Prevalence and Pattern of Dyslipidemia in a Patient with Type 2 DM in North Eastern Region of Bangladesh
Swapan Kumar Singha1, Mohammad Zabed Jillul Bari2, Md. Jahangir Khan3, Md. Solaiman Mia4, Halima Naznin5, Partha Sarathi Roy Chowdhury6, Golam Md. Moin Uddin7, Mst. Ruzina Rahman8, Sunia Sinha9, Soumitra Sinha10
1Assistant Professor, Department of Medicine, Habiganj Medical College, Habiganj, Bangladesh
2Professor (Principal and Head), Department of Medicine, Habiganj Medical College, Habiganj, Bangladesh
3Associate Professor, Department of Biochemistry, Habiganj Medical College, Habiganj, Bangladesh
4Assistant Professor, Department of Cardiology, Habiganj Medical College, Habiganj, Bangladesh.
5Assistant Professor, Department of Gynecology and Obstetric, Habiganj Medical College, Habiganj, Bangladesh
6Junior Consultant, Department of Cardiology, 250 Bed Sadar Hospital, Habiganj, Bangladesh
7Assistant Professor, Department of Community Medicine, Habiganj Medical College, Habiganj, Bangladesh
8Registrar, Department of Paediatrics, Habiganj Medical College, Habiganj, Bangladesh
9OSD, Director General of Health Services, Attachment : Department of Pathology, Sylhet MAG Osmani Medical College, Bangladesh
10Pathologist, Department of Pathology, 250 Beded General Hospital, Moulvibazar, Bangladesh
*Corresponding author: Swapan Kumar Singha, Assistant Professor, Department of Medicine, Habiganj Medical College, Habiganj. Bangladesh.
Received: 23 May 2025; Accepted: 05 Aug 2025; Published: 08 July 2025
Article Information
Citation: Swapan Kumar Singha, Mohammad Zabed Jillul Bari, Mohammad Jahangir Khan, Mohammad Solaiman Mia, Halima Naznin, Partha Sarathi Roy Chowdhury, Golam Md. Moin Uddin, Mst. Ruzina Rahman, Sunia Sinha, Soumitra Sinha. Prevalence and Pattern of Dyslipidemia in a Patient with Type 2 DM in North Eastern Region of Bangladesh. Cardiology and Cardiovascular Medicine 9 (2025): 334-343.
View / Download Pdf Share at FacebookAbstract
Background: Dyslipidemia is a major modifiable risk factor for cardiovascular disease among patients with Type 2 diabetes mellitus (T2DM). However, data on the prevalence and patterns of dyslipidemia in diabetic patients from the northeastern region of Bangladesh are limited. This study aimed to investigate the prevalence, patterns, and associated factors of dyslipidemia among patients with T2DM in this region. Methods: This cross-sectional study included 200 patients with T2DM from the northeastern region of Bangladesh. Demographic and clinical data were collected using a structured questionnaire. Anthropometric measurements and blood pressure were recorded, and blood samples were collected for assessment of glycemic parameters and lipid profile. Dyslipidemia was defined according to the National Cholesterol Education Program Adult Treatment Panel III guidelines. Statistical analyses were performed using SPSS version 25.0. Results: The overall prevalence of dyslipidemia was 87.5%, with high LDL-C being the most common lipid abnormality (72.0%), followed by hypertriglyceridemia (63.5%), hypercholesterolemia (60.5%), and low HDL-C (54.0%). Among patients with dyslipidemia, 34.3% had all four lipid abnormalities concurrently. Female patients had significantly higher total cholesterol (212.6 ± 46.7 vs. 198.3 ± 41.9 mg/dL, p=0.031) and LDL-C (131.5 ± 39.2 vs. 118.7 ± 35.6 mg/dL, p=0.024) levels, while males had lower HDL-C (37.4 ± 8.6 vs. 42.9 ± 9.8 mg/dL, p=0.001). Multivariate analysis identified age ≥50 years (adjusted OR=2.31, 95% CI: 1.18-4.52), female gender (adjusted OR=1.87, 95% CI: 1.06-3.29), duration of diabetes ≥5 years (adjusted OR=2.63, 95% CI: 1.35-5.12), poor glycemic control (HbA1c ≥7%) (adjusted OR=3.18, 95% CI: 1.72-5.88), and BMI ≥25 kg/ m² (adjusted OR=2.05, 95% CI: 1.14-3.69) as independent predictors of dyslipidemia. A significant correlation was observed between HbA1c and all lipid parameters. Conclusion: The alarmingly high prevalence of dyslipidemia among T2DM patients in northeastern Bangladesh, particularly the high proportion with multiple concurrent lipid abnormalities, emphasizes the need for regular screening and aggressive management of dyslipidemia in this population. The identified risk factors should guide targeted interventions to reduce cardiovascular risk in this vulnerable population.
Keywords
Type 2 Diabetes Mellitus; Dyslipidemia; Lipid Profile; Cardiovascular Risk; Bangladesh
Article Details
1. Introduction
Diabetes mellitus (DM) represents one of the most significant global health challenges of the 21st century, with Type 2 diabetes mellitus (T2DM) accounting for approximately 90-95% of all diabetes cases worldwide [1]. The International Diabetes Federation (IDF) estimated that 537 million adults were living with diabetes in 2021, with projections suggesting this number could rise to 783 million by 2045 [2]. In Bangladesh, the prevalence of diabetes has been increasing at an alarming rate, with recent studies indicating that approximately 8.4-10.7% of the adult population is affected, placing a substantial burden on the nation's healthcare system [3].
