Single versus Dual-Chamber Pacing in a Sub-Saharan African Heart Center: Characteristics and Prognosis
Anicet Kassi Adoubi1*, Florent Diby2, Pinnin Ouattara2, Ambroise Gnaba2, Flavien Kendja3
1Abidjan Heart Center, Université Alassane Ouattara, Bouaké, Côte d'Ivoire
2Université Alassane Ouattara, Bouaké, Côte d'Ivoire
3Abidjan Heart Center, Université Félix Houphouet Boigny, Abidjan, Côte d'ivoire
*Corresponding author: Anicet Kassi Adoubi, Abidjan Heart Center, Université Alassane Ouattara, Abidjan, Bouaké, Côte d'Ivoire
Received: 20 December 2020; Accepted: 04 January 2021; Published: 20 January 2021
Article Information
Citation: Anicet Kassi Adoubi, Florent Diby, Pinnin Ouattara, Ambroise Gnaba, Flavien Kendja. Single versus Dual-Chamber Pacing in a Sub-Saharan African Heart Center: Characteristics and Prognosis. Cardiology and Cardiovascular Medicine 5 (2021): 73-85.
View / Download Pdf Share at FacebookAbstract
Context: The pacemaker since the 2000s has seen technical improvements. In Sub-Saharan Africa, we often implant single-ventricular chamber pacemakers because of patients' limited financial resources.
Objective: This work sought to compare our patients' characteristics and prognosis with single-chamber ventricular pacing with those with dual-chamber pacing.
Methods: We conducted a retrospective study of patients implanted with pacemakers between 2006 and 2016 at Abidjan Heart Center in Ivory Coast. We compared demographic, clinical, and follow-up data of patients with single versus dual-chamber pacemakers. The endpoint was all-causes of death.
Results: Of the 283 patients (67.3 ± 12.6 years; 49.1% of males) selected for the study, 189 (66,8%) had a single chamber pacemaker. Patients with this type of pacemaker were older, with more often syncopes and atrial fibrillation before implantation. Sex and underlying disease were comparable in the two groups. During follow-up, early and late complications were not statistically different. At the end of the follow-up period (median:3.67 years, IQ [2.07; 6.10], 73 patients (25.8%) were dead. In univariate Cox model analysis, a single-chamber pacemaker was associated with risk of death (RR =1.974; 95% CI [1.132,3.44], p = 0.017), as well as age, heart failure, atrial fibrillation and, left ventricular ejection fraction <0.40. In multivariate analysis, only age was a factor of poor prognosis.
Conclusion: Our patients with single-chamber pacing had a more severe prognosis than patients with dual-chamber pacing. But this higher mortality was linked to older age and a more significant presence of atrial fibrillation in this group.
Keywords
<p>Pacemaker; Single-ventricular pacing; Dual-chamber pacing; Prognosis; Sub-Saharan Africa; Age; Atrioventricular block; Atrial fibrillation</p>
Article Details
1. Introduction
In sub-Saharan Africa, pacemaker therapy is still in the embryonic stage [1, 2]. A Pan-African Society of Cardiology (PASCAR) survey about 31 African countries reported that 30% of African countries had limited access to pacemaker insertion [3]. Eight of the 31 countries surveyed (26%) did not have access to pacemaker implantation. So, this practice is limited by insufficient technical, human resources, and patients' incomes. Thus, the dual-chamber pacemaker may appear to be significantly much more expensive than the single-chamber pacemaker. So in practice, we often suggest that patients choose the pacing mode according to their financial capabilities. Randomized studies from the early 2000s had compared dual-chamber (atrioventricular) and single chamber (ventricular) pacing mode [4-6]. Although the dual-chamber pacing had appeared to be more beneficial in terms of quality of life, this mode had not demonstrated superiority in morbidity and mortality. Current guidelines do not exclude the choice of single-ventricular pacing, particularly in cases of atrioventricular block [7, 8]. But several experts have found these results questionable [9, 10]. In practice, the use of single-ventricular pacemakers in developed countries has significantly decreased in favor of dual-chamber pacemakers [11, 12]. Besides, numerous cardiac pacing concepts and pacemaker technology have evolved [13, 14]. In this context, this work sought to compare our patients' characteristics and prognosis with single-chamber ventricular pacing with those with dual-chamber pacing.
