A Comparative Study of Functional and Clinical Outcome of Proximal Humerus Fracture Treated with PHILOS Plate
Dr. Abhishek Dhoke1, Dr. Sandeep Bhinde2*, Dr. Vinayak Mani Dwivedi3, Dr. Shubham Nagdev4, Dr. Vipin Kumar Raghuwanshi5
1Senior Resident, Department of Orthopaedics, Shyam Shah Medical College, Rewa, Madhya Pradesh, India
2Associate Professor, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India
3Senior Resident, Department of Orthopaedics, MGM Medical College, Indore, Madhya Pradesh, India
4Senior Resident, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Madhya Pradesh, India
5Senior Resident, Department of Orthopaedics, Dr. Laxminarayan Panday, Govt Medical College, Ratlam, Madhya Pradesh, India
*Corresponding Author: Dr. Sandeep Bhinde, Associate Professor, Department of orthopaedics, R.D Gardi Medical College M.P. India.
Received: 26 June 2025; Accepted: 24 July 2025; Published: 11 August 2025
Article Information
Citation:
Abhishek Dhoke, Sandeep Bhinde, Vinayak mani Dwivedi, Shubham Nagdev, Vipin Raghuvanshi, Vivek Singh. A Comparative Study of Functional and Clinical Outcome of Proximal Humerus Fracture Treated with PHILOS Plate. Journal of Orthopedics and Sports Medicine. 7 (2025): 406-411.
View / Download Pdf Share at FacebookAbstract
Introduction: Proximal humerus fractures (PHFs) are the predominant form of humeral fractures, encompassing a spectrum of injuries affecting the articulating surface, greater tuberosity, lesser tuberosity, or the surgical neck of the humerus. PHFs account for approximately 10% of fractures in patients aged over 65 years. The third most prevalent type of osteoporotic fractures are PHFs, with a lifetime risk of 13% for women aged 50 years and above.
Materials and Methods: As per study criteria 40 patients with fracture of shoulder was included in this study. After admission of patients a detailed, careful history was taken to know the mechanism of injury. Patient was assessed clinically to evaluate general condition; vitals were recorded and examination of fracture site was done. Radiological assessment was done and fracture was classified and preoperative routine haematological investigation was done.
Result: According to NEER’s classification of fractures, 14 (34.41%) cases had two-part fractures, 19 (46.3%) cases had three-part fractures and 8 (19.5%) cases had four-part fractures. Excellent results (score > 89) were noticed in 27 (65.85%) of the instances, good results (scoring 80-89) in 10 (24.39%) and fair results (score 7079) in 4 (9.75%).
Discussion and Conclusion: After a mean follow up of 12 months, the mean Constant score was 88.90 ± 7.31 we recommend the use of the PHILOS plate as a surgical alternative in the management of displaced proximal humeral fractures.
Keywords
<p>Proximal humerus fracture; PHILOS plating; Osteoporotic fractures; Arthroplasty; Osteonecrosis</p>
Article Details
1. Introduction
Proximal humerus fractures (PHFs) are the predominant form of humeral fractures, encompassing a spectrum of injuries affecting the articulating surface, greater tuberosity, lesser tuberosity, or the surgical neck of the humerus [1]. PHFs account for approximately 10% of fractures in patients aged over 65 years [2,3]. The third most prevalent type of osteoporotic fractures are PHFs, with a lifetime risk of 13% for women aged 50 years and above [4,5]. Many treatment methods are available for these types of fractures such as locking plates, arthroplasty, cabling, and nailing [6]. Elderly patients with osteoporotic bone mostly benefit from arthroplasty, whereas younger patients are mainly treated through closed reduction and internal fixation with intramedullary nailing or open reduction and plate osteosynthesis to achieve satisfactory function [7-11]. However, these modalities are associated with various complications such as implant failure, non or malunion, and osteonecrosis of the humeral head [6]. The PHILOS implant, with its anatomically analogous design, is the preferred choice for treating PHFs, as it facilitates angled stabilization and enhances the pull-out strength of osteoporotic bone, thereby improving its ability to withstand physiological loads [12]. This prospective study evaluated the effectiveness of the PHILOS plate in the surgical fixation of two, three- and four-part proximal humeral fractures.