Type 2 diabetes is characterized by insulin resistance and relative insulin deficiency, leading to chronic hyperglycemia and various metabolic abnormalities [4]. Among these metabolic disturbances, dyslipidemia is particularly concerning as it significantly increases cardiovascular disease (CVD) risk, which remains the leading cause of morbidity and mortality in diabetic populations [5]. Diabetic dyslipidemia typically presents with elevated triglycerides, decreased high-density lipoprotein cholesterol (HDL-C), and increased small dense low-density lipoprotein (LDL) particles, often referred to as the "atherogenic lipid triad" [6].
The relationship between T2DM and dyslipidemia is complex and bidirectional. Insulin resistance, which precedes the development of T2DM, affects lipid metabolism by increasing free fatty acid flux from adipose tissue to the liver, enhancing very low-density lipoprotein (VLDL) production, and reducing lipoprotein lipase activity [7]. Conversely, dyslipidemia can exacerbate insulin resistance through lipotoxicity mechanisms, creating a vicious cycle that accelerates the progression of both conditions [8].
In Bangladesh, particularly in the northeastern region, the pattern and prevalence of dyslipidemia in T2DM patients have not been extensively studied [9]. This region presents unique demographic, socioeconomic, and cultural characteristics that may influence both the development of T2DM and associated lipid abnormalities [10]. Dietary habits, physical activity levels, genetic factors, and access to healthcare services vary significantly across Bangladesh, potentially contributing to regional variations in the manifestation of diabetic dyslipidemia [11].
Early detection and management of dyslipidemia in T2DM patients are crucial for preventing cardiovascular complications and reducing overall mortality [12]. However, implementing effective prevention and treatment strategies requires a comprehensive understanding of the local patterns and determinants of dyslipidemia in specific populations [13]. This research aims to address this knowledge gap by investigating the prevalence and patterns of dyslipidemia among T2DM patients in the northeastern region of Bangladesh, providing valuable insights for clinicians and policymakers to develop targeted interventions for this high-risk population [14,15].
2. Materials and Methods
2.1 Study Design and Setting
This cross-sectional observational study was conducted in the Northeastern Region of Bangladesh from August 2024 to January 2025. Patients were recruited from the outpatient departments of major tertiary care hospitals and specialized diabetes care centers in the region . The study protocol was approved by the Institutional Ethics Committee (Reference No.59.14.3600.155.000.99.0004.23.567(3) Date 01/08/2024), and all procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments [16].
2.2. Study Population
A total of 200 patients with previously diagnosed Type 2 diabetes mellitus were enrolled in the study using a systematic random sampling technique. The sample size was calculated using the formula n = Z²P(1-P)/d², where Z is the confidence level at 95% (1.96), P is the expected prevalence of dyslipidemia in diabetic patients based on previous studies (50%), and d is the margin of error (7%) [17]. Patients aged 18 years and above with confirmed diagnosis of Type 2 diabetes mellitus according to the American Diabetes Association criteria were included in the study [18]. Patients with type 1 diabetes, gestational diabetes, secondary diabetes and acute illness were excluded.
2.3. Data Collection
After obtaining written informed consent, demographic and clinical data were collected using a structured questionnaire through face-to-face interviews. The questionnaire included information on age, sex, occupation, smoking status, non-smoking tobacco use, food habits, family history of T2DM, duration of diabetes, blood pressure medication, and history of chronic kidney disease. Anthropometric measurements including height, weight, body mass index (BMI), and waist circumference were recorded using standardized techniques [19]. BMI was calculated as weight in kilograms divided by height in meters squared.
2.4. Clinical and Laboratory Assessments
Blood pressure was measured in a seated position after at least 5 minutes of rest using a standard mercury sphygmomanometer, with the average of two readings recorded [20]. Venous blood samples were collected after an overnight fast of at least 8 hours. Fasting plasma glucose (FPG), 2-hour postprandial glucose (2HAPPG), glycated hemoglobin (HbA1c), serum creatinine, and alanine aminotransferase (ALT) were measured using standard laboratory methods.
The lipid profile, which included total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglycerides (TG), was assessed using enzymatic colorimetric methods with an automated analyzer (Hitachi 902, Japan) [21]. The TC/HDL ratio was calculated by dividing the total cholesterol by HDL-C values. Estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI equation [22].
2.6. Definition of Dyslipidemia
Dyslipidemia was defined according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) guidelines [23]. The cutoff values were as follows: hypercholesterolemia (TC ≥ 200 mg/dL), hypertriglyceridemia (TG ≥ 150 mg/dL), high LDL-C (LDL-C ≥ 100 mg/dL), low HDL-C (HDL-C < 40 mg/dL for males and < 50 mg/dL for females), and high TC/HDL ratio (> 4.5). A patient was considered to have dyslipidemia if at least one of these parameters was abnormal [24].
2.7. Statistical Analysis
Data were analyzed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as mean ± standard deviation (SD) or median with interquartile range (IQR) depending on the distribution of data. Categorical variables were presented as frequencies and percentages. The Kolmogorov-Smirnov test was used to check the normality of the data distribution. The prevalence of dyslipidemia was calculated as the percentage of patients with at least one abnormal lipid parameter. Chi-square test or Fisher's exact test was used to examine the association between categorical variables. Independent t-test or Mann-Whitney U test was employed to compare continuous variables between groups. Bivariate and multivariate logistic regression analyses were performed to identify factors associated with dyslipidemia, with results expressed as odds ratios (OR) with 95% confidence intervals (CI). A p-value < 0.05 was considered statistically significant.