2. Patients and Methods
2.1 Selection
We conducted a non-randomized retrospective cohort study of patients implanted with pacemakers between 2006 and 2016 at Abidjan Heart Center in Ivory Coast. Patients included in our study had a typical indication for cardiac pacing (bradycardia). For this reason, we inserted a single or a dual-chamber pacemaker according to the underlying disease and financial capabilities of patients. We excluded for this study all patients who received an implantable cardiac defibrillator, a pacemaker for cardiac resynchronisation therapy, had the right ventricular lead positioned outside the apex, or have had a cardiac surgery three months before or in the years following the pacemaker's implantation.
2.2 Analyzed parameters
At the time of the first pacemaker implantation, we systematically recorded
- demographic data (sex and age at pacemaker implantation),
- patient history ( hypertension, diabetes),
- functional and clinical signs (syncope, pre-syncope, palpitations, dizziness, asthenia, confusion, NYHA stage),
- echocardiographic findings (structural heart disease or not, left ventricular ejection fraction),
- indications for cardiac pacing (atrioventricular block, sick sinus syndrome, atrial fibrillation),
- type of pacemaker implanted,
- and the medications at discharge (use of ACE inhibitors, Angiotensin 2 receptors blockers, diuretics, beta-blockers, nitrates, calcium channel blockers, digoxin, amiodarone, vitamin K antagonist, aldosterone antagonist).
- Jouven X. La stimulation cardiaque en Afrique de l’ouest. Annales de cardiologie et d'angeiologie 52 (2003): 204.
- Thomas MO. Cost issues in pacemaker surgery in Nigeria. Nigerian Quarterly Journal of Hospital Medicine 14 (2004): 140-142
- Bonny A, Ngantcha M, Jeilan M, Okello E, Kaviraj B, Talle MA, et al. Statistics on the use of cardiac electronic devices and interventional electrophysiological procedures in Africa from 2011 to 2016: report of the Pan African Society of Cardiology (PASCAR) Cardiac Arrhythmias and Pacing Task Forces. Europace 20 (2018): 1513-1526.
- Connolly SJ, Kerr CR, Gent M, Roberts RS, Yusuf S, Gillis AM, et al. Canadian Trial of Physiologic Pacing Investigators. Effects of physiologic pacing versus ventricular pacing on the risk of stroke and death due to cardiovascular causes. N Engl J Med 342 (2000): 1385-1391.
- Lamas GA, Lee KL, Sweeney MO, Silverman R, Leon A, Yee R, et al. Mode Selection Trial in Sinus-Node-Dysfunction. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med 346 (2002) :1854-1862.
- Toff WD, Camm AJ, Skehan JD. United Kingdom Pacing and Cardiovascular Events (UKPACE) Trial Investigators. Single-chamber versus dual-chamber pacing for high-grade atrioventricular block. N Engl J Med 353 (2005): 145-155.
- Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 74 (2019): e51-e156.
- Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, et al. European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA),. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 15 (2013): 1070-1118.
- Naegeli B, Kurz DJ, Koller D, Straumann E, Furrer M, Maurer D, et al. Single-chamber ventricular pacing increases markers of left ventricular dysfunction compared with dual-chamber pacing. Europace 9 (2007): 194-199.
- Lin JC, Goldstein M, Benditt DG. UKPACE: to die, or not to die ... is that the question?. Europace 8 (2006): 852-854.
- Greenspon AJ, Patel JD, Lau E, Ochoa JA, Frisch DR, Ho RT, et al. Trends in permanent pacemaker implantation in the United States from 1993 to 2009: increasing complexity of patients and procedures. J Am Coll Cardiol 60 (2012): 1540-1545.
- Mond HG, Proclemer A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009--a World Society of Arrhythmia's project. Pacing Clin Electrophysiol 34 (2011): 1013-1027.
- Auricchio A, Ellenbogen KA. Reducing Ventricular Pacing Frequency in Patients With Atrioventricular Block: Is It Time to Change the Current Pacing Paradigm?. Circ Arrhythm Electrophysiol 9 (2016): e004404.
- Madhavan M, Mulpuru SK, McLeod CJ, Cha YM, Friedman PA. Advances and Future Directions in Cardiac Pacemakers: Part 2 of a 2-Part Series. J Am Coll Cardiol 69 (2017): 211-235.
