No Stents, No Bypass Surgery: A Cultural Shift Toward Drug-Coated Balloons in Indonesia
Prof. Dasaad Mulijono1,2,3
1Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia
2Indonesian College of Lifestyle Medicine, Indonesia
3Department of Cardiology, Faculty of Medicine, Prima University, Medan, Indonesia
*Corresponding author:Prof. Dasaad Mulijono, Department of Cardiology, Bethsaida Hospital
Received: 24 June 2025; Accepted: 02 July 2025; Published: 04 July 2025
Article Information
Citation: Dasaad Mulijono. No Stents, No Bypass Surgery: A Cultural Shift Toward Drug- Coated Balloons in Indonesia. Cardiology and Cardiovascular Medicine 9 (2025): 227-233.
View / Download Pdf Share at FacebookAbstract
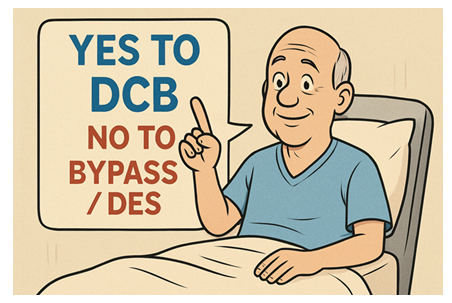
In many Southeast Asian countries, including Indonesia, there is a notable cultural reluctance toward invasive cardiovascular procedures such as coronary artery bypass grafting (CABG) and the implantation of permanent foreign bodies like coronary stents. Beyond this cultural aversion, drugcoated balloon (DCB) technology offers distinct clinical advantages over drug-eluting stents (DES), including eliminating permanent implants, preserving vascular integrity, and reducing the need for prolonged dual antiplatelet therapy.
In recent years, the clinical indications for DCB use have expanded significantly now encompassing not only in-stent restenosis (ISR) and small vessel disease but also de novo lesions of all sizes, acute myocardial infarction, left main and ostial lesions, bifurcation lesions, chronic total occlusions, long and diffuse disease, heavily calcified lesions, vulnerable plaques, and patients at high bleeding risk or with anticipated noncompliance.
This article examines the sociocultural and clinical factors driving the adoption of DCB technology. It highlights our experience at the Cardiac Centre of Bethsaida Hospital, pioneered by Prof. Dasaad Mulijono, where the integration of DCB interventions with a plant-based diet (PBD) program has resulted in restenosis rates as low as 2%—a stark contrast to the 10–20% commonly reported at other centres. We also present evidence from computed tomography coronary angiography (CTCA) and coronary angiography demonstrating atherosclerosis regression in patients adhering to the PBD approach.
Given the proliferation of unproven and potentially harmful therapies, such as chelation therapy, enhanced external counterpulsation (EECP), and unvalidated thrombectomy techniques, knowledgeable and dedicated physicians must proactively educate patients about evidence-based treatment options. Furthermore, integrating artificial intelligence (AI) presents a transformative opportunity to personalize patient education, enhance clinical decision-making, and guard against misinformation and medical fraud.
As the landscape of coronary artery disease (CAD) management continues to evolve, the appropriate utilization of DCB technology, combined with patient-centred education and holistic care models, represents a critical step forward in improving cardiovascular outcomes across diverse populations.
Keywords
<p>Drug-coated balloon; Coronary artery disease; Restenosis; Plant-based diet, Bethsaida hospital; Prof. Dasaad Mulijono; Artificial intelligence in healthcare; Cultural perceptions in medicine; Atherosclerosis reversal; Chelation therapy; Enhanced external counterpulsation; Thrombectomy device; Medical fraud prevention</p>
Article Details
1. Introduction
Invasive cardiovascular procedures, including CABG and percutaneous coronary interventions (PCIs) involving stent placement, have become the mainstay of treatments in Western cardiology practice. However, in Indonesia and among broader Asian populations, cultural and perceptual hesitation exists regarding these interventions. Traditional health beliefs, fear of foreign materials within the body, and historical scepticism regarding invasive procedures have driven the preference for less invasive alternatives [1-3]. DCB technology has emerged as a promising option, offering a non-stent-based approach that aligns more closely with patient preferences while maintaining clinical efficacy.