3. Results
3.1. Demographic and Clinical Characteristics
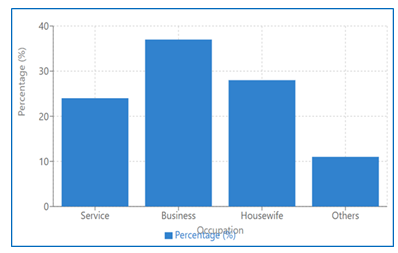
A total of 200 patients with Type 2 diabetes mellitus from the northeastern region of Bangladesh were included in this study. The demographic and clinical characteristics of the study population are presented in Table 1. The mean age of the participants was 53.8 ± 11.4 years, with a male predominance (67.5%). The median duration of diabetes was 7.0 years (IQR: 3.0-12.0). The majority of patients (58.5%) had a family history of T2DM, and 43.5% were on antihypertensive medication. The mean BMI was 26.9 ± 3.7 kg/m², indicating that most patients were overweight according to WHO Asian criteria.
|
Characteristics |
Value |
|
Age (years), mean ± SD |
53.8 ± 11.4 |
|
Sex, n (%) |
|
|
Male |
135 (67.5) |
|
Female |
65 (32.5) |
|
Occupation, n (%) |
|
|
Service |
48 (24.0) |
|
Business |
74 (37.0) |
|
Housewife |
56 (28.0) |
|
Others |
22 (11.0) |
|
Smoking status, n (%) |
|
|
Current smoker |
53 (26.5) |
|
Non-smoker |
147 (73.5) |
|
Non-smoking tobacco use, n (%) |
62 (31.0) |
|
Food habit, n (%) |
|
|
Vegetarian |
14 (7.0) |
|
Non-vegetarian |
186 (93.0) |
|
Family history of T2DM, n (%) |
117 (58.5) |
|
Duration of DM (years), median (IQR) |
7.0 (3.0-12.0) |
|
On antihypertensive medication, n (%) |
87 (43.5) |
|
History of CKD, n (%) |
23 (11.5) |
|
BMI (kg/m²), mean ± SD |
26.9 ± 3.7 |
|
Waist circumference (cm), mean ± SD |
|
|
Male |
91.7 ± 9.3 |
|
Female |
87.2 ± 8.6 |
|
Blood pressure (mmHg), mean ± SD |
|
|
Systolic |
131.5 ± 17.2 |
|
Diastolic |
79.8 ± 9.3 |
SD: Standard deviation; IQR: Interquartile range; T2DM: Type 2 diabetes mellitus; CKD: Chronic kidney disease; BMI: Body mass index
Table 1: Demographic and Clinical Characteristics of the Study Population (N=200).
3.2. Glycemic and Biochemical Parameters
The glycemic and biochemical parameters of the study participants are summarized in Table 2. The mean HbA1c was 8.7 ± 2.1%, indicating poor glycemic control among the majority of patients. The mean fasting plasma glucose was 9.8 ± 3.7 mmol/L, and the mean 2-hour postprandial glucose was 13.4 ± 4.9 mmol/L. The mean serum creatinine was 1.1 ± 0.4 mg/dL, and the mean ALT was 36.7 ± 18.9 U/L.
|
Parameters |
Value |
|
FPG (mmol/L), mean ± SD |
9.8 ± 3.7 |
|
2HAPPG (mmol/L), mean ± SD |
13.4 ± 4.9 |
|
HbA1c (%), mean ± SD |
8.7 ± 2.1 |
|
Serum creatinine (mg/dL), mean ± SD |
1.1 ± 0.4 |
|
eGFR (mL/min/1.73m²), mean ± SD |
76.3 ± 22.5 |
|
ALT (U/L), mean ± SD |
36.7 ± 18.9 |
SD: Standard deviation; FPG: Fasting plasma glucose; 2HAPPG: 2-hour postprandial glucose; HbA1c: Glycated hemoglobin; eGFR: Estimated glomerular filtration rate; ALT: Alanine aminotransferase
Table 2: Glycemic and Biochemical Parameters of the Study Population (N=200).
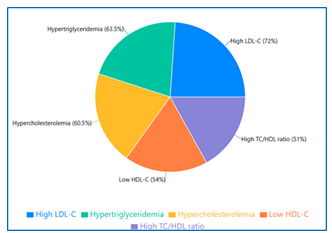
3.3. Prevalence of Dyslipidemia
The overall prevalence of dyslipidemia in our study population was 87.5% (175/200). The prevalence of individual lipid abnormalities is shown in Table 3. High LDL-C was the most common lipid abnormality (72.0%), followed by hypertriglyceridemia (63.5%), hypercholesterolemia (60.5%), low HDL-C (54.0%), and high TC/HDL ratio (51.0%).
|
Lipid Abnormalities |
n (%) |
|
Overall dyslipidemia (at least one abnormal lipid parameter) |
175 (87.5) |
|
Hypercholesterolemia (TC ≥ 200 mg/dL) |
121 (60.5) |
|
Hypertriglyceridemia (TG ≥ 150 mg/dL) |
127 (63.5) |
|
High LDL-C (LDL-C ≥ 100 mg/dL) |
144 (72.0) |
|
Low HDL-C (< 40 mg/dL for males, < 50 mg/dL for females) |
108 (54.0) |
|
High TC/HDL ratio (> 4.5) |
102 (51.0) |
TC: Total cholesterol; TG: Triglycerides; LDL-C: Low-density lipoprotein cholesterol; HDL-C: High-density lipoprotein cholesterol
Table 3: Prevalence of Dyslipidemia and Lipid Abnormalities (N=200).
