Explorations Gone Viral: A Comparative Study of Emergency Laparotomies in COVID-19 Positive vs COVID-19 Negative Patients at A Tertiary Care Hospital during the COVID-19 Pandemic
Dr. Aishwarya Dutt1*, Dr. Ajay Bhandarwar1, Dr. Girish Bakhshi1, Dr. Nikhil Dhimole1, Dr. Harshal Padekar1, Dr. Snehal Dandge1, Dr. Kaushal Lahoti1, Dr. Advaith Chetan2, Dr. Apoorva Raichur1
1Department of General Surgery, Grant Government Medical College and Sir J. J. Group of Hospitals, Mumbai, Maharashtra, India
2Department of Critical Care, Chandramma Dayanand Sagar Institute of Medical Education and Research, Bangalore, Karnataka, India
*Corresponding author: Dr. Aishwarya Sunil Dutt, Department of General Surgery, Grant Government Medical College and Sir J. J. Group of Hospitals, Mumbai, Maharashtra, India.
Received: 31 August 2023; Accepted: 12 September 2023; Published: 03 October 2023.
Article Information
Citation: Aishwarya Dutt, Ajay Bhandarwar, Girish Bakhshi, Nikhil Dhimole, Harshal Padekar, Snehal Dandge, Kaushal Lahoti, Advaith Chetan, Apoorva Raichur. Explorations Gone Viral: A Comparative Study of Emergency Laparotomies in COVID-19 Positive vs COVID-19 Negative Patients at A Tertiary Care Hospital during the COVID-19 Pandemic. Archives of Clinical and Biomedical Research. 7 (2023): 510-521.
View / Download Pdf Share at FacebookAbstract
Aim: To compare the mortality in emergency laparotomy cases between those with COVID-19 infection to those without the infection and to identify predicting factors that would help in optimum management for the same.
Method: A prospective observational study was conducted in a tertiary care centre in Mumbai. Patients underwent exploratory laparotomy of which 20 were COVID-19 positive (Group A) while 20 were COVID-19 negative (Group B). Patient’s details with blood investigations, radiological investigations, preoperative and postoperative stay were taken into consideration. All these parameters were studied and compared in detail.
Result: 40 cases that underwent emergency laparotomy for various causes were compared. Pulmonary complications were seen postoperatively in 45% patients of Group A and 15% patients of Group B. Mortality was seen in 40% cases of Group A of which 87.5% cases were due to postoperative respiratory complications due to COVID-19 infection. Group B had one mortality, due to septic shock. Mortality was significantly higher in Group A(p-value: 0.008). Comorbidities such as hypertension, diabetes mellitus and ischemic heart disease were seen to be associated with a higher incidence of mortality. Mortality was witnessed more in the age group above 40 years. High APACHE-II score and Computed Tomography severity index (CTSI) showed higher mortality. Antivirals did not show any effect on postoperative survival.
Conclusion: Emergency operations can be taken up in COVID-19 positive patients with adequate precautions. Postoperative complications are related to comorbidities, age and CTSI. High index of suspicion for pulmonary complications and aggressive postoperative management with steroids gives improved outcomes.
