Understanding Fundamentals of Electrophysiology and Wide Complex Tachycardia through a Case Report
Nayanjyoti Kaushik1*, Deobrat C Mallick2, Prabhat Singh3
1CHI Health Nebraska Heart Institute, Lincoln, Nebraska, USA
2Department of Internal Medicine, Christus Spohn Hospital, Corpus Christi, Texas, USA
3Department of Nephrology, Kidney Specialist of South Texas, Corpus Christi, Texas, USA
*Corresponding author: Nayanjyoti Kaushik, CHI Health Nebraska Heart Institute, Lincoln, Nebraska, USA.
Received: 04 December 2024; Accepted: 12 December 2024; Published: 24 December 2024
Article Information
Citation: Nayanjyoti Kaushik, Prabhat Singh, Deobrat C Mallick. Understanding Fundamentals of Electrophysiology and Wide Complex Tachycardia through a Case Report. Cardiology and Cardiovascular Medicine. 8 (2024): 515-520.
View / Download Pdf Share at FacebookAbstract
Wide complex tachycardia (WCT) is common clinical condition seen in Emergency Department (ED), post cardiac surgery patient, coronary care or intensive care unit posing diagnostic challenge to physician. While there are several arrhythmias that can manifest as WCT, in one extreme of this spectrum there are potentially life threatening and hemodynamically unstable arrhythmia like Ventricular Tachycardia (VT) versus non lethal Supraventricular tachycardia, or other medical causes such as electrolyte imbalance, acid-base and metabolic disorders. An accurate diagnosis and appropriate arrhythmia management is critical for effective therapy and good outcome. WCT is a rhythm with a rate of more than 100 beats/min and a QRS duration of more than 120 milliseconds [1].
In this case report we seek to describe a patient presenting with WCT and subsequent methodical approach to diagnosis illustrating few common fundamental electrophysiology concepts.
Keywords
<p>Ventricular tachycardia; Wide complex tachycardia; Supraventricular tachycardia; Aberrant conduction; Coumel’s law; Orthodromic reciprocating tachycardia; Accessory pathway; Arrhythmia; Ablation</p>
Article Details
1. Introduction
Wide complex tachycardia (WCT) is common clinical condition seen in Emergency Department (ED), post cardiac surgery patient, coronary care or intensive care unit posing diagnostic challenge to physician. While there are several arrhythmias that can manifest as WCT, in one extreme of this spectrum there are potentially life threatening and hemodynamically unstable arrhythmia like Ventricular Tachycardia (VT) versus non-lethal Supraventricular tachycardia, or other medical causes such as electrolyte imbalance, acid-base and metabolic disorders. An accurate diagnosis and appropriate arrhythmia management is critical for effective therapy and good outcome. WCT is a rhythm with a rate of more than 100 beats/min and a QRS duration of more than 120 milliseconds [1].
In this case report we seek to describe a patient presenting with WCT and subsequent methodical approach to diagnosis illustrating few common fundamental electrophysiology concepts.