2. Cultural and Sociological Perspectives: Reluctance Toward Invasive Procedures
The hesitance toward invasive cardiac procedures in Indonesian and other Asian communities is multifactorial. Deeply ingrained cultural beliefs often emphasise natural healing and minimal interference with the body’s inherent balance [4-6]. The concept of implanting a foreign body whether it be a coronary stent or prosthetic material can evoke concerns regarding long-term compatibility, the potential for complications, and even ethical or spiritual dissonance. This cultural mindset is compounded by anecdotal experiences and historical mistrust in specific healthcare interventions, contributing to a pervasive preference for non-invasive or minimally invasive therapeutic strategies.
3. Impact on Treatment Decisions
Patients’ reluctance to undergo procedures perceived as invasive has influenced the clinical landscape, prompting cardiologists and interventionalists to consider alternative approaches. The adoption of DCB technology has been particularly noteworthy, as it aligns with patient values while offering comparable outcomes in treating various coronary pathologies. The patient-centric approach in regions such as Indonesia emphasises informed decision-making, wherein the risks of traditional stenting and bypass surgery are weighed against innovative, less invasive alternatives.
4. Comparative Advantages of DCBs Over DES
DES has long represented the standard of care in the percutaneous management of CAD. While DES technology has significantly improved clinical outcomes compared to bare-metal stents, it has limitations. The deployment of a permanent metallic scaffold can introduce a range of complications, particularly in patients with heightened inflammatory responses or cultural aversions to foreign body implantation.
5. Limitations and Complications Associated with DESs
A substantial body of literature has emerged over the past decade, comparing DESs and DCBs to evaluate their advantages and limitations across various clinical settings. These comparative studies, encompassing randomized controlled trials, meta-analyses, and large-scale registries, have provided critical insights into each modality's efficacy, safety profiles, and long-term outcomes. While DES has traditionally been the standard of care for a wide range of coronary artery lesions, increasing evidence supports the non-inferiority—and in select scenarios, the superiority—of DCB [7-20].
The challenges associated with DES include:
- Delayed endothelialization increases the risk of late stent thrombosis.
- Alteration of vessel geometry and biomechanics, which may compromise physiological vascular function.
- Chronic inflammation and irritation, including possible allergic reactions to the polymer or metal alloy.
- Development of neoatherosclerosis, a progressive form of vascular remodelling within the stent.
- Mechanical issues such as stent fracture, leading to target lesion failure.
- ISR, which may be caused by local hypersensitivity or mechanical underexpansion.
- The necessity for prolonged dual antiplatelet therapy (DAPT), increasing the risk of bleeding, particularly in elderly or high-risk patients.
6. Advantages of the "Leave Nothing Behind" Strategy with DCBs
DCBs offer a fundamentally different therapeutic approach by delivering antiproliferative agents directly to the vessel wall, eliminating the need to implant a permanent device. This “leave nothing behind” strategy yields several key clinical and procedural advantages [7-17]:
- Preservation of native vessel architecture and vasomotor function, supporting long-term physiological remodelling.
- Late lumen enlargement and positive vessel remodelling, potentially contributing to plaque regression and favourable hemodynamic adaptation.
- Reduction in procedural complexity, with shorter fluoroscopy time and lower radiation exposure.
- Facilitation of future surgical options, such as coronary artery bypass grafting, due to the absence of metallic implants.
- DCBs reduce the need for prolonged DAPT, making them suitable for patients with active bleeding, high bleeding risk, or upcoming surgical interventions.
- Cultural compatibility, particularly in Asian populations, including Indonesians, who frequently express reluctance toward permanent foreign body implantation.
- Suitability in patients with suboptimal medication adherence is critical in settings where non-compliance may reach up to 50%.
- Viability in populations with high inflammation burdens, where adherence to lifestyle modifications is limited and stent-related inflammation poses an additional risk.
- DCB's ability to preserve native vasculature makes it ideal for younger patients, where long-term outcomes and technological adaptability are paramount.
- Avoid complications associated with stent failure, particularly in ISR cases linked to hypersensitivity or suboptimal initial implantation.
1. Broadened Clinical Utility of DCBs in Complex Coronary Lesions
Recent advancements have significantly broadened the indications for DCB therapy. Initially applied to manage ISR and small vessel disease, the utility of DCBs now extends to a variety of complex coronary lesions, including:
- • De Novo Lesions: Applicable in vessels of all sizes [21-30].
- • Acute Myocardial Infarction: Offering a potential alternative in the acute setting [31-35].