Keywords
<p>COVID-19; Emergency laparotomy; SARS-CoV2; Postoperative mortality</p>
Article Details
1. Introduction
The coronavirus disease 2019(COVID-19) pandemic has significantly affected health and aggravated the previously milder diseases. Declared as a pandemic since March 2020 by World Health Organization, COVID-19 has been added as an important epidemic alongside Spanish flu, Severe Acute Respiratory Syndrome (SARS) and avian flu [1]. Many aspects of this disease, as well as treatment protocol and risks, remain unclear [2]. The virus has an impact on the respiratory system and other organs, such as the gastrointestinal system. Reports of thromboembolic events in this group of patients has led to a new spectrum of clinical presentations [3,4]. Gastrointestinal complications such as hollow viscus perforation and obstructions requiring urgent surgical intervention have also been seen. These imbalances, in conjunction with the disease, cause increased risk of surgery and possibility of higher complications during the perioperative period. The second wave showed an increase in the number of cases as compared to the first wave. Escalation in cases after a period of time could be due to the highly infectious double mutant variant of SARS-CoV-2 or the negligent behaviour of population and relaxation of interventions [5]. Omicron variant brought in the virulent third wave which had a shorter incubation period and faster doubling time [6]. Few studies show a higher mortality rate in surgical cases who developed COVID-19 pneumonia during the perioperative period [7,8]. This requires additional support by larger case series in tertiary care hospitals. The present study aims to detect the mortality related to COVID-19 infection in emergency laparotomy cases and to identify predicting factors that would help in the further optimum management for the same.
2. Materials and Methods
A prospective observational study was conducted in a tertiary care hospital in Mumbai from April 2020 to March 2022 after taking approval of The Institutional Ethics Committee. This included the first wave (April 2020 to September 2020), second wave (February 2021 to May 2021) and the third wave(December 2021 to March 2022) of the pandemic in India. A study group (Covid-19 positive patients) was compared with a control group (Covid-19 negative patients). Pre-operative Computed Tomography (CT) scan was done for all the patients with respiratory complaints in both groups. The patient’s demographics, presentation, APACHE-II scoring, blood investigations including on admission, CT findings, perioperative condition, type of anaesthesia administered and the need of ICU (Intensive Care Unit) stay were considered. The treatment for the SARS-CoV-2 virus was done as per the protocols as per the time of admission of the patient. Precautions were taken to prevent exposure, with personal protective equipment worn by the surgical and anaesthetic team during the surgery. All instruments were autoclaved before and after usage, with fumigation done after every surgery in the operation theatre. Mortality in both groups was compared and significance was checked with the help of chi square (χ2) test. Patient complaints and recovery were followed up for a period of one month after surgery, which included clinical history and examination. The study was done according to STROBE guidelines for observational studies. The χ2 test was used for categorical data for test of Significance. P-value of <0.05 was considered significant with a confidence interval of 95%..
3. Results
40 emergency laparotomy cases were studied out of which 20 were suffering from COVID-19 infection (Group A) during the surgery while 20 were not infected(Group B). Of the COVID-19 positive patients, 11 cases were from the first wave of the pandemic, while five cases were from the second wave and four from the third wave. The mean hospital stay was 26.2 days, with most patients taken for surgery within 12 hours of admission, barring a re-exploration taken up after six days of admission and a sigmoid colon mass perforation which occurred after 10 days of admission. Patients presented with similar abdominal complaints in both the groups. All patients complained of abdominal pain. Group A had symptoms such as vomiting (50%), fever (15%), abdominal distension (15%) and inability to pass stools (15%). Patients from Group B had complaints such as vomiting (50%), inability to pass stools (40%), fever (35%), and abdominal distension (5%). One patient in Group B also gave a history of foreign body insertion through rectum. Twelve patients had associated respiratory symptoms of breathlessness, cough, and sore throat from Group A while only one patient had complaints of breathlessness in Group B. This was seen to be statistically significant between the groups with a p-value of 0.0002. Comorbidities between the two groups were comparable (Table1).