2. Material and Method
2.1 Place and time of study: The study was conducted at the Department of Orthopaedics at R.D. Gardi Medical College, Ujjain. This study was completed within two years after receiving approval from the ethics committee.
2.2 Type of study: This is a prospective observational study. Ethics: Approval from the institutional ethics committee was taken before start of the study. Written informed consent was obtained from all patients before enrolling them for the study. Selection of patients
The patients admitted in the department of orthopaedics with displaced fracture of the proximal humerus were enrolled for this study as per the following exclusion and inclusion criteria.
2.3 Inclusion criteria
- Displaced proximal humerus fracture by
- Neer’s classification.
- Patients older than 18 years of age with proximal humerus fracture.
- Patients willing for surgery.
2.4 Exclusion criteria
- Non-displaced proximal humerus fracture.
- Severely comminuted, open fractures and valgus impacted
- A previous fracture to the proximal humerus, or patients presenting more than three weeks after the injury.
- Pathological fracture from primary or metastatic tumours and skeletally immature patients.
2.5 Method
As per study criteria, 40 patients with fracture of shoulder was included in this study. After admission of patients a detailed, careful history was taken to know the mechanism of injury. Patient was assessed clinically to evaluate general condition, vitals were recorded and examination of fracture site was done. Radiological assessment was done and fracture was classified and preoperative routine haematological investigation was done.
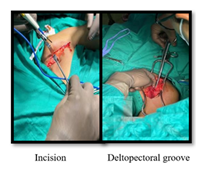
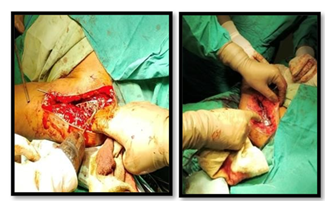
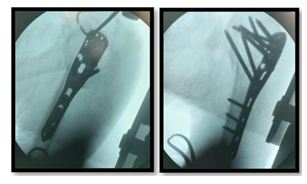
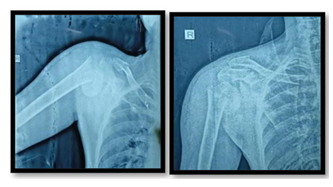
2.6 Surgical procedure
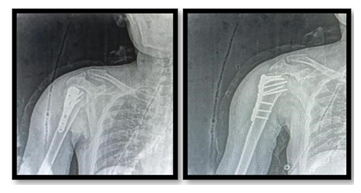
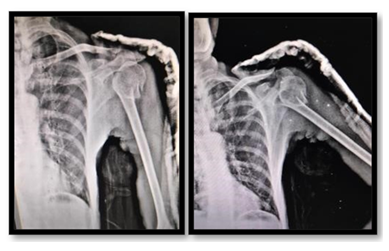
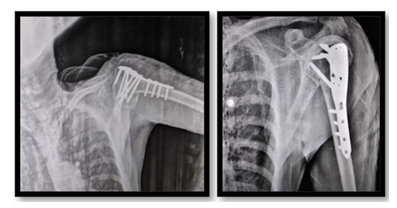
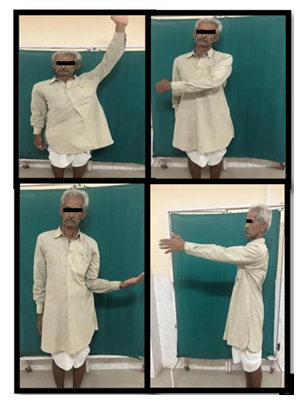
Deltopectoral approach used in all cases. Patient was placed in a supine position employing a deltopectoral approach. Locate the deltopectoral groove. "Initiate the incision just medial to the coracoid at the clavicle and extend it distally along the deltopectoral groove to the deltoid insertion, spanning approximately 15 cm. Develop skin flaps to expose the deep fascia. Use blunt scissors to open the fascia over the deltopectoral groove, ensuring to locate the cephalic vein. Bluntly develop the avascular interval between the deltoid and pectoralis major muscles. The vein can be ligated or retracted with the deltoid. For broader exposure, transecting the muscle origins from the coracoid can be considered. The osseous attachments of the rotator cuff are frequently displaced and require identification and retraction using sharp hook retractors. In cases of fracture-dislocation, reduction of the humeral head is achieved through closed manipulation without opening the joint capsule. K-wires were utilized for preliminary reduction, which was confirmed in both orthogonal views. The PHILOS plate was positioned 5-8 mm posterior to the bicipital groove and 2-4 mm distal to the greater tuberosity. Using the woodpecker technique, the plate was first fastened to the distal fragment, and screws were inserted into the head. An immediate check x-ray was obtained to evaluate the alignment of the bones and confirm that the reduction was ideal. Wound closure with drain beneath the deltoid muscle. Closure of anteromedial raphe, the subcutaneous tissues, and the skin. At the end of surgical procedure sterile dressings applied. No cast or splint was applied. Immediate post-operative x rays were taken in both AP and Lateral views. The patient was followed follow-up for1 year after surgery and the constant score was used for functional assessment higher the score better was the outcome (Figure 1-9).
