The Effect of High-Dose Statin Therapy on Reducing Major Adverse Cardiac Events in Diabetic Patients: A Systematic Review and Meta-Analysis
Karan Rajeshkumar Chaudhari1, Sarah Hack2, Sumaiya Khan3, Lakshmi Malavika Reddy Meka4, Ahsan Munir5, Dost Mohammad Zumman6, Khadijat Ishola-Gbenla7, Zaki Ur Rahman Mohammed8, Marium Abid9, Binish Essani10, Shah Zaib Bhindar11, Muhammad Sohail S. Mirza12*
1Gujarat Medical Education Research Society, Sola, Ahmedabad, India
2St. George’s University, Grenada, West Indies
3Khaja Bandanawaz Institute of Medical Sciences, Karnataka, India
4Gandhi Medical College and Hospital, Hyderabad, Telangana, India
5Al-Nafees Medical College, Islamabad, Pakistan
6Sylhet M. A. G. Osmani Medical College, Sylhet, Bangladesh
7University of Medicine and Health Sciences, St. Kitts, West Indies
8North Dakota State University, North Dakota, USA
9Jinnah Medical & Dental College, Karachi, Pakistan
10Jinnah medical and dental college, Karachi, Pakistan
11Nishtar Medical College, Multan, Pakistan
12Muhammad Sohail S. Mirza, MBBS. Shandong University School of Medicine, Jinan, China
*Corresponding author: Muhammad Sohail S. Mirza, MBBS, Shandong University School of Medicine, Jinan, China.
Received: 29 August 2025; Accepted: 17 September 2025; Published: 19 September 2025.
Article Information
Citation:
Karan Rajeshkumar Chaudhari, Sarah Hack, Sumaiya Khan, Lakshmi Malavika Reddy Meka, Ahsan Munir, Dost Mohammad Zumman, Khadijat Ishola-Gbenla, Zaki Ur Rahman Mohammed, Marium Abid, Binish Essani, Shah Zaib Bhindar, Muhammad Sohail S. Mirza. The Effect of High-Dose Statin Therapy on Reducing Major Adverse Cardiac Events in Diabetic Patients: A Systematic Review and Meta-Analysis. Cardiology and Cardiovascular Medicine 9 (2025): 404-414.
View / Download Pdf Share at FacebookAbstract
High-dose statin therapy has been widely used for cardiovascular risk management, particularly in diabetic patients who are at high risk of major adverse cardiovascular events (MACE). This systematic review and meta-analysis aimed to assess the effectiveness of high-dose statins in reducing MACE in diabetic patients while also evaluating the potential risk of new-onset diabetes mellitus (NODM). A comprehensive search was conducted across databases, including PubMed, Cochrane Library, and Google Scholar, focusing on studies published between 2020 and 2025. The inclusion criteria targeted studies that compared high-dose statin therapy with either lower doses or placebo in diabetic populations, with MACE and NODM as primary outcomes. The pooled analysis revealed a moderate positive effect of high-dose statins on reducing cardiovascular events (effect size = 0.90, 95% CI: 0.68–1.12), though there was significant variability across studies. Additionally, high-dose statins were associated with an increased risk of NODM, consistent with other research in the field. The I² statistic was 91.18%, indicating substantial heterogeneity across studies. Publication bias was minimal, as assessed by funnel plots and Egger’s regression. Quality assessment using the RoB 2 and NOS tool revealed variability in methodological rigor, with some studies showing higher risks in randomization and blinding. Despite the benefits of statin therapy in preventing cardiovascular events, the potential for increased diabetes risk suggests the need for a balanced, personalized approach. Further research is required to optimize statin regimens, minimize side effects, and refine treatment strategies for diabetic patients at cardiovascular risk.
Keywords
High-dose statins, Major adverse cardiovascular events, Newonset diabetes mellitus, Diabetic patients, Meta-analysis
High-dose statins articles, Major adverse cardiovascular events articles, New-onset diabetes mellitus articles, Diabetic patients articles, Meta-analysis articles
Article Details
1. Introduction and Background
Diabetes mellitus (DM) is a significant risk factor for cardiovascular disease (CVD), with diabetic patients experiencing a substantially higher risk of major adverse cardiac events (MACE) such as myocardial infarction (MI), stroke, and death due to cardiovascular causes [1,2]. The use of statins in reducing cholesterol levels in the body can be regarded as the foundation of cardiovascular event prevention, especially in high-risk groups of people, such as diabetic patients [3]. Nevertheless, the most effective statin regimen for diabetic patients, particularly regarding the intensity and dose, is an issue to be investigated [4].
Intensive statin treatment has been related to lower MACE rates not only in the general population, but also in patients with type 2 diabetes (T2DM) [5]. Specifically, the statins with the highest intensity, such as atorvastatin and rosuvastatin, are commonly prescribed in people with CVD because they strongly reduce lipids [6]. Nevertheless, the drugs also have an increased risk of the development of new-onset diabetes mellitus (NODM) [7]. This irony, the association of statins in decreasing cardiovascular events, yet putting the patient at risk of diabetes, has led to a surge of studies on the net benefit of statin therapy at high doses in diabetic individuals [8].
According to various studies, it has been proposed that high-dose statins are effective in lessening MACE among diabetic patients, but depending on the initial patient profile and the kind of statin administered [9]. A study revealed that in diabetic patients subjected to percutaneous coronary intervention (PCI) after pre-treatment with high-dose statins, the rates of MACE and periprocedural MI were significantly reduced as compared to low-dose statin patients or those without the intake of statins [10]. On the same note, the combination of statin therapy with diabetes treatment has consistently demonstrated significant effects on lowering adverse cardiovascular events, including patients with prediabetes [11].
Nonetheless, although statin therapy has been demonstrated to lower MACE in patients with diabetes, this is controversial in terms of the association of statin dosage and the risk of diabetes [12]. Evidence shows that statin therapy sometimes, most particularly when used in high doses, increases the chances of developing diabetes [13]. This increased risk of diabetes is important to appreciate because the long-term effectiveness of statins to reduce MACE is more than worth it.