Table 1: Patient demographics and co-morbidities
|
Group A |
Group B |
|||
|
Category |
N (%) |
Mortality |
N (%) |
Mortality |
|
Sex |
||||
|
Female |
20% |
75%(3 of 4) |
15% |
0%(0 of 3) |
|
Male |
80% |
31.25%(5 of 16) |
85% |
5.8%(1 of 17) |
|
Age |
||||
|
>=39yrs |
45% |
22.22%(2 of 9) |
50% |
0%(0 of 10) |
|
40-59yrs |
45% |
55.55%(5 of 9) |
35% |
0%(0 of 7) |
|
60=<yrs |
10% |
50%(1 of 2) |
15% |
33.33%(1 of 3) |
|
Co-morbidities |
||||
|
Diabetes |
25% |
80%(4 of 5) |
15% |
33.33%(1 of 3) |
|
Hypertension |
15% |
66.6%(2 of 3) |
10% |
0%(0 of 2) |
|
Ischemic Heart Disease |
10% |
50%(1 of 2) |
5% |
0%(0 of 1) |
|
Abdominal Symptoms |
||||
|
Abdominal Pain |
100% |
40%(8 of 20) |
95% |
5.26%(1 of 19) |
|
Fever |
15% |
100%(3 of 3) |
35% |
0% |
|
Vomiting |
50% |
60%(6 of 10) |
50% |
0% |
|
Constipation |
5% |
0% |
20% |
0% |
|
Abdominal Distension |
15% |
66.66% |
5% |
0% |
|
Respiratory Symptoms |
||||
|
Cough |
25% |
60%(3 of 5) |
0% |
0% |
|
Breathlessness |
25% |
20%(1 of 5) |
5% |
0% |
|
Sore Throat |
10% |
0%(0 of 2) |
0% |
0% |
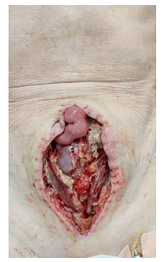
Of the 20 cases in Group A, 12 were operated for perforation peritonitis, one for appendicular tip perforation, one for gall stone ileus, two for acute intestinal obstruction, one for superior mesenteric artery(SMA) thrombosis (Figures1&2), one for acute appendicitis, one for hemoperitoneum with sigmoid laceration and one for ruptured hepatic abscess. From Group B, seven patients were operated for perforation peritonitis, six cases for intestinal obstruction, one for anastomotic leak, two for burst abdomens (post appendicectomy and ileal perforation repair), one for a foreign body inserted in the rectum, one for emphysematous cholecystitis, one for SMA thrombosis and one for a perianal and intraabdominal abscess. All surgeries were done under general anaesthesia, other than an appendicectomy in Group A, which was done under spinal anaesthesia. Explanation was given to all about the possible complications of their respective surgeries and anaesthesia. The added risk associated with SARS-CoV-2 infection leading to pulmonary complications was also emphasised to the patients in Group A.
Intensive care was required for 55% (11 of 20) of Group A cases. In Group B, 60% (12 of 20) patients required ICU care postoperatively. Group A and B respectively had eight and nine patients requiring postoperative mechanical ventilation with an average stay in ICU of 1.5 and 3.18 days, amongst the patients who were discharged. There was no significant difference between the two groups regarding post-operative need for ICU (p-value: 0.75) and mechanical ventilation(p-value:0.34). Postoperative ICU stay in those who did not survive was seen to be less than two days in Group A and three days in Group B. High flow nasal oxygen was administered for one COVID-19 positive patient with SMA thrombosis and was started on Category-1 AKT for a pre-existing tubercular lesion. Antivirals were given to 12 patients of the 20 in Group A and showed no effect on mortality. CT Thorax was done and compared for the patients with respiratory complaints in both the groups. In Group A, 12 patients underwent CT thorax with all showing changes in the pulmonary fields and 11 patients having ground glass opacities. Bilateral pleural effusion was seen in six patients, patchy areas of consolidation in five patients and cavitatory lesions in two patients suggestive of Koch’s infection, of which only one tested positive on sputum GeneXpert testing. CT Severity index (CTSI) calculated for the patients ranged from 4 to 12, with the average being 5.08. Amongst the mortalities in Group A, the average CTSI was 8.75. Hence, a higher CT Severity score showed a higher mortality. In Group B, one patient with respiratory complaints showed no abnormalities on CT. APACHE-II scoring was calculated preoperatively, ranging from 2 to 32. Amongst the eight postoperative mortalities in Group A, the average APACHE-II score was 14(ranging from 2 to 32), while that of the patients who survived in Group A was 5.33(ranging from 3 to 8). Two patients had an APACHE-II score of more than 30, with both experiencing a fatal outcome. In Group B the one mortality had a score of 10 whereas the patients who survived had an average score of 5.53(ranging from 2 to 8). Statistically, APACHE-II score showed no significant difference between Group A and B(p-value: 2.11) and lacked the sensitivity to predict eventual mortality. Postoperatively, three patients, all from Group A, underwent re-exploration. One underwent refashioning of prolapsed ileostomy stoma and the other two were taken up to for repair of burst abdomen (Figure3).