- Adedinsewo D, Omole O, Oluleye O, Ajuyah I, Kusumoto F. Arrhythmia care in Africa. J Interv Card Electrophysiol 59 (2019): 127-135.
- Kane A, Sarr SA, Ndobo JVD, Tabane A, Babaka K, Aw F, et al. Cardiac pacing challenge in Sub-Saharan Africa environnement: experience of the Cardiology Department of Teaching Hospital Aristide Le Dantec in Dakar. BMC Cardiovasc Disord 19 (2019): 197.
- Kane A, Adoubi A, Niakara A, Houenassi M, Mbaye A, Sarr SA. et al. Diplôme universitaire de stimulation cardiaque en Afrique subsaharienne: un bel exemple de coopération Nord-Sud et Sud-Sud. La Presse Médicale Formation 1 (2020): 294-298.
- Udo EO, Zuithoff NP, van Hemel NM, de Cock CC, Hendriks T, Doevendans PA, et al. Incidence and predictors of short- and long-term complications in pacemaker therapy: the FOLLOWPACE study. Heart Rhythm 9 (2012): 728-735.
- Mulpuru SK, Madhavan M, McLeod CJ, Cha YM, Friedman PA. Cardiac Pacemakers: Function, Troubleshooting, and Management: Part 1 of a 2-Part Series. J Am Coll Cardiol 69 (2017): 189-210.
- Krzemie?-Wolska K, Tomasik A, Wojciechowska C, Bara?ska-Pawe?czak K, Nowalany-Kozielska E, Jache? W. Prognostic Factors in Patients with an Implanted Pacemaker after 80 Years of Age in a 4-Year Follow-Up. Gerontology 64 (2018): 107-117.
- Ouali S, Neffeti E, Ghoul K, Hammas S, Kacem S, Gribaa R, et al. DDD versus VVIR pacing in patients, ages 70 and over, with complete heart block. Pacing Clin Electrophysiol 33 (2010): 583-589.
- Ricci F, Sutton R, Palermi S, Tana C, Renda G, Gallina S, et al. Prognostic significance of noncardiac syncope in the general population: A systematic review and meta-analysis. J Cardiovasc Electrophysiol 29 (2018): 1641-1647.
- Nielsen JC. Mortality and incidence of atrial fibrillation in paced patients. J Cardiovasc Electrophysiol 13 (2002): S17-S22.
- Israel CW. The role of pacing mode in the development of atrial fibrillation. Europace 8 (2006): 89-95.
- Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 98 (1998): 946-52.
- Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the longterm risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/ Paisley study. Am J Med 113 (2002): 359-364.
- Kishore A, Vail A, Majid A, Dawson J, Lees KR, Tyrrell PJ, et al. Detection of atrial fibrillation after ischemic stroke or transient ischemic attack: a systematic review and meta-analysis. Stroke 45 (2014): 520-526.
- Davis RC, Hobbs FD, Kenkre JE, Roalfe AK, Hare R, Lancashire RJ, et al. Prevalence of left ventricular systolic dysfunction and heart failure in high risk patients: community based epidemiological study. BMJ 325 (2002): 1156.
After discharge, patients had a visit the first month, the third month, and then every six months. At the third month, we recorded the NYHA stage, early complications (i.e., those that occurred before three months), pacemakers parameters, and possible pacemaker dependency. The deadline for follow-up was December 31, 2017.We obtained data on late complications (those that occurred after the follow-up at three months), rehospitalizations, and deaths. If these data were not available in patients' files, we collected these data by telephone from the patients (with their prior agreement) or their referring physicians. We defined partial pacemaker dependency in patients with sinus dysfunction whose percentage of atrial stimulation was above 80% at a frequency programmed at a minimum frequency of 60 bpm and in patients with an atrioventricular block if the rate of ventricular stimulation was above 80% programmed at a minimum frequency of 60 bpm. Total pacemaker dependency was defined if, in addition to partial pacemaker dependency, spontaneous activity was absent at single atrial-chamber pacing (AAI) at 30 bpm (in sinus dysfunction) or single-ventricular chamber pacing (VVI) 30 bpm (in atrioventricular block) for 30 seconds.