- • Left Main and Ostial Lesions: Addressing high-risk anatomical locations [9, 36,37].
- • Chronic Total Occlusions: Providing a therapeutic option where traditional interventions may be limited [38-40].
- • Bifurcations: Enhancing Treatment Options in Challenging Anatomical Contexts [41-44].
- • Severely Calcified Lesions, Long, Diffuse Lesions: Addressing the Spectrum of Coronary Artery Disease with Tailored Pharmacotherapy [45-51].
- • High Bleeding Risk Patients: Offering a safer profile by potentially reducing the need for prolonged dual antiplatelet therapy [52-54]
- • Vulnerable plaques: refer to lesions with intermediate degrees of stenosis that may not appear hemodynamically significant but possess high-risk morphological features, rendering them prone to rupture and capable of precipitating acute coronary events [55-57].
2. Clinical Experience at Cardiac Centre, Bethsaida Hospital
At Cardiac Centre, Bethsaida Hospital, a novel integrative approach has been adopted that combines DCB technology with a PBD program. This multidisciplinary strategy aims not only to treat CAD but also to address its underlying atherosclerotic pathology. Clinical outcomes have been impressive, with a reported restenosis rate of 2%, a significant improvement over the approximately 10-20% rate observed in other centres. Additionally, serial CTCA combined with coronary angiography studies have demonstrated reversal of atherosclerotic changes, underscoring the potential of dietary intervention in cardiovascular disease management [58-61].
3. Challenges with Unproven Therapies and the Role of AI
9.1 Unproven Interventions in Cardiovascular Care
The fear and avoidance of invasive cardiovascular procedures are frequently compounded by the widespread promotion of unproven and scientifically unsubstantiated therapies, which often target vulnerable patient populations. Interventions such as chelation infusion, EECP, and specific thrombectomy-based techniques—particularly those marketed in neighbouring regions, including parts of Malaysia—have not consistently demonstrated reliable clinical efficacy in controlled studies. A recurring concern is the inappropriate expansion of indications beyond what is supported by evidence-based guidelines. For instance, EECP is specifically indicated for patients with refractory angina who are not suitable candidates for revascularization via PCI or CABG [62,63]. Yet, it is often promoted indiscriminately for all forms of CAD [64,65]. Similarly, chelation therapy, which lacks robust clinical validation for coronary atherosclerosis, is frequently advertised as a universal treatment for coronary obstruction.
The propagation of such interventions—often described within the medical community as pseudoscientific or even "quackery"—poses a significant threat to patient safety, undermines trust in the healthcare system, and may result in delayed or inappropriate care by diverting patients away from proven, evidence-based therapies. However, the arrival of DCB therapy into the Indonesian interventional cardiology market has significantly shifted this landscape. The availability of DCB—an evidence-based, minimally invasive, and effective modality for select cases of CAD— has altered patient preferences. The desire to fall into the trap of unproven treatments such as chelation, EECP, and thrombectomy has notably decreased. Instead, there is now a growing wave of acceptance, as many patients who previously relied on unvalidated therapies are actively seeking DCB as a safer and more scientifically grounded alternative.
9.2 Integrating AI for Patient Education
AI is valuable for enhancing patient education and clinical decision-making in this complex therapeutic landscape. AI algorithms can assimilate vast amounts of clinical data and literature to provide personalised treatment recommendations grounded in evidence-based medicine. By integrating AI into patient education platforms, healthcare providers can provide clear and accurate information about the risks and benefits of various coronary interventions. This technology also holds promise in identifying and flagging unproven or potentially fraudulent therapies, thereby protecting patients from exploitation and ensuring adherence to high standards of clinical care [66-68].
At Bethsaida, we actively educate our patients to differentiate between unproven and scientifically validated therapies. Recognising the power of digital tools, we also coach our patients to utilize AI platforms, such as ChatGPT, to evaluate and cross-check medical information critically. The results have been outstanding. Not only have patients become more confident in making informed decisions, but many have also emerged as ambassadors in their communities, helping to spread accurate, up-to-date knowledge about the latest advances in CAD management. This grassroots movement has proven invaluable in countering misinformation and fostering a more informed, health-literate society.