Furthermore, statins' efficacy in diabetic patients depends on the ability to take medication, the length of treatment, and levels of lipid starting point [14]. Analyses of observational studies meta-analytically revealed that statin treatment can decrease the MACE and death rate substantially in T2DM patients with high LDL cholesterol levels, in particular [15]. Nevertheless, it remains unclear how long and how intensively statins should be taken, especially in patients with well-controlled diabetes [16]. Recent evidence indicates that statin exposure is one of the most effective factors in protecting against cardiovascular disease, and the length of when the person takes the treatment may be more important than the level of the dose [17].
To this end, under these complexities, this systematic review and meta-analysis would attempt to evaluate the impact of high-dose statin therapy on the reduction of MACE in diabetics. A synthesis of recent clinical trials and observational studies will enable this review to develop a full picture of the therapeutic promise of implementing high-dose statin treatment and the risks that it implies, especially regarding the occurrence of diabetes in predisposed populations. This review is also going to touch on the literature gaps on the most effective dose/duration of statin dose on maximizing cardiovascular advantage in diabetic individuals and minimizing the negative aspects associated with glucose metabolism.
2. Methods
2.1 Data Sources and Search Strategy
The effect of high-dose statin therapy on the reduction of MACE among diabetic individuals was determined by conducting a comprehensive literature review. The search was limited to include only the most current and up-to-date evidence up to 2025. Leading databases were searched, which are PubMed, Cochrane Library, and Google Scholar. This search strategy was conducted transparently and reproducibly, based on PRISMA. Both keywords and controlled vocabulary (MeSH terms) were used to capture the broadest range of studies. Keywords such as “high-dose statins,” “diabetes mellitus,” “major adverse cardiac events,” “myocardial infarction,” “stroke,” “cardiovascular mortality,” “atorvastatin,” “rosuvastatin,” and “secondary prevention” were used in various combinations. The Boolean operators AND and OR were employed to combine these terms. The search was limited to human studies published in English to ensure the accessibility and relevance of the findings. Additionally, conference abstracts, grey literature, and unpublished data were excluded to maintain the quality of the review.
|
Database |
Search Terms Used |
Filters Applied |
Truncations/Syntax |
|
PubMed |
("high-dose statins" OR atorvastatin OR rosuvastatin) AND ("diabetes mellitus" OR "type 2 diabetes") AND ("major adverse cardiac events" OR MACE OR "myocardial infarction" OR stroke) |
Human studies, English, 2020-2025 |
Quotation marks for phrases, OR for alternate terms, AND for combining concepts |
|
Cochrane Library |
("high-dose statin" OR atorvastatin OR rosuvastatin) AND ("diabetes mellitus" OR "type 2 diabetes") AND ("no wildcard support") |
Human studies, Systematic Reviews, English |
Use of AND/OR for terms, no truncations needed |
|
Google Scholar |
("high-dose statins" OR atorvastatin OR rosuvastatin) AND ("diabetes mellitus" OR "type 2 diabetes") AND ("major adverse cardiac events" OR MACE OR "myocardial infarction") |
Human studies, English, 2020-2025 |
Use of quotation marks for exact phrases, OR for alternate terms, AND for combining terms |
Table 1: Search strategy across databases.
2.2 Inclusion and exclusion criteria: The PICOS framework guided the inclusion and exclusion criteria, ensuring that only studies on high-dose statin therapy in diabetic patients with MACE outcomes were included, while irrelevant studies were excluded (see Table 2).
|
PICOS Element |
Inclusion Criteria |
Exclusion Criteria |
|
Population |
Diabetic patients (type 1 or type 2 diabetes), with or without cardiovascular comorbidities (e.g., myocardial infarction, stroke, undergoing PCI). |
Non-diabetic patients, patients with other primary conditions (e.g., non-cardiovascular diseases), or patients under 18 years old. |
|
Intervention |
High-dose statin therapy (e.g., atorvastatin 40–80 mg, rosuvastatin 20–40 mg, or equivalent doses of other high-intensity statins). |
Low-dose statin therapy (e.g., atorvastatin ≤20 mg or simvastatin ≤20 mg), non-statin therapies, or studies not focusing on statins. |
|
Comparison |
Studies comparing high-dose statin therapy to lower doses of statins or placebo. |
Studies that do not include a comparison group, such as single-arm studies. |
|
Outcome |
MACE, including myocardial infarction, stroke, cardiovascular death, revascularization, and other related cardiovascular events. |
Studies that do not report MACE or related cardiovascular outcomes (e.g., studies focused on diabetes-specific outcomes). |
|
Study Design |
RCTs, cohort studies, and case-control studies. |
Animal studies, case reports, observational studies with insufficient data, and non-controlled studies. |
Table 2: PICOS Framework for Recent Study.
2.3 Data Extraction: Data extraction for this systematic review was carried out using a standardized form by two independent reviewers to ensure consistency and accuracy. The extracted data included study characteristics such as author(s), publication year, study design, and location. Participant details, including sample size, age, gender, comorbidities, and diabetes type, were also recorded. For the intervention, information was collected regarding the specifics of high-dose statin therapy, including the type of statin, dosage, and duration of treatment. The main effects, such as MACE, were recorded, and the minor results (adverse events or new-onset diabetes) were taken. Where there was any inconsistency between reviewers when identifying the data to be extracted, a third reviewer was utilized to clarify the inconsistency and make it uniform.
2.4 Quality Assessment: Each study included was assessed as part of quality in accordance with the right tools, depending upon the characteristics of the study performed. To assess the risk of bias, a Cochrane Risk of Bias 2 (RoB 2) tool was applied to identify possible biases based on aspects of randomization, allocation concealment, blindness, incomplete data on outcomes, and selective reporting in the context of RCTs [18]. In the case of the cohort studies, the Newcastle-Ottawa Scale (NOS) was used to evaluate the selection of the people, group-comparability, and measurement of the outcomes [19].
There were funnel plots, and asymmetry was assessed, and the Egger regression test was applied to identify the small-study effects to examine publication bias. Provided that publication bias was likely, the trim-and-fill technique was used to correct the outcomes to reflect more properly on the evidence [20].