Pulmonary complications were seen postoperatively in 9(45%) patients in Group A as compared to three(15%) patients in Group B. Out of the nine patients in Group A, respiratory failure was seen in five patients, pneumonia in two patients. One of the patients who developed pneumonia was seen to develop respiratory failure as well. Out of the three patients in Group B, two suffered from pneumonia, of which one had respiratory failure and required a prolonged postoperative ICU stay. The remaining one patient of Group B had lung atelectasis and recovered in two days postoperatively (Table 2a &b). This showed a significant difference in pulmonary complications between the groups (P-value: 0.047), with it being greater in Group A.
Table 2(a): Procedures done along with their pre and post-operative course in COVID-19 positive patients (Group A)
*: Mortality
#: Done under Spinal anaesthesia (Others were done under General anaesthesia)
DM: Diabetes mellitus
HTN: Hypertension
IHD: Ischemic heart disease
CT: Computed tomography
CTSI: Computed tomography severity index
GGO: Ground glass opacities
SSI: Surgical site infection
Table 2(b): Procedures done along with their pre and post-operative course in COVID-19 negative patients (Group B)
*: Mortality
CT: Computed tomography
CTSI: Computed tomography severity index
SSI: Surgical site infection
Mortality was seen in 40% (8 of 20) cases in Group A, of which 87.5% (7 of 8) cases were attributed to postoperative respiratory complications due to COVID-19 infection and 12.5%(1 of 8) cases were due to septic shock due to peritonitis. The flaring up of COVID-19 infection after surgical and anaesthetic insult could be due to the added surgical stress, superadded abdominal infection, and postoperative respiratory compromise. In Group B, there was only one mortality which was due to post-operative septic shock. Hence, the mortality in Group A was seen to be significantly different (higher) with a P-value of 0.008. Amongst the mortalities in Group A, five of them had small bowel perforations; two had acute intestinal obstruction while one patient had SMA thrombosis. Of the eight mortalities, six (of 11 cases) were seen during the first wave while there was only one (of 5 cases) seen during the second wave and one (of 4 cases) in the third wave. Comorbidities were seen in nine patients from Group A and five patients from Group B. Amongst the nine from Group A, six (66.67%) developed postoperative respiratory complications while four of the 11(36.36%) patients without comorbidities suffered from the same. On comparing the mortality, in Group A, five of the nine (55.56%) patients with comorbidities had a fatal outcome compared to three of the 11(27.27%) patients without any. In Group B, two out of the five(40%) patients with comorbidities developed postoperative respiratory complications as compared to one out of the 15(6.67%) without comorbidities. There were no mortalities amongst the patients without comorbidities in Group B, as compared to one amongst the five (20%) with comorbidities. The age groups between 40-59 years had the highest mortalities, with five of the nine mortalities within this age group and from Group A. Six of the eight (75%) deaths from Group A were above 40 years of age, while two (25%) deaths were below 40 years of age. The p-value was calculated to compare Group A and B with respect to age, pulmonary complication, and mortality. There was no significant difference between the two groups with regards to pulmonary complications. Group A patients were seen to have a significantly greater mortality in the age groups between 40-60 years compared to Group B(p-value:0.017). Group B had one mortality which was above 60 years of age. All 31 discharged patients (12 from Group A and 19 from Group B) were followed up after one month. Complaints were reviewed, and patients examined (Table 3a and b). Two patients from Group A had mild breathlessness on exertion, relieved on taking rest. No patients from Group B had any respiratory complaints and no respiratory compromise was seen in any of the discharged patients after one month. Three patients (one from Group A and two from Group B) had a postoperative surgical site infection which was treated with daily dressings.