4. Conclusion
The cultural predisposition among Indonesian and broader Asian populations to avoid invasive cardiac procedures has catalysed a shift towards less invasive modalities, notably DCB technology. The expanded clinical indications for DCB and its favourable profile compared to DESs make it a desirable option in regions where traditional interventional methods are met with scepticism. Furthermore, innovative approaches, such as integrating a PBD at Cardiac Centre Bethsaida Hospital, demonstrate the potential for synergistic strategies that not only treat but may also reverse CAD. As the field of interventional cardiology continues to evolve, the incorporation of AI promises to enhance patient education further and safeguard against the encroachment of unproven therapies, ensuring that clinical decisions remain both culturally sensitive and scientifically robust.
Conflict of Interest: The authors declare no conflict of interest.
5. References
- Qanitha A, Qalby N, Amir M, Uiterwaal CSPM, Henriques JPS, et al. Clinical Cardiology in South East Asia: Indonesian Lessons from the Present towards Improvement. Glob Heart 17 (2022): 66.
- Asa GA, Fauk NK, McLean C, Ward PR. Medical tourism among Indonesians: a scoping review. BMC Health Serv Res 24 (2024): 49.
- Iryanidar I, Irwan AM. Stress and coping mechanisms in patients undergoing CABG: An integrative review, Clinical Epidemiology and Global Health 23 (2023): 101388.
- Febriyanti RM, Saefullah K, Susanti RD, Lestari K. Knowledge, attitude, and utilization of traditional medicine within the plural medical system in West Java, Indonesia. BMC Complement Med Ther 24 (2024): 64.
- Widayanti AW, Green JA, Heydon S, Norris P. Health-Seeking Behavior of People in Indonesia: A Narrative Review. J Epidemiol Glob Health 10 (2020): 6-15.
- Peltzer K, Pengpid S. Traditional Health Practitioners in Indonesia: Their Profile, Practice and Treatment Characteristics. Complement Med Res 26 (2019): 93-100.
- Niu J, Wang K, Wang W, Liu Y, Yang J, et al. Drug-Coated Balloons versus Drug-Eluting Stents for the Treatment of De Novo Coronary Artery Disease: A Meta-Analysis of Randomized Controlled Trials. Rev Cardiovasc Med 25 (2024): 446.
- Keefe N, Shull T, Botea L, McGinigle K. Drug-Coated Balloon versus Drug-Eluting Stent: The Debate of Leave Nothing Behind. Semin Intervent Radiol 40 (2023): 161-166.
- Gunawardena TD, Corballis N, Merinopoulos I, Wickramarachchi U, Reinhold J, et al. Drug-Coated Balloon vs. Drug-Eluting Stents for De Novo Unprotected Left Main Stem Disease: The SPARTAN-LMS Study. J Cardiovasc Dev Dis 10 (2023): 84.
- Muramatsu T, Kozuma K, Tanabe K, Morino Y, Ako J et al. Task Force of the Japanese Association of Cardiovascular Intervention, Therapeutics (CVIT). Clinical expert consensus document on drug-coated balloon for coronary artery disease from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc Interv Ther 38 (2023): 166-176.
- Rykowska I, Nowak I, Nowak R. Drug-Eluting Stents and Balloons-Materials, Structure Designs, and Coating Techniques: A Review. Molecules 25 (2020): 4624.
- Verde N, Ciliberti G, Pittorino L, Ferrone M, Franzese M, et al. Contemporary Use of Drug-Coated Balloons for Coronary Angioplasty: A Comprehensive Review. J Clin Med 13 (2024): 6243.
- Jeger RV, Eccleshall S, Wan Ahmad WA, Ge J, Poerner TC, et al. International DCB Consensus Group. Drug-Coated Balloons for Coronary Artery Disease: Third Report of the International DCB Consensus Group. JACC Cardiovasc Interv 13 (2020): 1391-1402.
- Korjian S, McCarthy KJ, Larnard EA, Cutlip DE, McEntegart MB, et al. Drug-Coated Balloons in the Management of Coronary Artery Disease. Circ Cardiovasc Interv 17 (2024): e013302.
- Lazar FL, Onea HL, Olinic DM, Cortese B. A 2024 scientific update on the clinical performance of drug-coated balloons. Asia Intervention 10 (2024): 15-25.
- Camaj A, Leone PP, Colombo A, Vinayak M, Stone GW, et al. Drug-Coated Balloons for the Treatment of Coronary Artery Disease: A Review. JAMA Cardiol 10 (2025): 189-198.