3.4. Patterns of Dyslipidemia
The patterns of dyslipidemia among the study participants are presented in Table 4. Among patients with dyslipidemia, 34.3% had all four lipid abnormalities (hypercholesterolemia, hypertriglyceridemia, high LDL-C, and low HDL-C), while 28.0% had three abnormalities, 18.3% had two abnormalities, and 6.9% had only one abnormal lipid parameter.
|
Pattern of Dyslipidemia |
n (%) |
|
Isolated hypercholesterolemia |
3 (1.7) |
|
Isolated hypertriglyceridemia |
5 (2.9) |
|
Isolated high LDL-C |
3 (1.7) |
|
Isolated low HDL-C |
1 (0.6) |
|
Hypercholesterolemia + hypertriglyceridemia |
8 (4.6) |
|
Hypercholesterolemia + high LDL-C |
12 (6.9) |
|
Hypercholesterolemia + low HDL-C |
3 (1.7) |
|
Hypertriglyceridemia + high LDL-C |
6 (3.4) |
|
Hypertriglyceridemia + low HDL-C |
2 (1.1) |
|
High LDL-C + low HDL-C |
1 (0.6) |
|
Hypercholesterolemia + hypertriglyceridemia + high LDL-C |
18 (10.3) |
|
Hypercholesterolemia + hypertriglyceridemia + low HDL-C |
11 (6.3) |
|
Hypercholesterolemia + high LDL-C + low HDL-C |
9 (5.1) |
|
Hypertriglyceridemia + high LDL-C + low HDL-C |
11 (6.3) |
|
All four lipid abnormalities |
60 (34.3) |
|
Dyslipidemia with high TC/HDL ratio only |
22 (12.6) |
LDL-C: Low-density lipoprotein cholesterol; HDL-C: High-density lipoprotein cholesterol; TC: Total cholesterol
Table 4: Patterns of Dyslipidemia Among Study Participants (N=175)
3.5. Lipid Profile Parameters by Gender
The comparison of lipid profile parameters between male and female patients is shown in Table 5. The mean total cholesterol (212.6 ± 46.7 vs. 198.3 ± 41.9 mg/dL, p=0.031) and LDL-C (131.5 ± 39.2 vs. 118.7 ± 35.6 mg/dL, p=0.024) were significantly higher in females compared to males. Conversely, the mean HDL-C was significantly lower in males than in females (37.4 ± 8.6 vs. 42.9 ± 9.8 mg/dL, p=0.001). There was no significant gender difference in triglyceride levels and TC/HDL ratio.
|
Parameters |
Male (n=135) |
Female (n=65) |
p-value |
|
TC (mg/dL), mean ± SD |
198.3 ± 41.9 |
212.6 ± 46.7 |
0.031* |
|
LDL-C (mg/dL), mean ± SD |
118.7 ± 35.6 |
131.5 ± 39.2 |
0.024* |
|
HDL-C (mg/dL), mean ± SD |
37.4 ± 8.6 |
42.9 ± 9.8 |
0.001* |
|
TG (mg/dL), mean ± SD |
192.5 ± 102.7 |
181.6 ± 95.3 |
0.469 |
|
TC/HDL ratio, mean ± SD |
5.5 ± 1.7 |
5.1 ± 1.4 |
0.096 |
*TC: Total cholesterol; LDL-C: Low-density lipoprotein cholesterol; HDL-C: High-density lipoprotein cholesterol; TG: Triglycerides; SD: Standard deviation; Statistically significant (p<0.05)
Table 5: Comparison of Lipid Profile Parameters Between Male and Female Patients.
3.6. Factors Associated with Dyslipidemia
The factors associated with dyslipidemia are presented in Table 6. In multivariate logistic regression analysis, after adjusting for potential confounders, the factors independently associated with dyslipidemia were age ≥50 years (adjusted OR=2.31, 95% CI: 1.18-4.52, p=0.015), female gender (adjusted OR=1.87, 95% CI: 1.06-3.29, p=0.031), duration of diabetes ≥5 years (adjusted OR=2.63, 95% CI: 1.35-5.12, p=0.004), poor glycemic control (HbA1c ≥7%) (adjusted OR=3.18, 95% CI: 1.72-5.88, p<0.001), and BMI ≥25 kg/m² (adjusted OR=2.05, 95% CI: 1.14-3.69, p=0.017).
|
Factors |
Crude OR (95% CI) |
p-value |
Adjusted OR (95% CI) |
p-value |
|
Age ≥50 years |
2.15 (1.14-4.07) |
0.018* |
2.31 (1.18-4.52) |
0.015* |
|
Female gender |
1.65 (0.98-2.79) |
0.062 |
1.87 (1.06-3.29) |
0.031* |
|
Current smoker |
1.41 (0.81-2.45) |
0.224 |
1.27 (0.69-2.31) |
0.443 |
|
Family history of T2DM |
1.58 (0.96-2.59) |
0.071 |
1.47 (0.86-2.52) |
0.163 |
|
Duration of DM ≥5 years |
2.39 (1.29-4.43) |
0.006* |
2.63 (1.35-5.12) |
0.004* |
|
HbA1c ≥7% |
2.96 (1.67-5.25) |
<0.001* |
3.18 (1.72-5.88) |
<0.001* |
|
BMI ≥25 kg/m² |
1.89 (1.09-3.27) |
0.023* |
2.05 (1.14-3.69) |
0.017* |
|
Hypertension |
1.64 (0.99-2.72) |
0.056 |
1.53 (0.88-2.66) |
0.133 |
*OR: Odds ratio; CI: Confidence interval; T2DM: Type 2 diabetes mellitus; DM: Diabetes mellitus; HbA1c: Glycated hemoglobin; BMI: Body mass index; Statistically significant (p<0.05).
Table 6: Factors Associated with Dyslipidemia in Multivariate Logistic Regression Analysis.
