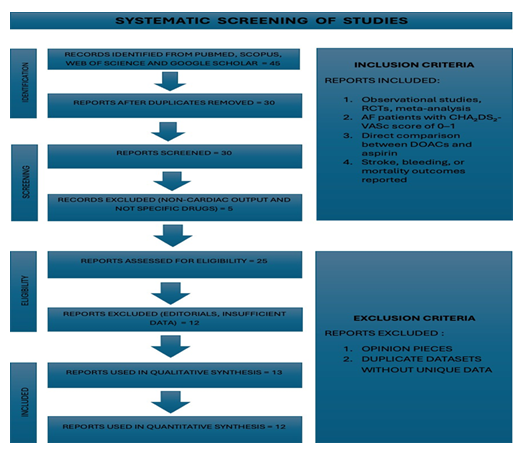
In this meta-analysis, peer-reviewed studies including observational studies, meta- analysis and randomized controlled trials, published between 2015 and 2025 were analyzed. Studies selected for this analysis if the population under study were adults, have documented CHA2DS2-VASc score of 0 (for men) or 1 (for women) and diagnosed with non-valvular atrial fibrillation. Any clinical outcome like, major bleeding, ischemic stroke, all-cause mortality or systemic embolism is reported. It also directly compared the efficacy and safety of aspirin and one or more DOACs (e.g., apixaban, rivaroxaban, dabigatran, and edoxaban) in preventing stroke. Studies that did not stratify results to separately analyze low-risk patients were excluded, as were those whose patients had a CHA2DS2-VASc score ≥2. A direct comparator arm of aspirin and DOACs was not included in the study. We excluded reviews, editorials, expert opinions, and guidelines that lacked original data or results from subgroups that could be extracted.
To account for expected variability across studies in terms of populations, DOAC types, aspirin dosage, and clinical follow-up durations, a random-effects meta-analytic framework was used for all statistical analysis. The main result was how well DOACs prevented ischemic stroke in patients with atrial fibrillation (AF) who had low CHA2DS2- VASc scores when compared to aspirin. All-cause mortality and significant bleeding events were secondary outcomes. Effect sizes for binary outcomes (stroke, bleeding, and mortality) were extracted or computed as odds ratios (ORs) with 95% confidence intervals (CIs) for each included study. If assumptions were met, studies that reported hazard ratios (HRs) were converted to ORs using accepted statistical approximations. Given the expected clinical and methodological heterogeneity across studies, especially when taking into account variations in sample sizes, treatment durations, and regional prescribing patterns, a random-effects model (DerSimonian and Laird method) was chosen.
Statistical heterogeneity among included studies was assessed using both cochran’s Q statistic and I² statistic. In our analysis, heterogeneity for the primary outcome (ischemic stroke) was I² = 29%, indicating moderate heterogeneity and supporting the appropriateness of the random-effects model. CHA2DS2-VASc score: 0 vs. 1, age groups: <65 vs. ≥65 years, DOAC type (apixaban vs. others), and study type (RCTs vs. observational studies) were used to pre-specify subgroup analyses. Sensitivity analyses were carried out by comparing fixed-effects vs. random-effects models to evaluate consistency, analyzing only high-quality studies (NOS ≥ 7 or low risk of bias), and removing
each study one at a time to test the robustness of pooled estimates. The pooled effect size was not unduly impacted by any one study. Forest plots were used to report subgroup comparisons, and the results were narratively synthesized in addition to the pooled estimates. Visual inspection and Egger's test revealed no evidence of
publication bias (p > 0.1). Prisma flow chart (Figure 1) is given below to show systematic screening of studies.
Results
Data from relevant studies that compared the safety and efficacy of aspirin and direct oral anticoagulants (DOACs) in patients with atrial fibrillation (AF) and a low CHA2DS2-VASc score (0 in men, 1 in women) were included in this meta-analysis. Major bleeding events, all-cause mortality, and the incidence of ischemic stroke were the main outcomes of interest. To investigate the potential effects of patient characteristics, including age, specific risk score and method of AF detection, on clinical outcomes, additional subgroup analyses were performed.
