Retrospective Comparative Study of the Short and Long Term Outcomes of Percutaneous Coronary Intervention and Coronary Artery Bypass Graft in Chronic Kidney Disease Population
Nishanthi WAAGN1*, Herath Chula1, Manjika Sithum3
1Dialysis and transplant center, Sri Jayawardenapura General Hospital, Srilanka
3Department of Community Medicine, University of Sri Jayawardenapura, Srilanka
*Corresponding author: Nishanthi WAAGN, Dialysis and transplant center, Sri Jayawardenapura General Hospital, Srilanka.
Received: 12 April 2022; Accepted: 18 April 2022; Published: 27 April 2022
Article Information
Citation: Nishanthi WAAGN, Herath Chula, Manjika Sithum. Retrospective Comparative Study of the Short and Long Term Outcomes of Percutaneous Coronary Intervention and Coronary Artery Bypass Graft in Chronic Kidney Disease Population. Cardiology and Cardiovascular Medicine 6 (2022): 217-228.
View / Download Pdf Share at FacebookAbstract
Introduction: Patients with chronic kidney disease are at increased risk of cardiovascular disease and death. For patients with Chronic Kidney Disease (CKD) and multivessel Coronary Artery Disease (CAD), the optimal revascularization study is still debatable. This is a single center retrospective study to compare the short- and long-term outcomes of Percutaneous Coronary Intervention (PCI) and Coronary Artery Bypass Graft (CABG) in CKD patients who presented with acute coronary syndrome. in Sri Lanka.
Objectives: This study was aimed to describe the sociodemographic distribution of the population with CKD and acute coronary syndrome, to compare the baseline characteristics with outcomes include recurrence of ACS and LV(left ventricular dysfunction) and to compare the short and long term outcomes of PCI and CABG in CKD population.
Methodology: A retrospective comparative study was conducted at Sri Jayewardenepura General Hospital on patients with CKD who underwent CABG and PCI since 2013 to 2017. Data were obtained from past medical records, clinic records and telephone interviews. The outcomes of the patients with CKD who underwent PCI were matched to patients who underwent CABG for multivessel disease by using univariate and multivariate statistical analysis methods. The outcomes include deaths, recurrence of acute coronary syndrome, left ventricular LV dysfunction, bleeding complications and stroke.
Results: There were 423 patients met inclusion criteria with mean age 59.94 ± 8.381 years. There were 81.3%(n=344) of males. The prevalence of Diabetes, hypertension, dyslipidemia in the study sample was 89.2%(n=363),83.3%(n=339), and 34.9%(n=142) respectively. The prevalence of CKD stage I, II ,111,1V and V was 1.4%(n=6) ,38% (n=165), 36.9% (n=156),12.5% (
Keywords
<p>Cardiovascular disease; Coronary syndrome; Chronic Kidney Disease; Retrospective; population</p>
Article Details
Abbreviations:
CKD: Chronic kidney disease; ESC: European Society Cardiology; ACS: Acute Coronary Syndrome; CABG: Coronary artery bypass graft; CAD: Coronary artery disease; PCI: Percutaneous coronary intervention; GFR: Glomerular filtration rate
1. Introduction
Cardiovascular disease is the leading cause of mortality and morbidity in patients with Chronic Kidney Disease (CKD). Atherosclerosis, vascular calcification, and resulting in coronary artery disease more common in patients with CKD. In all patients with coronary artery disease, deciding when and what type of coronary artery revascularization to be performed is needed, in addition to medical management is often important and difficult decision. However there is a treatment risk contradictory, in that these high risk patients have lower rates of medical therapy, referral for cardiac stress testing, cardiac revascularization when compared to lower risk patients [1]. According to European Society Cardiology (ESC )guidelines for Acute Coronary Syndrome (ACS), multivessel disease opted for either PCI or CABG. The revascularization strategy should be based on the clinical status as well as the severity and distribution of the Coronary Artery Disease (CAD) and the lesion characteristics [2]. A prior study using the Duke Databank compared CABG and PCI in year 1995-2000;this study found a mortality benefit of CABG over PCI patients with moderate and severe CKD. The majority of patients, both CABG and PCI are suitable, thus the care team and patient must decide which is better in order to achieve the preferred patient centred goals of care [3]. There were few retrospective studies done to compare PCI vs CABG in CKD population. In a population of patients with multivessel coronary artery disease, CABG associated with lower risk of death when compared with medical management for those with mild, moderate and severe CKD. There was a trend towards lower mortality with CABG compared with PCI ,either with (bare metal stent or drug eluding stent) BMS or DES, among patients with mild, moderate ,and severe CKD ,but majority of these associations didn’t reach any statistical significance [1].CABG is associated with higher rate of stroke and periprocedural death, whereas PCI is associated with the higher rates of repeat revascularization and possible recurrent Myocardial infarction. However, the same rules apply for CKD population is debatable. The biology of heart disease is altered in CKD, consequence of the complex interplay between arteriosclerosis, atherosclerosis and uremic cardiomyopathy [4].
