Revisiting Landmark Trials: How DCB Therapy and Plant-Based Diets Transform Chronic Coronary Syndrome Care
Prof. Dasaad Mulijono1-3*
1Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia
2Indonesian College of Lifestyle Medicine, Indonesia
3Department of Cardiology, Faculty of Medicine, Prima University, Medan, Indonesia
*Corresponding author: Prof. Dasaad Mulijono, Department of Cardiology, Bethsaida Hospital, Tangerang, Indonesia, Email: mulijonodasaad@yahoo.com
Received: 01 April 2025; Accepted: 09 June 2025; Published: 10 June 2025
Article Information
Citation: Dasaad Mulijono. Revisiting Landmark Trials: How DCB Therapy and Plant-Based Diets Transform Chronic Coronary Syndrome Care. Cardiology and Cardiovascular Medicine 9 (2025): 192-197.
View / Download Pdf Share at FacebookAbstract
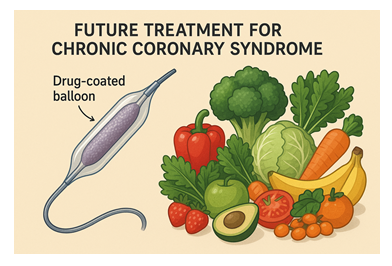
Landmark trials, from COURAGE to ISCHEMIA, have profoundly influenced clinical guidelines by emphasizing optimal medical therapy (OMT) as the primary management strategy for chronic coronary syndrome (CCS) due to limited incremental benefits demonstrated by invasive percutaneous coronary interventions (PCI) utilizing conventional stents. However, significant advancements in Drug-Coated Balloon (DCB) technology and Plant-Based Diet (PBD) strategies have demonstrated exceptional clinical outcomes, dramatically reshaping the therapeutic landscape. Clinical results, including exceedingly minor procedural complications, low rates of repeat revascularization, minimal restenosis (<2%), complete elimination of stent thrombosis, and markedly reduced bleeding risks associated with abbreviated or eliminated dual antiplatelet therapy (DAPT), are primarily attributed to meticulous lesion preparation protocols and diet-driven systemic improvements. This review comprehensively discusses these novel findings, exploring their implications for updating clinical guidelines. Real-world data from Bethsaida Hospital, chaired by Prof. Dasaad Mulijono, substantiates these outcomes, emphasizing the clinical superiority of integrating advanced DCB therapies and PBD, suggesting the need to revisit foundational conclusions drawn from previous landmark trials.
Keywords
Chronic coronary syndrome; Drug-Coated Balloon; ISCHEMIA trial; COURAGE trial; Optimal medical therapy; Restenosis; Stent thrombosis; Plant-based diets; Bethsaida Hospital; Prof. Dasaad Mulijono
Chronic coronary syndrome articles; Drug-Coated Balloon articles; ISCHEMIA trial articles; COURAGE trial articles; Optimal medical therapy articles; Restenosis articles; Stent thrombosis articles; Plant-based diets articles; Bethsaida Hospital articles; Prof. Dasaad Mulijono articles
Article Details
1. Introduction
The management of CCS has been profoundly influenced by landmark clinical trials such as COURAGE, BARI 2D, FAME 2, ORBITA, and ISCHEMIA. Collectively, these trials established OMT as the primary recommended strategy, due to limited incremental benefits observed with invasive PCI involving conventional stenting. These studies consistently highlighted minimal reductions in primary cardiovascular outcomes, including mortality and myocardial infarction (MI), reinforcing the appropriateness of a conservative, medication-centered approach to CCS management [1-3].
However, the clinical landscape has undergone transformative changes driven by significant technological and lifestyle advancements. DCB therapy has emerged as a superior interventional strategy, addressing several critical limitations inherent in conventional stent technologies, such as restenosis, stent thrombosis, and bleeding complications associated with prolonged DAPT [4-51]. Concurrently, evidence supporting the systemic benefits of PBD has grown robustly, highlighting their role in significantly improving cardiovascular health outcomes by reducing inflammation, enhancing endothelial function, and decreasing thrombogenic risks [52-56].