Table 3(a): One month Follow Up in Group A Patients
|
Diagnosis |
Respiratory complaints |
Abdominal complaints |
Examination |
Co-morbidities |
|
Prepyloric Perforation |
None |
None |
Normal |
None |
|
Appendicular tip Perforation |
Breathlessness on exertion |
None |
Normal |
Hypertension, Ischaemic Heart Disease |
|
Ileal Perforation |
None |
None |
Normal |
None |
|
Ileal Perforation due to Stab injury |
None |
Abdominal Pain |
Normal |
None |
|
Acute Appendicitis |
None |
None |
Normal |
None |
|
Prepyloric Perforation |
Breathlessness on exertion |
None |
Normal |
None |
|
Peri-colic abscess secondary to diverticulitis |
None |
None |
Normal |
Diabetes Mellitus |
|
Prepyloric Perforation |
None |
Surgical site wound |
Surgical site infection |
None |
|
Sigmoid Colon Adenocarcinoma with Metastasis |
None |
None |
Normal |
Abdominal Koch's, Retroviral disease |
|
Distal Ileal Obstruction with Ileal Perforation |
None |
None |
Normal |
Abdominal Koch's |
|
Hemoperitoneum with Sigmoid colon laceration |
None |
None |
Normal |
None |
|
Ruptured hepatic abscess |
None |
Abdominal Pain |
Normal |
None |
Table 3(b): One month Follow Up in Group B Patients
|
Diagnosis |
Respiratory complaints |
Abdominal complaints |
Examination |
Co-morbidities |
|
Anastomotic leak post Resection and Anastomosis |
None |
None |
Normal |
None |
|
Prepyloric Perforation |
None |
None |
Normal |
None |
|
Burst Abdomen post appendicectomy |
None |
None |
None |
None |
|
Duodenal perforation with worm infestation |
None |
None |
Normal |
None |
|
Acute Intestinal obstruction |
None |
None |
Normal |
None |
|
Acute Intestinal obstruction |
None |
None |
Normal |
None |
|
Ileal Perforation |
None |
None |
Normal |
None |
|
Sigmoid Perforation |
None |
Surgical site wound |
Surgical site infection |
Abdominal Koch’s, Retroviral disease |
|
Prepyloric Perforation |
None |
None |
Normal |
None |
|
Foreign body insertion per rectum |
None |
None |
Normal |
None |
|
Prepyloric Perforation |
None |
None |
Normal |
None |
|
Adenocarcinoma of transverse colon |
None |
None |
Normal |
None |
|
Acute Intestinal obstruction |
None |
None |
Normal |
None |
|
SMA thrombosis with ileum necrosis |
None |
Abdominal Pain |
Normal |
Hypertension |
|
Emphysematous cholecystitis with liver abscess |
None |
Abdominal Pain |
Normal |
Diabetes Mellitus, Hypertension |
|
Acute Intestinal obstruction |
None |
None |
Normal |
None |
|
Burst abdomen post Primary repair of Ileal Perforation |
None |
None |
Normal |
None |
|
Intra-abdominal and perianal abscess |
None |
Surgical site wound |
Surgical site infection |
Diabetes Mellitus, Ischaemic Heart Disease |
|
Acute intestinal obstruction |
None |
None |
Normal |
None |
4. Discussion
COVID-19 is known to cause a number of complications such as acute respiratory distress syndrome, gastrointestinal disturbances, acute cardiac injury, acute kidney injury and secondary infections [9]. The increase in reactive oxygen species and activation of the renin–angiotensin–aldosterone system causes insulin resistance and hyperglycaemia. There is an increase in fibrinogen and D-Dimer, increasing the blood viscosity and vascular endothelial damage and, hence, the associated cardiovascular events, thromboembolism and disseminated intravascular coagulation [10]. The present study determines the difference in outcomes in patients undergoing emergency laparotomy with SARS-CoV-2 infection compared to those unaffected. Infected patients had a significantly higher (p-value: 0.008) number of preoperative respiratory complaints as compared to those without the infection. Although there was no significant difference between patients with or without the infection for the requirement of postoperative ventilation(p-value:0.34) or ICU care(p-value:0.75), pulmonary complications were significantly higher in patients with COVID-19 infection(45%) as compared to those without the infection(15%) and undergoing emergency