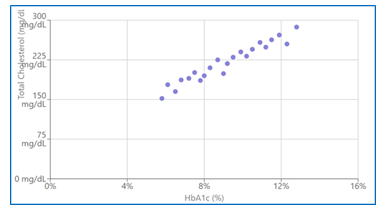
3.7. Correlation Between Glycemic Control and Lipid Parameters
The correlation between glycemic control (HbA1c) and lipid parameters is presented in Table 7. HbA1c showed a significant positive correlation with total cholesterol (r=0.347, p<0.001), LDL-C (r=0.329, p<0.001), triglycerides (r=0.384, p<0.001), and TC/HDL ratio (r=0.376, p<0.001). A significant negative correlation was observed between HbA1c and HDL-C (r=-0.254, p<0.001).
|
Lipid Parameters |
Correlation Coefficient (r) |
p-value |
|
Total cholesterol |
0.347 |
<0.001* |
|
LDL-C |
0.329 |
<0.001* |
|
HDL-C |
-0.254 |
<0.001* |
|
Triglycerides |
0.384 |
<0.001* |
|
TC/HDL ratio |
0.376 |
<0.001* |
*LDL-C: Low-density lipoprotein cholesterol; HDL-C: High-density lipoprotein cholesterol; TC: Total cholesterol; Statistically significant (p<0.05)
Table 7: Correlation Between HbA1c and Lipid Parameters.
3.8. Prevalence of Dyslipidemia Based on Duration of Diabetes
The prevalence of dyslipidemia according to the duration of diabetes is illustrated in Table 8. Patients with longer duration of diabetes (≥10 years) had significantly higher prevalence of dyslipidemia (96.4%) compared to those with 5-9 years (89.7%) and <5 years (77.8%) duration (p=0.003).
|
Duration of Diabetes |
Total Patients |
Patients with Dyslipidemia |
Prevalence (%) |
p-value |
|
<5 years |
63 |
49 |
77.8 |
0.003* |
|
5-9 years |
78 |
70 |
89.7 |
|
|
≥10 years |
56 |
54 |
96.4 |
|
|
Unknown |
3 |
2 |
66.7 |
Statistically significant (p<0.05) using Chi-square test
Table 8: Prevalence of Dyslipidemia Based on Duration of Diabetes.
4. Discussion
The present study investigated the prevalence and patterns of dyslipidemia among patients with Type 2 diabetes mellitus in the northeastern region of Bangladesh. Our findings revealed a markedly high prevalence of dyslipidemia (87.5%) in this population, with high LDL-C being the most common lipid abnormality. Several factors including age ≥50 years, female gender, longer duration of diabetes, poor glycemic control, and overweight/obesity were independently associated with dyslipidemia [25].
The overall prevalence of dyslipidemia in our study (87.5%) is consistent with previous studies conducted in different regions of Bangladesh. Islam et al. reported a prevalence of 85.8% in a study conducted in Dhaka city [26], while Rahman et al. found a prevalence of 83.4% among diabetic patients in Sylhet division [27]. Our findings are also comparable to studies from neighboring countries; Lakshminarayanan et al. reported a prevalence of 85.5% in India [28], and Aryal et al. found 88.1% in Nepal [29]. However, our prevalence is somewhat higher than those reported in Western populations. For instance, Jacobs et al. observed a prevalence of 77.2% among diabetic patients in the United States [30], and Taskinen et al. reported 76.8% in European populations [31]. These differences may be attributed to variations in dietary habits, physical activity levels, genetic factors, and access to healthcare services across different populations.
Regarding the pattern of dyslipidemia, our study identified high LDL-C (72.0%) as the most prevalent lipid abnormality, followed by hypertriglyceridemia (63.5%), hypercholesterolemia (60.5%), and low HDL-C (54.0%). This pattern differs somewhat from the classical diabetic dyslipidemia described in literature, which typically features hypertriglyceridemia and low HDL-C as the predominant abnormalities [32]. Wu and Parhofer reported that elevated triglycerides and decreased HDL-C were the most common lipid abnormalities in Asian diabetic populations [33]. The higher prevalence of elevated LDL-C in our study population may be explained by several factors, including dietary patterns rich in saturated fats, sedentary lifestyle, and possibly inadequate use of lipid-lowering medications among diabetic patients in this region [34].
Interestingly, our study found that 34.3% of dyslipidemic patients exhibited all four lipid abnormalities concurrently. This high prevalence of combined dyslipidemia is concerning as it substantially increases cardiovascular risk. Arca et al. demonstrated that patients with multiple lipid abnormalities have a 2-4 fold higher risk of cardiovascular events compared to those with a single abnormality [35]. Similarly, the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Lipid trial emphasized that addressing multiple lipid abnormalities is essential for comprehensive cardiovascular risk reduction in diabetic patients [36].
Gender differences in lipid profiles were notable in our study, with females having significantly higher total cholesterol and LDL-C levels, while males had lower HDL-C. These findings align with the study by Bhowmik et al. conducted in rural Bangladesh, which reported similar gender differences in lipid parameters among diabetic patients [37]. Hormonal factors, particularly the loss of estrogen's protective effect after menopause, may contribute to the relatively adverse lipid profile in diabetic women [38]. Estrogen is known to increase HDL-C and decrease LDL-C levels, and its decline during menopause can lead to a more atherogenic lipid profile [39]. Additionally, Zhang et al. suggested that women with diabetes experience a greater deterioration in their lipid profile compared to men, possibly due to differences in fat distribution and insulin sensitivity [40].
Our study identified several factors independently associated with dyslipidemia. Age ≥50 years was significantly associated with dyslipidemia (adjusted OR=2.31), consistent with findings from Akter et al., who reported increasing prevalence of dyslipidemia with advancing age among Bangladeshi adults [41]. Aging is associated with changes in body composition, reduced physical activity, and alterations in liver metabolism, all of which can adversely affect lipid profiles [42].
Duration of diabetes ≥5 years was strongly associated with dyslipidemia in our study (adjusted OR=2.63). This finding is supported by Santos-Gallego et al., who demonstrated progressive deterioration of lipid profiles with increasing duration of diabetes [43]. Chronic hyperglycemia leads to increased insulin resistance, hepatic very low-density lipoprotein production, and impaired lipoprotein lipase activity, resulting in worsening dyslipidemia over time [44].