Real-world clinical data from Bethsaida Hospital, under the leadership of Prof. Dasaad Mulijono, demonstrate groundbreaking outcomes that challenge established clinical paradigms. Over five years of follow-up involving nearly two thousand patients, integrated DCB and PBD strategies have consistently yielded exceptionally low complication rates: procedural complications remain minimal, repeat revascularization rates are less than 3%, restenosis rates have dropped below 2%, and stent thrombosis has been eliminated. Additionally, significantly reduced or eliminated reliance on prolonged DAPT has markedly decreased bleeding risks.
These compelling clinical achievements suggest that the foundational assumptions of the landmark trials, conducted primarily using older stent technologies, may no longer reflect the potential of modern therapeutic interventions. This review critically examines the implications of advanced DCB techniques combined with evidence-based nutritional interventions, proposing a necessary reappraisal of current clinical guidelines for CCS management. Such reassessment, supported by ongoing and future randomized controlled trials, is crucial for optimizing patient outcomes and defining the next era in cardiovascular care.
2. Optimal Medical Therapy vs. Intervention: Insights from Landmark Trials
Several pivotal trials have fundamentally reshaped clinical guidelines in managing CCS. The Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE, 2007) trial first demonstrated that adding PCI with conventional stenting to OMT did not significantly reduce mortality, MI, or major cardiovascular events in CCS patients, thus reinforcing the appropriateness of initial conservative management [57].
Further, the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D, 2009) trial confirmed similar outcomes in diabetic patients, indicating no substantial benefit in mortality or cardiovascular events with routine revascularization compared to intensive OMT alone [58].
The Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME 2, 2012) trial demonstrated reduced urgent revascularization rates with FFR-guided PCI. Still, it failed to show significant reductions in mortality or MI rates, highlighting limited incremental benefits beyond symptom relief [59].
The Objective Randomized Blinded Investigation with optimal medical Therapy of Angioplasty in stable angina (ORBITA) in 2017, a placebo-controlled trial, provided rigorous evidence showing a minimal symptomatic advantage of PCI over placebo, critically challenging established symptom-relief perceptions [60].
Finally, in 2019 the International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA) trial further solidified these findings, demonstrating that initial invasive strategies offered no significant advantage over OMT alone in reducing cardiovascular death or MI, thus firmly cementing OMT's role as the foundational management strategy in CCS guidelines [61].
3. Limitations of Landmark Trials with Advancements in DCB and PBD
Despite their critical influence, landmark trials from COURAGE to ISCHEMIA were conducted using conventional stent technologies, which were inherently limited by high rates of restenosis (10-20%), stent thrombosis (1-3%), and prolonged antiplatelet therapy-associated bleeding complications. Recent advancements, notably DCB therapy integrated with comprehensive lesion preparation and PBD, dramatically mitigate these limitations.
Over a five-year follow-up on almost two thousand patients, clinical evidence from Bethsaida Hospital highlights remarkable outcomes: no mortality reported, minor procedural complications, repeat revascularization rates below 3%, restenosis below 2%, complete elimination of stent thrombosis incidents, and negligible bleeding complications due to significantly shortened or eliminated DAPT. These outcomes indicate that advanced DCB therapies eliminate historical limitations and substantially enhance clinical efficacy and patient safety [62-71].
4. Role of Plant-Based Diets
Integration of plant-based dietary interventions significantly contributes to enhanced clinical outcomes through systemic improvements. PBD reduces inflammation, improves endothelial function, and lowers thrombogenicity, critically supporting lesion stabilization and vascular health post-DCB treatment [52-56]. These synergistic effects substantially mitigate the risk factors historically responsible for adverse cardiovascular outcomes post-intervention, including restenosis and thrombosis.
4. Implications for Clinical Practice and Guidelines
Given these substantial advancements, the foundational assumptions of landmark trials, particularly regarding the comparative efficacy and safety of invasive versus conservative strategies, require significant reconsideration. With advanced DCB interventions achieving unprecedentedly low complication rates and vastly superior outcomes, invasive strategies now potentially surpass the benefits of OMT alone, especially in complex or higher-risk patient populations previously deemed optimally managed conservatively. Larger randomized clinical trials are needed to confirm this view.