2. General Objective
To identify the better treatment modality for coronary intervention in CKD population.
3. Specific Objective
To describe the demographic distribution of the population with CKD and acute coronary syndrome.
To compare the baseline characteristics of patients with outcomes.
To compare the outcomes of PCI and CABG in patients with CKD (GFR<60ml/mt),
4. Methodology
The study was a single center retrospective comparative study conducted in Sri Jayewardenepura General Hospital from 1st of January 2013 to 31st of December 2017 among patients with CKD and acute coronary syndrome underwent PCI and CABG.
4.1. Inclusion criteria
- Patients with CKD with an estimated GFR less than 60 ml/mt and patient with estimated GFR 60 to 90 ml/mt with proteinuria (calculated using the MDRD study equation)
- Patients with multivessel disease defined as severe stenosis (>70%) in at least 2 major coronary arteries
- Patients underwent PCI with drug eluding or bare metal stents and patients who underwent isolated CABG
4.2. Exclusion Criteria
- Patients who underwent prior cardiac surgery or prior PCI
- Patients who underwent renal transplantation.
- Patients who were lost to follow up regularly in the clinic visits.
- Patients with significant life limiting co-morbidities like advanced metastatic cancer.
- Patients who underwent balloon angioplasty
- Patients who received isolated medical treatment
- Patients who response to telephone calls
4.3. Sample size calculation
The sample size will be 423 according to following formula
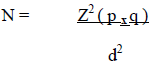
N= Sample size
P= Rough estimate for proportion of occurrence of event being measured 50%.
Z= Significant level at 95% confidence limit 1.96
q = (1-p)
d = The degree of accuracy (precision) desired for margin of error set at 0.05 (5%)
Considering nonresponse rate of 10%
Total sample size of the study is 423.
The sample size of this study was based on the number of CKD patients admitted to Sri Jayewardenepura General Hospital who underwent CABG and PCI since 1st of January 2013 to 31st of December 2017. 423 Patients were recurred to the study based on convention sampling method. Data of all selected patients with CKD who underwent CABG and PCI during study period at Sri Jayewardenepura General Hospital were taken to the study.
4.4. Ethical clearance
Ethical clearance was obtained from Ethical Review Committee, Sri Jayewardenepura General Hospital. Participation in this study was voluntary and confidentiality was ensured. This study did not cause any known harm to participants. Benefits were informed to participant through information sheet. Anonymity was ensured. Identity and information of the participant collected separately and kept confidentially. Any personal information of participant was not disclosed in any reports that we may publish in journals. However, participant was given the opportunity to review and approve any material that is published. Data was stored with restricted access only to the principal investigator. The computerized data was password protected and only available to the investigator. Any participants had the rights to refuse to take part in the study at any time without affecting the relationship with the investigators of this study. Also, they had the right not to answer any single question, as well as to withdraw completely from the interview at any point during the process; additionally, participants had the right to request that the interviewer not use any of interview material. participants had the right to ask questions about this research study during or after the research.
4.5. Data collection
Data was collected from all the patient’s past medical and clinic records and telephone interviews by principal investigator in a data extraction sheet.
4.6. Data analysis
Categorical variables include gender, smoking, history of diabetes mellitus, history of hypertension, history of dyslipidemia and family hx of ischemic heart disease. Categorical variables were described as frequencies and percentages. Continuous variables were described using frequency distributions. CKD was divided into 5 stages (I-V). In our study CKD again classified into mild (stage I and 11), moderate (stage 111 and IV), severe (stage V). The interactions in between categorical variables were estimated using the chi-square test and fisher’s exact test. Patients with CKD who underwent PCI, the outcomes were matched to patients who underwent isolated CABG for multivessel disease by using univariate and multivariate statistical analysis methods. The outcomes including deaths, recurrence of ACS, bleeding, left ventricular dysfunction (defined as systolic ejection fraction less than 50%) and end up in hemodialysis were compared with the PCI and CABG in CKD population using chi-square test and fishers exact test. The P value<0.05 was taken as statistically significant. Data was analyzed using Statistical Package for Social Sciences (SPSS- version 22).
