Evaluating the Therapeutic Value of Low-Intensity Pulsed Ultrasound for Tibial Fracture Management: A Systematic Review of Randomized Controlled Trials
Noman Mansoor1*, Aimen Warsi1, Amna Warsi2, Jahangir Ahmed1, Rishi Ramnani2, Zainab Naseer3, Jawad Ur Rehman3, Marium Zahid1, Naveera Raffat1, Hammad Jabbar1, Syed Haider Ali Warsi3
1Karachi Medical and Dental College, Karachi Metropolitan University, Karachi, Pakistan
2Liaquat National Hospital and Medical College, Karachi, Pakistan
3Jinnah Medical and Dental College, Karachi, Pakistan
*Corresponding Author: Noman Mansoor, Karachi Medical and Dental College, Karachi, Pakistan.
Received: 14 May 2025; Accepted: 20 June 2025; Published: 27 June 2025
Article Information
Citation: Noman Mansoor, Aimen Warsi, Amna Warsi, Jahangir Ahmed, Rishi Ramnani, Zainab Naseer, Jawad Ur Rehman, Marium Zahid, Naveera Raffat, Hammad Jabbar, Syed Haider Ali Warsi. Evaluating the Therapeutic Value of Low-Intensity Pulsed Ultrasound for Tibial Fracture Management: A Systematic Review of Randomized Controlled Trials. Journal of Orthopedics and Sports Medicine. 7 (2025): 281-286.
View / Download Pdf Share at FacebookAbstract
Background: Osteopetrosis is a rare genetic disorder characterized by defective osteoclast function, leading to increased bone density and skeletal fragility. The condition manifests in various forms, ranging from mild adult-onset to severe infantile types, often associated with hematologic, neurological, and growth complications.
Introduction: Osteopetrosis patients will mostly suffer from pathologic fractures and progressive cranial nerve compression neuropathies. There are two sub classifications of autosomal dominant osteopetrosis, and these patients are often asymptomatic in adults.
Objective: To present a comprehensive case report of osteopetrosis, emphasizing its clinical presentation, diagnostic challenges, and therapeutic considerations. Additionally, this study provides a narrative review of the different types of osteopetrosis, their clinical manifestations, and the multidisciplinary approaches involved in their management. We have focused to discuss case analysis, diagnostic challenges, therapeutic insights and role of stem cell transplant.
Results and conclusion: Osteopetrosis is a complex genetic disorder requiring a multidisciplinary approach for effective management due to its wide-ranging complications. Pediatricians play a crucial role in early diagnosis and monitoring growth-related issues, while hematologists manage bone marrow failure and related hematologic abnormalities. Three types of osteopetrosis with different severity degrees of skeletal disorders and pathological severity are explained. BMT markedly improves cases of infantile osteopetrosis. It cures bone marrow failure and metabolic abnormalities in patients. Multidisciplinary team approach is needed for treatment and management of complications.
Keywords
<p>Tibial fractures; Injuries; Long bone; Low-Intensity Pulsed Ultrasound (LIPUS); Healing; Adult patients; Radiographic</p>
Article Details
1. Introduction
Low-Intensity Pulsed Ultrasound (LIPUS) is a therapeutic technique that delivers low-power acoustic waves in short bursts to stimulate healing in musculoskeletal tissues [1]. Unlike traditional ultrasound used for imaging or thermal therapy, LIPUS uses non-thermal mechanical stimulation to influence cellular behavior without causing tissue heating [2]. The therapy has been most commonly used to support fracture healing, particularly in patients with delayed union or non-union of bones [3].
Clinical and preclinical studies have shown that LIPUS can enhance bone regeneration by promoting the activity of bone-forming cells, improving vascular growth, and accelerating mineral deposition [4]. These effects are largely attributed to mechanotransduction—where mechanical forces are converted into biochemical signals inside cells [5]. The ultrasound waves activate receptors on the cell membrane, which then stimulate pathways involved in cell growth, differentiation, and tissue repair [6]. This results in improved cellular organization and tissue remodeling, especially in bone and connective tissues [7]. Devices used for LIPUS are compact and typically require patients to perform daily sessions lasting around 20 minutes, making it feasible for outpatient or home use [8]. Although most evidence supports its use in bone healing, ongoing research is evaluating its potential in soft tissue recovery, dental applications, and even nerve repair [9].