Poor glycemic control (HbA1c ≥7%) emerged as the strongest predictor of dyslipidemia in our study (adjusted OR=3.18). The UK Prospective Diabetes Study (UKPDS) similarly demonstrated a strong association between glycemic control and lipid abnormalities [45]. We observed significant correlations between HbA1c and all lipid parameters, particularly with triglycerides (r=0.384) and TC/HDL ratio (r=0.376). Verges reported that hyperglycemia increases hepatic de novo lipogenesis and decreases apolipoprotein B degradation, leading to increased VLDL production and subsequent dyslipidemia [46]. Additionally, glycation of apolipoproteins can impair their function and clearance, further exacerbating lipid abnormalities [47].
BMI ≥25 kg/m² was also independently associated with dyslipidemia (adjusted OR=2.05). This finding aligns with the multicenter CURES study by Mohan, et al., which demonstrated that overweight and obese diabetic patients had significantly worse lipid profiles compared to normal-weight counterparts [48]. Adipose tissue, particularly visceral fat, is metabolically active and produces various adipokines and inflammatory mediators that can promote insulin resistance and dyslipidemia [49]. Bays et al. described this relationship as "adiposopathy" or "sick fat," emphasizing that adipose tissue dysfunction rather than just adiposity itself contributes to metabolic abnormalities [50].
The alarmingly high prevalence of dyslipidemia observed in our study underscores the need for regular lipid screening and aggressive management strategies in diabetic patients. The American Diabetes Association recommends annual lipid profile assessment for most diabetic patients, with more frequent monitoring for those with abnormal values [51]. Despite these recommendations, studies from low and middle-income countries like Bangladesh suggest that lipid monitoring is often inadequate in clinical practice [52].
Furthermore, our findings of multiple concurrent lipid abnormalities in a substantial proportion of patients highlight the importance of comprehensive lipid management beyond just LDL-C-focused approaches. While statins remain the cornerstone of dyslipidemia management in diabetes, combination therapy may be necessary for patients with multiple lipid abnormalities [53]. The dyslipidemia in our study population, with high prevalence of elevated triglycerides and low HDL-C alongside high LDL-C, suggests that a more nuanced approach to lipid management may be beneficial. Combination of statins with fibrates or other agents has shown promise in addressing the complex dyslipidemia associated with diabetes, though concerns about adverse effects necessitate careful monitoring [54].
The strong association between glycemic control and dyslipidemia observed in our study emphasizes the importance of integrated management approaches. The Steno-2 study demonstrated that multifactorial intervention addressing hyperglycemia, dyslipidemia, hypertension, and other risk factors significantly reduced cardiovascular complications and mortality in type 2 diabetes [55]. Therefore, healthcare providers in this region should focus on comprehensive risk factor management rather than addressing these issues in isolation.
Finally, the regional context of our findings deserves consideration. The northeastern region of Bangladesh has unique demographic, socioeconomic, and cultural characteristics that may influence both the development of T2DM and associated lipid abnormalities [56]. Traditional dietary patterns in this region often include high consumption of polished rice, saturated fats, and limited intake of fruits and vegetables, which may contribute to the observed lipid abnormalities [57]. Additionally, Rahman et al. reported that access to healthcare services, including specialized diabetes care and lipid management, is limited in this region compared to urban centers like Dhaka [58]. These contextual factors should be considered when developing interventions to address dyslipidemia in this population.
Our study has several implications for clinical practice and public health. First, it highlights the need for routine lipid screening in all diabetic patients, regardless of age or gender. Second, it emphasizes the importance of aggressive glycemic control as a strategy for improving lipid profiles. Third, it suggests that multifactorial risk reduction approaches addressing diet, physical activity, and pharmaceutical management may be particularly beneficial in this population. Finally, it underscores the need for region-specific interventions that consider the unique cultural, dietary, and healthcare access factors in northeastern Bangladesh.
Despite the comprehensive nature of our study, several limitations should be acknowledged. The cross-sectional design precludes establishment of causal relationships between the identified factors and dyslipidemia. Information on medication use, particularly lipid-lowering therapies, was not fully captured, which might have influenced the observed lipid profiles. Additionally, our study did not assess more advanced lipid parameters such as apolipoprotein levels, LDL particle size, or non-HDL cholesterol, which might provide further insights into cardiovascular risk in this population.
5. Limitations
The study’s cross-sectional nature limits the ability to establish causality between Type 2 diabetes and dyslipidemia. It only provides a snapshot of the prevalence and pattern of dyslipidemia at a specific point in time.The sample was selected from a single region in northeastern Bangladesh, which may not be representative of the entire population of Type 2 diabetes patients in the country. This may limit the generalizability of the findings to other regions with different socioeconomic, dietary, and lifestyle factors.The study relies on self-reported data for the collection of some demographic and clinical information, which could introduce recall bias or inaccuracies in reporting.Other factors that influence dyslipidemia, such as genetics, medication use, and physical activity, were not thoroughly controlled for in this study, which could affect the results.Since this is a cross-sectional study, there is no follow-up to observe changes in lipid profiles over time or the impact of interventions on dyslipidemia.
6. Conclusion
This cross-sectional study conducted in the northeastern region of Bangladesh reveals an alarmingly high prevalence of dyslipidemia (87.5%) among patients with Type 2 diabetes mellitus. High LDL-C was the most common lipid abnormality, followed by hypertriglyceridemia, hypercholesterolemia, and low HDL-C. A substantial proportion of patients (34.3%) exhibited all four lipid abnormalities concurrently, indicating a severe atherogenic profile that significantly increases cardiovascular risk.