5. Conclusion
The integration of DCB therapy and PBD strategies represents a transformative evolution in the management of CCS. Advanced DCB interventions have overcome significant limitations previously associated with conventional stent technologies, drastically reducing restenosis, eliminating stent thrombosis, and minimizing bleeding risks related to DAPT. Furthermore, the systemic benefits of PBD substantially enhance vascular health and mitigate inflammation, augmenting the long-term effectiveness of invasive treatments. Under Prof. Dasaad Mulijono's leadership, real-world outcomes from Bethsaida Hospital underscore this integrative approach's clinical superiority and practical feasibility. Consequently, established guidelines, informed mainly by earlier landmark trials employing older technologies, require critical reassessment. Future randomized clinical trials are essential to validate these promising findings further and refine clinical practice, ultimately improving patient care and outcomes in contemporary cardiology.
- Author Contributions:M.; Conceptualization, writing, review, and editing.
- Funding: This research received no external funding.
- Institutional Review Board Statement: Not applicable.
- Informed Consent Statement: Not applicable.
- Data Availability Statement: Data are contained within the article.
- Conflict of Interest: The authors declare no conflict of interest.
12. References
- Vrints C, Andreotti F, Koskinas KC, Rossello X, Adamo M, et al. ESC Scientific Document Group. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur Heart J 45 (2024): 3415-3537.
- Virani SS, Newby LK, Arnold SV, Bittner V, Brewer LC, et al. Peer Review Committee Members. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation148 (2023): e9-e119.
- 2023 Guidelines of the Taiwan Society of Cardiology on the Diagnosis and Management of Chronic Coronary Syndrome. Acta Cardiol Sin 39 (2023): 4-96.
- Verde N, Ciliberti G, Pittorino L, Ferrone M, Franzese M, et al. Contemporary Use of Drug-Coated Balloons for Coronary Angioplasty. J Clin Med (2024): 13(20)-6243.
- Jeger RV, Eccleshall S, Wan Ahmad WA, Ge J, Poerner TC, et al. International DCB Consensus Group. Drug-Coated Balloons for Coronary Artery Disease: Third Report of the International DCB Consensus Group. JACC Cardiovasc Inter 13 (2023): 1391-1402.
- Muramatsu T, Kozuma K, Tanabe K, Morino Y, Ako J, et al. Task Force of the Japanese Association of Cardiovascular Intervention, Therapeutics (CVIT). Clinical expert consensus document on drug-coated balloon for coronary artery disease from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc Interv Ther 38 (2023): 166-176.
- Korjian S, McCarthy KJ, Larnard EA, Cutlip DE, McEntegart MB, et al. Drug-Coated Balloons in the Management of Coronary Artery Disease. Circ Cardiovasc Interv 17 (2024): e013302.
- Lazar FL, Onea HL, Olinic DM, Cortese B. A 2024 scientific update on the clinical performance of drug-coated balloons. AsiaIntervention 10(2024): 15-25.
- Camaj A, Leone PP, Colombo A, Vinayak M, Stone GW, et al. Drug-Coated Balloons for the Treatment of Coronary Artery Disease: A Review. JAMA Cardiol 10 (2025): 189-198.
- Expert Writing Committee of the Chinese Expert Consensus on Clinical Applications of Drug-Coated Balloon (2nd Edition); Ge JB, Chen YD. Chinese expert consensus on the clinical application of drug-coated balloon (2nd Edition). J Geriatr Cardiol 21 (2024): 135-152.
- Wang L, Li X, Li T, Liu L, Wang H, et al. Novel application of drug-coated balloons in coronary heart disease: A narrative review. Front Cardiovasc Med (2023): 1055210-1055274.
- Kundu A, Moliterno DJ. Drug-Coated Balloons for In-Stent Restenosis-Finally Leaving Nothing Behind for US Patients. JAMA 331 (2024): 1011-1012.
- Giacoppo D, Alfonso F, Xu B, Claessen BEPM, Adriaenssens T, et al. Drug-Coated Balloon Angioplasty Versus Drug-Eluting Stent Implantation in Patients With Coronary Stent Restenosis. J Am Coll Cardiol 75 (2020): 2664-2678.
- Sabaté M. Drug-Coated Balloon for De Novo Lesions: Back to the Past or Back to the Future? JACC Cardiovasc Interv (2023): 1804-1806.
- Colombo A, Leone PP, Ploumen EH, von Birgelen C. Drug-coated balloons as a first choice for patients with de novo lesions: pros and cons. EuroIntervention 20 (2024): e120-e122.
- Jiang JL, Huang QJ, Chen MH. Efficacy and safety of drug-coated balloon for de novo lesions of large coronary arteries: Systematic review and meta-analysis of randomized controlled trials. Heliyon 10 (2024): e25264.