2. Case Report
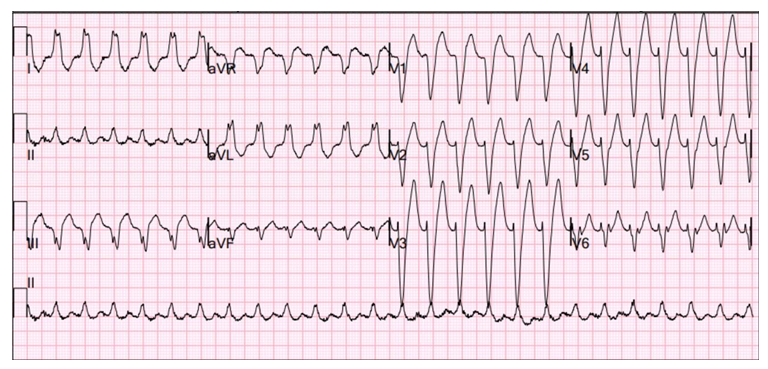
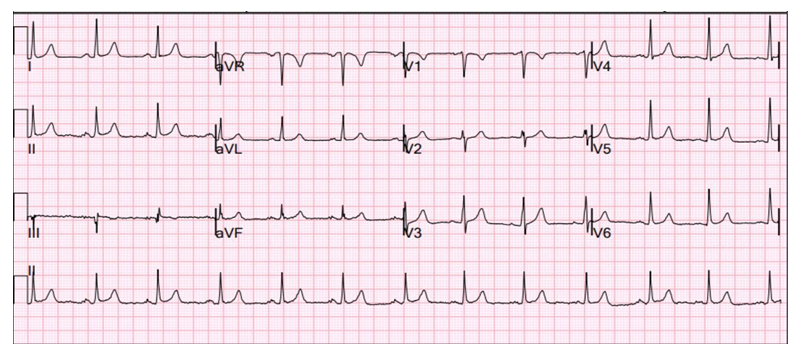
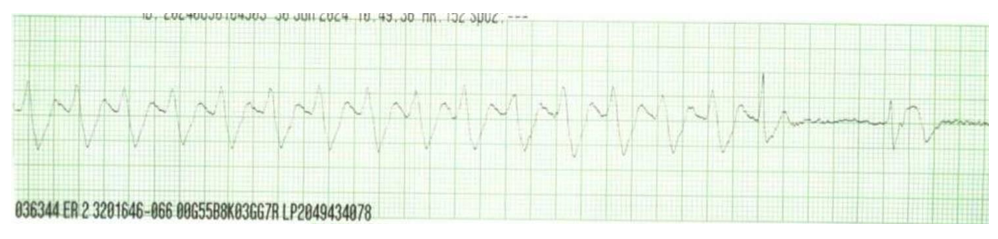
62 year gentleman with past medical history of Essential Hypertension, Benign Prostate Hyperplasia has been experiencing abrupt onset and termination of palpitation and chest discomfort lasting for 10-15 minutes, symptoms occur 1-2 times per week. He has required 3 emergency room visits for same symptoms over a 4-6 week period. His home medications include amlodipine Lisinopril, Tamsulosin. No known prior history of myocardial infarction, heart failure, cardiac arrest or need for cardiopulmonary resuscitation. No family history of sudden cardiac death, cardiomyopathy, premature coronary artery disease. During initial ED visit ECG showed wide complex tachycardia (Figure 1). On physical examination, he was awake and alert during the arrhythmia, Blood pressure 122/94 mm Hg, Heart rate 160 bpm, cardiac auscultation revealed normal heart sound, no murmur, rub or gallop, lung auscultation showed normal breath sound with no crepitation or wheezing, abdomen was soft and non tender, no lump, Neurological examination showed no focal deficit, extremities showed no edema, palpable peripheral pulses, skin warm to touch. Laboratory work up with complete blood count and comprehensive metabolic panel was normal, 3 sets of high sensitivity troponin were negative, baseline ECG during sinus rhythm is shown below (Figure 2) which showed no myocardial ischemic changes, and Left bundle branch block seen during tachycardia resolved during sinus rhythm, Chest X Ray normal, no cardiomegaly or pulmonary vascular congestion. Trans thoracic echocardiogram showed structurally normal heart with normal Left ventricular ejection fraction 60%, mild concentric Left ventricular hypertrophy consistent with history of essential hypertension, no segmental wall motion abnormality, no congenital heart disease particularly Ebstein anomaly, no gross valvular heart disease. Following Differential diagnoses for hemodynamically stable regular monomorphic wide complex tachycardia in a patient with structurally normal heart were considered: Ventricular tachycardia, Supraventricular tachycardia with aberrant conduction, Atrial Flutter with aberrant conduction. Carotid sinus massage was unsuccessful. He initially received intravenous Amiodarone 150 mg bolus in ED for wide complex tachycardia which failed to terminate tachycardia. Next, he was given intravenous adenosine by Cardiologist which terminated tachycardia converting tachycardia into sinus rhythm (Figure 3). He was started on Metoprolol succinate 50 mg daily for symptomatic tachycardia after first emergency room visit despite which he continued to have recurrent episodes requiring 2 more subsequent emergency room visits within next
month, each visit showed exactly similar morphology tachycardia in 12 lead ECG.