Several factors were independently associated with dyslipidemia in this population, including age ≥50 years, female gender, longer duration of diabetes (≥5 years), poor glycemic control (HbA1c ≥7%), and overweight/obesity (BMI ≥25 kg/m²). A significant correlation was observed between glycemic control and lipid parameters, with higher HbA1c values associated with worse lipid profiles, highlighting the interconnected nature of glucose and lipid metabolism in diabetes.
The distinctive pattern of dyslipidemia observed in our study population, characterized by a high prevalence of elevated LDL-C alongside the classical diabetic dyslipidemia features of hypertriglyceridemia and low HDL-C, suggests that comprehensive lipid management strategies are essential. The traditional focus on LDL-C reduction alone may be insufficient for optimal cardiovascular risk reduction in this population.
Our findings emphasize the critical need for regular lipid screening and aggressive management of dyslipidemia in patients with Type 2 diabetes mellitus. Healthcare providers should adopt an integrated approach that addresses both glycemic control and lipid abnormalities, along with other cardiovascular risk factors. Region-specific interventions that consider the unique demographic, socioeconomic, and cultural characteristics of northeastern Bangladesh are necessary to effectively combat the high burden of dyslipidemia and reduce cardiovascular risk in this vulnerable population.
Future longitudinal studies are warranted to establish causal relationships and evaluate the long-term impact of different intervention strategies on dyslipidemia and cardiovascular outcomes in this population. Additionally, research into cost-effective approaches for screening and managing dyslipidemia in resource-limited settings like northeastern Bangladesh would be valuable for informing public health policies and clinical practice guidelines.
13. References
- International Diabetes Federation. IDF Diabetes Atlas, 10th Brussels, Belgium: International Diabetes Federation, 2021.
- Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 14 (2018): 88-98.
- Akhter S, Begum N, Ferdousi S, Khan SH, Ali T. Prevalence of diabetes mellitus in Bangladesh: a systematic review and meta-analysis. Diabetes Metab Syndr 15 (2021): 102166.
- Defronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 58 (2009): 773-795.
- Leon BM, Maddox TM. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes 6 (2015): 1246-1258.
- Wu L, Parhofer KG. Diabetic dyslipidemia. Metabolism 63 (2014): 1469-1479.
- Taskinen MR, Borén J. New insights into the pathophysiology of dyslipidemia in type 2 diabetes. Atherosclerosis 239 (2015): 483-495.
- Parhofer KG. Interaction between glucose and lipid metabolism: more than diabetic dyslipidemia. Diabetes Metab J 39 (2015): 353-362.
- Khan MMH, Gruebner O, Kraemer A. The geography of diabetes among the general adults aged 35 years and older in Bangladesh: recent evidence from a cross-sectional survey. PLoS One 9 (2014): e110756.
- Biswas T, Islam MS, Linton N, Rawal LB. Socioeconomic inequality of chronic non-communicable diseases in Bangladesh. PLoS One 11 (2016): e0167140.
- Bhowmik B, Afsana F, Siddiquee T, Munir SB, Sheikh F, et al. Comparison of the prevalence of metabolic syndrome and its association with diabetes and cardiovascular disease in the rural population of Bangladesh using the modified National Cholesterol Education Program Expert Panel Adult Treatment Panel III and International Diabetes Federation definitions. J Diabetes Investig 6 (2015): 280-288.
- American Diabetes Association. 10. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes–2021. Diabetes Care 44 (2021): S125-S150.
- Schofield JD, Liu Y, Rao-Balakrishna P, Malik RA, Soran H. Diabetes dyslipidemia. Diabetes Ther 7 (2016): 203-219.
- Islam FM, Chakrabarti R, Islam MT, Wahab MD, Lamoureux E, et al. Prediabetes, diagnosed and undiagnosed diabetes, their risk factors and association with knowledge of diabetes in rural Bangladesh: The Bangladesh Population-based Diabetes and Eye Study. J Diabetes 8 (2016): 260-268.
- Zaman MM, Chowdhury MAJ, Numan SM, et al. The Rural Dhaka Diabetes Study: Hospital-based survey of urban and rural Bangladesh. Diab Vasc Dis Res 17 (2020): 1479164120924097.
- World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310 (2013): 2191-2194.
- Daniel WW, Cross CL. Biostatistics: A Foundation for Analysis in the Health Sciences. 10th ed. New York: John Wiley & Sons; 2018.
- American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes–2021. Diabetes Care 44 (2021): S15-S33.
- World Health Organization. WHO STEPwise approach to surveillance (STEPS). Geneva: World Health Organization; 2017.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J Am Coll Cardiol 71 (2018): e127–e248.
- Rifai N, Warnick GR, Dominiczak MH. Handbook of Lipoprotein Testing. 2nd Washington, DC: AACC Press. 2000.
- Levey AS, Stevens LA, Schmid CH, Zhang Y, Castro AF, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 150 (2009): 604-612.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 285 (2001): 2486-2497.
- Grundy SM, Stone NJ, Bailey AL, Beam C, Kim K. Birtcher, et al. AHA/ ACC/ AACVPR/ AAPA/ ABC/ ACPM/ ADA/ AGS/ APhA/ ASPC/ NLA/ PCNA Guideline on the Management of Blood Cholesterol. J Am Coll Cardiol 73 (2018): e285–e350.
- IBM Corp. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. 2017.
- Islam MS, Alam MT, Islam MR, et al. Prevalence of dyslipidemia and associated factors among the type 2 diabetic patients in a tertiary care hospital of Bangladesh. BMC Res Notes 15 (2022): 131.
- Rahman MM, Gilmour S, Saito E, Sultana P, Shibuya K. Health-related financial catastrophe, inequality and chronic illness in Bangladesh. PLoS One 8 (2013): e56873.