2.5 Statistical Analysis: The statistical analysis for this systematic review was done using a random effect model due to study design, participant characteristics, interventions, and variability in the results. Power size with 95% confidence interval (CI) was used to determine the effect of high-khurak statin treatment on MACE and other cardiovascular consequences. The random power model was chosen to provide more reliable results for potential differences in studies. The degree of asymmetry between studies was evaluated using the statistical, which indicated low, moderate, and high inequality with values of 25%, 50% and 75% respectively. Subscribers were analyzed to check the effect of variables such as study design, state type, age, gender, and compliance with treatment on treatment effects.
3. Results
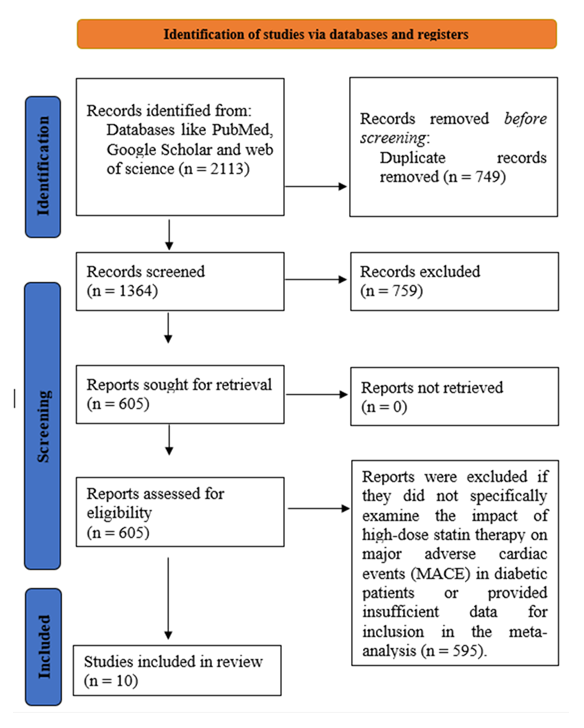
3.1 Study selection: Initially, 2113 studies were identified through searches across multiple databases and other sources. After removing duplicates and articles that did not meet the initial criteria, 1364 studies were assessed for eligibility. Among these, 759 studies were excluded as they did not focus on high-dose statin therapy or relevant cardiovascular outcomes. After a thorough full-text review, 605 studies were considered in detail. Of these, 595 were excluded because they did not meet the inclusion criteria, either due to not involving high-dose statins, lacking relevant outcomes such as MACE, or missing necessary data for meta-analysis. Ultimately, 10 clinical trials were included in the review, providing data on the effects of high-dose statin therapy on reducing MACE in diabetic patients.
3.2 Characteristics of the included studies: The studies included in this systematic review and meta-analysis cover a diverse range of designs, populations, and interventions. The studies primarily focus on patients with T2DM and those at high cardiovascular risk, including patients with coronary artery disease (CAD), AMI, and those undergoing coronary interventions. The majority of studies examine the effect of high-dose statin therapy (atorvastatin, rosuvastatin) on MACE and NODM. Study designs include RCTs, prospective and retrospective cohort studies, and observational studies. Most studies compare high-intensity statin therapy to lower doses or placebo, with outcomes focusing on cardiovascular events such as myocardial infarction, ischemic stroke, and cardiovascular death, as well as the development of diabetes. The risk of bias varies, with most studies showing low or moderate risk, while some, especially retrospective cohort studies, face challenges related to confounding factors and study design. The studies are well-suited for analyzing the impact of high-dose statins on cardiovascular outcomes in diabetic patients, providing valuable data on the efficacy and safety of statin therapy in this high-risk population.
|
Study Details |
Study Design |
Population |
Intervention |
Comparison |
Outcomes |
|
Poorhosseini et al. [21] |
Retrospective cohort study |
819 post-CABG patients with prediabetes at the time of surgery |
Atorvastatin (10–80 mg), Rosuvastatin (5–40 mg) |
High-intensity statins vs. low-intensity statins |
Primary: Development of T2DM; Secondary: MACE |
|
Takahashi et al. [22] |
Retrospective cohort study |
927 diabetic patients with CAD |
Statin therapy (various doses) |
High Lp(a) group vs. low Lp(a) group |
Primary: MACE including cardiovascular death, non-fatal MI, non-fatal CI |
|
Thongtang et al. [23] |
RCT |
150 T2D patients with no established ASCVD, LDL-C <100 mg/dl on low-dose statin therapy |
Low-dose statin (simvastatin ≤20 mg/day) vs. high-intensity statin (atorvastatin 40–80 mg/day) |
Low-dose statin group vs. high-intensity statin group |
Primary: Plasma LDL-C levels; Secondary: Safety (adverse events) and muscle symptoms |
|
Choi et al. [24] |
Prospective cohort study |
2,221 patients with AMI without diabetes at baseline, treated with high-intensity statins |
Atorvastatin 40–80 mg, Rosuvastatin 20 mg |
Atorvastatin vs. Rosuvastatin |
Primary: NODM, MACE (death, MI, revascularization) |
|
Kim et al. [25] |
Population-based cohort study |
8,937 patients with T2D (≥40 years) who received statins |
Statin therapy (low, moderate, or high intensity) |
Low-intensity statins vs. moderate/high-intensity statins |
Primary: MACE, including ischemic heart disease, ischemic stroke, cardiovascular death |
|
Kim et al. [26] |
Cohort study |
11,900 T2DM patients (≥40 years) |
Statins (moderate or high intensity) |
No direct comparison between statin doses; focus on lipid profile effects |
Primary: MACE, including ischemic heart disease (IHD), ischemic stroke (IS), cardiovascular death |
|
Steenhuis et al. [27] |
Retrospective cohort study |
39487 primary prevention patients with diabetes on statin therapy |
Statin therapy (low, moderate, or high intensity) |
Statin users with MACE vs. non-MACE statin users |
Primary: MACE including MI, ischemic stroke, and cardiovascular death |
|
Wu et al. [28] |
Observational cohort study |
45013 patients with T2D and CVD |
Statin therapy (low and high intensity) |
Statin therapy vs. no statin therapy |
Primary: MACE, including MI, stroke, cardiovascular death |
|
Lee et al. [29] |
Prospective cohort study |
13104 AMI patients without diabetes at baseline, treated with atorvastatin or rosuvastatin after PCI |
Atorvastatin (moderate to high intensity), Rosuvastatin (moderate to high intensity) |
Moderate-intensity statins vs. high-intensity statins |
Primary: NODM, MACE |
|
Shah et al. [30] |
Retrospective cohort study |
7,239 adults with diabetes, no prior atherosclerotic cardiovascular disease (ASCVD), and LDL-C ≥100 mg/dL |
Statin therapy (delayed vs. immediate initiation) |
Immediate statin initiation vs. delayed statin therapy |
Primary: MACE including MI and ischemic CVA |
Table 3: Summary of studies involved in the study.