Tibial fractures are among the most frequently encountered long bone injuries in orthopedic practice, largely due to the tibia’s limited soft tissue coverage and its role as a primary weight-bearing bone in the lower extremity [10]. These fractures can result from both high-energy mechanisms, such as road traffic accidents, and low-energy injuries, particularly in individuals with reduced bone mineral density or underlying pathology [11].
Tibial fractures are categorized by their anatomical location—proximal, shaft, or distal—as well as their morphological characteristics, including whether they are open or closed, comminuted, or involve the articular surface [12]. Of these, mid-shaft tibial fractures are especially prone to complications such as delayed union, nonunion, and infection due to the bone’s poor vascular supply and thin soft tissue envelope [13].
Management of tibial fractures typically includes conservative methods like functional bracing for stable, minimally displaced fractures, and surgical interventions—most commonly intramedullary nailing—for unstable or complex injuries [14]. Despite these advancements, a significant proportion of patients still experience impaired healing, necessitating the use of adjunctive treatments to enhance recovery.
One such adjunct is Low-Intensity Pulsed Ultrasound (LIPUS), a non-invasive modality that uses pulsed acoustic waves to stimulate cellular activity and promote bone repair. LIPUS has been shown to accelerate healing in both fresh and nonunion tibial fractures by enhancing angiogenesis, osteoblast differentiation, and extracellular matrix production [15,16]. The technology is particularly beneficial in patients at higher risk for delayed healing, such as smokers, diabetics, or those with open fractures. Clinical studies have demonstrated that daily LIPUS treatment can reduce healing time and improve functional outcomes in tibial shaft fractures [17].
2. Methodology
2.1 Eligibility Criteria
Population: Patients with tibial fractures, including open, comminuted, segmental, or complex fractures.
Intervention: Low-Intensity Pulsed Ultrasound (LIPUS) treatment.
Comparators: Control or sham treatment groups with no LIPUS or dummy devices.
Outcomes: Clinical healing time, radiographic healing (callus formation), bone mineral content, biochemical markers (e.g., bone-specific alkaline phosphatase), complication rates.
Study Types: Randomized controlled trials (RCTs) and prospective cohort studies with adequate control groups.
Exclusion: Simple fractures or fractures in other bones.
Information Sources
- • PubMed
- • Ultrasound in Medicine & Biology journal archives
- • Relevant clinical trial registries and orthopedic databases
2.2 Search Strategy
Keywords: "low-intensity pulsed ultrasound," "LIPUS," "tibial fractures," "fracture healing," "open fractures," "high-energy trauma," "bone healing ultrasound".
Filters: Human studies, English language, publication dates 1990-2025
2.3 Selection Process
- • Titles and abstracts screened by two independent reviewers.
- • Full-text screening for eligibility based on criteria.
- • Discrepancies resolved by consensus or third reviewer.
2.4 Data Collection Process
- • Data extracted independently by two reviewers using standardized forms.
- • Extracted data included patient demographics, fracture characteristics, treatment protocols, clinical and radiological outcomes, biochemical markers, and adverse events.
2.5 Data Items
- • Time to clinical healing (full weight bearing)
- • Time to radiographic callus appearance
- • Bone mineral content changes
- • Plasma bone-specific alkaline phosphatase (ALP) levels
- • Complications and adverse effects
2.6 Study Risk of Bias Assessment
- • RCTs assessed using Cochrane Risk of Bias tool: sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other biases.
- • Non-RCTs assessed with Newcastle-Ottawa Scale.
2.7 Effect Measures
- • Mean difference (weeks) for healing time and callus appearance.
- • Percentage change for bone mineral content and ALP activity.
- • Risk ratios for complications.
2.8 Synthesis Methods
- • Narrative synthesis due to heterogeneity in fracture types and outcome reporting.
- • Descriptive statistics and comparative analysis of mean differences and p-values.
- • No meta-analysis due to limited number of comparable studies.
2.9 Reporting Bias Assessment
- • Search included unpublished and grey literature to minimize publication bias.
- • Funnel plots not feasible due to small number of studies.