Figure 3: Telemetry strip showing termination of tachycardia during Adenosine administration. There is resolution of Left Bundle Branch aberration in the last QRS (narrow) complex of the tachycardia followed by immediate termination of tachycardia with conversion into sinus rhythm. Atrial Flutter or Atrial tachycardia with aberrant conduction as a differential diagnosis of the WCT was ruled out because one would have expected to see Atrial Flutter waves during transient AV block with Adenosine administration. Transient adenosine induced AV block allowed Left Bundle Branch to recover conduction and resolution of rate related Left Bundle Aberration. Because of this, the tachycardia circuit became shorter (as will be explained in detail in the following text) and the Concealed Accessory Pathway was refractory to conduct retrograde thus terminating the tachycardia. Based on this telemetry strip observation we postulated that the patient's wide complex tachycardia is Orthodromic Reciprocating Tachycardia with Left Bundle Branch Aberration with participation of Left Free Wall concealed Accessory Pathway.
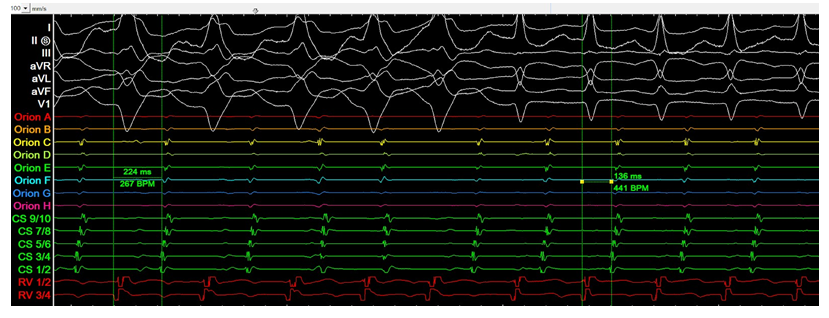
As patient was having recurrent symptoms requiring multiple emergency room visits despite being on Metoprolol succinate, he underwent a comprehensive Electrophysiology (EP) study (Figure 4).
Figure 4: During EP study patient developed exactly similar morphology WCT (surface ECG leads at sweep speed of 100 mm/s shown at top panel in white color) seen clinically which spontaneously converted into narrow complex tachycardia. Decapolar coronary sinus catheter electrograms (Green color) are arranged in order as proximal pair being 9/10, and distal pair being 1/2, Right Ventricular Apex quadripolar catheter is shown in red color. As we can see the activation pattern in Coronary sinus catheter is eccentric with distal to proximal activation sequence indicating conduction over a Left free wall accessory pathway thus earliest local atrial activation in the mitral isthmus region of Left atrium and then spreading to coronary sinus osmium. During retrograde VA conduction over AV node, activation sequence is concentric i.e. proximal to distal activation sequence in CS catheter. A key observation is longer VA interval (measured from beginning of earliest QRS in surface ECG to earliest local atrial electrogram in CS catheter) during WCT (224 ms) compared to VA interval during narrow complex tachycardia (136 ms), and TCL
is longer during WCT compared to shorter TCL or acceleration of tachycardia during narrow complex tachycardia.