3. Intra OP Images
Case 1:
Case 2
4. Result
|
Type of fracture |
Number |
Percentage |
|
2 part |
14 |
34.1 |
|
3 part |
19 |
46.3 |
|
4 part |
8 |
19.5 |
|
Total |
41 |
100.0 |
Table 1: Distribution of study subjects according to Type of fracture.
Table 1 represents the study subjects according to type of fracture, it was observed that a majority 46.3% study subjects had 3 part fracture followed by 34.1% having 2 part fracture and lastly only 19.5% had 4 part fracture.
|
CMS score at |
Mean |
SD |
Test statistic value |
p-value* |
|
months |
74.66 |
3.94 |
59.663 |
<0.001(s) |
|
months |
84.2 |
5.52 |
||
|
months |
88.9 |
7.31 |
Table 2: Comparison of overall CMS Scores at 3, 6 and 12 months.
Table 2 compares the overall CMS score among the study subjects at 3 months, 6 months and 12 months, it was observed that there was a significant difference in the overall CMS score at different time period. On comparing, pair wise it was observed that there was a significant increase in the CMS score from 3 months to 6 months, 3 months to 6 months as well as from 6 months to 12 months.
|
Outcome |
Frequency |
Percentage (%) |
|
Excellent |
27 |
65.85 |
|
Good |
10 |
24.39 |
|
Fair |
4 |
9.75 |
|
Total |
41 |
100.00 |
Table 3: Distribution of study subjects according to outcome.
Table 3 represents the study subjects according to months, outcome; it was observed that a majority 65.85% study subjects were in the excellent outcome closely followed by 24.39 % in good outcome lastly 9.75% in fair outcome.
|
Complications |
No. |
Percentage |
|
Yes |
5 |
12.2 |
|
No |
36 |
87.8 |
|
Total |
41 |
100.0 |
Table 4: Represents the study subjects according to complications,
Table 04 represents the study subject according to complication; it was observed that a majority 87.8% study subjects had no complications *Friedman’s test however, 12.2% had some complication.
5. Discussion
In present study the mean age was 61.10 ± 8.01 at different time period. On comparing, pair wise, years. Of the total 41 cases of proximal humerus it was observed that there was a significant fractures. Out of 41 cases, 25(61.0%) were males increase in the CMS score from 3 months to 6 and 16(39.0%) were females. Patients suffering months, from 3 months to 12 months as well as from proximal humerus fractures arrived at our from 6 months to 12 months. Centres as they were part of motor vehicle injuries 27 (65.9%). this was followed by fall from height 14 (34.1%). According to NEER’s classification of fractures, 14 (34.41%) cases had two-part fractures,19 (46.3%) cases had three-part fractures and 8 (19.5%) cases had four-part fractures. Excellent results (score > 89) were noticed in 27 (65.85%) of the instances, good results (scoring 80-89) in 10 (24.39%) and fair results (score 70-79) in 4 (9.75%). After a mean follow up of 12 the mean Constant score was 88.90± 7.31. In 86.8 % of cases, follow-up showed no complication, Shoulder stiffness was the most lastly 9.75% in fair outcome. frequent consequences, followed by persistant pain, screw back out, wound dehiscence. results are comparable with those reported for the PHILOS plate. Ethiraj et al. [13] showed that mean forty patients was 46.8 (2070), with a female: male ratio of 1:2.3 [14].