2.3 Clinical endpoint
Because of the lack of possibility to determine the exact cause of death of most patients on the data obtained, death for all-cause was established as the endpoint.
2.4 Statistical analysis
We presented the characteristics of the study population and the cardiac pacing using descriptive statistics. We carried out the comparisons between the groups for the descriptive variables with the chi-square test, and, if not possible, Fisher's exact test for the categorical variables. The continuous variables were compared using the Student's t-test or the Mann-Whitney U test, according to their characteristics. A univariate Cox proportional hazards model was used to identify the independent predictors of all-cause death from the variables usually known as such. Variables with a p-value < 0.05 were included in the multivariable Cox model. The final models for predicting each study outcome were determined using all the variables from the initial model. The bootstrap method with 1000 iterations was used to validate the final model. The cumulative incidence of deaths was generated using the Kaplan-Meier method and compared using the log-rank test between the two groups studied and according to the type of pacemaker (single versus dual-chamber pacemaker). All the analysis were done in intention-to-treat. A value of p < 0.05 was considered statistically significant. The data were analyzed using SPSS software version 23.
2.5 Ethical considerations
The Abidjan Heart Institute ethics committee approved the study. The data collected were analyzed under the data protection laws for individuals, following ethical principles according to the Declaration of Helsinki.
3. Results
3.1 Patients' characteristics
During the period, among 325 patients implanted, 283 patients met the selection criteria. The patients' mean age was 67.3 ± 12.6 years; 49.1% were male (Table1). The main symptoms were syncope (38.5%) and dizziness (30.5%). Eighty-five patients (30%) had underlying heart disease. The primary indication for pacing was a complete atrioventricular (AV) block (83.3%). One hundred and eighty-nine patients (66.8%) received a single chamber ventricular pacemaker, and 94 (33.2%) a dual-chamber pacemaker. After implantation, 16 patients (5.7%) experienced early complications and 15 (5.3%) late complications (Table 2). After discharge, 257 patients (91.2%) had their pacemaker checked at three months. Six patients died before three months, and 20 others were not present at the visit on this date. The tests revealed frequent pacemaker dependency (76%).
3.2 Comparison of patients with single versus dual-chamber pacemaker (Table 1 & 2)
These two groups of patients were comparable concerning gender, comorbidities, underlying heart disease, and left ventricular ejection fraction (Table 1). But the patients with single-chamber pacemakers were significantly older (68.7 ± 11.2 vs 64 ± 14.8, p = 0.02), and more often had syncope (43.3% vs 28.7, p = 0.017). Single-chamber ventricular pacing was prescribed more often in patients with atrioventricular block (86.2 vs76.2, p = 0.042) and much less often in sinus dysfunction (1.1% vs 17%, p <0.001). Postoperatively, the complications were comparable in the two groups, as were the readmissions (Table 2). At 3 months, we observed a stronger dependency of patients with single-chamber pacemakers (34.9% vs 19.3%, p = 0.009) and a higher percentage of ventricular pacing (90.4 ± 19% vs 84.4 ± 28.1%, p = 0.043). During follow-up period, three patients with single-ventricular pacemaker experienced severe pacemaker syndrome. We upgraded their pacemaker to dual-chamber. Two patients with a dual-chamber pacemaker with atrial lead dislodgement had their pacemakers reprogrammed in single-ventricular pacing mode. We did the same procedure for two patients who had a permanent atrial fibrillation one year after dual-chamber pacemaker implantation.
3.3 Patients' prognosis (Table 3)
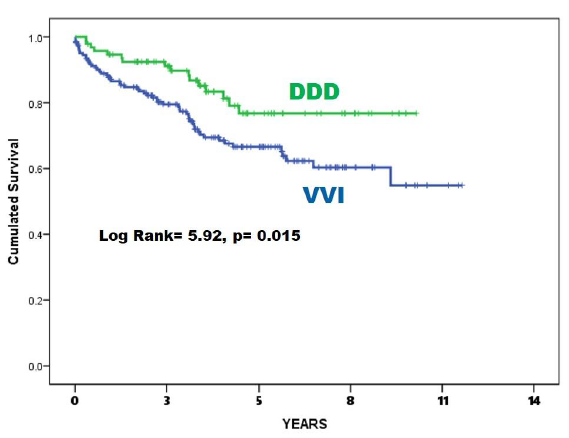
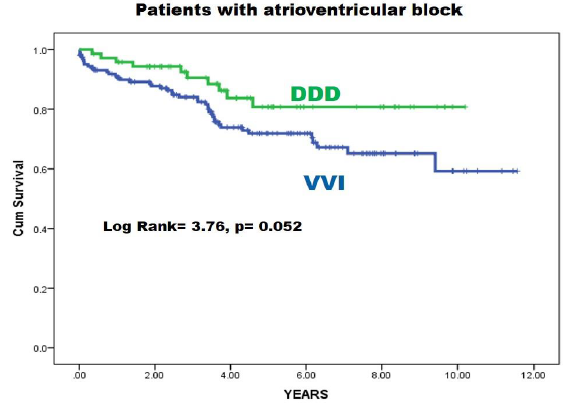
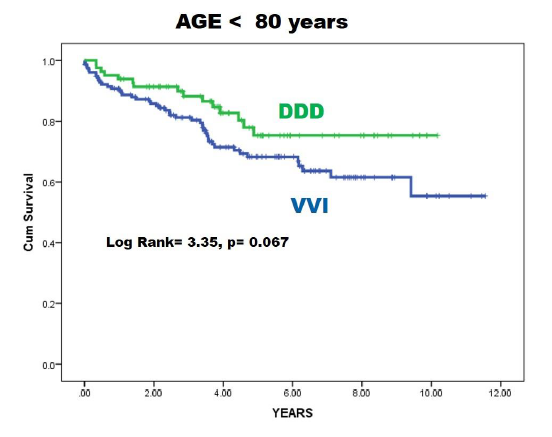
At the end of the follow-up period (median : 3.67 years, IQ [2.07;6.10], 73 patients (25.8%) was dead. In univariate analysis, according to the Cox model, the risk factors for death in our retrospective cohort were age, the presence of heart failure on admission, a left ventricular ejection fraction <0.40, syncope, the presence of atrial fibrillation, the occurrence of complications and the insertion of a single-chamber pacemaker (RR =1.974; 95% CI [1.132,3.44], p = 0.017) In multivariate analysis, only age was a factor of poor prognosis (RR = 1.027 95% CI [1.005,1.050], p = 0.017). The Kaplan-Meier curve and the Log-Rank test confirmed the prognostic role of the type of pacemaker (Log Rank = 5.97, p = 0.015) (Figure 1). But in the subgroups of patients with an atrioventricular block (without atrial fibrillation) (Figure 2) and in that of subjects under 80 years of age (Figure 3), this prognostic role was not confirmed (respectively p = 0.052 and p = 0.067).
|
Characteristics |
Overall N=283 |
VVI (N=189) |
DDD (N=94) |
p-value |
|
Demographic |
||||
|
Male (%) |
139 (49.1) |
89 (47.1) |
50 (53.2) |
0.33 |
|
Age (years) |
67.3 ± 12.6 |
68.7± 11.2 |
64 ± 14.8 |
0.02 |
|
Symptoms |
||||
|
Syncopes (%) |
109 (38.5) |
82 (43.3) |
27 (28.7) |
0.017 |
|
Presyncope (%) |
42 (14.8) |
30 (15.9) |
12 (12.8) |
0.49 |
|
Dizziness (%) |
86 (30.5) |
56 (29.6) |
30 (31.9) |
0.69 |
|
Asthenia (%) |
22 (7.8) |
10 (5.3) |
12 (12.8) |
0.027 |
|
Confusion |
12 (4.2) |
11 (5.8) |
1 (1,1) |
0.068 |
|
NYHA at admission |
||||
|
I |
179 (63.3) |
122 (64.9) |
57 (60.6) |
0.79 |
|
II |
21 (7.4) |
15 (7.9) |
6 (6.4) |
|
|
III |
74 (26.1) |
46 (24.3) |
28 (29.8) |
|
|
IV |
9 (3.2) |
6 (3.2) |
3 (3.2) |
|
|
Comorbidities |
||||
|
Hypertension (%) |
211 (74.6) |
140 (74.1) |
71 (75.5) |
0.79 |
|
Diabetes (%) |
45 (15.9) |
29 (15.3) |
16 (17) |
0.71 |
|
Heart failure |
68 (24) |
44 (23.3) |
24 (25.5) |
0.68 |
|
Main echocardiography findings |
||||
|
DCM (%) |
37 (13.1) |
22 (11.6) |
15 (16) |
0.35 |
|
ICM (%) |
10 (3.5) |
7 (3.7) |
3 (3.2) |
0.56 |
|
LVH |
29 (10.2) |
20 (10.6) |
9 (9.6) |
0.49 |
|
Normal heart (%) |
198 (70) |
137 (72.5) |
61 (64.9) |
0.12 |
|
Others (%) |
||||
|
LVEF |
0.61 ± 0.11 |
0.61 ± 0.11 |
0.60 ±0.12 |
0.56 |
|
LVEF<40% (%) |
20 (7.1) |
11 (5.8%) |
9 (9.6) |
0.25 |
|
Indications |
||||
|
AVB (%) |
235 (83) |
163 (86.2) |
72 (76.2) |
0.042 |
|
SND (%) |
18 (6.4) |
2 (1.1) |
16 (17) |
<0.001 |
|
AF (%) |
30 (10.6) |
24 (12.7) |
6 (6.4) |
0.10 |
|
Mode of Stimulation |
||||
|
VVI (%) |
189 (66.8) |
|||
|
DDD (%) |
94 (33.2) |
|||
|
Length of stay at Hospital (days) |
6 (4-8) |
6 (4-8) |
5 (4-7) |
0.07 |
|
Rehopitalization |
58 (20.5) |
41 (21.7) |
21 (18.1) |
0.48 |
|
Heart failure de novo |
12 (4,2) |
7 (3.7) |
5(5.3) |
0.54 |
|
Temporary pacing (%) |
184 (65) |
137 (72.5) |
47 (50) |
<0.0001 |
|
Medication at discharge |
||||
|
ACEI /ARB |
183 (64.7 |
124 (65.6) |
59 (62.8) |
0.64 |
|
Diuretics |
162 (57.2) |
108 (57.1) |
54 (57.4) |
0.96 |
|
Betablockers |
21 (7.4) |
8 (4.2) |
13 (14) |
0.003 |
|
Aldosteron Antagonist |
29 (10.2) |
14 (7.4) |
15 (16) |
0.025 |
|
Digoxin |
15 (5.3) |
12 (6.3) |
4 (4.3) |
0.47 |
|
Nitrates |
32 (11.3) |
22 (11.6) |
11 (11.7) |
0.99 |
|
Calcium channel blockers |
81 (29.4)) |
54 (28.7) |
29 (30.9) |
0.71 |
|
Amiodarone |
15 (5.3) |
9 (4.8) |
6 (6.4) |
0.56 |
|
Aspirin |
49 (17.3) |
31 (16.4) |
18 (19.1) |
0.57 |
|
Vitamin K antagonist |
17 (6) |
12 (6.3) |
4 (5.3) |
0.73 |
|
NYHA: New York Heart Association, DCM: Dilated cardiomyopathy, ICM: ischemic cardiomyopathy, LVEF: Left Ventricular Ejection Fraction, LVH: Left ventricular hypertrophy, AVB= atrioventricular block, SND: sinus node dysfunction, AF: Atrial Fibrillation. ACEI/ARB: angiotensin conversion enzyme inhibitors/ angiotensin 2 receptor blockers. |
||||
Table 1: Baseline characteristics of all patients and comparison between patients with a single-ventricular pacemaker (VVI) and a dual-chamber pacemaker (DDD).
|
Characteristics |
Overall N=283 |
VVI N= 169 |
DDD N= 88 |
P |
|
Pacemaker parameters at three months |
N = 257 |
|||
|
A pacing threshold, V |
0.5 (0.5-0.7) |
/ |
0.5 (0.5-0.7) |
/ |
|
Sensed P voltage, mV |
3.1 (2.25 – 4.95) |
/ |
3.1 (2.25 – 4.95) |
|
|
A lead impedance, ohm |
347.7 ± 121.3 |
/ |
347.7 ± 121.3 |
/ |
|
V pacing threshold, V |
0.93 ± 3.2 |
0.72 ± 0.72 |
1,33 ± 5.33 |
0.15 |
|
Sensed QRS voltage, mV |
10.5 ± 5 |
9.9 ± 4.3 |
10.5 ± 5 |
0.06 |
|
V lead impedance, ohm |
403.5 ± 93.2 |
413.3 ± 102.3 |
384.5 ± 69.6 |
0.018 |
|
Cumulative A pacing, % |
31.24 ± 33.4 |
/ |
31.24 ± 33.4 |
/ |
|
Cumulative V pacing, % |
88.4 ± 22.7 |
90.4 ± 19 |
84.4 ± 28.1 |
0.043 |
|
Complete pacemaker Dependency (n= 257) |
76 (26.9) |
39 (34.9) |
17 (19.3) |
0.009 |
|
Partial pacemaker Dependency (n= 257) |
215 (83.7) |
145 (85.8) |
70 (79.5) |
0.2 |
|
NYHA at 3 months (n = 257) |
||||
|
I. |
216 (84)) |
140 (82.8) |
76 (86.4) |
0.11 |
|
II |
29 (10.9) |
17 (10.1) |
11(12.5) |
|
|
III |
13 (5.1) |
12 (7.1) |
1 (7.7) |
|
|
Early complications |
16 (5.7) |
7 (4.1) |
8 (9.1) |
0.11 |
|
Late complications (%) |
15 (5.3) |
8 (4.7) |
6 (6.8) |
0.48 |
|
Rehospitalisation |
58 (20.5) |
41 (21.7) |
21 (18.1) |
0.48 |
Table 2: Data on the patients’ follow-up. Comparison between patients with a single-ventricular pacemaker (VVI) and a dual-chamber pacemaker (DDD).
|
Variables |
Univariate analysis |
Multivariate analysis |
|||||||
|
p-value |
HR |
95% CI |
p-value |
HR |
95% CI |
||||
|
Lower |
Upper |
Lower |
Upper |
||||||
|
Age |
0.005 |
1.030 |
1.009 |
1.052 |
0.017 |
1.027 |
1.005 |
1.050 |
|
|
Hypertension |
0.999 |
1.000 |
0.580 |
1.723 |
|||||
|
Diabete |
0.703 |
1.125 |
0.616 |
2.054 |
|||||
|
Temporary pacing |
0.135 |
.821 |
.633 |
1.063 |
|||||
|
VVI ± R pacing |
0.017 |
1.974 |
1.132 |
3.441 |
0.07 |
0.588 |
0.333 |
1.040 |
|
|
Complications |
0.005 |
2.39 |
1.31 |
4.36 |
0.103 |
1.720 |
0.895 |
3.305 |
|
|
Atrial Fibrillation |
<0.001 |
3.694 |
2.102 |
6.492 |
0.015 |
2.181 |
1.162 |
4.092 |
|
|
AVB |
0.001 |
0.432 |
0.257 |
0.725 |
|||||
|
Syncopes |
0.014 |
1.797 |
1.128 |
2.861 |
0.145 |
1.439 |
0.882 |
3.241 |
|
|
Heart failure |
0.002 |
2.139 |
1.335 |
3.428 |
0.185 |
1.444 |
0.839 |
2.487 |
|
|
LVEF < 0.40 |
<0.001 |
3.671 |
1.968 |
6.846 |
0.093 |
1.925 |
0.897 |
4.131 |
|
|
NYHA: New York Heart Association, LVEF: Left Ventricular Ejection Fraction, SND: Sinus Node Disease, AVB: AtrioVentricular Block. |
|||||||||
Table 3: Univariate and Multivariate analysis of prognostic factors of death.
4. Discussion
In our cohort of patients from sub-Saharan Africa, patients with single-chamber pacing had a more severe prognosis than patients with dual-chamber pacing. But this higher mortality was linked to older age and a more significant presence of atrial fibrillation in this group. The characteristics of patients receiving cardiac stimulation in sub-Saharan Africa differ from those in developed countries: they are much fewer, younger, and have a more severe clinical status [1, 15, 16]. Indeed, there is insufficient infrastructure and a lack of specialists practicing pacemaker therapy [2, 17]. It doesn't even exist in some countries. Besides, the cost appears excessive for the populations [2]. So much so that, among the patients who indicate cardiac pacing, very few benefit from it. These are generally the youngest patients (still in activity, therefore able to cover the pacemaker's cost) and the most serious (those who have frequent syncopes or pre-syncopes). In our cohort, we have a large number of patients who had syncopes or pre-syncopes (53.3%), a large number of patients with pacemaker dependency, and very few presenting with sinus node dysfunction.
In our context, patients prefer single-ventricular pacemakers because of their lowest cost. Although being the third choice in an atrioventricular block, it is easier to implant in the ESC guidelines and is associated with fewer complications than the DDD pacemaker [8, 18]. In our work, we have twice more difficulties with DDD, but this difference is not significant. But in 2020, the advantages of the dual-chamber pacemaker are indisputable [19]: it avoids the pacemaker syndrome, which may require reoperation. It allows, with its memories, to diagnose with precision paroxysmal ventricular and supraventricular arrhythmias. It avoids the unnecessary pacing of the right ventricle, which can be deleterious in certain situations with the news algorithm for preserving ventricular pacing. It decreases the risk of atrial fibrillation [4-6]. When we compare the two groups of patients, we realize that the single-chamber pacemaker was (unintentionally) chosen for the most severe cases: older subjects with a greater syncope and atrial fibrillation frequency. These three characteristics may explain the higher mortality in this group.
Older subjects naturally have a poorer prognosis than younger subjects. They also have a more significant number of comorbidities. Finally, the dual-chamber pacing would be more beneficial for them in this area. In a study of 140 patients over 80 years of age followed for four years after implantation of pacemakers, the prognosis was significantly favorable in the group of patients with dual versus single-chamber pacing (20). In a randomized, double-blind study with double cross-over, Ouali et al. analyzed patients' clinical status over 70 years of age stimulated for atrioventricular block [21]. They showed that patients in single-chamber with rate response (VVIR mode) had a lower quality of life than dual-chamber pacing. Also, they experienced impaired left ventricular function, left atrium enlargement, and degradation of their functional capacity. These changes can lead to heart failure more quickly and then to death. Syncope is usually a clinical manifestation that unequivocally indicates pacemaker implantation for patients with proven or suspected severe bradycardia. But another aetiology cannot be ruled out if the mechanism of syncope is not documented. Ricci et al.'s meta-analysis showed that among older, diabetic, and/or hypertensive individuals, a history of noncardiac/unexplained syncopes, even in the absence of an obvious cardiac etiology, is associated with higher all-cause mortality [22]. Atrial fibrillation is relatively common in the elderly and among patients with pacemakers [23]. Single-ventricular pacing, in that case, favors its occurrence [4]. Atrial fibrillation increases the risk of death by two in women and by 1.5 in men [25, 26]. 20 to 30% of strokes are due to this condition [27]. And we find 20 to 30% of left ventricular dysfunction among patients with atrial fibrillation [28]. The single ventricular- pacing mode (with rate response) is recommended for patients with permanent atrial fibrillation [7, 8]. All these facts combined may explain that, in our cohort, atrial fibrillation is a predictor of death and associated with single-ventricular pacing.
4.1 Limitations
This work was a retrospective, non-randomized study. So, some data could not be obtained. Left ventricular ejection fraction was not assessed, after pacemaker implantation, during the follow-up. QRS duration and type were not taken into account and could help to understand patients' outcomes. Switches from dual-chamber mode to single ventricular mode and vice-versa were not considered. But despite these shortcomings, our study had the advantage of being carried out in real life and giving results consistent with the randomized studies.
5. Conclusion
This study allows us to consider changes to our practices even though our resources are limited. Thus, we need to reconsider the dual-chamber pacing in the elderly. Besides, we should use the methods of preservation of right ventricular pacing to avoid the occurrence of de novo atrial fibrillation. If the left ventricular ejection fraction is impaired, it would be helpful to avoid pacing in the apex of the right ventricle; It would be better to perform His or left bundle branch pacing.
Ethics Statement
The Abidjan Heart Institute ethics committee approved the study. The data collected were analyzed under the data protection laws for individuals, following ethical principles according to the Declaration of Helsinki.
Acknowledgements
The authors express their gratitude to the staff of the pacing unit of Abidjan Heart Institute.
Conflicts of Interest
None declared. All the authors express that there was no conflict of interest in writing this research article


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 