- Expert Writing Committee of the Chinese Expert Consensus on Clinical Applications of Drug-Coated Balloon (2nd Edition); Ge JB, Chen YD. Chinese expert consensus on the clinical application of drug-coated balloon (2nd Edition). J Geriatr Cardiol 21 (2024): 135-152.
- Wang L, Li X, Li T, Liu L, Wang H, Wang C. Novel application of drug-coated balloons in coronary heart disease: A narrative review. Front Cardiovasc Med 10 (2023): 1055274.
- Kundu A, Moliterno DJ. Drug-Coated Balloons for In-Stent Restenosis-Finally Leaving Nothing Behind for US Patients. JAMA 331(2024): 1011-1012.
- Giacoppo D, Alfonso F, Xu B, Claessen BEPM, Adriaenssens T, et al. Drug-Coated Balloon Angioplasty Versus Drug-Eluting Stent Implantation in Patients With Coronary Stent Restenosis. J Am Coll Cardiol 75 (2020): 2664-2678.
- Sabaté M. Drug-Coated Balloon for De Novo Lesions: Back to the Past or Back to the Future? JACC Cardiovasc Interv 16 (2023): 1804-1806.
- Colombo A, Leone PP, Ploumen EH, von Birgelen C. Drug-coated balloons as a first choice for patients with de novo lesions: pros and cons. EuroIntervention 20 (2024): e120-e122.
- Jiang JL, Huang QJ, Chen MH. Efficacy and safety of drug-coated balloon for de novo lesions of large coronary arteries: Systematic review and meta-analysis of randomized controlled trials. Heliyon (2024): e25264.
- Ma Z, Liu K, Hu Y, Hu X, Wang B, Li Z. Comparison Between Drug-Coated Balloon and Stents in Large De Novo Coronary Artery Disease: A Systematic Review and Meta-Analysis of RCT Data. Cardiovasc Drugs Ther 13 (2025): 1320.
- Zhang W, Zhang M, Tian J, Zhang M, Zhou Y, Song X. Drug-Coated Balloon-Only Strategy for De Novo Coronary Artery Disease: A Meta-analysis of Randomized Clinical Trials. Cardiovasc Ther 2023 (2023): 3121601.
- Wang D, Wang X, Yang T, Tian H, Su Y, Wang Q. Drug-Coated Balloons for De Novo Coronary Artery Lesions: A Meta-Analysis of Randomized Clinical Trials. Yonsei Med J 64 (2023): 593-603.
- Gobbi C, Giangiacomi F, Merinopoulos I, Gherbesi E, Faggiano A, et al. Drug coated balloon angioplasty for de novo coronary lesions in large vessels: a systematic review and meta-analysis. Sci Rep 15 (2025): 4921.
- Zilio F, Verdoia M, De Angelis MC, Zucchelli F, Borghesi M, et al. Drug Coated Balloon in the Treatment of De Novo Coronary Artery Disease: A Narrative Review. J Clin Med 12 (2023): 3662.
- Rosenberg M, Waliszewski M, Krackhardt F, Chin K, Wan Ahmad WA, et al. Drug Coated Balloon-Only Strategy in De Novo Lesions of Large Coronary Vessels. J Interv Cardiol 2019 (2019): 6548696.
- Sciahbasi A, Mazza TM, Pidone C, Samperi S, Cittadini E, et al. A New Frontier for Drug-Coated Balloons: Treatment of "De Novo" Stenosis in Large Vessel Coronary Artery Disease. J Clin Med 13 (2024): 1320.
- Cioffi GM, Madanchi M, Attinger-Toller A, Bossard M, Cuculi F. Pushing the Boundaries: Drug-Coated Balloons to Treat a Calcified and Thrombotic Lesion in Acute Coronary Syndrome. Am J Case Rep 23 (2022): e936950.
- Su H, Li M, Hao L, Wang H. Comparison of Drug-Coated Balloons and Drug-Eluting Stents in Primary Percutaneous Coronary Interventions for ST-Segment Elevated Myocardial Infarction: A Systemic Review and Meta-Analysis. Rev Cardiovasc Med 23 (2022): 203.
- Hu H, Shen L. Drug-coated balloons in the treatment of acute myocardial infarction (Review). Exp Ther Med 21 (2021): 464.