- Ma Z, Liu K, Hu Y, Hu X, Wang B, et al. Comparison Between Drug-Coated Balloon and Stents in Large De Novo Coronary Artery Disease: A Systematic Review and Meta-Analysis of RCT Data. Cardiovasc Drugs Ther (2024): s10557-024-07548-2.
- Zhang W, Zhang M, Tian J, Zhang M, Zhou Y, et al.. Drug-Coated Balloon-Only Strategy for De Novo Coronary Artery Disease: A Meta-analysis of Randomized Clinical Trials. Cardiovasc Ther (2023): 3121601.
- Wang D, Wang X, Yang T, Tian H, Su Y, et al.. Drug-Coated Balloons for De Novo Coronary Artery Lesions: A Meta-Analysis of Randomized Clinical Trials. Yonsei Med J 64 (2023): 593-603.
- Gobbi C, Giangiacomi F, Merinopoulos I, Gherbesi E, Faggiano A, et al. Drug coated balloon angioplasty for de novo coronary lesions in large vessels: a systematic review and meta-analysis. Sci Rep 15 (2025): 4921.
- Zilio F, Verdoia M, De Angelis MC, Zucchelli F, Borghesi M, et al. Drug Coated Balloon in the Treatment of De Novo Coronary Artery Disease: A Narrative Review. J Clin Med 12 (2023): 3662.
- Rosenberg M, Waliszewski M, Krackhardt F, Chin K, Wan Ahmad WA, et al. Drug Coated Balloon-Only Strategy in De Novo Lesions of Large Coronary Vessels. J Interv Cardiol (2019): 6548696.
- Sciahbasi A, Mazza TM, Pidone C, Samperi S, Cittadini E, et al. A New Frontier for Drug-Coated Balloons: Treatment of "De Novo" Stenosis in Large Vessel Coronary Artery Disease. J Clin Med 13 (2024): 1320.
- Cioffi GM, Madanchi M, Attinger-Toller A, Bossard M, Cuculi F. Pushing the Boundaries: Drug-Coated Balloons to Treat a Calcified and Thrombotic Lesion in Acute Coronary Syndrome. Am J Case Rep 23 (2022): e936950.
- Su H, Li M, Hao L, Wang H. Comparison of Drug-Coated Balloons and Drug-Eluting Stents in Primary Percutaneous Coronary Interventions for ST-Segment Elevated Myocardial Infarction: A Systemic Review and Meta-Analysis. Rev Cardiovasc Med 23 (2022): 203.
- Hu H, Shen L. Drug-coated balloons in the treatment of acute myocardial infarction (Review). Exp Ther Med 21 (2021): 464.
- Sanz-Sánchez J, Teira Calderón A, Neves D, Cortés Villar C, Lukic A, Rumiz González E, et al. Culprit-Lesion Drug-Coated-Balloon Percutaneous Coronary Intervention in Patients Presenting with ST-Elevation Myocardial Infarction (STEMI). J Clin Med 14 (2025): 869.
- Kondo Y, Ishikawa T, Shimura M, Yamada K, Ukaji T, et al. Cardiovascular Outcomes after Paclitaxel-Coated Balloon Angioplasty versus Drug-Eluting Stent Placement for Acute Coronary Syndrome: A Systematic Review and Meta-Analysis. J Clin Med 13 (2024): 1481.
- Uskela S, Eranti A, Kärkkäinen JM, Rissanen TT. Drug-coated balloon-only strategy for percutaneous coronary intervention of de novo left main coronary artery disease: the importance of proper lesion preparation. Front Med 17 (2023): 75-84.
- Her AY, Kim TH, Shin ES, Kim S, Kim B, et al. Drug-Coated Balloon-Based Treatment of Left Main True Bifurcation Lesion. Catheter Cardiovasc Interv (2025): 31416.
- Gunawardena TD, Corballis N, Merinopoulos I, Wickramarachchi U, Reinhold J, et al. Drug-Coated Balloon vs. Drug-Eluting Stents for De Novo Unprotected Left Main Stem Disease: The SPARTAN-LMS Study. J Cardiovasc Dev Dis 10 (2023): 84.
- Sanchez-Jimenez E, El-Mokdad R, Chaddad R, Cortese B. Drug-coated balloon for the management of coronary chronic total occlusions. Rev Cardiovasc Med 23 (2022): 42.
- Qin Q, Chen L, Ge L, Qian J, Ma J, et al. Long-term clinical outcomes of drug-coated balloon for the management of chronic total occlusions. Coron Artery Dis 34 (2023)-555-561.
- Shin ES, Her AY, Jang MH, Kim B, Kim S, et al. Impact of Drug-Coated Balloon-Based Revascularization in Patients with Chronic Total Occlusions. J Clin Med 13(2024)-3381.
- Allana SS, Brilakis ES. What is the role of drug-coated balloons in chronic total occlusion percutaneous coronary intervention? Catheter Cardiovasc Interv 101 (2023): 957-958.
- Lazar FL, Prvulovic D, Onea HL, Cortese B. The role of drug-coated balloons for coronary bifurcation management: results from the prospective EASTBOURNE-BIF study. Minerva Cardiol Angiol 72 (2024): 346-354.
- Gao X, Tian N, Kan J, Li P, Wang M, et al. Drug-Coated Balloon Angioplasty of the Side Branch During Provisional Stenting: The Multicenter Randomized DCB-BIF Trial. J Am Coll Cardiol 85(2025): 1-15.
- Dash D, Mody R, Ahmed N, Malan SR, Mody B. Drug-coated balloon in the treatment of coronary bifurcation lesions: A hope or hype? Indian Heart J 74 (2022): 450-457.
- Mitsui K, Lee T, Miyazaki R, Hara N, Nagamine S, et al. Drug-coated balloon strategy following orbital atherectomy for calcified coronary artery compared with drug-eluting stent: One-year outcomes and optical coherence tomography assessment. Catheter Cardiovasc Interv 102 (2023): 11-17.
- Shan Y, Lu W, Han Z, Pan S, Li X, et al. Long-term outcomes of drug-coated balloon treatment of calcified coronary artery lesions: a multicenter, retrospective, propensity matching study. Front Cardiovasc Med 10 (2023): 1122290.
- Basavarajaiah S, Loku Waduge BH, Watkin R, Athukorala S. Is a high calcific burden an indication, or a contraindication for Drug Coated Balloon? Rev Cardiovasc Med 22 (2021): 1087-1093.
- Rivero-Santana B, Jurado-Roman A, Galeote G, Jimenez-Valero S, Gonzalvez A, et al. Drug-Eluting Balloons in Calcified Coronary Lesions: A Meta-Analysis of Clinical and Angiographic Outcomes. J Clin Med 13 (2024): 2779.
- Yang X, Lu W, Pan L, Han Z, Pan S, et al. Long-term outcomes of drug-coated balloons in patients with diffuse coronary lesions. Front Cardiovasc Med (2022): 9-935263.
- Xu H, Qiao S, Cui J, Yuan J, Yang W,et al. Drug-eluting stent and drug-coated balloon for the treatment of de novo diffuse coronary artery disease lesions: A retrospective case series study. Clin Cardiol 46(2023): 1511-1518.
- Gonzalo N, Shabbir A. The longest way round is the shortest way home: drug-coated balloons for long lesions in large coronary arteries. EuroIntervention 19 (2023): e882-e883.
- Scheller B, Rissanen TT, Farah A, Ohlow MA, Mangner N, et al. BASKET-SMALL 2 Investigators. Drug-Coated Balloon for Small Coronary Artery Disease in Patients With and Without High-Bleeding Risk in the BASKET-SMALL 2 Trial. Circ Cardiovasc Interv 15 (2022): e011569.
- Räsänen A, Kärkkäinen JM, Eranti A, Eränen J, Rissanen TT. Percutaneous coronary intervention with drug-coated balloon-only strategy combined with single antiplatelet treatment in patients at high bleeding risk: Single center experience of a novel concept. Catheter Cardiovasc Interv 101 (2023): 569-578.
- Lim GB. Drug-coated balloons for high-bleeding-risk PCI. Nat Rev Cardiol 16(2019): 516.
- van Veelen A, Küçük IT, Fuentes FH, Kahsay Y, Garcia-Garcia HM, et al. First-in-Human Drug-Eluting Balloon Treatment of Vulnerable Lipid-Rich Plaques: Rationale and Design of the DEBuT-LRP Study. J Clin Med 12 (2023): 5807.