5. Results
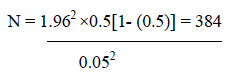
There were 423 patients met inclusion criteria with mean age 59.94 ± 8.381 years. There were 81.3% (n=344) of males. The prevalence of Diabetes, hypertension, dyslipidemia in the study sample was 89.2% (n=363),83.3% (n=339), and 34.9% (n=142) respectively. The prevalence of CKD stage I, II ,111,1V and V was 1.4%(n=6), 38%(n=165), 36.9% (n=156), 12.5%(n=54), 11.3%(n=48) respectively (Table 1). The recurrence of ACS in PCI group was 14.3% (n=34),23.6% (n=56),12.7% (n=30) compared to CABG group 7.5%(n=14),7%(n=13),0% in 1 month , 1 year and 3 years ( X2=4.817,p<0.05, X2=21.136,P<0.01,P<0.05 ). There was a statistically significant reduction in recurrences of ACS in CABG group compared to PCI group in CKD population. The incidence of LV dysfunction in the PCI group was 24%(n=18) 50.7% (n=38),29.3% (n=22) compared to CABG group 80%(n=12),20%(n=3),0% in 1 month,1 year and 3 years.(p<0.05 using fishers exact test)There was a significant reduced occurrence of LV dysfunction in CABG group compared to PCI group in 1 year and 3 years. The recurrence of ACS in PCI group was 14.3%(n=34),23.6%(n=56),12.7%(n=30) compared to CABG group 7.5%(n=14),7%(n=13),0% in 1 month , 1 year and 3 years ( X2=4.817,p<0.05, X2=21.136,P<0.01,P<0.05 ). There was a statistically significant reduction in recurrences of ACS in CABG group compared to PCI group in CKD population. The incidence of LV dysfunction in the PCI group was 24%(n=18)50.7% (n=38),29.3%(n=22) compared to CABG group 80%(n=12),20%(n=3),0% in 1 month,1 year and 3 years (p<0.05 using fishers exact test). There was a significant reduced occurrence of LV dysfunction in CABG group compared to PCI group in 1 year and 3 years .Survival in PCI group was 99.6%(n=236),95.8%(n=227),90.7%(n=215) compared to survival in CABG group 96.2%(n=179)95.7%(n=178)94.6%(n=176) in 1 month,1 year and 3 years. (X2=0.002, P>0.05, X2=2.274, P>0.05). Even though CABG group had overall better outcomes there is no significant survival benefit in our study, might be due to lower number of stage 5 and dialysis population. The hemodialysis dependence after PCI was 6.3%(n=15) and CABG was 8.1%(n=8.1) (X2=0.476, P>0.05). There is no significant difference between PCI vs CABG in hemodialysis dependence after the procedure. Bleeding complication in PCI group was 10.1%(n=24) compared to CABG group was 0(P<0.05 using Fishers exact test), so there were significant bleeding complications in PCI group compared to CABG group (Table 2).
|
Características. |
n |
% |
|
Age (years) |
||
|
<50 years |
42 |
9.9 |
|
51 - 55 |
60 |
14.2 |
|
56 – 60 |
114 |
27 |
|
61 – 65 |
111 |
26.2 |
|
66 – 70 |
66 |
15.6 |
|
> 70 |
30 |
8.1 |
|
Gender |
||
|
Male |
344 |
81.3 |
|
Female |
79 |
18.7 |
|
Smoking |
258 |
61 |
|
Family history of ischemic heart disease |
90 |
22.1 |
|
Diabetes |
363 |
89.2 |
|
Hypertension |
339 |
83.3 |
|
Dyslipidemia |
142 |
34.9 |
|
CKD Stage |
||
|
Stage I |
6 |
1.4 |
|
Stage II |
159 |
37.6 |
|
Stage III |
156 |
36.9 |
|
Stage IV |
54 |
12.8 |
|
Stage V |
48 |
11.3 |
|
Dialysis in Stage V |
19 |
4.4 |
Table 1: Demographics and baseline characteristics (n=423).