laparotomies(p-value:0.047). The study showed that patients with comorbidities such as DM and hypertension had a worse outcome compared to those without them. There was a higher incidence of postoperative complications (COVID-19 positive: 66.67% vs 36.3% and COVID-19 negative: 40% vs 6.67%) and mortality (COVID-19 positive:55.56% vs 27.27% and COVID-19 negative:20% vs 0%) in those with comorbidities in both groups. The use of antivirals did not correlate to a reduction in postoperative mortality. APACHE-II score, for indicating postoperative outcomes, was not sensitive as scores ranged between 2 to 32 in the patients with eventual mortality. It did not show a significant increase in COVID-19 positive patients as well (p-value: 2.11). However, despite lacking sensitivity, all patients with an APACHE-II score of more than 30 had a fatal outcome.
Postoperatively, respiratory complaints increased which signified a possible subtle presentation which flared up after surgical and anaesthetic trauma. Mortality was most commonly due to respiratory failure in cases with COVID-19 infection (87.5%) as compared to those not infected(0%). This also corresponded to the higher CTSI in the patients with mortalities. The mortality in COVID-19 positive patients was also seen to be significantly higher (p-value: 0.008). As we progressed onwards with our experience with COVID-19 emergencies and improved knowledge about the disease we could see an improvement in outcomes of the patients. This was confirmed with the decrease in mortality as seen in the second and third wave. Initial high mortality rates could also be due to delayed presentations to the hospital due to lack of transportation and referral facilities during the peak of lockdown imposed around our district. As these facilities were made available later, patients were able to report to facilities promptly and get the necessary treatment. Aggressive use of steroids also helped with decreasing mortality over the months. Few studies have been done to detect the effect of SARS-CoV-2 on surgical procedures and its increased morbidity and mortality associated with it. A study by COVIDsurg collaborative was done on mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection during the first wave of the pandemic [11]. This cohort study covered 235 hospitals with 1128 patients who had undergone surgeries, of which 373 had undergone gastrointestinal surgeries like the present study. It showed that emergency surgeries had a higher incidence of mortality compared to elective surgeries (25.6% [214 of 835] vs 18.9% [53 of 280]). The present study showed similar results with a high mortality seen in the patients operated on emergency basis for exploratory laparotomy with COVID-19 infection as compared to patients without the infection (40% vs 5%). Pulmonary complications related to COVID-19 infection such as pneumonia, pleural effusion and ventilatory requirement was recorded in both studies as well. Handaya et al conducted a study consisting of four cases that underwent emergency laparotomy surgeries in COVID-19 positive patients with gastrointestinal emergencies [5]. All the patients underwent emergency laparotomy, received postoperative care, and were discharged from the hospital. After one month follow-up, one patient had no complaints, two patients had surgical site infections, and one patient died because of acute respiratory distress syndrome due to lung metastasis. Compared to the present study the mortality was seen to be less. With similar follow up periods, surgical site infections were seen in both studies. Acute respiratory distress, however, was not seen as a delayed presentation in the present study. Antiviral treatment has been studied extensively with multiple trials attempting to bring about better outcomes. It has been seen that antiviral medication, alone or in combination with other medications, did not show an increase in survival. However, increased