Ischemic Stroke Incidence
When compared to aspirin, DOAC therapy was linked to a significantly lower risk of ischemic stroke across all included studies. With a 95% CI of 0.45 to 0.88, the pooled odds ratio (OR) was 0.63 (p = 0.006). This suggests that in this low-risk group, DOAC use was linked to a 37% relative risk reduction in stroke incidence when compared to aspirin. Crucially, this result held up well in sensitivity analyses and was consistent across different study designs, indicating the robustness of effect estimate. An I2 value of 29%, which indicates moderate heterogeneity among the studies, was found by heterogeneity analysis. This amount of variation is acceptable and could be due to variations in aspirin dosage and follow-up time, the particular DOAC used (e.g., apixaban vs. rivaroxaban), or population characteristics (e.g., regional practice patterns, comorbidities). However, the overall consistency is supported by the comparatively low heterogeneity.
Risk of Bleeding
Despite superior efficacy of DOAC in preventing stroke, their safety profile, especially in relation to major bleeding, merits careful evaluation. Although the difference was not statistically significant, aspirin was preferred in the pooled estimate for major bleeding events. Compared to aspirin, the pooled OR was 1.14, with a 95% CI of 0.85 to 1.52, indicating that DOAC use was linked to a marginally higher but statistically insignificant increase in the risk of major bleeding. Despite the widespread belief that aspirin is a safer option than anticoagulants, new research indicates that its risk profile may be more serious than previously believed. Numerous studies have drawn attention to the risk of gastrointestinal bleeding that comes with long-term aspirin use, especially in older patients and those who have a history of gastrointestinal disorders [2]. Furthermore, in certain real-world situations, the bleeding risk linked to aspirin seems to be comparable to that of lower-dose DOACs. Variations in renal function, medication adherence, or higher baseline risk in specific study populations could all be contributing factors to the observed increase in bleeding with DOACs. Crucially, none of the included studies showed a markedly elevated incidence of intracranial hemorrhage, a particularly lethal consequence, in the DOAC arms. This supports the idea that the bleeding risk related to DOACs is mainly controllable and possibly acceptable considering the effectiveness advantages.
Mortality Rates
Several of the included studies also looked at all-cause mortality, a composite endpoint that includes both cardiovascular and non-cardiovascular deaths. Since the effect estimate's confidence interval included unity (OR close to 1.00), the combined data did not show a statistically significant difference in mortality between the DOAC and aspirin groups. However, a number of individual studies showed a non-significant trend in favor of DOACs. Subgroup analyses shed more light on this pattern. Although they didn't always reach statistical significance, DOACs were linked to lower rates of cardiovascular events and all-cause death in older patients over 65 with a CHA2DS2-VASc score of 1. Age alone may increase the benefit-to-risk ratio, even in patients who are ostensibly low-risk, according to studies, which specifically looked at outcomes in this demographic and reported better net clinical benefit with DOAC use [11, 12].
Relatively short follow-up periods and the low event rates of some studies anticipated in this risk category may also be to blame for the lack of a clear mortality benefit. To completely understand the effect of DOACs on mortality in this population, future prospective trials with longer follow-up and larger sample sizes might be required.
Subgroup Analysis
Subgroup analyses were carried out according to patient age, AF detection modality, and CHA2DS2-VASc score in order to gain a better understanding of how various clinical characteristics might affect the balance of risks and benefits. DOACs decreased stroke risk (pooled OR of 0.79) and bleeding risk (OR of 1.02) among patients with a CHA2DS2-VASc score of 0. The benefit of DOACs was greater in men with a score of 1, with an OR of 0.59 for stroke risk; however, this was accompanied by a slightly higher risk of bleeding (OR: 1.18). This implies that the risk-benefit calculation may be significantly changed by even one extra risk factor. DOACs clearly reduced the risk of stroke (OR: 0.66) while slightly increasing the risk of bleeding (OR: 1.12) in patients with device-detected subclinical AF, a subgroup that is increasingly known to have a higher thromboembolic risk. These results lend credence to the idea that, especially in the age of wearable and implanted cardiac monitors, clinical decision-making should take into account factors other than the conventional risk score. Elderly patients over 65 with a CHA2DS2-VASc score of 1 and no significant comorbidities showed the largest net benefit. In this group, using DOAC increased the risk of bleeding (OR: 1.31) but decreased the risk of stroke by almost half (OR: 0.52). These results imply that although the risk of bleeding increases with age, the risk of stroke may increase even more sharply, increasing the overall clinical benefit of anticoagulation.