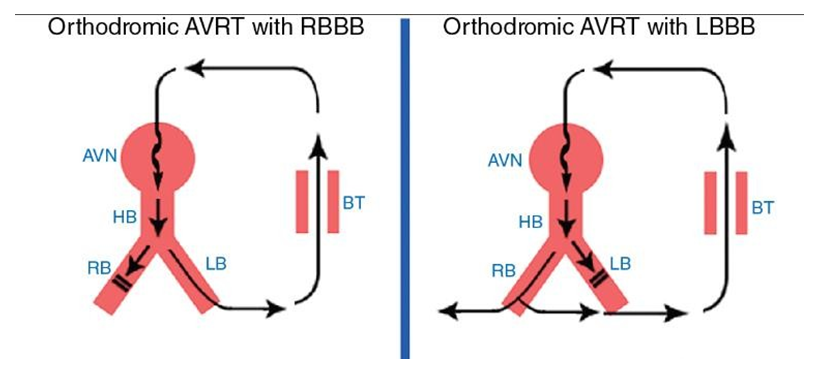
Figure 5: Coumel’s law. Left panel shows the ORT circuit which includes atrium, AVN, His Bundle, LBB, Ventricle, Bypass tract. Right panel shows development of LBBB during ORT when tachycardia circuit includes atrium, AVN, His Bundle, RBBB, Ventricle and Bypass Tract which makes the tachycardia circuit longer thus slowing the tachycardia.
After comprehensive EPS, WCT was diagnosed as ORT with LBBB Aberration with a participating Left Free Wall AP. Successful Radiofrequency ablation was performed for the AP. During follow up office visits, patient has been doing well with resolution of pre ablation symptoms, successfully discontinued Metoprolol Succinate, no recurrence of arrhythmia, and no procedural complication.
2.1 Pathophysiology:
Under normal circumstances, ventricular depolarization occurs through the efficient rapidly conducting Atrio-ventricular node-His Purkinje conduction system (AVN-HPS) followed by synchronous electrical activation of Right Ventricle (RV) and Left Ventricle (LV) via Right Bundle Branch (RBB) and Left Bundle Branch (LBB) respectively resulting in narrow QRS. On the other hand during conduction through myocardium (cell to cell depolarization) during VT, pre excitation of ventricles bypassing the normal AVN-HPS via Bypass Tract (BT), underlying Bundle Branch Block (BBB) or Aberrantion, various anti-arrhythmic agents specially Class IC drugs (e.g. Flecainide, Propafenone), Ventricular pacing, Electrolyte abnormalities etc is propagation of activation wavefront is inefficient, resulting in electrical dyssynchrony and Wide QRS complex.
|
Causes of WCT |
Example |
|
VT |
Myocardial VT |
|
Focal/Triggered VT e.g. Idiopathic outflow tract VT, Papillary muscle VT |
|
|
Macro Re entrant VT e.g. Scar related re entrant VT in patient with prior MI/CAD, Bundle Branch Re-entrant VT in Dilated Cardiomyopathy |
|
|
Epicardial VT in nonischemic cardiomyopathy (e.g. Sarcoidosis, ARVC) Inherited channelopathies e.g. Brugada syndrome, CPVT, LQT etc (usually polymorphic) |
|
|
SVT with Aberrancy |
Functional/Rate related Aberration Pre existing BBB/IVCD |
|
Pre-excited SVT |
Antidromic Atrio Ventricular reciprocating Tachycardia Atrial Fibrillation with Prexcitation |
|
SVT (AT/AVNRT) with bystander BT |
|
|
Antiarrhyth mic Drugs |
Class IA and IC Antiarrhythmic (e.g. Flecainide, propafenone), Amiodarone |
|
Digitalis toxicity (Bidirectional VT) |
|
|
Electrolyte Abnormality |
Hyperkalemia |
|
Ventricular pacing |
Table 1: Causes of Wide Complex tachycardia.