- Lakshminarayanan S, Kalathil AC, Radhakrishnan S, Sivaprakasam K. Prevalence and pattern of dyslipidemia among type 2 diabetes mellitus patients in a rural tertiary care centre in South India. Indian J Community Med 46 (2021): 494-497.
- Aryal M, Poudel A, Satyal B, et al. Prevalence and associated risk factors of dyslipidemia among patients with type 2 diabetes mellitus in Kathmandu, Nepal. Sci Rep 12 (2022): 1825.
- Jacobs MJ, Kleisli T, Pio JR, et al. Prevalence and control of dyslipidemia among persons with diabetes in the United States. Diabetes Res Clin Pract 70 (2005): 263-269.
- Taskinen MR, Packard CJ, Borén J. Dietary fructose and the metabolic syndrome. Nutrients 11 (2019): 1987.
- Verges B. Pathophysiology of diabetic dyslipidaemia: where are we? Diabetologia 58 (2015): 886-899.
- Wu L, Parhofer KG. Diabetic dyslipidemia. Metabolism 63 (2014): 1469-1479.
- Bhowmik B, Siddiquee T, Mujumder A, et al. Serum lipid profile and its association with diabetes and prediabetes in a rural Bangladeshi population. Int J Environ Res Public Health 15 (2018): 1944.
- Arca M, Pigna G, Favoccia C. Mechanisms of diabetic dyslipidemia: relevance for atherogenesis. Curr Vasc Pharmacol 10 (2012): 684-686.
- ACCORD Study Group. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med 362 (2010): 1563-1574.
- Bhowmik B, Munir SB, Diep LM, Siddiquee T, Habib SH, et al. Anthropometric indicators of obesity for identifying cardiometabolic risk factors in a rural Bangladeshi population. J Diabetes Investig 4 (2013): 361-368.
- Anagnostis P, Stevenson JC, Crook D, Johnston DG, Godsland IF. Effects of menopause, gender and age on lipids and high-density lipoprotein cholesterol subfractions. Maturitas 81 (2015): 62-68.
- Godsland IF. Effects of postmenopausal hormone replacement therapy on lipid, lipoprotein, and apolipoprotein (a) concentrations: analysis of studies published from 1974–2000. Fertil Steril 75 (2001): 898-915.
- Zhang H, Zhang T, Li S, et al. Long-term impact of diabetes on cardiovascular diseases. Ther Adv Endocrinol Metab 12 (2021): 2042018821997356.
- Akter S, Rahman MM, Abe SK, Sultana P. Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: a nationwide survey. Bull World Health Organ 92 (2014): 204-213A.
- Félix-Redondo FJ, Grau M, Fernández-Bergés D. Cholesterol and cardiovascular disease in the elderly. Facts and gaps. Aging Dis 4 (2013): 154-169.
- Santos-Gallego CG, Rosenson RS. Role of HDL in those with diabetes. Curr Cardiol Rep 16 (2014): 512.
- Verges B. Lipid disorders in type 1 diabetes. Diabetes Metab 35 (2009): 353-360.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352 (1998): 837-853.
- Verges B. Pathophysiology of diabetic dyslipidaemia: where are we? Diabetologia 58 (2015): 886-899.
- Taskinen MR. Diabetic dyslipidaemia: from basic research to clinical practice. Diabetologia 46 (2003): 733-747.
- Mohan V, Deepa R, Velmurugan K, Premalatha G, et al. Association of C-reactive protein with body fat, diabetes and coronary artery disease in Asian Indians: the Chennai Urban Rural Epidemiology Study (CURES-6). Diabet Med 22 (2005): 863-870.
- Rocha VZ, Libby P. Obesity, inflammation, and atherosclerosis. Nat Rev Cardiol 6 (2009): 399-409.
- Bays HE, Toth PP, Kris-Etherton PM, Nicola Abate, Louis J Aronne, et al. Obesity, adiposity, and dyslipidemia: a consensus statement from the National Lipid Association. J Clin Lipidol 7 (2013): 304-383.
- American Diabetes Association. 10. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes–2021. Diabetes Care 44 (2021): S125-S150.
- Uddin MJ, Alam N, Sarma H, Muhammad Ashique Haider Chowdhury, Dewan S Alam, et al. Consequences of hypertension and chronic obstructive pulmonary disease, healthcare-seeking behaviors of patients, and responses of the health system: a population-based cross-sectional study in Bangladesh. BMC Public Health 14 (2014): 547.
- Handelsman Y, Jellinger PS, Guerin CK, Zachary T Bloomgarden, Eliot A Brinton, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the management of dyslipidemia and prevention of cardiovascular disease algorithm – 2020 executive summary. Endocr Pract 26 (2020): 1196-1224.
- Elam MB, Ginsberg HN, Lovato LC, Marshall Corson, Joseph Largay, et al. Association of fenofibrate therapy with long-term cardiovascular risk in statin-treated patients with type 2 diabetes. JAMA Cardiol 2 (2017): 370-380.
- Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358 (2008): 580-591.
- Rahman MS, Akter S, Abe SK, Md Rafiqul Islam, Md Nazrul Islam Mondal, et al. Awareness, treatment, and control of diabetes in Bangladesh: a nationwide population-based study. PLoS One 10 (2015): e0118365.
- Hossain S, Talukder MH, Biswas A, et al. Dietary patterns and their association with socio-demographic characteristics and dietary beliefs of Bangladeshi adults. Heliyon 7 (2021): e07004.
- Rahman MM, Gilmour S, Saito E, Sultana P, Shibuya K. Self-reported illness and household strategies for coping with health-care payments in Bangladesh. Bull World Health Organ 91 (2013): 449-458.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 