survival has been associated with low molecular weight heparin and tocilizumab [12]. The effect of antivirals or additional medications required perioperatively in emergency surgeries in COVID-19 needs further research. The present study involved the enrolment of consecutive cases in a single centre which provided results of a consistent and uniform management protocol. This helped in reducing the varied outcomes due to different surgical techniques practiced in different set ups. At the same time the evolving concepts of COVID-19 infection management brought a heterogeneity in the management of the cases over the months. The limitation of the study was loss to follow up of the patients beyond a month after discharge. This caused a difficulty in recording any delayed presentations of the cases. It was seen in the present study that patients with comorbidities like DM, hypertension and ischemic heart disease (IHD) were at a higher risk for mortality in patients operated for exploratory laparotomy with COVID-19 infection. It was seen that the surgical and anaesthetic insult in COVID-19 infected individuals can cause unfavourable results and high risk of mortality compared to non-infected individuals undergoing emergency laparotomy. As our understanding of the disease improved the percentage of mortality decreased in the second and third wave as compared to the first wave.
5. Conclusion:
Emergency operations can be taken up in COVID-19 positive patients with adequate precautions, after judging the benefits of surgery, due to increased chances of postoperative pulmonary complications and mortality. Patients with comorbidities like DM, hypertension and IHD are at a higher risk of having adverse postoperative outcomes. Radiological studies such as CT are helpful in detecting the severity and the mortality. Antivirals may not have an effect in the treatment for these patients. High index of suspicion of pulmonary complications helps in early detection. This predisposes to early introduction of steroid and aggressive management that helps in the reduction of mortality.
Conflict of Interest:
None
References:
- Rafiq D, Batool A, Bazaz MA. Three months of COVID-19: A systematic review and meta-analysis. Rev Med Virol 30 (2020): 2113.
- Agnes A, Greca ALA, Tirelli F, et al. Duodenal perforation in a SARS-CoV-2-positive patient with negative PCR results for SARS-CoV-2 in the peritoneal fluid. Eur Rev Med Pharmacol Sci 24 (2020): 12516-12521.
- Mehrabi Nasab E, Heidarzadeh S, Yavari B, et al. Acute upper limb ischemia in a patient with COVID-19: A case report. Ann Vasc Surg 77 (2021): 83-85.
- Parminder Kaur, Sahitya Posimreddy BS, Firas Qaqa, et al. COVID-19 Presenting as Acute Limb Ischaemia. Eur J Case Reports Intern Med 7 (2020): 001724.
- Handaya AY, Andrew J, Hanif AS, et al. Covid-19 mimicking symptoms in emergency gastrointestinal surgery cases during pandemic: A case series. Int J Surg Case Rep [Internet] 77 (2020): 22-27.
- Singhal T. The Emergence of Omicron: Challenging Times Are Here Again! Indian J Pediatr [Internet] 89 (2022): 490-496.
- Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine [Internet] 21 (2020): 100331.
- Aminian A, Safari S, Razeghian-Jahromi A, et al. COVID-19 Outbreak and Surgical Practice: Unexpected Fatality in Perioperative Period. Ann Surg 272 (2020): 27-29.
- Chaolin Huang, Yeming Wang, Xingwang Li, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (2020): 497-506.
- Lim S, Bae JH, Kwon HS, et al. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol [Internet] 17 (2021): 11-30.
- Bhangu A, Nepogodiev D, Glasbey JC, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative sars-cov-2 infection: An international cohort study. Lancet 396 (2020): 27-38.
- Guglielmetti L, Aschieri D, Kontsevaya I, et al. Treatment for COVID - 19- a cohort study from Northern Italy. Sci Rep [Internet] 11 (2021): 19-22.




 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 