Pandemic Rumination and Resilience on Frontline Health Care Professionals in India: A Cross-Sectional Survey
Sonali Vadi1*, Neha Rungta2, Sagar Shah3, Ashwini Pednekar4
1Consultant Intensivist, Department of Intensive Care Medicine, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai, India
2Associate Professor, Hirabai Cowasji Jehangir Medical Research Institute, Jehangir Hospital, Pune, India
3Clinical Associate, Accident and Emergency Department, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai, India
4Clinical Associate, Department of Intensive Care Medicine, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai, India
*Corresponding author: Sonali Vadi, Department of Intensive Care Medicine, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai, Maharashtra, India; E-mail: sonali.vadi@kokilabenhospitals.com
Received: 11 May 2022; Accepted: 23 May 2022; Published: 31 May 2022
Article Information
Citation: Sonali Vadi, Neha Rungta, Sagar Shah, Ashwini Pednekar. Pandemic Rumination and Resilience on Frontline Health Care Professionals in India: A Cross-Sectional Survey. Archives of Clinical and Biomedical Research 6 (2022): 481-491.
View / Download Pdf Share at FacebookAbstract
Background High workload during pandemic has caused psychological stress in Healthcare Professionals (HCPs). It is necessary to identify factors that lead to negative mental health effects, and those that create resilience to withstand stress.
Aim: We examined relationship between stress & perseverative thinking, and social networking & resilience in HCPs working in Emergency Room (ER) and intensive care unit (ICU).
Methods Cross-sectional survey conducted from 15th April-15th May, 2021 using questionnaire with clinically-validated scales: WHO 5 Well-being Index, Brief Resilience Scale (BRS), UCLA Loneliness Scale, Perseverative Thinking Questionnaire (PTQ), Impact of Event Scale – 6 (IES 6), and Berkman-Syme Social Networking Index (SNI). We analysed effect of age, location of work, marital status, and participation in community activity on these indices.
Results 39.6% had low resilience, 34.8% had high impact of pandemic. BRS and IES 6 score varied significantly when classified according to age and marital status (p<0.05). WHO-5 Wellbeing Index was negatively correlated with UCLA Loneliness Scale, PTQ and IES 6 (p<0.05). SNI and BRS was negatively correlated with UCLA loneliness scale (p<0.05).
Conclusions Perseverative thinking exacerbates burden of ongoing stressors counteractive to psychological well-being. Modifiable factor, our findings underscore value of helping frontline HCPs manage these circumstances.
Keywords
<p>Pandemic stressor; Stress-related consequences; Rumination; Resilience; Social network</p>
Article Details
1. Introduction
Downstream negative consequences of pandemic has generated psychological trauma in frontline Healthcare Workers (HCW). Harsh clinical case load in terms of numbers and complexity paralleled second wave. ICU providers routinely manage patients on organ support, care for patients at end-of-life, and do cardiopulmonary resuscitation making them prone to high incidence for exhaustion, burnout, and post-traumatic stress disorder (PTSD). Social support is an important aspect for psychological well-being the dearth of which leads to perseverative thinking, negatively impacting well-being with increased symptoms of anxiety and depression. Rumination increases psychiatry morbidity. Augmented during pandemic, this resulted in a negative spiral. Resilience, a behavioural characteristic influences adjustment following a stressful event. The only choice available to the front-liners at this stage was to adapt. Aim of this study was to seek wide-ranging assessment of pandemic’s impact on mental health during its second wave. We postulated a model to test our hypothesis (H)- [H1] positive correlation between stress and perseverative thinking, [H2] perseverative thinking is negatively related to resilience, [H3] positive correlation between respondent’s social networking and resilience, a coping mechanism, and [H4] well-being of HCWs was (a) negatively influenced by perseverative thinking while (b) counterbalanced by social networking and resilience.
2. Methods
2.1. Study design
A cross sectional survey was conducted from 15th April - 15th May, 2021 of ER front-liners and ICU providers using purposive sampling. Respondents were invited to participate in this one-time self-administered close ended online questionnaire in English after an informed consent. Research anonymity was assured.
2.2. Method of data collection
Data was collected via Google forms from respondents of multiple institutions. There were no missing data because survey incorporated only mandatory fields of response.
2.3. Demographic information
This included age, gender, place of work, marital status, and number of dependents.
2.4. Research instrument
Key mental health outcomes were measured using validated WHO 5 Well-being Index [1] (WHO-5), Brief Resilience Scale [2] (BRS), UCLA Loneliness Scale [3], Perseverative Thinking Questionnaire [4] (PTQ), Impact of Event Scale – 6 [5] (IES-6), and Berkman-Syme Social Networking Index [6] (SNI). Two additional open-ended questions were, ‘What was your most hopeful experience during the pandemic?’ and ‘What was your most upsetting experience during this phase?’