2.2 Rate related Aberration:
The term aberrant conduction is used for transient functional block in conduction in the absence of persistent bundle branch block, prexcitation, drug effect etc. Rate related aberration can be tachycardia dependent or Bradycardia dependent:
Acceleration or Tachycardia Dependent or Phase 3 block or Voltage Dependent block: This occurs when a premature impulse occurs during phase 3 of action potential when tissue is still refractory due to incomplete repolarization[1]. Acceleration dependent aberration is often seen when a Premature Atrial Complex (PAC) occurs early enough when AVN and His Bundle are still partially refractory and PAC conducts with RBBB type aberration. Another example of acceleration dependent aberration is seen during Atrial Fibrillation (Ashman Phenomenon) with a long short sequence. Usually preceding RR interval predicts the refractory period of HPS during next cycle. Due to irregular RR interval during Atrial Fibrillation, if a short RR interval immediately follow a long RR interval (Long short sequence), due to long refractory period of HPS created by preceding long RR interval, next conducted supra ventricular complex (short RR interval) conducts aberrantly because the bundle branches are still refractory. Tachycardia dependent aberration can also be seen at a faster atrial rate beyond which ERP of one of the bundle branches fails to shorten any further. During normal heart rate, aberration is seen mostly in RBBB pattern because ERP of RBB is long during normal heart rate, while at faster heart rate it is in the form of LBBB as Effective refractory period (ERP) of RBB is shortens to a greater degree compared to LBB at faster heart rate. Importantly, acceleration-dependent aberration is a marker of a diseased HPS when it appears at relatively slow heart rates (less than 70 beats/min); displays LBBB or appears with gradual rather than abrupt acceleration of the heart rate.
Bradycardia or Pause Dependent of Phase 4 block: During phase 4 of action potential, cardiac pacemaker cells have the natural ability to slowly depolarize, a property which is not seen in HPS cells at heart rate usually faster than 40/min. But under pathological states such as increased automaticity or injured myocardial tissue, these cells may start depolarizing slowly during phase 4 making resting membrane potential less negative causing inactivation of some Na channels. If a stimulus is delivered early enough immediately after reploarization, there will still be enough Na channels available to generate a steeper Phase 0 of AP and hence an increased conduction velocity, but if the stimulus arrives late after a pause (eg a compensatory pause after a PVC or a PAC) or slow HR, when due to phase 4 depolarization resting membrane potential is less negative resulting in reduced availability of Na channels, generated AP may not be enough to allow conduction. Phase 4 block almost always manifest in the form of LBBB [1], not commonly seen in normal myocardial tissue and perceived as pathological when seen.
2.3 Approach to Wide QRS tachycardia:
Various algorithms have been described to diagnose Ventricular tachycardia with variable sensitivity and specificity such as Brugada [2], Griffith [3], Vereckei [4] etc. We will keep this discussion limited to the relevance of our case.
Findings such as AV dissociation with ventricular rate faster than atrial rate, captured or fusion beat if seen are specific for VT. However, these are not always visible in the ECG, and under these circumstances morphology criteria have been applied. If there is BBB seen during tachycardia, it is extremely important to distinguish between SVT with underlying BBB or aberrant conduction versus VT to guide further management and predict prognosis. If BBB is present in baseline ECG during sinus rhythm, it provides significant clue because if contralateral bundle branch block pattern is seen during tachycardia this strongly favors VT. If there is no baseline BBB during sinus rhythm, BBB seen during tachycardia may be SVT with aberration or VT. Usually SVT with aberrant conduction should give either a typical RBBB or Typical LBBB pattern. Typical LBBB manifests an rS or QS wave in leads V1 and V2, delay to S wave nadir less than 70 milliseconds, and R wave and no Q wave in lead V6 [1,3]. Typical RBBB manifests an rSR' wave in lead V1 and an RS wave in lead V6, with R wave height greater than S wave depth [1-3].