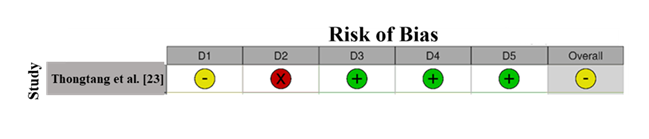
3.3 Quality assessment: RoB assessment for Thongtang et al. [23] using the Cochrane Risk of Bias 2 (RoB 2) tool reveals some concerns (Figure 2). The study has a high risk of bias in the deviations from the intended interventions domain (D2), marked with a red "X," indicating issues in how the intervention was conducted. However, it shows low risk of bias in missing outcome data (D3), measurement of the outcome (D4), and selection of reported results (D5), all marked with green ticks. The overall assessment is marked with a yellow circle, indicating some concerns due to the intervention deviations.
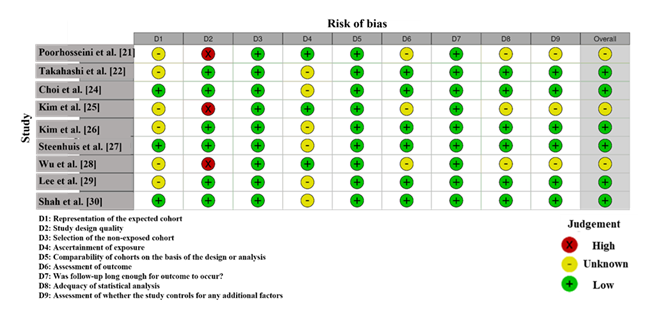
Figure 3 displays the RoB assessment across nine studies (Poorhosseini et al. [21], Takahashi et al.[22], Choi et al.[24], Kim et al. [25], Kim et al. [26], Steenhuis et al. [27], Wu et al.[28], Lee et al.[29], Shah et al.[30]) using the RoB 2 tool, which evaluates nine domains (D1-D9). The studies generally show a low risk of bias (green) across most domains, with only a few studies exhibiting high risk (red). For example, Poorhosseini et al. [21] and Wu et al. [28] show a high risk in D2 (Deviations from intended interventions), indicating issues with intervention implementation. Several studies, including Shah et al.[30] and Kim et al. [26] display an unclear risk (yellow) for domains like D1 (Randomization) and D9 (Selection of reported result), suggesting potential ambiguities in methodology. Most studies are assessed as having a low risk of bias, with specific concerns related to intervention deviations and randomization. While the majority demonstrate methodological robustness, the unclear risks and a high risk in intervention implementation for a few studies.
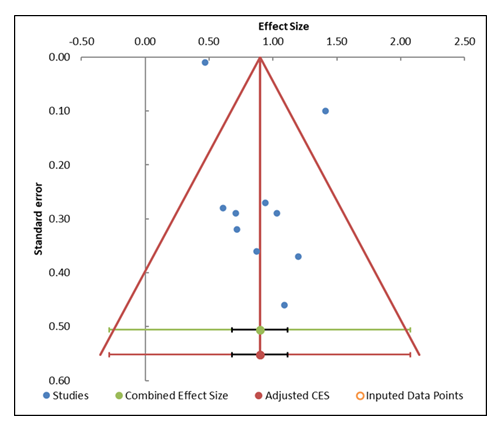
3.4 Publication Bias: The funnel plot (Figure 4) and accompanying Egger's regression results (Table 5) provide valuable insights into the potential for publication bias in this meta-analysis. The funnel plot demonstrates a relatively symmetrical distribution of studies on both sides of the combined effect size, which suggests no substantial publication bias. Studies with larger standard errors are clustered towards the bottom of the plot, and studies with smaller standard errors are distributed towards the top, consistent with typical funnel plot patterns. The Egger regression test further confirms this lack of significant bias. The intercept value is 0.95, with a slope of 0.34, and the p-value for the slope is 0.663, which is greater than the conventional threshold of 0.05. This suggests that there is no statistically significant evidence of publication bias in the data. The 95% confidence interval for the slope ranges from –3.79 to 2.32, which includes zero, further supporting the absence of bias. Additionally, the trim-and-fill analysis was performed to adjust for missing studies. The results indicate that no studies needed to be imputed, meaning there are no missing studies affecting the symmetry of the funnel plot. This supports the conclusion that the funnel plot is balanced and free from significant publication bias.
|
Study name |
Effect Size (z) |
Standard error (z) |
|
Poorhosseini et al. [21] |
1.09 |
0.46 |
|
Takahashi et al. [22] |
1.41 |
0.10 |
|
Takahashi et al. [23] |
0.71 |
0.29 |
|
Choi et al. [24] |
0.94 |
0.27 |
|
Kim et al. [25] |
0.72 |
0.32 |
|
Kim et al. [26] |
0.61 |
0.28 |
|
Steenhuis et al. [27] |
1.03 |
0.29 |
|
Wu et al. [28] |
0.87 |
0.36 |
|
Lee et al. [29] |
1.20 |
0.37 |
|
Shah et al. [30] |
0.47 |
0.01 |
|
Combined effect size |
Observed |
|
|
Effect size |
0.90 |
Not analyzed |
|
SE |
0.10 |
Not applicable |
|
CI Lower limit |
0.68 |
Not applicable |
|
CI Upper limit |
1.12 |
Not applicable |
|
PI Lower limit |
-0.28 |
Not applicable |
|
PI Upper limit |
2.08 |
Not applicable |
|
Heterogeneity |
Not analyzed |
|
|
Q |
102.06 |
Not analyzed |
|
pQ |
0.000 |
Not analyzed |
|
I2 |
91.18% |
Not applicable |
|
T2 |
0.26 |
Not applicable |
|
T |
0.51 |
Not applicable |
Table 4: Information related to funnel plot.
|
Parameter |
Estimate |
SE |
CI LL |
CI U |
|
Intercept |
0.95 |
2.09 |
-3.79 |
5.68 |
|
Slope |
0.34 |
1.23 |
-2.43 |
3.12 |
|
t test |
0.45 |
Not applicable |
Not applicable |
Not applicable |
|
p-value |
0.663 |
Not applicable |
Not applicable |
Not applicable |
Table 5: Egger Regression.