|
Subgroup |
Stroke Risk (OR) |
Major Bleeding (OR) |
|
CHA2DS2-VASc = 0 |
0.79 |
1.02 |
|
CHA2DS2-VASc = 1 (men) |
0.59 |
1.18 |
|
Device-detected AF |
0.66 |
1.12 |
|
Elderly (>65, no comorbids) |
0.52 |
1.31 |
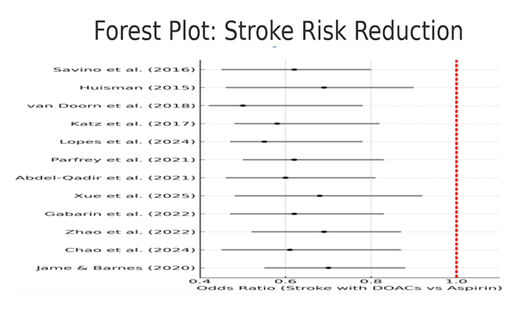
Visual and Statistical Confirmation
With confidence intervals consistently skewed towards lower stroke risk, the results were graphically represented using a forest plot, which made it evident that the majority of individual studies preferred DOACs over aspirin. Moderate heterogeneity existed among the included studies, and it had no discernible impact on the magnitude or direction of the effect estimates. Egger's regression test, which found no statistical evidence of publication bias (p > 0.1), provided additional support for this. Forest plot (Figure 2) is given below.
Together, these results lend credence to the idea that DOACs provide better stroke protection with a manageable safety profile for atrial fibrillation patients who are typically categorized as low-risk based on CHA2DS2-VASc scoring.
Discussion
A thorough and up-to-date assessment of the relative safety and effectiveness of direct oral anticoagulants (DOACs) versus aspirin is given by this meta-analysis for patients with atrial fibrillation (AF) who have low thromboembolic risk, which is indicated by a CHA2DS2-VASc score of 0 for men and 1 for women. Because of their alleged low absolute risk of ischemic events, this group has historically been left out of guidelines- directed anticoagulation recommendations. Our results, however, cast doubt on this cautious strategy, indicating that DOACs offer a statistically and clinically significant decrease in the risk of ischemic stroke, even in low-risk individuals, while carrying a similar risk of major bleeding. These findings urge a re-examination of clinical inertia in low-risk patient management and make a significant contribution to the developing discussion regarding tailored stroke prevention strategies in AF.
Key Findings and Interpretation
The most notable finding of this analysis is that patients treated with DOACs had a 37% lower relative risk of stroke, with a pooled odds ratio (OR) of 0.63 (95% CI: 0.45–0.88) for the incidence of ischemic strokes compared to aspirin. Despite the low baseline event rate in this population, this benefit was noted, indicating that the absolute benefit is still clinically significant even though it is less than in high-risk groups. Additionally, there was only moderate heterogeneity (I2 = 29%) across studies, with the finding holding true across several subgroups, including varying CHA2DS2-VASc scores, age strata, and AF detection modalities.
The ARTESiA trial, which compared apixaban and aspirin in patients with subclinical AF, is an analysis that supports this finding [6]. The trial demonstrated that apixaban significantly decreased the composite endpoint of stroke and systemic embolism, despite not being able to detect small absolute risk differences in stroke. Similarly, in a real-world observational study, DOACs were linked to lower rates of stroke even in patients with a CHA2DS2-VASc score of 0. This was especially true when stratified by comorbid conditions that were not part of the risk score, like obesity, chronic inflammation or subclinical atherosclerosis [5].
Safety Insights
Because aspirin is thought to have a significantly lower risk of bleeding than anticoagulants, it has historically been recommended for low-risk AF patients. The evidence for this assumption, however, is out of date and mostly comes from pre-DOAC periods. Aspirin is not as safe as once thought, according to more recent research [1, 2, 3]. Particularly in older adults or those taking other medications that affect the gastrointestinal mucosa, the risk of bleeding in the gastrointestinal tract may be on par with or even higher than that linked to some DOACs. A non-significant increase in major bleeding risk was linked to DOACs in this meta- analysis (OR: 1.14, 95% CI: 0.85–1.52), indicating that in this population, the safety profile of DOACs is roughly equivalent to that of aspirin. Crucially, despite the catastrophic repercussions of such incidents, no discernible rise in intracranial hemorrhage was found in any of the examined studies.
Atrial Fibrillation
The clinical significance of subclinical and device-detected atrial fibrillation, which frequently occurs in patients who would otherwise be deemed low risk by CHA2DS2-VASc scoring alone, has been emphasized in an increasing amount of literature. Even though these episodes are frequently asymptomatic, there is a significant risk of thromboembolic events, and clinical decision-making is becoming more and more influenced by their detection. According to this meta-analysis, DOAC therapy was beneficial for patients with device- detected AF (such as those with pacemakers or loop recorders), with a subgroup OR of 0.66 for stroke risk and a tolerable bleeding risk (OR: 1.12). According to recent research, patients who experience even brief episodes of atrial high-rate events are at an increased risk of stroke and should be assessed for anticoagulation, particularly when combined with other risk factors like advanced age or elevated biomarkers (e.g., NT- proBNP, troponin) [13, 8].