2.4 Bundle Branch Block during Orthodromic Reciprocating tachycardia:
Development of functional bundle branch block during orthodromic reciprocating tachycardia (ORT) with slowing of tachycardia rate indicates presence and participation of BT ipsilateral to the BBB. This classic phenomenon is commonly known as Coumel’s law [5]. Antegrade limb of ORT circuit includes antegrade conduction from atrium over the AV node-His Bundle- Right and Left bundle branches to the ventricles and retrograde limb is the BT. If there is functional BBB ipsilateral to the BT (LBBB for a left free wall BT, RBBB for Right free wall BT), this makes the tachycardia circuit longer. For example, if there is a left free wall BT and there is functional LBBB during ORT, antegrade conduction will be from Atrium, AVN-His through the RBBB (due to functional LBBB) to RV and then transeptal from RV to LV followed by retrograde conduction over the BT. Due to long circuit, tachycardia cycle length will be longer. In surface ECG this will be seen as narrow complex tachycardia transitioning to a wide complex tachycardia (due to functional BBB) with a slower rate due to longer tachycardia circuit. This is more noticeable in free wall AP compared to posteroseptal pathway.
Initiation of ORT requires sufficient delay to allow the bypass tract to recover from its refractory period to be able to conduct retrograde. This delay is sometimes seen in the AV node when there is dual AV nodal physiology present. When a premature atrial complex arrives at the AV node and fast pathway is refractory, it conducts over the slow pathway with a long AH interval. This delay allows the BT to recover excitability from its refractory period and be able to conduct retrograde thus initiating ORT. Similarly, development of functional BBB may provide ideal delay to allow the BT to conduct retrogradely facilitating initiation of ORT.
Paradoxical response to Coumel’s law [6] may be seen in presence of Dual AV node physiology. In this case, Antegrade conduction during narrow complex tachycardia is over slow pathway. During functional BBB, the delay allows fast pathway to recover and antegratd conduction switches from slow pathway to fast pathway. Since conduction over the fast pathway is shorter, during wide complex tachycardia with ipsilateral BBB, tachycardia cycle length may not be longer or remain unchanged compared to narrow complex tachycardia which is inconsistent with coumel’s law.
3. Discussion
This case report highlights several well described foundational concepts of electrophysiology as will be described below in detail particularly mechanism of aberrant conduction, differentiating WCT into VT versus SVT with aberration based on typical BBB morphology versus atypical BBB morphology, observation of effect of bundle branch block during WCT which is a very important diagnostic clue, Coumel’s law etc. Though it may not be always possible to see these findings, fortunately we could see several classic key observations in this case allowing readers to understand these key concepts which will enhance clinical diagnostic ability.
4. Conclusion
This case study elucidates several well established fundamental electrophysiological concepts which are extremely helpful for the clinician to make an accurate diagnosis of WCT confidently and offer appropriate potentially curative treatment to patient ensuring patient safety.
References
- Clinical Arrhythmology and Electrophysiology: A companion to Braunwald's Heart Disease. In: Issa ZF, Miller JM, Zipes DP. 2nd edition (2012).
- Brugada P, Brugada J, Mont L, et al. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation 83 (1991): 1649-1659.
- Jastrzebski M, Kukla P, Czarnecka D, et al. Comparison of five electrocardiographic methods for differentiation of wide QRS-complex tachycardias. Europace 14 (2012): 1165-1171.
- Vereckei A, Duray G, Szénási G, et al. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J 28 (2007): 589-600.
- Coumel P, Attuel P. Reciprocating tachycardia in overt and latent preexcitation. Influence of functional bundle branch block on the rate of the tachycardia. Eur J Cardiol 1 (1974): 423-36.
- Motoyoshi T, Nishiuchi S, Yamagami S, et al. Detailed Mechanism of the Paradoxical Coumel Phenomenon in a Case of Orthodromic Reciprocating Tachycardia. HeartRhythm Case Reports 8 (2024): 288-291.


 Impact Factor: * 5.6
Impact Factor: * 5.6 Acceptance Rate: 74.36%
Acceptance Rate: 74.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 