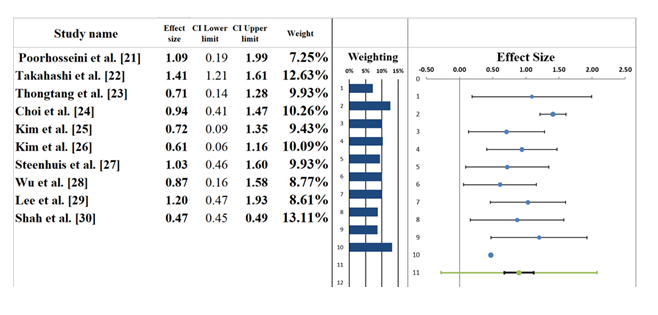
3.5 Forest plot: The forest plot (Figure 5) presents the results of a meta-analysis evaluating the impact of high-dose statin therapy on reducing MACE in diabetic patients. A random-effects model was utilized, yielding a pooled effect size of 0.90, with a 95% CI ranging from 0.68 to 1.12. This suggests high effectiveness, but the wide confidence interval highlights significant heterogeneity in the individual study outcomes. Individual studies contribute differently to the overall effect, with varying effect sizes and confidence intervals. For instance, Poorhosseini et al. [21] reports an effect size of 1.09, indicating a modest effect of statins in preventing cardiovascular events. In contrast, Shah et al. [30] shows a smaller effect size (0.47), with a broader confidence interval, suggesting weaker evidence of benefit in that cohort. On the other hand, Takahashi et al. [22] demonstrates a higher effect size of 1.41, highlighting a stronger positive outcome from statin therapy. The study weights, ranging from 7.25% to 13.11%, reflect the influence of each study on the overall pooled effect size. The results indicate a moderate effect of statins, but the wide variability in the findings suggests that further research is required to clarify the effectiveness and optimize the use of statins in diabetic patients with cardiovascular risk [31].
|
Meta-analysis model |
|
|
Effect Size |
0.90 |
|
Standard Error |
0.10 |
|
Confidence interval LL |
0.68 |
|
Confidence interval UL |
1.12 |
|
Prediction interval LL |
-0.28 |
|
Prediction interval UL |
2.08 |
|
Z-value |
9.26 |
|
One-tailed p-value |
0.000 |
|
Two-tailed p-value |
0.000 |
|
Number of incl. subjects |
1469 |
|
Number of incl. studies |
10 |
|
Heterogeneity |
|
|
Q |
102.06 |
|
pQ |
0.000 |
|
I2 |
91.18% |
|
T2 (z) |
0.26 |
|
T (z) |
0.51 |
Table 6: Information correlated with Forest plot.
3.6 Heterogeneity Assessment: The heterogeneity assessment of the studies (Table 6) included in this meta-analysis shows considerable variation in the results. The I² statistic is 91.18%, indicating that a substantial portion of the total variation in effect sizes is attributable to real differences between studies rather than random sampling error. This level of heterogeneity falls into the moderate to high range, suggesting that factors such as study design, patient characteristics, statin dosage, and cardiovascular risk profiles likely contributed to variability in outcomes. The Q-statistic value of 102.06, with a p-value of 0.000, confirms that the observed heterogeneity is statistically significant. This suggests that the differences between the studies are not due to chance but reflect genuine disparities in the way the statin therapy impacts cardiovascular events in diabetic patients. Additionally, the T² value of 2.08 quantifies the between-study variance, further highlighting the considerable variability in the effects observed across the included studies. These findings underscore the need for caution when interpreting the overall pooled effect. The variability across studies suggests that the effectiveness of statin therapy on MACE in diabetic patients may depend on various factors, including statin type, dosage, and patient characteristics [32].
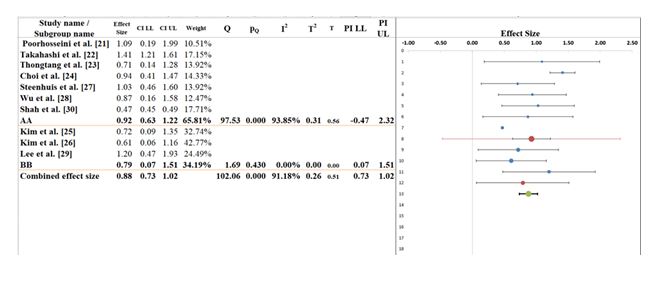
3.7 Subgroup analysis: The subgroup assessment (Figure 5) evaluates the consequences of statin remedy on cardiovascular effects in fantastic subgroups, AA and BB, to find out the versions in impact sizes during the ones organizations. The common pooled impact length, calculated at 0.88 (95% CI: 0.73 to at least 1.02), indicates a slight excellent impact throughout all studies covered within the analysis. However, the high heterogeneity, contemplated by means of the I² statistic of 91.18%, suggests that huge version exists within the consequences throughout the research, and this variability can be due to versions in affected person populations, statin doses, or have a look at methodologies [33].