- Zhang YB, Liu HD, Xing JH, Chen BW, Zhao YY, et al. Safety and Efficacy of Drug-Coated Balloons in Patients with Acute Coronary Syndromes and Vulnerable Plaque. Clin Appl Thromb Hemost (2022): 28:10760296221130063.
- van Veelen A, Küçük IT, Garcia-Garcia HM, Fuentes FH, Kahsay Y, et al. Paclitaxel-coated balloons for vulnerable lipid-rich plaques. EuroIntervention 20 (2024): e826-e830.
- Tuso P, Stoll SR, Li WW. A plant-based diet, atherogenesis, and coronary artery disease prevention. Perm J 19 (2015): 62-67.
- Peña-Jorquera H, Cid-Jofré V, Landaeta-Díaz L, Petermann-Rocha F, Martorell M, et al. Plant-Based Nutrition: Exploring Health Benefits for Atherosclerosis, Chronic Diseases, and Metabolic Syndrome-A Comprehensive Review. Nutrients 15 (2023): 3244.
- Mehta P, Tawfeeq S, Padte S, Sunasra R, Desai H, et al. Plant-based diet and its effect on coronary artery disease: A narrative review. World J Clin Cases 11 (2023): 4752-4762.
- Salehin S, Rasmussen P, Mai S, Mushtaq M, Agarwal M, et al. Plant Based Diet and Its Effect on Cardiovascular Disease. Int J Environ Res Public Health 20 (2023): 3337.
- Koutentakis M, Surma S, Rogula S, Filipiak KJ, Gasecka A. The Effect of a Vegan Diet on the Cardiovascular System. J Cardiovasc Dev Dis 10 (2023): 94.
- Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, et al. COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 356 (2007): 1503-1516.
- BARI 2D Study Group; Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 360 (2009): 2503-2515.
- De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, et al. FAME 2 Trial Investigators. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 367 (2012): 991-1001.
- Al-Lamee R, Thompson D, Dehbi HM, Sen S, Tang K, et al. ORBITA investigators. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet 391 (2018): 31-40.
- Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O'Brien SM, et al. ISCHEMIA Research Group. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med 382 (2020): 1395-1407.
- Mulijono D, Hutapea AM, Lister INE, Sudaryo MK, Umniyati H. Mechanisms of Plant-Based Diets Reverse Atherosclerosis. Cardiology and Cardiovascular Medicine 8 (2024): 290-302.
- Mulijono D. Plant-Based Diet in Regressing/Stabilizing Vulnerable Plaques to Achieve Complete Revascularization. Archives of Clinical and Biomedical Research 8 (2024): 236-244.
- Mulijono D, Hutapea AM, Lister INE, Sudaryo MK, Umniyati H. How a Plant-Based Diet (PBD) Reduces In-Stent Restenosis (ISR) and Stent Thrombosis (ST). Cardio Open 9 (1): 01-15.
- Mulijono D, Hutapea AM, Lister INE, Sudaryo MK, Umniyati H. Plant-Based Diet to Reverse/ Regress Vulnerable Plaque: A Case Report and Review. Archives of Clinical and Medical Case Reports 8 (2024): 126-135.
- Mulijono D. Reclaiming Healing Through Nutrition: Resistance to Plant-Based Diets and the Biblical Call to Restoration. Arch Epidemiol Pub Health Res 4 (2025): 01-03.
- Mulijono D. Bethsaida Hospital: Pioneering Plant-Based Diet and Lifestyle Medicine Revolution in Indonesia. Arch Epidemiol Pub Health Res 4 (2025): 01-03.
- Mulijono D. Prof. Dasaad Mulijono: The Plant-Based Guru Redefining Cardiology and Preventive Medicine. On J Cardio Res & Rep 8 (1): 2025.
- Mulijono D. Healing with Food or Managing with Injection? A New Era in Chronic Disease Care. J Biomed Res Environ Sci 6 (2025): 373-377.
- Mulijono D. How a Plant-Based Diet and Ultra-Low LDL Levels Can Reverse Atherosclerosis and Prevent Restenosis: A Breakthrough in Heart Health. J Biomed Res Environ Sci 6 (2025): 368-372.
- Mulijono D. What Was Meant for Harm. A Testimony of Healing, Faith, and Medical Revolution. Arch Epidemiol Pub Health Res 4(2025): 01-05.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 