|
Outcome |
Treatment Mode |
Significant |
|||
|
PCI |
CABG |
||||
|
N |
% |
N |
% |
||
|
Survival |
|||||
|
1 month |
236 |
99.6 |
179 |
96.2 |
Fishers exact test p=0.024 (p<0.05) |
|
1 year |
227 |
95.8 |
178 |
95.7 |
X2 =0.002, df=1,p=0.967 (p>0.05) |
|
3 year |
215 |
90.7 |
176 |
94.6 |
X2 =2.274, df=1,p=0.132 (p>0.05) |
|
Recurrence of ACS |
|||||
|
1 Month |
34/237 |
14.3 |
14/186 |
7.5 |
X2=4.817, df=1,p=0.028 (p<0.05) |
|
1 Year |
56/237 |
23.6 |
13/186 |
7 |
X2=21.136,df=1,p=0.000 (p<0.01) |
|
3 Years |
30/237 |
12.7 |
0/186 |
0 |
Fishers exact test p=0.000 (p<0.05) |
|
End up in Dialysis |
15/237 |
6.3 |
15/186 |
8.1 |
X2=0.476, df=1,p=0.490 (p>0.05) |
|
LV Dysfunction |
|||||
|
1 Month |
18/75 |
24 |
15-Dec |
80 |
Fishers exact test p=0.000 (p<0.05) |
|
1 Year |
38/75 |
50.7 |
15-Mar |
20 |
Fishers exact test p=0.045 (p<0.05) |
|
3 Years |
22/75 |
29.3 |
0/75 |
0 |
Fishers exact test p=0.018 (p<0.05) |
|
Bleeding complication |
24/237 |
10.1 |
0/186 |
0 |
Fishers exact test p=0.000 (p<0.05) |
|
Strokes |
15/237 |
6.3 |
3/183 |
1.6 |
Fishers exact test p=0.000 (p<0.05) |
Table 2: Association between outcome and the treatment mode
|
Recurrence of ACS |
Significant |
||||
|
Yes |
% |
No |
% |
||
|
CKD |
|||||
|
Mild stage |
36 |
25 |
129 |
46.2 |
|
|
Moderate Stage |
84 |
58.3 |
126 |
45.2 |
X2=19.744,df=2,p=0.000 (p<0.01) |
|
Severe Stage |
24 |
16.7 |
24 |
8.6 |
|
|
Age group |
|||||
|
<60 years |
102 |
70.8 |
114 |
40.9 |
X2=34.147,df=1,p=0.000 (p<0.01) |
|
>60 years |
42 |
29.7 |
165 |
59.1 |
|
|
Hypertension (Past history) |
120/139 |
86.3 |
219/268 |
81.7 |
X2=1.401,df=1,p=0.237 (p>0.05) |
|
Dyslipidemia |
47/139 |
33.8 |
95/268 |
35.4 |
X2=0.108,df=1,p=0.743 (p>0.05) |
|
Diabetes |
126/139 |
90.6 |
237/268 |
88.4 |
X2=0.466,df=1,p=0.495 (p>0.05) |
Table 3: Comparison of baseline characteristics with outcome.
|
Characteristic |
LV Dysfunction |
Significant |
|||
|
Yes |
% |
No |
% |
||
|
CKD |
|||||
|
Mild stage |
18 |
20 |
147 |
44.1 |
|
|
Moderate Stage |
42 |
46.7 |
168 |
50.5 |
X2=59.492,df=2,p=0.000 (p<0.01) |
|
Severe Stage |
30 |
33.3 |
18 |
5.4 |
|
|
Age group |
|||||
|
<60 years |
60 |
66.7 |
156 |
46.8 |
X2=11.138,df=1,p=0.001 (p<0.05) |
|
>60 years |
30 |
33.3 |
177 |
53.2 |
|
|
past history of hypertension |
60/90 |
66.7 |
279/317 |
88 |
X2=22.952,df=1,p=0.000 (p<0.01) |
|
Dyslipidemia |
24/90 |
26.7 |
118/317 |
37.2 |
X2=3.439,df=1,p=0.064 (p>0.05) |
|
Diabetes |
84/90 |
93.3 |
279/317 |
88 |
X2=2.058,df=1,p=0.151 (p>0.05) |
Table 4: Comparison of baseline characteristics with LV function.
|
Baseline Characteristics |
Treatment Mode |
Significant |
|||
|
PCI |
CABG |
||||
|
N |
% |
N |
% |
||
|
Family history of IHD |
60/221 |
27.1 |
30/186 |
16.1 |
X2 =7.122, df=1, p=0.008 (p<0.05) |
|
Past history of Diabetes |
189/221 |
85.5 |
174/186 |
93.5 |
X2=6.751, df=1, p=0.009 (p<0.05) |
|
Past history of Hypertension |
174/221 |
78.7 |
165/186 |
88.7 |
X2=7.224, df=1, p=0.007 (p<0.05) |
|
Past history of Dyslipidemia |
59/221 |
26.7 |
83/186 |
44.6 |
X2=14.288, df=1, p=0.000 (p<0.01) |
Table 5: Comparison of treatment mode with outcomes.