For Subgroup AA, which includes the majority of the research, the pooled impact size is 0.90 (95% CI: 0.63 to at least 1.22), displaying a moderate exceptional impact with a self warranty c programming language that doesn't pass zero, indicating statistical importance. The heterogeneity on this subgroup is extremely immoderate (I² = 93.85%), pointing to considerable versions within the studies covered on this subgroup. Factors along with the kind of statin used, the duration of treatment, or affected individual traits might also make contributions to this variability. In Subgroup BB, which includes fewer studies, the pooled impact length is 0.79 (95% CI: 0.51 to 1.02), indicating a smaller effect, despite the fact that the self assurance c language although does now not move 0. The heterogeneity in this subgroup is decrease (I² = 0.00%), suggesting that there's much less variability among studies on this group. Despite this, the statistical significance of the variations among the two subgroups is confirmed with the aid of using the Q-statistic (102.06) with a p-rate of 0.000, indicating that the located variant [34].
|
Meta-analysis model |
||
|
Effect size |
0.88 |
|
|
Standard Error |
0.06 |
|
|
Confidence interval LL |
0.73 |
|
|
Confidence interval UL |
1.02 |
|
|
Prediction interval LL |
0.73 |
|
|
Prediction interval UL |
1.02 |
|
|
Number of incl. subjects |
129797 |
|
|
Number of subgroups |
2 |
|
|
Analysis of variance |
||
|
Between / Model (Q*) |
0.20 |
|
|
Between / Model (Df) |
1 |
|
|
Between / Model (P) |
0.651 |
|
|
Within / Residual (Q*) |
3.30 |
|
|
Within / Residual (Df) |
8 |
|
|
Within / Residual (P) |
0.914 |
|
|
Total (Q*) |
3.51 |
|
|
Total (Df) |
9 |
|
|
Total (P) |
0.941 |
|
|
Pseudo R2 |
5.84% |
|
Table 7: Information related to Sub-group analysis.
3.8 Narrative analysis: The systematic review and meta-evaluation incorporated data from 10 studies investigating the consequences of excessive-dose statin therapy on MACE in diabetic patients. These studies included a range of patient demographics, statin kinds, and dosages, in addition to specific techniques for measuring cardiovascular consequences. The number one effects analyzed had been the incidence of MACE (e.G., myocardial infarction, ischemic stroke, and cardiovascular loss of life) and the improvement of NODM. Despite variability in observe designs and patient populations, the overall effects continuously indicate a mild fine impact of excessive-dose statins in reducing cardiovascular occasions on this high-risk population.
3.9 Effectiveness of High-Dose Statin Therapy in Reducing MACE: This systematic review and meta-analysis included studies assessing the effect of excessive-dose statin remedy on MACE, which includes myocardial infarction, ischemic stroke, and cardiovascular loss of life, in diabetic sufferers. The pooled outcomes reveal a mild high-quality impact of excessive-dose statins, with an normal effect length of 0.88. Most of the research covered in the evaluation, which includes Takahashi et al. [22] and Poorhosseini et al. [21], continually observed that excessive-dose statins extensively reduce cardiovascular risks in high-risk diabetic patients. Statins like atorvastatin and rosuvastatin, at higher doses, were specifically effective in lowering the prevalence of MACE, confirming the ability gain of statins in stopping cardiovascular complications in this populace.
4.0 Impact of High-Dose Statins on NODM: While excessive-dose statins have been powerful in lowering MACE, numerous studies, which includes Choi et al. [24] and Lee et al. [29], also highlighted a potential risk of NODM with higher statin doses. The findings suggest that although statins efficiently reduce cardiovascular events, their use may also growth the probability of developing NODM, particularly with rosuvastatin. The pooled effect length shows a mild risk of developing diabetes in patients on high-dose statin therapy. These final results underline the need for cautious monitoring of glucose levels in diabetic patients, in addition to the importance of balancing the benefits of statin therapy with the potential metabolic side effects.
4.1 Clinical Implications of Statin Therapy in Diabetic Populations: The effects of this meta-analysis have enormous clinical implications, in particular for diabetic sufferers at high cardiovascular risk. The findings assist the use of excessive-dose statin therapy as an effective intervention for decreasing MACE in this high-risk population. However, healthcare companies have to keep in mind the capability change-off among cardiovascular safety and the elevated risk of developing diabetes. The evidence shows that tailor-made treatment methods, including often monitoring glucose levels and adjusting statin dosage, can be critical to minimizing the threat of NODM whilst optimizing cardiovascular benefits.
5. Discussion
This systematic overview and meta-analysis tested the consequences of high-dose statin remedy on lowering MACE in diabetic patients. The pooled effect length indicates a mild tremendous impact of high-dose statins in preventing cardiovascular occasions, regular with findings from studies like Takahashi et al. [22] and Poorhosseini et al. [21]. This research mentioned giant discounts in MACE with excessive-dose statins, particularly atorvastatin and rosuvastatin, in high-risk diabetic populations. The beneficial cardiovascular consequences of excessive-dose statins determined on this review are in step with previous literature and help the clinical use of excessive-intensity statins for lowering cardiovascular events in diabetic patients.
However, a huge challenge highlighted in this evaluation is the improved threat of NODM associated with excessive-dose statins. This locating is constant with several research, along with Choi et al. [24] and Lee et al. [29], which stated a higher occurrence of NODM with excessive-depth statins. The accelerated hazard of NODM has been properly-documented inside the literature, noting that statins can impair insulin sensitivity and boom blood glucose tiers, particularly in people with other threat factors for diabetes [35]. This twin impact of statins—decreasing cardiovascular hazard even as increasing the likelihood of diabetes—indicates the want for cautious affected person tracking, mainly concerning glucose metabolism [36].
The findings of this meta-evaluation also underscore the heterogeneity discovered throughout studies, suggesting that various factors, together with statin kind, dose, patient demographics, and comorbid conditions, probable contribute to the variability in outcomes. Studies have shown comparable variability within the advantages of statins, highlighting the importance of tailoring statin therapy to person patient characteristics to optimize each cardiovascular and metabolic results [37]. This version reinforces the significance of thinking about a personalized method when prescribing high-dose statins to diabetic sufferers, taking into consideration both cardiovascular danger and potential metabolic side outcomes.
Comparing our findings with medical tips, such as those from the American College of Cardiology (ACC) and American Heart Association (AHA), which advocate excessive-depth statins for high-threat patients, our consequences align with the current clinical recommendations for diabetic sufferers at risk of cardiovascular events [38]. However, our evaluate additionally emphasizes the need for clinicians to stability the cardiovascular advantages of statins with the capability hazard of NODM. This reinforces the want for affected person monitoring, consisting of glucose stages, and adjusting statin therapy while necessary to avoid unfavorable metabolic consequences.