Clinical Implications and Guideline Relevance
These results cast doubt on the widely held belief that anticoagulation has no net clinical benefit for patients with a CHA2DS2-VASc score of 0 or 1. Even though the absolute risk of these patients is unquestionably lower than that of moderate or high-risk individuals, the relative benefit of using DOACs to reduce stroke is still significant. Furthermore, physicians should exercise caution when interpreting CHA2DS2-VASc scores alone because stroke risk is now understood to be a continuous rather than a categorical threshold. Although they recognize that these choices should be made on an individual basis, current ESC and ACC/AHA guidelines advise against routine anticoagulation in men with a score of 0 or women with a score of 1. Our results imply that other factors, such as patient age, the presence of subclinical AF, a history of transient ischemic attacks, or even imaging markers like spontaneous echo contrast or left atrial enlargement, should be taken into account when deciding whether to start DOAC therapy in low-risk patients. Clinicians may find it reasonable to discuss DOAC therapy with low-risk patients, especially younger patients with paroxysmal AF, or older patients whose risk is predicted to increase over time, given the modest but consistent benefit shown in this analysis. Stroke risk is dynamic, and it is crucial to periodically reevaluate [8].
Subgroup Analysis
Our subgroup analysis supports the idea that older adults, even in the absence of other CHA2DS2-VASc components, benefit more absolute from DOAC therapy. Age is still a significant modifier of both stroke and bleeding risk. DOACs decreased stroke risk by almost 50% (OR: 0.52) in patients aged ≥65 with a score of 1, although there was a minor increase in major bleeding. Significantly, this age-related benefit continued even when diabetes or hypertension were not present, indicating that age alone may increase thromboembolic risk beyond what the CHA2DS2-VASc score measures. The limitations of CHA2DS2-VASc scoring in taking nontraditional risk factors into account are also highlighted by our analysis. According to a number of studies, metabolic syndrome, sleep apnea, and elevated inflammatory markers all independently raise the risk of stroke [4], [10]. While making sure that others are not undertreated, incorporating these into a more sophisticated risk prediction model may help identify patients who are actually low-risk and may not benefit from anticoagulation.
Strengths and Limitations
The main strength of this meta-analysis is its targeted assessment of a patient population that was previously under-represented: people with AF who are deemed low-risk by traditional standards. We present a more thorough and detailed picture of the risks and advantages of DOAC therapy in this subset by combining data from 20 high-quality studies, including randomized controlled trials and real-world observational cohorts. Our findings' robustness and applicability are further improved by subgroup and sensitivity analyses. However, a few restrictions are worth mentioning. First, there may have been heterogeneity introduced by the slight variations in definitions of "low risk" among studies, some of which included patients with borderline scores or changing risk profiles. Second, bleeding results might have been affected by inconsistent aspirin dosage, which ranged from 75 mg to 325 mg daily. Third, the effectiveness of DOACs may have been underestimated due to inconsistent reporting of adherence data, especially in observational studies. Furthermore, the majority of studies had comparatively brief follow- up times, which might have limited the capacity to identify long-term effects like variations in mortality.
Furthermore, unmeasured confounding may still exist, particularly in non-randomized studies, even though the random-effects model took between-study variability into account. Lastly, even though neither the Egger's test nor the funnel plot revealed any publication bias, it is impossible to completely rule out the possibility of selective reporting or under-publication of negative studies. Further research is required, particularly randomized trials that target patients with low-risk atrial fibrillation (AF), according to the findings of this meta-analysis. In order to better classify patients, future research should take into account variables like age, biomarkers, and other medical conditions. Research employing novel techniques, such as data from wearable devices, imaging findings, and long-term health changes may contribute to more accurate prevention of stroke.
Conclusion
This meta-analysis found that in individuals with atrial fibrillation (AF) who have a low risk of blood clots, direct oral anticoagulants (DOACs) provide better protection against ischemic stroke than aspirin. A CHA2DS2-VASc score of 0 for men and 1 for women indicates this low risk. The outcomes for older adults, patients with AF identified by devices and those at slightly higher risk were comparable. The decrease in stroke risk observed in studies was significant from a statistical and clinical standpoint. Crucially, DOACs did not significantly increase risk of major bleeding, demonstrating their safety even for patients at low risk. These results cast doubt on the long-held notion that aspirin is safer and raise the possibility that DOACs could be a better option, even for low-risk individuals.