- Sanz-Sánchez J, Teira Calderón A, Neves D, Cortés Villar C, Lukic A, et al. Culprit-Lesion Drug-Coated-Balloon Percutaneous Coronary Intervention in Patients Presenting with ST-Elevation Myocardial Infarction (STEMI). J Clin Med 14 (2025): 869.
- Kondo Y, Ishikawa T, Shimura M, Yamada K, Ukaji T, et al. Cardiovascular Outcomes after Paclitaxel-Coated Balloon Angioplasty versus Drug-Eluting Stent Placement for Acute Coronary Syndrome: A Systematic Review and Meta-Analysis. J Clin Med 13 (2024): 1481.
- Uskela S, Eranti A, Kärkkäinen JM, Rissanen TT. Drug-coated balloon-only strategy for percutaneous coronary intervention of de novo left main coronary artery disease: the importance of proper lesion preparation. Front Med 17(2023): 75-84.
- Her AY, Kim TH, Shin ES, Kim S, Kim B, et al. Drug-Coated Balloon-Based Treatment of Left Main True Bifurcation Lesion. Catheter Cardiovasc Interv 105 (2025): 1024-1031.
- Sanchez-Jimenez E, El-Mokdad R, Chaddad R, Cortese B. Drug-coated balloon for the management of coronary chronic total occlusions. Rev Cardiovasc Med 23 (2022): 42.
- Qin Q, Chen L, Ge L, Qian J, Ma J, et al. Long-term clinical outcomes of drug-coated balloon for the management of chronic total occlusions. Coron Artery Dis 34 (2023): 555-561.
- Shin ES, Her AY, Jang MH, Kim B, Kim S, et al. Impact of Drug-Coated Balloon-Based Revascularization in Patients with Chronic Total Occlusions. J Clin Med 13 (2024): 3381.
- Allana SS, Brilakis ES. What is the role of drug-coated balloons in chronic total occlusion percutaneous coronary intervention? Catheter Cardiovasc Interv 101 (2023): 957-958.
- Lazar FL, Prvulovic D, Onea HL, Cortese B. The role of drug-coated balloons for coronary bifurcation management: results from the prospective EASTBOURNE-BIF study. Minerva Cardiol Angiol 72 (2024): 346-354.
- Gao X, Tian N, Kan J, Li P, Wang M, et al. Drug-Coated Balloon Angioplasty of the Side Branch During Provisional Stenting: The Multicenter Randomized DCB-BIF Trial. J Am Coll Cardiol 85 (2025): 1-15.
- Dash D, Mody R, Ahmed N, Malan SR, Mody B. Drug-coated balloon in the treatment of coronary bifurcation lesions: A hope or hype? Indian Heart J 74 (2022): 450-457.
- Mitsui K, Lee T, Miyazaki R, Hara N, Nagamine S, et al. Drug-coated balloon strategy following orbital atherectomy for calcified coronary artery compared with drug-eluting stent: One-year outcomes and optical coherence tomography assessment. Catheter Cardiovasc Interv 102 (2023): 11-17.
- Shan Y, Lu W, Han Z, Pan S, Li X, et al. Long-term outcomes of drug-coated balloon treatment of calcified coronary artery lesions: a multicenter, retrospective, propensity matching study. Front Cardiovasc Med 10 (2023): 1122290.
- Basavarajaiah S, Loku Waduge BH, Watkin R, Athukorala S. Is a high calcific burden an indication, or a contraindication for Drug Coated Balloon? Rev Cardiovasc Med 22 (2021): 1087-1093.
- Rivero-Santana B, Jurado-Roman A, Galeote G, Jimenez-Valero S, Gonzalvez A, et al. Drug-Eluting Balloons in Calcified Coronary Lesions: A Meta-Analysis of Clinical and Angiographic Outcomes. J Clin Med 13 (2024): 2779.
- Yang X, Lu W, Pan L, Han Z, Pan S, et al. Long-term outcomes of drug-coated balloons in patients with diffuse coronary lesions. Front Cardiovasc Med 9 (2022): 935263.
- Xu H, Qiao S, Cui J, Yuan J, Yang W, et al. Drug-eluting stent and drug-coated balloon for the treatment of de novo diffuse coronary artery disease lesions: A retrospective case series study. Clin Cardiol 46 (2023): 1511-1518.