2.10 Certainty Assessment
GRADE approach to assess quality of evidence across studies, focusing on risk of bias, consistency, directness, precision, and publication bias.
3. Results
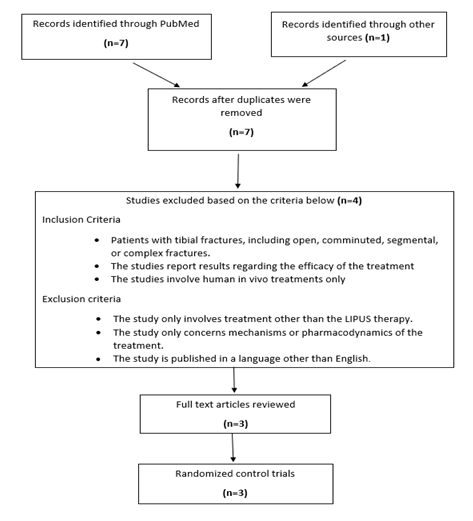
8 articles were found using the methodology outlined above. Of these, 5 records were identified by title, and further narrowed to three records after inclusion criteria were applied and duplicates were removed. Two of the studies were published in the last 3 decades, while one was published in the last decade. All of them were randomized control trials. All of the studies used LIPUS for the treatment of tibial fractures. A total of 591 human subjects were studied (Figure 1).
3.1 Assessing the efficacy of LIPUS in treatment of tibial fractures
Our first study was conducted by Leung et al. [18]. This clinical study evaluated the impact of low-intensity pulsed ultrasound (LIPUS) on the healing process of complex tibial fractures. A total of 30 patients with such fractures were randomly assigned to either the LIPUS treatment group (n = 16) or a control group receiving a sham treatment with a dummy machine (n = 14). Fractures were immobilized using internal or external fixation methods based on clinical needs. Patients in the LIPUS group received daily ultrasound stimulation for 20 minutes over a 90-day period.
Fracture healing was monitored through multiple assessments: clinical examination, radiological imaging, densitometry, and biochemical markers. The results showed that the LIPUS-treated group experienced significantly enhanced fracture healing compared to the control group, as evidenced across all assessment modalities.
Complications were minimal in the LIPUS group. There were two cases of delayed union—one in each group—and two cases of infection, all of which occurred in the control group. Delayed union cases were subsequently managed with LIPUS therapy, and infection cases were treated according to standard protocols before also receiving LIPUS treatment. Ultimately, these patients achieved fracture healing.
This study suggests that LIPUS is a safe and effective adjunctive therapy that can accelerate fracture healing in complex tibial fractures and reduce the incidence of complication.
The study conducted by Kristiansen et al. [19] evaluated the effect of low-intensity pulsed ultrasound (LIPUS) on the healing of dorsally angulated distal radial fractures in 60 patients. Participants were randomly assigned to either an active LIPUS group or a placebo group, with treatments administered daily for 20 minutes over a 10-week period. The primary outcomes measured were the time to clinical and radiographic fracture union, as well as the maintenance of fracture reduction. The results showed that the LIPUS-treated group had a significantly shorter mean time to clinical and radiographic union—61 days compared to 98 days in the placebo group—indicating an accelerated healing process. Additionally, the LIPUS group demonstrated less secondary displacement, with a smaller loss of fracture reduction, suggesting that ultrasound stimulation helped maintain fracture stability during healing. The study concluded that LIPUS is effective in accelerating the healing of distal radial fractures, reducing immobilization time, and potentially improving clinical outcomes by enhancing fracture stability and reducing complications associated with delayed union.
The TRUST trial, a large randomized clinical study involving 501 patients with operatively managed tibial shaft fractures, investigated the effectiveness of low-intensity pulsed ultrasound (LIPUS) therapy in accelerating fracture healing and improving functional recovery. Patients were randomly assigned to receive either active LIPUS or a placebo treatment daily for 20 minutes over 90 days. The study found no significant difference between the LIPUS and placebo groups in terms of time to radiographic healing or physical function measured by the SF-36 Physical Component Summary score. Additionally, safety outcomes were similar across both groups, and patient compliance was moderate, with 73% of patients completing at least half of the recommended treatments. Overall, the trial concluded that LIPUS did not provide a clinically meaningful benefit in healing tibial fractures or enhancing patient function, suggesting it should not be routinely used as an adjunctive therapy in this context.