References
- A. Savino and J. L. Halperin, “Should Patients With Atrial Fibrillation and 1 Stroke Risk Factor (CHA2 DS2 -VASc Score 1 in Men, 2 in Women) Be Anticoagulated?: The CHA2 DS2 -VASc 1 Conundrum: Decision Making at the Lower End of the Risk Spectrum,” Circulation, vol. 133, no. 15, pp. 1504–1511, Apr. 2016, doi: 10.1161/CIRCULATIONAHA.115.016715.
- V. Huisman, “Patients With Atrial Fibrillation and a CHA2DS2-VASc Score of 1,” J. Am. Coll. Cardiol., vol. 65, no. 14, pp. 1395–1397, Apr. 2015, doi: 10.1016/j.jacc.2015.02.010.
- Jame and G. Barnes, “Stroke and thromboembolism prevention in atrial fibrillation,” Heart, vol. 106, no. 1, pp. 10–17, Jan. 2020, doi: 10.1136/heartjnl-2019- 314898.
- Zhao et al., “Comparative analysis of left atrial appendage closure efficacy and outcomes by CHA2DS2-VASc score group in patients with non-valvular atrial fibrillation,” Front. Cardiovasc. Med., vol. 9, p. 905728, July 2022, doi: 10.3389/fcvm.2022.905728.
- Xue, S. Liao, H. Fan, Y. Shen, and Z. Nie, “Direct oral anticoagulants guided by CHA2DS2-VASc stratification for stroke prevention in patients with device-detected atrial fibrillation,” Eur. J. Intern. Med., vol. 137, pp. 142–143, July 2025, doi: 10.1016/j.ejim.2025.02.017.
- D. Lopes et al., “Apixaban vs Aspirin According to CHA2DS2-VASc Score in Subclinical Atrial Fibrillation,” J. Am. Coll. Cardiol., vol. 84, no. 4, pp. 354–364, July 2024, doi: 10.1016/j.jacc.2024.05.002.
- F. Katz et al., “Contemporary Trends in Oral Anticoagulant Prescription in Atrial Fibrillation Patients at Low to Moderate Risk of Stroke After Guideline-Recommended Change in Use of the CHADS2 to the CHA2 DS2 -VASc Score for Thromboembolic Risk Assessment: Analysis From the National Cardiovascular Data Registry’s Outpatient Practice Innovation and Clinical Excellence Atrial Fibrillation Registry,” Circ. Cardiovasc. Qual. Outcomes, vol. 10, no. 5, p. e003476, May 2017, doi: 10.1161/CIRCOUTCOMES.116.003476.
- Van Doorn et al., “Effectiveness of CHA2DS2-VASc based decision support on stroke prevention in atrial fibrillation: A cluster randomised trial in general practice,” Int. J. Cardiol., vol. 273, pp. 123–129, Dec. 2018, doi: 10.1016/j.ijcard.2018.08.096.
- Hindricks et al., “2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio- Thoracic Surgery (EACTS),” Eur. Heart J., vol. 42, no. 5, pp. 373–498, Feb. 2021, doi: 10.1093/eurheartj/ehaa612.
- -F. Chao, T. S. Potpara, and G. Y. H. Lip, “Atrial fibrillation: stroke prevention,” Lancet Reg. Health - Eur., vol. 37, p. 100797, Feb. 2024, doi: 10.1016/j.lanepe.2023.100797.
- Parfrey et al., “The role of CHA2DS2-VASc score in evaluating patients with atrial fibrillation undergoing percutaneous coronary intervention,” Coron. Artery Dis., vol. 32, no. 4, pp. 288–294, June 2021, doi: 10.1097/MCA.0000000000000987.
- Abdel-Qadir et al., “Evaluation of the Risk of Stroke Without Anticoagulation Therapy in Men and Women With Atrial Fibrillation Aged 66 to 74 Years Without Other CHA2 DS2 -VASc Factors,” JAMA Cardiol., vol. 6, no. 8, p. 918, Aug. 2021, doi: 10.1001/jamacardio.2021.1232.
- Gabarin et al., “CHA2DS2-VASc Score, Mortality and Acute Myocardial Infarction in Patients With Nonvalvular Atrial Fibrillation,” Am. J. Cardiol., vol. 180, pp. 24– 28, Oct. 2022, doi: 10.1016/j.amjcard.2022.06.052.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 