2.5. Statistical analysis
Data was analysed using SPSS version 25 for Windows (version 25, 2017, IBM Corporation, Armonk, New York, United States) and presented as mean±SD or Frequency (%). Cross tabulations were computed for WHO-5 Well-being index according to gender, age, place of work, marital status, community activity levels and were compared using chi-square test. Mann Whitney U test analysed difference in mean scores of various scales when classified according to gender, age, place of work, marital status and community activity levels. Kruskal Wallis-H test with post hoc Mann Whitney U test was used to analyse difference in mean scores of various scales when classified according to number of dependents. Spearman’s correlation was used to find correlation between various scales. Multiple linear regressions were used to further determine effect of age, gender, place of work, marital status, number of dependents and participation in community activity on various indices. Data presented as B (parameter estimate) with 95% confidence interval and p value. p<0.05 was considered to be statistically significant.
3. Results
Total of 135 responses were obtained. Table 1 shows demographic data of study participants.
|
Frequency (%) |
|
|
Age |
|
|
21-25 years |
45 (33.3%) |
|
25 – 30 years |
26 (19.3%) |
|
31 – 35 years |
33 (24.4%) |
|
36 – 40 years |
15 (11.1%) |
|
>40 years |
16 (11.9%) |
|
Gender |
|
|
Males |
51 (37.8%) |
|
Females |
84 (62.2%) |
|
Place of work |
|
|
ICU |
101 (74.8%) |
|
Emergency room |
34 (25.2%) |
|
Marital status |
|
|
Single |
76 (56.3%) |
|
Married |
59 (43.7%) |
|
Number of dependents |
|
|
0 |
20 (14.8%) |
|
1 to 2 |
37 (27.4%) |
|
3 or more |
78 (57.8%) |
|
Attended community activity |
|
|
Yes |
48 (35.6%) |
|
No |
87 (64.4%) |
Table 1: Demographic data in study participants.
3.1. WHO 5 Well-being Index
Mean score 52.4±23.7 [range: 0-100; scores are changed to percentage by multiplying them with 4.]. Scores ≤ 50 are indicative of poor psychological well-being meriting screening for depression. Overall, 54.1% had normal wellbeing index, 31.9% had low mood and 14.1% were likely depressed. There was a significant association of community activities and WHO-5 (χ2=6.578 p=0.037). Higher percentage of participants (17.2%) who did not participate in any community activity were likely depressed versus those who did (8.3%).
3.2. Brief Resilience Scale
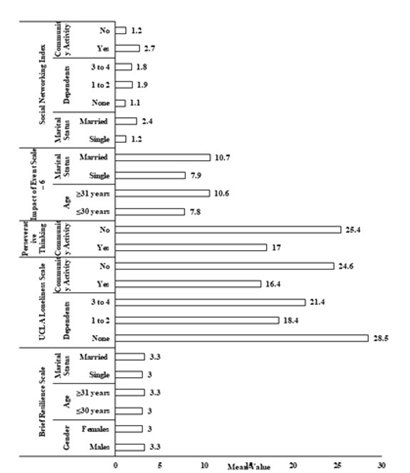
Mean score 3.1±0.5 [range: 1.8-5]. Overall, 39.6% had low resilience, 69.6% had normal resilience and 0.7% had high resilience. BRS varied significantly when classified according to age, gender and marital status (p<0.05) (Figure 1).
3.3. UCLA loneliness Scale
Mean score 21.6±14.3 [range: 0-60]. UCLA score varied significantly when classified according to number of dependents and those who attended community activities (p<0.05) (Figure 1). There was a sobering preponderance of loneliness amongst ER front-liners (UCLA score = 25.4) as opposed to their ICU counterparts (UCLA score = 20.4), however this was not significantly different (p>0.05).
3.4. Perseverative Thinking Questionnaire
Mean score 22.4±11.8 [range: 0-60]. PTQ score was significantly higher for those who did not attend community activities versus those who did (p<0.05) (Figure 1).
3.5. Impact of Event Scale – 6:
Mean score of 9.1±5.6 [range: 0-24]. Age and marital status significant influence on IES-6 (p<0.05) (Figure 1). Even though higher impact was seen in more ER front-liners (IES-6 = 10.2, vs 8.8 in ICU counterparts), this difference was not statistically significant (p>0.05). Overall, 2.5% had normal impact whereas 34.8% had high impact of COVID-19.
3.6. Berkman-Syme Social Networking Index:
Mean score 1.7±1.1 [range: 0-4]. Overall, 42.2% had low social network while 3.7% had high social networking. Marital status, number of dependents and participation in community activities significantly influenced social networking index (p<0.05) (Figure 1).