6. Discussion
In our study we have collected data from the CKD patients who underwent CABG and PCI since 1st of January 2013 to 31ST of December 31, 2017. Data was collected from past medical records follow up was done with clinic records and telephone interviews. It was not possible to collect the data from the patients who lost to follow up. In our study population the patients with CKD and coronary artery disease were younger male group might be due to association with smoking, diabetes mellitus, dyslipidemia and hypertension. Despite the known associations among CAD, CKD and mortality risk the optimal method of treating CAD in patients with CKD had been a matter of option, rather than evidence, because of the paucity of randomized controlled studies of this population [5]. In a population with multivessel CAD, there was a trend towards lower mortality with CABG compared with PCI among mild, moderate , and severe CKD, but the associations did not reach statistically significant .However, in first month PCI group had better survival than CABG group and reached statistically significant irrespective of CKD stage. However, when compared the overall outcomes including recurrence of acute coronary syndrome, LV dysfunction and bleeding, the CABG group had better outcome than PCI group which was statistically significant in all stages of CKD. A prior study using the Duke Databank compared CABG and PCI in years 1995-2000;this study found a mortality benefit of CABG over PCI in patients with moderate and severe CKD [6]. Other retrospective studies found lower risk of deaths or recurrence of acute coronary syndrome with CABG compared with PCI ,but many studies included percutaneous coronary angioplasty [7]. While studies with longer term follow up found have more consistent benefits with CABG compared with PCI [5-7]. However, since patients with CKD have more complex and diffuse CAD, our study results in CABG had better long-term outcomes than PCI group. Most studies compared only recurrence of MI and deaths, however our study compared recurrence of acute coronary syndrome, LV dysfunction, bleeding risk and dialysis dependence after the procedure. Our study also showed significant association between baseline characteristics with outcomes which other studies didn’t compare. Depend on the CKD stage, hypertension, diabetes mellitus, there is a significant association with recurrence of acute coronary syndrome and LV dysfunction, which were not compared in other studies. Our study only had 19 dialysis patients: the small sample size limited the ability to discern any differences in outcomes among different treatment groups. Larger registry analysis have found a long-term mortality benefit associated with CABG compared with PCI in for multivessel disease in dialysis patients [7-9]. The number of patients with severe CKD only 102 patients, compared to the lower CKD group, which was 302 patients, which was possible explanation for a lack of significant difference in mortality comparing PCI vs CABG group and there is no significant association with CKD stage and treatment outcomes. Even post hoc analysis from a small group of patients with non-HD CKD from the Arterial Revascularization Therapy Study 11 trial did not show a statistically significant difference in the adjusted 5-year mortality rate for patients with CABG (15%) or PCI (12%) [10]. Our databank didn’t include the indication or urgency for procedure and didn’t mention the type of stenting and didn’t compare with the patients who underwent medical treatment only. As we have done the study in between 1st of January 2013 to 31st of December 2017, all the patients had drug eluding stents in that era.
Observational studies comparing CABG and drug eluding stents for treating multivessel CAD in the general populations have mostly found that CABG offers greater longer-term survival [11]. The important finding in our study that CABG was associated with more hemodialysis dependence (8.3%) than PCI (6.3%) this might be due to fluid shifts and sometimes using on pump procedure and due to hypotensive episodes. Also, improvement in periprocedural renal care for patients undergoing PCI, such as administration of IV fluids and acetylcysteine might have helped to decrease the rate of renal failure after PCI. The advantages of our study were both short- and longer-term outcomes were compared. There was a significant reduction in recurrence of acute coronary syndrome and LV dysfunction in CABG group compared to PCI group. Also, in our study, multiple outcomes were compared in between the treatment groups. We were able to identify statistically significant association with age group (56-60) and severity of CKD with recurrence of acute coronary syndrome. We were also able to identify statistically significant association with age group (56-60), severity of CKD and hypertension with LV dysfunction. Our study had some notable limitations. This was a non-randomized and used observational data from a single center. The number of patients with CKD stage 5 and dialysis only 48, which was limited number compared to CKD stage 2 and 4 population. This might be the reason that there was no significant survival benefit in CABG group than the PCI group(p-0.967 in 1 year,p-0.132 in 3 years P>0.05).The selection for the revascularization method was physician dependent and the data that affected the selection was also unavailable to us. We couldn’t compare the type of the stent and type of lesion as some data was unavailable as this was a retrospective study. The small number of patients, especially in the end stage renal disease group, limited our study’s statistical power.