4. Discussion
Research on the application of LIPUS in the treatment of tibial fracture is still in its early stages and is restricted to a few prospective studies, randomized-controlled trials, and retrospective reviews of medical records. Overall findings from the first two studies examining the effectiveness of the procedure indicate encouraging outcomes and non-inferiority when compared to other interventions.
Low-Intensity Pulsed Ultrasound (LIPUS) was found to be both safe and effective for enhancing bone healing in fracture management. The most common side effect was Mild swelling and erythema (redness) at the application site, which lasted for a few weeks. The results showed that the fracture-healing process was significantly accelerated, which resulted in a significant reduction in the amount of time required to reach each radiographic stage of healing. Additionally, the group treated with active, pulsed low-intensity ultrasound experienced a significant reduction in the loss of reduction during healing. All strata, even those for which longer healing durations are anticipated, showed consistent, rapid healing, according to the study of treatment impact within the patient and fracture-characteristics stratum.
Despite rigorous methodology and comprehensive outcome measures, the study, conducted by Busse et al. [20] found no significant differences between the LIPUS and placebo groups in terms of time to radiographic healing, functional recovery as assessed by SF-36 Physical Component Summary scores, or other functional outcomes. These findings align with previous studies that have questioned the clinical benefits of LIPUS in fracture healing.
The lack of observed benefit in this large-scale trial raises important considerations regarding the clinical application of LIPUS. While LIPUS is a non-invasive and generally well-tolerated modality, its cost-effectiveness and clinical utility in routine practice remain uncertain. The study's robust design and comprehensive data collection provide a high level of evidence that challenges the routine use of LIPUS in tibial fracture management.
Given the negative findings of the TRUST trial, it is imperative for clinicians to critically assess the use of LIPUS in their practice. The decision to employ LIPUS should be based on individual patient circumstances and a thorough evaluation of available evidence. Further research is necessary to identify specific patient populations or fracture types that may benefit from LIPUS therapy.
When LIPUS is utilized in an outpatient setting, patients use the device on their own. Treatment compliance is generally low [21]; this is especially true for treatments that involve the degree of burden or inconvenience associated with LIPUS (for instance, the American College of Chest Physicians Evidence-Based Clinical Practice Guidelines, 9th edition, stated that the biggest obstacle to using outpatient limb compression devices in patients undergoing orthopedic surgery is compliance [22].
Another domain which needs to be evaluated is the cost of the device and the procedure. A study conducted by Tarride et al. [23] conducted an economic evaluation of 501 patients undergoing LIPUS on tibial shaft fractures managed with intramedullary nailing. The study demonstrated that Low-Intensity Pulsed Ultrasound (LIPUS) treatment for tibial fractures resulted in significantly higher costs compared to placebo, with a mean increase of $3,647 from the payer perspective and $3,425 from the societal perspective. However, LIPUS did not yield a statistically significant improvement in quality-adjusted life years (QALYs), with a mean difference of only 0.023 (95% CI: -0.035 to 0.069; p = 0.474). The resulting incremental cost-effectiveness ratios—$155,433/QALY from the payer perspective and $146,006/QALY from the societal perspective—suggested that LIPUS was not a cost-effective intervention for the treatment of tibial fractures.
The heterogeneity of study protocols, sample sizes, follow-up durations, and treatment dosages presents challenges in generalizing the results to broader populations. Future research should focus on large-scale, high-quality randomized controlled trials with standardized treatment protocols, longer follow-up periods. Furthermore, assessing the cost-effectiveness of LIPUS in comparison to alternative treatments would provide valuable insights for clinical decision-making. Despite these limitations, LIPUS remains a promising therapeutic option for tibial fractures, demonstrating notable benefits in the recovery process and functional improvement, warranting further investigation and broader clinical application (Table 1).
Table 1: Summarizing the results of the studies.
Conflict of Interest: None to declare.
Acknowledgements: None to declare.
Funding: None to declare.
References
- Padilla F, Puts R, Vico L, et al. Stimulation of bone repair with ultrasound: A review of the possible mechanic effects. Ultrasound in Medicine and Biology 40 (2014): 1211-1224.