3.7. Correlation between various scales
|
WHO-5 |
BRS |
Berkman’s SNI |
UCLA Loneliness Scale |
PTQ |
IES-6 |
|
|
WHO-5 |
-- |
0.209* |
0.194* |
-0.327** |
-0.383** |
-0.325** |
|
BRS |
0.209* |
-- |
0.301** |
-0.347** |
-0.375** |
0.12 |
|
Berkman’s SNI |
0.194* |
0.301** |
-- |
-0.351** |
-0.355** |
0.079 |
|
UCLA Loneliness Scale |
-0.327** |
-0.347** |
0.351** |
-- |
0.566** |
0.263** |
|
PTQ |
-0.383** |
-0.375** |
-0.355** |
0.556** |
-- |
0.436** |
|
IES-6 |
-0.325** |
-0.12 |
0.079 |
0.263** |
0.436** |
-- |
|
Data presented as Spearman’s Correlation Value. *p<0.05 for correlation **p<0.01 for correlation |
||||||
Table 2: Correlation of various scales with each other.
Multiple linear regressions (Table 3) were run to determine effect of various parameters on mental health indices. Model for BRS, UCLA, PTQ and SNI was statistically significant. Marital status significantly predicated BRS. Place of work and participation in community activity significantly predicated UCLA loneliness scale and PTQ. Marital status and community activity which are integral part of SNI had significant predictive effect on SNI scale. Even though model for WHO-5 was not significant, participation in community activity had a significant effect on WHO-5 score. Though p value for model constant was significant (p<0.05), individual factors did not have significant predictive effect on IES-6.
Table 3: Risk factors for mental health indices identified by multivariable linear regression.
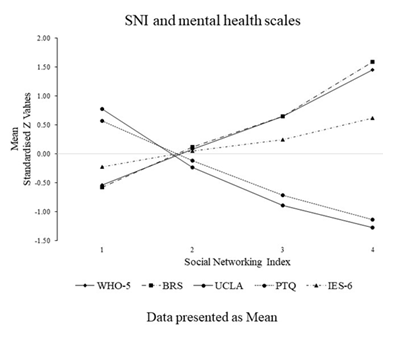
To further explore relation of SNI with other scales, mean standardized Z scores obtained by regression model above were plotted for SNI categories (Figure 2).
Stated hopeful experiences included “getting an opportunity to help those in need, team work, patient recovery, chance to know oneself by getting to spend time alone, and words of recognition from patients who were discharged”. “Lack of civic understanding of gravity of situation, arrogance and naivety of public, inadequate community cooperation towards public health guidelines, mortality, rapidity with which situation had worsened, suffocating experience wearing personal protective equipment, prolonged working hours, victimized, witnessing patients gasping for oxygen amidst non-availability of beds, inability to help the dying, distance from loved ones, death of immediate family members, distrust voiced from next-of-kin, shortage of staff, low salary, stigmatized by colleagues” were the reported upsetting experiences during this phase. Of note, some respondents chose not to respond to these open-ended questions.
4. Discussion
4.1. Interpretation of scales
4.1.1. Measures of positive psychological functioning
WHO 5 Well-being Index- measures current mental wellbeing. It assesses subjective quality of life based on positive mood, vitality, and general interest. The index has a sensitivity of 0.93 with a specificity of 0.83 for detection of depression [7]. Brief Resilience Scale- Resilience depicts a person’s ability to cope with difficulties. It is a distinctive reflection of behavioural response to stress.
4.1.2. Evaluating trans-diagnostic mental health
UCLA Loneliness Scale- each item measures one of 3 dimensions of loneliness [8] 1) social connectedness, 2) relational connectedness, and 3) self-perceived connectedness. Higher scores reflect higher expression of loneliness. Feelings of loneliness are not equivalent of being alone but instead implicate feelings of seclusion, feelings of separation, and feelings of not belonging. Loneliness is linked to mental health issues such as greater chance of depression, anxiety, issues related to sleep, lower sense of worth and higher stress. Perseverative Thinking Questionnaire- rumination on stressful situation is a maladaptive response to stress. It assesses for (1) repetitive intrusive thoughts that can be (2) difficult to disengage, (3) unproductive, (4) capturing mental resources [9].
4.1.3. Measure of mental health symptomatology
Impact of Event Scale- 6- a measure of posttraumatic stress, captures 3 current symptom clusters of PTSD diagnosis viz. re-experiencing, avoidance/numbing, and hyperarousal [6].
4.1.4. Measure of social relationships
Berkman-Syme Social Networking Index- is a combined evaluation of four social connections i.e. marital status, sociability, membership of church group, and other community organizations. Individuals are categorized into socially isolated, moderately isolated, moderately integrated, and socially integrated.