6.1. Study limitations
- The analysis does not control for unmeasured confounders.
- They-up outcomes based on patient registries so that it is likely that the patients where records not available could have been missed.
- Since this was a retrospective study there were selection bias and unmeasured variables that were not captured in the propensity model.
- The patients who had isolated medical treatment were not compared
7. Conclusion and Recommendation
In conclusion, the population of CKD stage mainly in CKD stage 11 and 111.people with less than 60 years with CKD underwent coronary intervention than the older age group. There is a statistically significant association with moderate and severe CKD group with recurrence of ACS. There is also a statistically significant association with hypertension and moderate and severe CKD stage with LV dysfunction. Even though the CABG group had showed better longer-term survival (94.6%) compared to PCI group (90.7%) it was not statistically significant in our study. This might be due to the limited number of severe CKD category. However, there is a significant reduction in recurrence in acute coronary syndrome in CABG group compared to PCI group in 1 month,1 year and 3 years.(p<0.05).There is also a significant reduction in LV dysfunction and bleeding complication in CABG group compared to PCI group.(p<0.05)In our study there is no significant association with dialysis dependence and the procedure. However, CABG group had ended up in dialysis more than PCI group that was not statistically significant in our study.(p>0.05)There are several limitations in our study as it was a single center retrospective study, the limited number of population in our study may be the reason that some findings in our study was not statically significant. There were no enough studies done in Asian among CKD population with CAD. Therefore, further multicenter longer term follows up studies are needed to investigate the optimum treatment option for CKD population with acute coronary syndrome.
Acknowledgements
Let me take this opportunity to convey my heartfelt gratitude for all the people who supported me and guided me in completing my thesis for the MD training in Nephrology. First and foremost, I wish to thank Dr Chula Hearth, Consultant Nephrologist for having so kindly consented to supervise my study and I am ever grateful for his invaluable guidance in this endeavour. I also thank to all participant who accept my invitation to participate in the study. I thank all my lectures, teachers from primary to tertiary for their contribution in my long academic journey, especially those who made valuable comments to make this study a success.
References
- Szczech LA, Reddan DN, Owen WF, et al. Differential survival after coronary revascularization procedures among patients with renal insufficiency. Kidney Int (2020): 292-299.
- Beest V. Statin users risk heart attacks by dropping treatment or taking l ow doses Doctors must emphasise importance of compl ying with treatment say researchers. Heart. 91 (2006): 250-256.
- Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 381 (2013): 629-638.
- Subbiah AK, Chhabra YK, Mahajan S. Cardiovascular disease in patients with chronic kidney disease: A neglected subgroup. Heart Asia 8 (2016): 56-61.
- Papadopoulos K, Lekakis I, Nicolaides E. Outcomes of coronary artery bypass grafting versus percutaneous coronary intervention with second-generation drug-eluting stents for patients with multivessel and unprotected left main coronary artery disease. SAGE Open Med 5 (2017): 205031211668770.
- Roberts JK, Rao S V, Shaw LK, et al. Comparative Efficacy of Coronary Revascularization Procedures for Multivessel Coronary Artery Disease in Patients With Chronic Kidney Disease. In: American Journal of Cardiology (2017): 1344-1351.
- Herzog CA. How to manage the renal patient with coronary heart disease: The agony and the ecstasy of opinion-based medicine [Internet]. Vol. 14, Journal of the American Society of Nephrology. American Society of Nephrology (2003): 2556-2572.
- Reddan DN, Szczech LA, Tuttle RH, et al. Chronic kidney disease, mortality, and treatment strategies among patients with clinically significant coronary artery disease. J Am Soc Nephrol 14 (2003): 2373-2380.
- Chakrabarti AK, Grau-Sepulveda MV, O’Brien S, et al. Angiographic validation of the american college of cardiology foundation-the society of thoracic surgeons collaboration on the comparative effectiveness of revascularization strategies study. Circ Cardiovasc Interv 7 (2014): 11-8.
- Shiomi H, Morimoto T, Furukawa Y, et al. Comparison of percutaneous coronary intervention with coronary artery bypass grafting in unprotected left main coronary artery disease – 5-year outcome from CREDO-Kyoto PCI/CABG registry cohort-2-Circ J 79 (2015):1281-1289.
- Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation 106 (2002): 2207-2211.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 