- Gonzalo N, Shabbir A. The longest way round is the shortest way home: drug-coated balloons for long lesions in large coronary arteries. EuroIntervention 19 (2023): e882-e883.
- Scheller B, Rissanen TT, Farah A, Ohlow MA, Mangner N, et al. BASKET-SMALL 2 Investigators. Drug-Coated Balloon for Small Coronary Artery Disease in Patients With and Without High-Bleeding Risk in the BASKET-SMALL 2 Trial. Circ Cardiovasc Interv 15 (2022): e011569.
- Räsänen A, Kärkkäinen JM, Eranti A, Eränen J, Rissanen TT. Percutaneous coronary intervention with drug-coated balloon-only strategy combined with single antiplatelet treatment in patients at high bleeding risk: Single center experience of a novel concept. Catheter Cardiovasc Interv 101 (2023): 569-578.
- Lim GB. Drug-coated balloons for high-bleeding-risk PCI. Nat Rev Cardiol 16 (2019): 516.
- van Veelen A, Küçük IT, Fuentes FH, Kahsay Y, Garcia-Garcia HM, et al. First-in-Human Drug-Eluting Balloon Treatment of Vulnerable Lipid-Rich Plaques: Rationale and Design of the DEBuT-LRP Study. J Clin Med. 2023 Sep 6;12(18):5807. doi: 10.3390/jcm12185807. Erratum in: J Clin Med 13 (2024): 1479.
- Zhang YB, Liu HD, Xing JH, Chen BW, Zhao YY, et al. Safety and Efficacy of Drug-Coated Balloons in Patients with Acute Coronary Syndromes and Vulnerable Plaque. Clin Appl Thromb Hemost 28 (2022): 10760296221130063.
- van Veelen A, Küçük IT, Garcia-Garcia HM, Fuentes FH, Kahsay Y, et al. Paclitaxel-coated balloons for vulnerable lipid-rich plaques. EuroIntervention 20 (2024): e826-e830.
- Mulijono D, Hutapea AM, Lister INE, Sudaryo MK, Umniyati H. Plant-Based Diet to Reverse/ Regress Vulnerable Plaque: A Case Report and Review. Archives of Clinical and Medical Case Reports 8 (2024): 126-135.
- Mulijono D. Plant-Based Diet in Regressing/Stabilizing Vulnerable Plaques to Achieve Complete Revascularization. Archives of Clinical and Biomedical Research 8 (2024): 236-244.
- Mulijono D, Hutapea AM, Lister INE, Sudaryo MK, Umniyati H. Mechanisms Plant-Based Diets Reverse Atherosclerosis. Cardiology and Cardiovascular Medicine 8 (2024): 290-302.
- Mulijono D, Hutapea AM, Lister INE, Sudaryo MK, Umniyati H. How a Plant-Based Diet (PBD) Reduces In-Stent Restenosis (ISR) and Stent Thrombosis (ST). Cardio Open 9 (2024): 01-15.
- Lin S, Xiao-Ming W, Gui-Fu W. Expert consensus on the clinical application of enhanced external counterpulsation in elderly people (2019). Aging Med (Milton) 3 (2020): 16-24.
- Akula A, Grafft HR, Tak N, Haberman DA, Tak T. Enhanced External Counterpulsation Outcomes Study: Retrospective Analyses of Data Obtained from Patients at a Single Medical Center in United States. Int J Angiol 33 (2024): 182-188.
- Villarruz-Sulit MV, Forster R, Dans AL, Tan FN, Sulit DV. Chelation therapy for atherosclerotic cardiovascular disease. Cochrane Database Syst Rev 5 (2020): CD002785.
- Ravalli F, Vela Parada X, Ujueta F, Pinotti R, Anstrom KJ, et al. Chelation Therapy in Patients With Cardiovascular Disease: A Systematic Review. J Am Heart Assoc 11 (2022): e024648.
- Bajwa J, Munir U, Nori A, Williams B. Artificial intelligence in healthcare: transforming the practice of medicine. Future Healthc J 8 (2021): e188-e194.
- Al Kuwaiti A, Nazer K, Al-Reedy A, Al-Shehri S, Al-Muhanna A, et al. A Review of the Role of Artificial Intelligence in Healthcare. J Pers Med 13 (2023): 951.
- London AJ. Artificial intelligence in medicine: Overcoming or recapitulating structural challenges to improving patient care? Cell Rep Med 3 (2022): 100622.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 