4.2. Our findings
HCWs experienced significant stress during pandemic placing them at risk of psychiatric morbidity. There was a sobering preponderance of depression as seen from place of work and the younger participants. 14.9% of ICU respondents were likely depressed vs 11.8% of ER respondents and 19.7% of those aged </= 30 years vs 7.8% in older counterparts. UCLA Loneliness Scale was negatively correlated with WHO- 5 and SNI. When social needs are not adequately met, feeling of loneliness sets in. Loneliness is an important aspect for one’s well-being and in turn self-resilience. This in turn was associated with perseverative thinking and impact of event. 31.7% of ICU respondents had low resilience vs 23.5% of ER respondents, and 1.6% of those aged >/= 31 years had higher resilience compared to their younger counterparts We found a positive correlation between perseverative thinking and IES- 6 [H1]. Perseverative thinking may have prolonged the time that stressors can have on a persons’ mental well-being [H4a], reducing resilience [H2] and influencing post-traumatic stress. Social networking sustained resilience [H3] and well-being [H4b] with a mutual sustenance [H4a] consistent with our hypothesis of a positive correlation between them.
4.3. Implications of our study
Though the pandemic has shown up as a transitory interlude in normal working, it will depart with a reflective aftermath in the life as well as professional calling of front-liners. Higher incidence of depression in ICU workers could possibly be attributed to long working hours, instilling a feeling of isolation and alienation. Affective rumination prolongs consequences of pandemic stressor. Negative approach interferes with adaptive problem solving increasing risk for negative psychological aftereffect, in the long term. Psychological support may help weaken this link. This non-normative stressor has shown us significance of social support network. Organization support is vital in moderating workplace ostracism of frontline HCWs.
4.4. Limitations of the study
Cross-sectional nature of the survey weakens the ability to make conclusions on cause-and-effect. Sample size of this survey was small. Sampling strategy may result in self-selection bias with those experiencing high levels of stress not participate in the survey concealing the magnitude of negative health impact than what is reported, with social-desirability bias. We did not have a control group of COVID- 19 naïve respondents providing only a partial picture of the psychological burden that this group of frontline HCWs experienced. IES- 6 scale is an abbreviated scale that cannot furnish a clinical diagnosis of PTSD. However, this was not the aim of current survey other than recognizing those with significant traumatic stress symptoms. Lastly, this survey was conducted during second wave of pandemic in the country. If this survey would have been deployed during the first wave, a greater amount of stress might have been revealed with possible lower social connectedness.
4.5. Strengths of the study
Wider range of socio-demographic data helps towards expansive investigations of at-risk groups. Survey team acted rapidly to study facets not included in baseline survey. Shorter scales were utilized to reduce burden on respondents. These scales have demonstrated a high and stable correlation across various demographics. Such research can guide on development of customized interventions for HCWs.
5. Conclusion and Recommendations
Our findings show that pandemic stressor has led to depression, rumination, loneliness and stress in front-liners. Loneliness can affect one’s psychological and physical wellness. Perseverative thinking, a maladaptive response to stress may exacerbate burden of ongoing stressor counteractive to psychological well-being. A modifiable factor, our findings underscore the value of helping ER and ICU professionals deal with these circumstances. Longitudinal study may help understand whether BRS predicts recovery from pandemic work-related stress. Because resilience can be an acquired quality, informative teaching for the healthcare workers may result in lesser symptoms with a reduction in high turnover rate especially of ICU staff. These findings have an institutional and societal bearing.
Acknowledgements
Our sincere gratitude to frontline doctors and nurses who made this survey possible with thanks to their active participation regardless of their busy schedules.
References
- Bech P, Olsen LR, Kjoller M, et al. Measuring well-being rather than the absence of distress symptoms: a comparison of the SF-36 Mental Health subscale and the WHO-Five well-being scale. Int J Methods Psychiatr Res 12 (2003): 85-91
- Smith BW, Dalen J, Wiggins K, et al. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 15 (2008): 194-200.
- Russell D, Peplau, LA. Ferguson ML. Developing a measure of loneliness. Journal of Personality Assessment 42 (1978): 290-294.
- Ehring T, Zetsche U, Weidacker K, et al. The Perseverative Thinking Questionnaire (PTQ): validation of a content-independent measure of repetitive negative thinking. J Behav Ther Exp Psychiatry 42 (2011): 225-232.
- Thoresen S, Tambs K, Hussain A, et al. Brief measure of posttraumatic stress reactions: Impact of Event Scale-6. Soc Psychiat Epidemiol 45 (2010): 405-412.
- Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 109 (1979): 186-204.
- Topp CW, Ostergaard SD, Søndergaard S, et al. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother Psychosom 84 (2015): 167-176.
- Hawkley LC, Browne MW, Cacioppo JT. How can I connect with thee? Let me count the ways. Psychol Sci 16 (2005): 798-804.
- Devynck F, Kornacka M, Baeyens C, et al. Perseverative Thinking Questionnaire (PTQ): French Validation of a Transdiagnostic Measure of Repetitive Negative Thinking. Front Psychol 8 (2017): 2159.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 