- Duarte LR. The stimulation of bone growth by ultrasound. Archives of Orthopaedic and Traumatic Surgery 101 (1983): 153-159.
- Busse JW, Bhandari M, Kulkarni AV, et al. The effect of low-intensity pulsed ultrasound therapy on time to fracture healing: A meta-analysis. Canadian Medical Association Journal 166 (2002): 437-441.
- Rutten S, Nolte PA, Korstjens CM, et al. Use of low-intensity pulsed ultrasound for post-operative treatment of osteotomies: A prospective randomized double blind placebo-controlled study. Journal of Orthopaedic Research 26 (2008): 1253-1260.
- Claes L, Willie B, Ignatius A. Mechanobiology of fracture healing and non-unions. Current Orthopaedic Practice 23 (2012): 577-583.
- Padilla F, Puts R, Vico L, et al. Stimulation of bone repair with ultrasound: A review of the possible mechanic effects. Ultrasound in Medicine and Biology 40 (2014): 1211-1224.
- Reher P, Doan N, Bradnock B, et al. Therapeutic ultrasound for osteoradionecrosis: An in vitro comparison of 1 MHz and 45 kHz machines. European Journal of Cancer: Part B, Oral Oncology 35 (1999): 307-312.
- Rutten S, Nolte PA, Korstjens CM, et al. Use of low-intensity pulsed ultrasound for post-operative treatment of osteotomies: A prospective randomized double-blind placebo-controlled study. Journal of Orthopaedic Research 26 (2008): 1253-1260.
- Padilla F, Puts R, Vico L, et al. Stimulation of bone repair with ultrasound: A review of the possible mechanic effects. Ultrasound in Medicine and Biology 40 (2014): 1211-1224.
- Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 37 (2006): 691-697.
- Milner SA, Davis TRC, Muir KR, et al. Long-term outcome after tibial shaft fracture: Is malunion important? The Journal of Bone and Joint Surgery - British 84 (2002): 1006-1010.
- AO Foundation. Fracture classification: AO/OTA classification (2020). Retrieved from https://www.aofoundation.org/
- Papakostidis C, Kontakis G, Giannoudis PV. The influence of timing of wound closure on infection rate following open tibial fractures: A systematic review and meta-analysis. Injury 42 (2011): 447-452.
- Bhandari M, Guyatt GH, Tornetta P, et al. Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. The Journal of Bone and Joint Surgery - American 83 (2001): 345-351.
- El-Mowafi H, Mohsen M. The effect of low-intensity pulsed ultrasound on bone healing. The Egyptian Orthopaedic Journal 40 (2005): 53-59.
- Padilla F, Puts R, Vico L, et al. Stimulation of bone repair with ultrasound: A review of the possible mechanic effects. Ultrasound in Medicine and Biology 40 (2014): 1211-1224.
- Busse JW, Bhandari M, Kulkarni AV, et al. The effect of low-intensity pulsed ultrasound therapy on time to fracture healing: A meta-analysis. Canadian Medical Association Journal 166 (2002): 437-441.
- Leung KS, Lee WS, Tsui HF, et al. Complex tibial fracture outcomes following treatment with low-intensity pulsed ultrasound. Ultrasound Med Biol 30 (2004): 389-95.
- Kristiansen TK, Ryaby JP, Mccabe J, et al. Accelerated Healing of Distal Radial Fractures with the Use of Specific, Low-Intensity Ultrasound. A Multicenter, Prospective, Randomized, Double-Blind, Placebo-Controlled Study. The Journal of Bone and Joint Surgery 79 (1997): 961-73.
- TRUST Investigators writing group, Busse JW, Bhandari M, et al. Re-evaluation of low intensity pulsed ultrasound in treatment of tibial fractures (TRUST): randomized clinical trial. BMJ 355 (2016): i5351.
- Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 353 (2005): 487-97.
- Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141 (2012): e278S-e325S.
- Tarride JE, Hopkins RB, Blackhouse G, et al. Low-intensity pulsed ultrasound for treatment of tibial fractures: an economic evaluation of the TRUST study. Bone Joint J 99-B (2017): 1526-1532.
Article Views: 1065
Journal Statistics




Discover More: Recent Articles
Grant Support Articles
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved!