Anatomic Suture Reconstruction of the Acromioclavicular Joint is Noninferior to Traditional Suture Constructs: A Biomechanical Study
Josiah A. Valk DO*, Erik W. Dorthé, Darryl D. D’Lima, MD, PhD, Heinz R. Hoenecke Jr., MD
Scripps Health, Shirley Center for Orthopaedics Research & Education (SCORE) at Scripps Clinic, La Jolla, California, USA
*Corresponding Author: Josiah Valk, Scripps Health, Shirley Center for Orthopaedics Research & Education (SCORE) at Scripps Clinic, La Jolla, California, USA.
Received: 18 June 2025; Accepted: 26 June 2025; Published: 03 July 2025
Article Information
Citation: Josiah A Valk, Erik W Dorthé, Darryl D D’Lima, Heinz R Hoenecke. Anatomic Suture Reconstruction of the Acromioclavicular Joint is Noninferior to Traditional Suture Constructs: A Biomechanical Study. Journal of Orthopedics and Sports Medicine. 7 (2025): 292-298.
View / Download Pdf Share at FacebookAbstract
Background: Acromioclavicular (AC) joint injuries, especially in highgrade cases, can result in persistent instability despite surgical intervention. Traditional reconstructions focus on vertical stability by addressing the coracoclavicular (CC) ligaments but may neglect the horizontal and rotational stability provided by the AC ligament complex.
Purpose: This study evaluates the biomechanical performance of an anatomic suture-based AC ligament reconstruction technique compared to traditional suture constructs.
Methods: Twenty 3D-printed scapula and clavicle models were randomly assigned to four reconstruction techniques: O-frame, X-frame, O + X-frame, and anatomic AC ligament reconstruction. Using a six-axis robotic testing system, superior translation, posterior translation, and both anterior and posterior rotation were cyclically loaded, and stiffness (N or Nm) was recorded.
Results: The anatomic reconstruction demonstrated comparable stiffness to traditional constructs in superior translation, posterior translation, and anterior rotation (p > 0.05). Notably, it exhibited significantly higher stiffness in posterior rotation (0.75 ± 0.36) compared to the X-frame (0.29 ± 0.26) (p = 0.048). All constructs maintained structural integrity throughout cyclic loading, with no anchor pullout or gross failures.
Conclusion: Anatomic suture reconstruction of the AC joint provided equivalent biomechanical stability to traditional constructs in most tested directions and demonstrated superior stiffness in posterior rotation. These findings support the inclusion of anatomic AC ligament suture augmentation to address persistent horizontal and rotational instability, while suggesting that simplified suture-based reconstructions can be biomechanically robust in 3D-printed models.
Keywords
<p>Acromioclavicular joint reconstruction; AC joint; Stabilization; Vertical instability; Horizontal instability; Rotational instability; Suture anchor</p>
Article Details
1. Introduction
Acromioclavicular (AC) joint injuries are a prevalent source of shoulder dysfunction, particularly among active individuals and contact athletes [1-3]. The severity of these injuries, classically described by the Rockwood classification [4-6], ranges from minor sprains to complete dislocations with significant displacement and instability [7,8]. In higher-grade injuries, particularly those involving complete rupture of the AC and coracoclavicular (CC) ligaments (types III-VI), surgical intervention is often pursued to restore joint alignment and functional stability [8,9]. Surgical treatment of type III injuries remains fiercely controversial [8,10-14].
Traditionally, surgical management has focused on reconstructing the CC ligaments to address vertical instability [2,3,16-19]. However, persistent horizontal and rotational instability remains a recognized cause of postoperative pain and functional limitation, even in anatomically successful reconstructions [3,16,18-22]. Biomechanical studies have underscored the critical role of the AC capsule and ligament complex, especially the anteroinferior and superoposterior bundles, in providing horizontal and rotational stability [10,23,24]. Techniques solely addressing the CC ligaments have demonstrated limitations in restoring this multidirectional stability [20,25,26].
Emerging surgical techniques aim to address these limitations through reconstruction of the AC capsule-ligament complex itself [21,27,28]. While various anatomic and biomechanical studies have examined different reconstruction strategies [1,16], there remains a paucity of direct biomechanical evaluations comparing isolated AC ligament reconstructions supplemented with traditional CC-based techniques [22,24,25]. Additionally, existing literature has not fully explored the mechanical performance of simplified suture-based AC ligament repairs under physiologically relevant loading conditions [7,9].
The purpose of this study is to evaluate the biomechanical performance of an anatomic, suture-based, AC ligament reconstruction technique. We hypothesize that this construct will demonstrate significant resistance to anterior-posterior and inferior-superior translations, as well as anterior-posterior rotations under loads, thereby contributing to improved horizontal and vertical stability of the AC joint. By establishing a reproducible biomechanical benchmark, our findings may inform surgical decision-making in cases where AC ligament integrity is critical to functional restoration.
2. Materials and Methods
This biomechanical study utilized twenty 3D-printed models of the scapula and clavicle, created from a high-resolution computed tomography (CT) scan of a consenting, 71 year-old male, without known acromioclavicular problems [24]. The CT data were segmented to create anatomically accurate models, which were then 3D-printed using acrylonitrile styrene acrylate (ASA) filament to ensure consistent mechanical properties across all specimens [29].
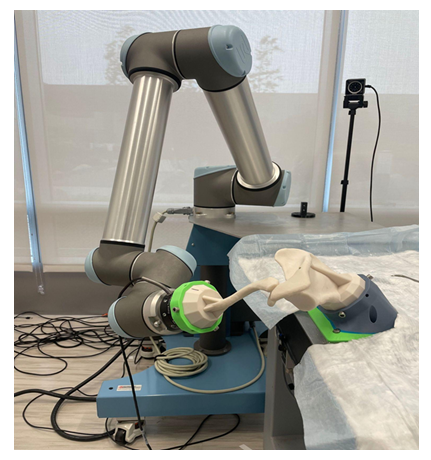
The experimental testing platform consisted of a Universal Robotics UR10 six-axis robotic arm equipped with a six-axis load cell (ATI Industrial Automation, Apex, NC, USA) (Figure 1). The scapula was rigidly fixed to a custom table mounted to the robot base, ensuring a stable and reproducible testing environment [16]. The clavicle was affixed to the tool flange of the robotic arm via the load cell, enabling precise three-dimensional measurement of forces and moments.
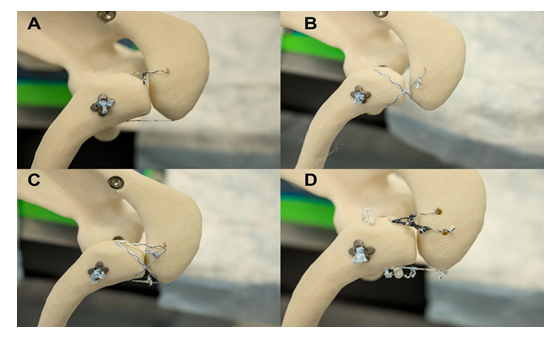
Each of the twenty specimens was randomly assigned to one of four reconstruction groups (n=5 per group). The O-frame group involved a single loop of 1.3 mm suture tape (SutureTape, Arthrex, Naples, FL, USA) passed through bone tunnels in the acromion and clavicle, creating a circular configuration (Figure 2A). The X-frame group used a single, crossing loop of 1.3 mm suture tape through bone tunnels in the acromion and clavicle (Figure 2B). The O + X-frame group combined the O-frame and X-frame constructs through the same set of bone tunnels (Figure 2C). The anatomic reconstruction aimed to replicate the anteroinferior and posterosuperior AC ligaments or capsular thickenings, utilizing three acromion-based and two clavicle-based all-suture anchors (Figure 2D) (FiberTak with SutureTape, Arthrex, Naples, FL, USA). The anatomic footprints and orientations were based on previously described anatomical studies [3,23].
Figure 2: Visual representation of the four reconstruction groups tested in this biomechanical study. A: O-frame configuration using a single loop of 1.3 mm suture tape through bone tunnels in the acromion and clavicle. B: X-frame configuration using a single, crossing loop of 1.3 mm suture tape through bone tunnels in the acromion and clavicle. C: O + X-frame configuration combining both loop constructs through the same bone tunnels. D: Anatomic reconstruction technique with three acromion-based and two clavicle-based all-suture anchors
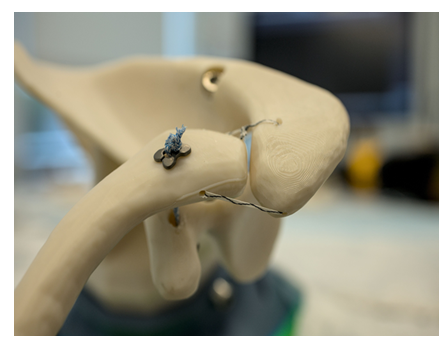
Coracoclavicular (CC) stabilization was performed in all specimens using a 2 mm FiberTape loop (Arthrex, Naples, FL, USA) secured with two titanium Dog Bone Buttons (Arthrex, Naples, FL, USA) (Figure 3) [17,18,27]. The clavicle was drilled centered anterior to posterior and 25mm medial to the AC joint [30]. The coracoid was drilled bicortically through the base.
For all constructs, precise drilling locations were used to replicate consistent and reproducible attachment points. The clavicle was drilled 10 mm medial to the AC joint on the direct anterior and direct posterior surfaces. The acromion was drilled in line with the clavicle tunnels, anteriorly and posteriorly, also 10 mm lateral to the AC joint. The third acromial fixation point was drilled 10 mm anterior to the posterior acromial point, creating an anatomic spread consistent with previous reconstructions [23,26]. Knots were hand-tied, and all-suture anchors were deployed bicortically to minimize the risk of pullout.
After application of the assigned reconstruction technique, the robotic arm was programmed to execute three physiologically relevant motions: posterior translation of the clavicle to assess horizontal stability [21,22,25], superior translation of the clavicle to measure vertical stability [1], and rotation around the clavicular long axis to evaluate rotational stiffness [20]. Motions were defined by the displacement of the lateral clavicle in relation to the acromion [31].
For each motion, the robotic arm displaced the clavicle relative to the scapula at a constant rate of 6 mm/s (for translations) or 2.75 °/s (for rotations) until a target displacement or rotation was reached. The target displacement was based on an initial test run to 20N which corresponded to 6mm of superior translation and 8mm of posterior translation. Twenty degrees of rotation was based on previous studies [22,27,28]. These ranges replicate physiologic motions observed in cadaveric studies of AC joint biomechanics [2,16,24]. Each motion was cycled ten times to precondition the constructs, and data from the final cycle were used for analysis to minimize artifacts from material creep or initial settling.
Real-time load and displacement data were recorded by the six-axis load cell during all motion sequences. The primary outcome measure for each reconstruction was stiffness, calculated as the load (N) or moment (Nm) required to achieve a target displacement or rotation. Post-testing inspections were conducted to assess each model for damage, loosening, or failure, ensuring the integrity and reliability of the data [22,25].
A formal a priori power analysis was not performed due to the exploratory nature of this in vitro study. Statistical analysis was conducted using independent samples t-tests to compare maximum and minimum load values across the four reconstruction groups for each testing condition. X-frame was used at the comparator. Data are reported as mean ± standard deviation, with a significance level set at p < 0.05.
3. Results
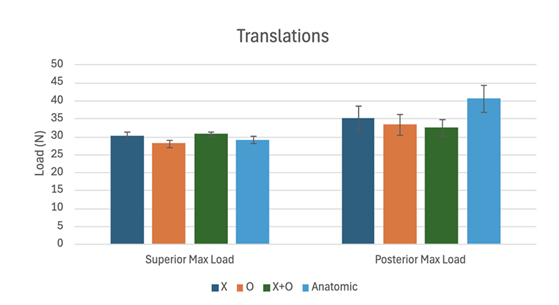
All four reconstruction techniques demonstrated comparable biomechanical performance across most tested motions. In superior translation, the X-frame group exhibited a mean stiffness of 30.30 ± 1.98 N, while the O-frame was 28.02 ± 2.42 N, the O + X-frame was 30.73 ± 1.10 N, and the anatomic construct was 29.07 ± 2.18 N (Table 1, Figure 4). No statistically significant differences were observed in superior load resistance between the groups (p > 0.05).
|
Superior Translation Max Load |
||||
|
X (N) |
O (N) |
X + O (N) |
Anatomic (N) |
|
|
Specimen 1 |
28.166 |
28.185 |
31.736 |
28.261 |
|
Specimen 2 |
28.691 |
29.921 |
30.452 |
28.937 |
|
Specimen 3 |
30.516 |
25.579 |
29.017 |
26.04 |
|
Specimen 4 |
33.126 |
25.576 |
31.623 |
30.27 |
|
Specimen 5 |
31.021 |
30.82 |
30.83 |
31.859 |
|
Average |
30.304 |
28.016 |
30.732 |
29.073 |
|
Standard Deviation |
1.981 |
2.419 |
1.099 |
2.183 |
|
P-Value |
0.14 |
0.684 |
0.379 |
|
Table 1: Superior Translation Max Load data table for four reconstruction groups across five specimens.
For posterior translation, the mean stiffness values were 35.03 ± 7.87 N for the X-frame, 33.42 ± 6.56 N for the O-frame, 32.42 ± 5.26 N for the O + X-frame, and 40.59 ± 8.63 N for the anatomic reconstruction (Table 2, Figure 4). Again, no significant differences were found between the constructs (p > 0.05).
|
Posterior Translation Max Load |
||||
|
X (N) |
O (N) |
X + O (N) |
Anatomic (N) |
|
|
Specimen 1 |
36.287 |
35.415 |
32.426 |
26.385 |
|
Specimen 2 |
43.787 |
27.924 |
41.375 |
44.973 |
|
Specimen 3 |
37.905 |
44.017 |
28.149 |
39.923 |
|
Specimen 4 |
22.339 |
30.398 |
30.867 |
49.099 |
|
Specimen 5 |
34.845 |
29.337 |
29.28 |
42.586 |
|
Average |
35.033 |
33.418 |
32.419 |
40.593 |
|
Standard Deviation |
7.868 |
6.563 |
5.261 |
8.629 |
|
P-Value |
0.734 |
0.554 |
0.318 |
|
Table 2: Posterior Translation Max Load data table for four reconstruction groups across five specimens.
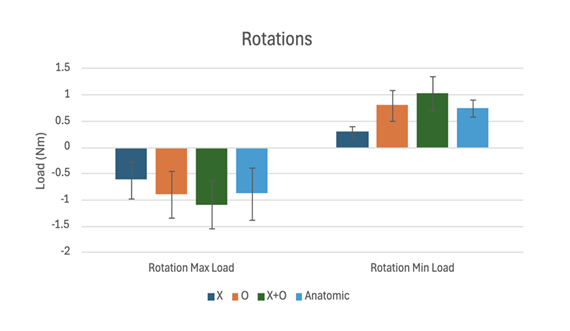
In anterior rotation, stiffness values were similar among the groups: -0.62 ± 0.79 for the X-frame, -0.90 ± 0.98 for the O-frame, -1.10 ± 1.02 for the O + X-frame, and -0.88 ± 1.11 for the anatomic group (Table 3, Figure 5). No statistically significant differences were identified in this loading mode (p > 0.05).
|
Anterior Rotation Max Load |
||||
|
X (N) |
O (N) |
X + O (N) |
Anatomic (N) |
|
|
Specimen 1 |
-0.798 |
-1.24 |
-1.968 |
-2.575 |
|
Specimen 2 |
0.114 |
0.114 |
-0.049 |
0.11 |
|
Specimen 3 |
0.181 |
0.166 |
0.064 |
0.086 |
|
Specimen 4 |
-1.733 |
-1.925 |
-1.972 |
-0.762 |
|
Specimen 5 |
-0.863 |
-1.62 |
-1.57 |
-1.278 |
|
Average |
-0.62 |
-0.901 |
-1.099 |
-0.884 |
|
Standard Deviation |
0.792 |
0.981 |
1.024 |
1.113 |
|
P-Value |
0.632 |
0.432 |
0.677 |
|
Table 3: Anterior Rotation Max Load data table for four reconstruction groups across five specimens.
In posterior rotation, the average stiffness was similar for most groups (0.79 ± 0.65 for the O-frame, 1.02 ± 0.71 for the O + X-frame, and 0.75 ± 0.36 for the anatomic group) (Table 4, Figure 5). However, the anatomic reconstruction demonstrated significantly higher stiffness than the X-frame (0.29 ± 0.26) with statistical significance (p = 0.048).
Throughout cyclic testing, all constructs maintained structural integrity, and no anchor pullout or gross failures were observed. Overall, while the anatomic reconstruction exhibited similar biomechanical performance to the other constructs in most directions, it provided improved posterior rotational stiffness compared to the traditional, X-frame, construct.
|
Posterior Rotation Min Load |
||||
|
X (N) |
O (N) |
X + O (N) |
Anatomic (N) |
|
|
Specimen 1 |
0.087 |
1.772 |
2.27 |
1.315 |
|
Specimen 2 |
0.495 |
0.506 |
0.765 |
0.363 |
|
Specimen 3 |
0.365 |
0.351 |
0.48 |
0.542 |
|
Specimen 4 |
-0.054 |
0.195 |
0.765 |
0.797 |
|
Specimen 5 |
0.531 |
1.132 |
0.831 |
0.711 |
|
Average |
0.285 |
0.791 |
1.022 |
0.746 |
|
Standard Deviation |
0.258 |
0.654 |
0.71 |
0.359 |
|
P-Value |
0.146 |
0.061 |
0.048 |
|
Table 4: Posterior Rotation Min Load data table for four reconstruction groups across five specimens.
4. Discussion
The primary finding of this biomechanical study is that anatomic suture reconstruction of the AC joint provides comparable biomechanical stability to traditional suture-based constructs in a 3D-printed in vitro model. Despite the inherent variability within groups, the anatomic reconstruction group did not demonstrate inferior mechanical performance compared to the O-frame, X-frame, and O + X-frame constructs in superior translation, posterior translation, or anterior rotation.
Our results align with previous biomechanical studies highlighting the critical role of AC ligament integrity in restoring horizontal and rotational stability [16,20,23]. While constructs focusing solely on CC stabilization have been effective in addressing vertical instability, they often fall short in resisting anterior-posterior translation and rotational forces [20,25,26]. By incorporating AC ligament repair in the anatomic construct, our findings support the concept that horizontal and rotational stability can be enhanced without compromising vertical stability.
Notably, there was a significant increase in posterior rotational stiffness observed in the anatomic construct (p = 0.048) which suggests a possible mechanical advantage for this technique in resisting rotational instability. This finding highlights the potential clinical relevance of anatomic AC reconstructions. While this certainly warrants further investigation, it is promising and may be of particular benefit in patients who remain symptomatic despite isolated CC-based repairs.
The study is not without limitations. First, the standard deviations observed across groups likely reflect variability in suture tensioning, tunnel placement, or minor model misalignments, limitations inherent to in vitro testing using 3D-printed bone models. Second, the absence of the soft tissue envelope, including dynamic stabilizers such as the deltoid and trapezius, likely influenced construct performance—highlighting the need for future cadaveric or in vivo studies to validate these results. Third, while the robotic testing platform provided reproducible and multi-axis loading, it did not replicate the full spectrum of dynamic and multi-directional forces experienced in vivo. Fourth, the relatively small sample size (n=5 per group) may limit the statistical power to detect subtle differences between constructs. Finally, we used 3D-printed ASA surrogate bone models of a single subject to reduce variation due to anatomic differences. ASA does not replicate the material properties of human bone. However, given the range of forces applied during testing, the difference in material stiffness likely had a minimal effect on measuring the stiffness of the repair constructs. Therefore, the results should be interpreted cautiously as the absence of muscle forces and neuromuscular control in these models may affect the generalizability of the findings to the clinical setting.
Despite the limitations, this pilot study suggests that anatomic based suture reconstructions are noninferior to traditional constructs and may offer a potential rotational advantage. This can provide surgeons with additional options for AC joint reconstruction, especially in cases where rotational and horizontal stability is of particular concern, either in a primary or revision setting.
Future research in this area may benefit from incorporating cadaveric models that more closely simulate the in vivo conditions observed in patients, particularly considering the influence of the surrounding soft tissue envelope. Additionally, the application of emerging knotless technology—which has garnered increasing popularity—could be explored. Further investigation into AC joint reconstruction in the context of both sufficient and deficient capsular tissue, as well as in the setting of bone loss, would also provide valuable insights for future treatment algorithms.
5. Conclusion
In this exploratory in vitro biomechanical study, anatomic suture reconstruction of the acromioclavicular joint demonstrated comparable mechanical stability to traditional suture-based constructs in most testing directions, while exhibiting improved posterior rotational stiffness. These findings highlight the potential benefit of incorporating anatomic AC ligament augmentation to address persistent horizontal and rotational instability, particularly in patients who remain symptomatic despite isolated CC-based repairs. Although the results must be interpreted within the limitations of a 3D-printed bone model and absence of soft tissue stabilizers, they provide encouraging evidence supporting the biomechanical robustness of simplified suture-based reconstructions. Future cadaveric studies and clinical investigations are warranted to validate these findings and refine surgical strategies for AC joint reconstruction.
Acknowledgement: The work was supported by the Scripps Clinic Medical Group and the San Diego Arthroscopy & Sports Medicine Fellowship. In-kind contributions in the form of implants were provided by Arthrex.
Conflicts of Interest: The authors report the following disclosures. Heinz R. Hoenecke Jr: American Shoulder and Elbow Surgeons: Board or committee member, Smith & Nephew: Paid consultant; Paid presenter or speaker, and Stryker: Paid presenter or speaker. Josiah A. Valk: Moximed: Type: Paid research consultant.
References
- Mazzocca AD, Santangelo SA, Johnson ST, et al. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med 34 (2006): 236-246.
- Barnes LA, Shi LL, Walters T, et al. Acromioclavicular joint injuries: Multi-center expert consensus study using the Delphi method. J Shoulder Elbow Surg 34 (2025): 1-12.
- Saccomanno MF, DE Ieso C, Milano G. Acromioclavicular joint instability: anatomy, biomechanics and evaluation. Joints 2 (2014): 87-92.
- Rockwood CA Jr, Green DP, eds. Fractures in Adults. Philadelphia, PA: Lippincott (1984): 860-910.
- Gorbaty JD, Hsu JE, Gee AO. Classifications in brief: Rockwood classification of acromioclavicular joint separations. Clin Orthop Relat Res 475 (2017): 283-287.
- Granville-Chapman J, Torrance E, Rashid A. The Rockwood classification in acute acromioclavicular joint injury does not correlate with symptoms. J Orthop Surg 26 (2018): 1-5.
- Berthold DP, Münch LN, Dyrna FGE, et al. Current concepts in acromioclavicular joint (AC) instability – a proposed treatment algorithm for acute and chronic AC-joint surgery. BMC Musculoskelet Disord 23 (2022): 1078.
- Albishi W, AlShayhan F, Alfridy A, et al. Acromioclavicular joint separation: Controversies and treatment algorithm. Orthop Rev 16 (2024): 1-7.
- Liu Y, Zhang X, Yu Y, et al. Suture augmentation of acromioclavicular and coracoclavicular ligament reconstruction for acute acromioclavicular dislocation. Medicine (Baltimore) 100 (2021): e27007.
- Tingle M, Wang T, Hoenecke Jr HR. Current trends in surgical treatment of the acromioclavicular joint injuries in 2023: A review of the literature. JSES Int 8 (2024): 389-393.
- Kim SH, Koh KH. Treatment of Rockwood Type III acromioclavicular joint dislocation. Clin Shoulder Elbow 21 (2018): 48-55.
- Paul RW, Tchangou N, Floyd K, et al. Timing of surgical treatment for high-grade acromioclavicular joint injuries does not affect functional outcomes. Arthrosc Sports Med Rehabil 7 (2025): 101017.
- Adra M, Mohamed Haroon A, Milchem H, et al. Operative versus nonoperative management of high-grade acromioclavicular injuries: a systematic review and meta-analysis. Cureus 16 (2024): e76682.
- Linborg CM, Smith RD, Reihl AM, et al. Current concepts in management of acromioclavicular joint injury. J Clin Med 13 (2024): 1413.
- Niehaus R, Schleicher A, Ammann E, et al. Operative versus conservative treatment of AC-joint dislocations Rockwood grade ≥ III: An economical and clinical evaluation. Cost Eff Resour Alloc 21 (2023): 63.
- Hislop P, Sakata K, Ackland DC, et al. Acromioclavicular joint stabilization: A biomechanical study of bidirectional stability and strength. Orthop J Sports Med 7 (2019): 2325967119836751.
- Liu T, Bao FL, Jiang T, et al. Acromioclavicular joint separation: Repair through suture anchors for coracoclavicular ligament and nonabsorbable suture fixation for acromioclavicular joint. Orthop Surg 12 (2020): 1362-1371.
- Seo JB, Heo K, Kim SJ, et al. Arthroscopic acromioclavicular fixation with suture tape augmentation after coracoclavicular fixation with dog bone button: Surgical technique. Arthrosc Tech 7 (2018): e1197-e1203.
- White CC, Cincere BA. Acromioclavicular joint reconstruction with acromioclavicular ligament augmentation using a knotless, all-suture anchor construct. Arthrosc Tech 14 (2025): e103226.
- Celik H, Chauhan A, Flores-Hernandez C, et al. Vertical and rotational stiffness of coracoclavicular ligament reconstruction: A biomechanical study of 3 different techniques. Arthroscopy 36 (2020): 1264-1270.
- Aliberti GM, Mulcahey MK, Brown SM, et al. Restoring horizontal stability of the acromioclavicular joint: open acromioclavicular ligament reconstruction and repair with semitendinosus allograft. Arthrosc Tech 9 (2020): e1619-e1626.
- Morikawa D, Mazzocca AD, Obopilwe E, et al. Reconstruction of the acromioclavicular ligament complex using dermal allograft: a biomechanical analysis. Arthroscopy 36 (2020): 108-115.
- Nakazawa M, Nimura A, Hagiwara Y, et al. The orientation and variation of the acromioclavicular ligament: An anatomic study. Am J Sports Med 44 (2016): 2690-2695.
- Velasquez Garcia A, Salamé Castillo F, Ekdahl Giordani M, et al. Anteroinferior bundle of the acromioclavicular ligament plays a substantial role in joint function during shoulder elevation and horizontal adduction: a finite element model. J Orthop Surg Res 17 (2022): 73.
- Ibrahim DK, Lam PH, Aveledo Anzola RJ, et al. Biomechanical evaluation of an independent acromioclavicular ligament repair for acromioclavicular joint reconstruction. Shoulder Elbow 12 (2020): 184-192.
- Rushton PRP, Gray JM, Cresswell T. A simple and safe technique for reconstruction of the acromioclavicular joint. Int J Shoulder Surg 4 (2010): 15-17.
- Dyrna FGE, Imhoff FB, Voss A, et al. The integrity of the acromioclavicular capsule ensures physiological centering of the acromioclavicular joint under rotational loading. Am J Sports Med 46 (2018): 1432-1440.
- Dyrna FGE, Imhoff FB, Haller B, et al. Primary stability of an acromioclavicular joint repair is affected by the type of additional reconstruction of the acromioclavicular capsule. Am J Sports Med 46 (2018): 3471-3479.
- McMillan A, Kocharyan A, Dekker SE, et al. Comparison of materials used for 3D-printing temporal bone models to simulate surgical dissection. Ann Otol Rhinol Laryngol 129 (2020): 1168-1173.
- Olivos-Meza A, Rodríguez-Argueta ME, Suarez-Ahedo C, et al. Free hand drilling technique to enhance central position of tunnels in arthroscopic acromioclavicular joint fixation using TightRope system. Arthrosc Tech 10 (2021): e1829-e1837.
- Beitzel K, Obopilwe E, Apostolakos J, et al. Rotational and translational stability of different methods for direct acromioclavicular ligament repair in anatomic acromioclavicular joint reconstruction. Am J Sports Med 42 (2014): 2141-2148.
Related PubMed Articles
- Delocalized electrolyte design enables 600 Wh kg(-1) lithium metal pouch cells.
- Noninvasive evaluation of treatment-related protein expression status in advanced gastric cancer using dynamic nomograms with dual-energy CT: a multicenter study.
- Biosynthesis of modular signaling molecules requires functional diversification of carboxylesterases in Pristionchus pacificus.
- Mutations in ClpC1 or ClpX subunit of caseinolytic protease confer resistance to ilamycins in mycobacteria.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 