6. Limitations
Despite the precious insights furnished with the aid of this systematic review and meta-evaluation, numerous limitations must be taken into consideration while deciphering the findings. Firstly, the research covered inside the analysis exhibited big heterogeneity in phrases of observe designs, patient populations, statin sorts, and dosages, which may additionally make contributions to variability within the impact sizes discovered. While a random-effects version become employed to account for this variability, the excessive I² statistic shows that elements consisting of statin type, treatment length, and baseline chance profiles probably have an effect on the outcomes. This variability may restrict the generalizability of the findings across different patient agencies. Additionally, the chance of bias in a few studies, specifically people with retrospective designs, may want to impact the validity of the consequences. The reliance on observational research, a lot of which had limited facts on confounders, further complicates the interpretation of causality among statin therapy and cardiovascular effects. Another problem is the lack of distinctive data on long-term effects and the effect of statins on NODM across numerous populations. This evaluate commonly focuses on quick- to medium-time period outcomes, and extra vast observe-up research are needed to better understand the lasting consequences of excessive-dose statin therapy in diabetic patients.
7. Future Research
Given the findings of this systematic evaluation and meta-analysis, future studies must awareness on addressing the dual impact of excessive-dose statins on cardiovascular effects and the hazard of NODM. While the beneficial outcomes of statins in decreasing MACE are well hooked up, the improved threat of NODM warrants further research into the long-time period metabolic outcomes of statin remedy in diabetic patients. Future research should intention to discover the most efficient dosing regimen for statins, specially in populations at excessive threat of growing diabetes. Research investigating the comparative effectiveness of various statins, such as atorvastatin and rosuvastatin, on both cardiovascular consequences and diabetes hazard could offer valuable insights into tailoring therapy for character sufferers. Additionally, research could attention on adjunctive treatment options to mitigate the hazard of NODM, including the use of glucose-reducing retailers in combination with statin therapy. Further RCTs with large pattern sizes and longer follow-up periods are needed to assess the lengthy-term protection and efficacy of excessive-dose statins in diabetic sufferers. Additionally, subgroup analyses specializing in specific populations, inclusive of people with prediabetes or older sufferers, may assist to higher understand the range in treatment results. Ultimately, future research should are looking for to refine tips for statin remedy in diabetic sufferers, ensuring each cardiovascular protection and metabolic protection.
8. Conclusions
This systematic review and meta -analysis provides strong evidence that supports the effectiveness of high -stable statin therapy to reduce MACA on patients with diabetes. The size of the overall effect indicates that high -color statin reduces the risk of heart deposits in this high -risk population. These results confirm the clinical use of high-intensity statin, such as atorvastatin and rosuvastatin, to prevent cardiovascular complications in diabetic patients, which have the increasing risk of heart disease. However, the potential risk of NODM related to high-dose statin is an important idea. Our findings suggest that although statin provides sufficient heart benefits, they also increase the chances of developing NODM. This double effect requires a careful, individual approach to treatment, where health professionals balance the cardiovascular benefits of statin with potential metabolic risks. The high difference seen in studies indicates that factors such as state types, doses, patient demographics and co-intelligence can contribute to variation in the results. Future research should focus on determining the optimal statin therapy regime for patients with diabetes, considering both cardiovascular risks. Treatment requires subordinate analysis and long-term random controlled tests to limit the guidelines and ensure that the benefits of statin are above potential risks, and finally strengthen the safety and effectiveness of statin therapy for patients with diabetes.
References
- Giugliano D, Maiorino MI, Bellastella G, Chiodini P, Esposito K. Glycemic control, preexisting cardiovascular disease, and risk of major cardiovascular events in patients with type 2 diabetes mellitus: systematic review with meta-analysis of cardiovascular outcome trials and intensive glucose control trials. J Am Heart Assoc 8 (2019): e012356.
- Lin FJ, Tseng WK, Yin WH, Yeh HI, Chen JW, et.al. Residual risk factors to predict major adverse cardiovascular events in atherosclerotic cardiovascular disease patients with and without diabetes mellitus. Sci Rep 7 (2017): 9179.
- Ramos R, Comas-Cufí M, Martí-Lluch R, Elisabeth Balló, Anna Ponjoan, et al. Statins for primary prevention of cardiovascular events and mortality in old and very old adults with and without type 2 diabetes: retrospective cohort study. BMJ 362 (2018): k3359.
- Crandall JP, Mather K, Rajpathak SN, Ronald B G, Karol W et al. Statin use and risk of developing diabetes: results from the Diabetes Prevention Program. BMJ Open Diabetes Res Care 5 (2017): e000438.
- Sasso FC, Lascar N, Ascione A, Ornella C, Luca De Nicola, et al. Moderate-intensity statin therapy seems ineffective in primary cardiovascular prevention in patients with type 2 diabetes complicated by nephropathy: a multicenter prospective 8 years follow up study. Cardiovasc Diabetol 15 (2016): 147.
- Perez-Calahorra S, Laclaustra M, Marco-Benedi V,Xavier Pinto, Rosa M Sanchez-Hernandez, et al. Comparative efficacy between atorvastatin and rosuvastatin in the prevention of cardiovascular disease recurrence. Lipids Health Dis 18 (2019): 216.
- Alajous S, Budhiraja P. New-onset diabetes mellitus after kidney transplantation. J Clin Med 13 (2024): 1928.
- Guber K, Pemmasani G, Malik A, Aronow WS, Yandrapalli S, et.al. Statins and higher diabetes mellitus risk: incidence, proposed mechanisms, and clinical implications. Curr Opin Cardiol 29 (2021): 314-322.
- Leibowitz M, Karpati T, Cohen-Stavi CJ, Becca S Feldman, Moshe Hoshen, et al. Association between achieved low-density lipoprotein levels and major adverse cardiac events in patients with stable ischemic heart disease taking statin treatment. JAMA Intern Med 176 (2016): 1105-1113.
- Xiao Y, He S, Zhang Z, Hongjian Feng,Sini Cui, et al. Effect of high-dose statin pretreatment for myocardial perfusion in patients receiving percutaneous coronary intervention: a meta-analysis of 15 randomized studies. Med Sci Monit 24 (2018): 9166.
- Galal H, Nammas W, Samir A. Impact of high dose versus low dose atorvastatin on contrast induced nephropathy in diabetic patients with acute coronary syndrome undergoing early percutaneous coronary intervention. Egypt Heart J 67 (2015): 329-336.
- Mach F, Ray KK, Wiklund O, Alberto C, Alberico L C, et al. Adverse effects of statin therapy: perception vs. the evidence—focus on glucose homeostasis, cognitive, renal and hepatic function, haemorrhagic stroke and cataract. Eur Heart J 39 (2018): 2526-2539.
- Adhyaru BB, Jacobson TA. Safety and efficacy of statin therapy. Nat Rev Cardiol 15 (2018): 757-769.
- Vavlukis M, Kedev S. Effects of high intensity statin therapy in the treatment of diabetic dyslipidemia in patients with coronary artery disease. Curr Pharm Des 24 (2018): 427-441.
- Morgan CL, Durand A, McCormack T, Hughes E, Berni TR, et.al. Risk of major adverse cardiovascular events associated with elevated low-density lipoprotein cholesterol in a population with atherosclerotic cardiovascular disease with and without type 2 diabetes: a UK database analysis. BMJ Open 13 (2023): e064541.
- Azemawah V, Movahed MR, Centuori P, Ryan P, P L Riel,et al. State of the art comprehensive review of individual statins, their differences, pharmacology, and clinical implications. Cardiovasc Drugs Ther 33 (2019): 625-639.
- Bibbins-Domingo K, Grossman DC, Curry SJ, K W Davidson, J W Epling Jr, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA 316 (2016): 1997-2007.
- Minozzi S, Cinquini M, Gianola S, Gonzalez-Lorenzo M, Banzi R. The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. J Clin Epidemiol 126 (2020): 37- 44.
- Carra MC, Romandini P, Romandini M. Risk of bias evaluation of cross-sectional studies: adaptation of the Newcastle-Ottawa Scale. J Periodontal Res (2025).
- Simmonds M. Quantifying the risk of error when interpreting funnel plots. Syst Rev 4 (2015): 24.
- Poorhosseini H, Tavolinejad H, Aminorroaya A, Hamidreza S, Ozra A, et al. Association of statins for secondary prevention with progression to diabetes in patients with prediabetic state after coronary artery bypass graft surgery: a retrospective cohort study. J Diabetes Complications 34 (2020): 107713.
- Takahashi N, Dohi T, Funamizu T, Hirohisa E, Hideki W, et al. Prognostic impact of lipoprotein(a) on long-term clinical outcomes in diabetic patients on statin treatment after percutaneous coronary intervention. J Cardiol 76 (2020): 25-29.
- Thongtang N, Piyapromdee J, Tangkittikasem N, Kittichai S, N Srikanchanawat, et al. Efficacy and safety of switching from low-dose statin to high-intensity statin for primary prevention in type 2 diabetes: a randomized controlled trial. Diabetes Metab Syndr Obes (2020): 423-431.
- Choi JY, Choi CU, Choi BG, Y Park, D O Kang, et al. New onset diabetes mellitus and cardiovascular events in Korean patients with acute myocardial infarction receiving high-intensity statins. BMC Pharmacol Toxicol 22 (2021): 11.
- Kim JY, Choi J, Kim SG, Kim NH. Relative contributions of statin intensity, achieved low-density lipoprotein cholesterol level, and statin therapy duration to cardiovascular risk reduction in patients with type 2 diabetes: population based cohort study. Cardiovasc Diabetol 21 (2022): 28.
- Kim JY, Choi J, Kim SG, Kim NH. Comparison of on-statin lipid and lipoprotein levels for the prediction of first cardiovascular event in type 2 diabetes mellitus. Diabetes Metab J 47 (2023): 837-845.
- Steenhuis D, de Vos S, Bos JH, Hak E. Risk factors for drug-treated major adverse cardio-cerebrovascular events in patients on primary preventive statin therapy: a retrospective cohort study. Prev Med Rep 34 (2023): 102258.
- Wu Q, He X, Tong X, Li Y, Wang X. Impact of diabetes mellitus and HBV infection on major adverse cardiovascular events related to statin use in the Chinese population with cardiovascular disease. medRxiv (2024): 24316797.
- Lee J, Choi JY, Choi BG, Choi YJ, Park S, et al. Different diabetogenic effect of statins according to intensity and dose in patients with acute myocardial infarction: a nationwide cohort study. Sci Rep 14 (2024): 19438.
- Shah N, Lan Z, Brown CJ, Martin SS, Turchin A. Impact of statin nonacceptance on cardiovascular outcomes in patients with diabetes. J Am Heart Assoc 14 (2025): e040464.
- Sarkar S, Baidya DK. Meta-analysis—interpretation of forest plots: a wood for the trees. Indian J Anaesth 69 (2025): 147-152.
- Sedgwick P. How to read a forest plot in a meta-analysis. BMJ 351 (2015): h4028.
- Richardson M, Garner P, Donegan S. Interpretation of subgroup analyses in systematic reviews: a tutorial. J Clin Epidemiol Glob Health 7 (2019): 192-198.
- Cheng C, Lau Y-C, Chan L, Luk JW. Prevalence of social media addiction across 32 nations: meta-analysis with subgroup analysis of classification schemes and cultural values. Addict Behav 117 (2021): 106845.
- Agouridis AP, Kostapanos MS, Elisaf MS. Statins and their increased risk of inducing diabetes. Expert Opin Drug Saf 14 (2015): 1835-1844.
- Sattar N. Statins and diabetes: what are the connections? Best Pract Res Clin Endocrinol Metab 37 (2023): 101749.
- Wazir M, Olanrewaju OA, Yahya M, J Kumari, Narendar K, et al. Lipid disorders and cardiovascular risk: a comprehensive analysis of current perspectives. Cureus 15 (2023): e51395.
- Arnett DK, Blumenthal RS, Albert MA, Albert MA, Buroker AB, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 74 (2019): e177-e232.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 