In this study mean age of patients were 60.32±9.34 years. There was female predominance [13]. The majority of patients were injured as a result of a traffic collision (70%), followed by a fall from a height (17.5%) and other reasons (12.5 %) [14]. Road traffic accident 26(65%) was a most common mode of injury, followed by fall from height 10 (25%) and trivial fall 4(10%) [15]. According to NEER’s classification of fractures, 14 (56.33%) cases had two-part fractures,19 (36.33%) cases had threepart fractures and 8 (19.5%) cases had four-part fractures [19]. According to NEER’s classification of fractures, 46.88% (n=15) cases had two-part fractures, 37.49% (n=12) cases had three part fractures and 9.38% (n=3) cases had four-part fractures whereas 6.25% (n=2) cases. Frankhauser et al. [16] evaluated 29 proximal humeral fractures in 28 patients treated with the Locking Proximal Humerus Plate (LPHP). The mean Constant Murley score was 74.6 after 12 months [17]. In a series of 20 consecutive patients showed favourable early results with surgical treatment of proximal humeral fractures using the PHILOS plate. After a mean follow up of 16 months, the mean Constant score was 76.1. Hente et al. [18] studied 31 patients with displaced 3- and 4-part fractures of the proximal humerus treated with the PHILOS plate. After a mean follow-up of 18.5 months, the mean Constant score was 76 [14]. The constant score was excellent in 20 (50%) patients; it was good in 18(45%) patients and fair in 2(5%) patients. The mean of the constant score was 88.64± 8.42, maximum value was 100 and minimum value was 72 [19]. According to NEER's classification of fractures, 6.25% of cases in our study showed fracture dislocation, whereas 46.88% of cases had two-part fractures, 37.49% had three-part fractures, and 9.38% had four-part fractures. The mean Constant-Murley score at the end of the follow-up period in this study was 85.8 [20]. Of 28 fractures, 20 (71.4%) healed in good anatomical position. At the end of the follow up period, the mean Constant Murley score was 57.9±21.7, and the mean adjusted Constant-Murley score was 67.5±23.6. The results were excellent or good in 16 patients (57.1%), moderate in one patient (3.6%), and poor in 11 patients (39.3%) [13]. The functional outcome was excellent in 2 patients (5%), good in 22 patients (55%), fair in 7 patients (17.5%), and poor in 9 patients (22.5%). The Constant mean score achieved was 68.75±14.03. Mootha et al. [2021] regarding complications of surgery, postoperative infection was found in 2(5%) patients, stiffness of the shoulder was present in 2(5%) patients, one patient developed malunion and Osteonecrosis was present in one patient. Egol et al. [21] studied a cohort of 51 patients treated with PHILOS® plates, reporting that 24% of patients experienced postoperative complications. The most frequent complications observed were screw penetration (16%), osteonecrosis (3.9%), nonunion (3.9%), and infection (2.0%).
6. Conclusion
PHILOS plate offers the advantage of providing a high degree of angular and axial stability. The convergent and divergent arrangement of the locking screws engaging in the humeral head prevents pull out and failure of fixation. It facilitates early mobilization, yielding excellent radiographic and functional results that enable patients to regain good shoulder function and return to work sooner. Considering these factors, we recommend the use of the PHILOS plate as a surgical alternative in the management of displaced proximal humeral fractures.
References
- Butler MW. Chapter 10 - Common Shoulder Diagnoses. In: Cooper C, editor. Fundamentals of Hand Therapy. Saint Louis: Mosby (2007): 150-82.
- Baron JA, Karagas M, Barrett J, et al. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology 7 (1996): 612-8.
- Kim SH, Robert M, Szabo RA. Epidemiology of Humerus Fractures in the United States: Nationwide Emergency Department Sample. Arthritis Care & Research 64 (2008): 407-14.
- Launonen AP, Vesa Lepola A, Saranko T, Flinkkilä M, Laitinen VM. Epidemiology of Proximal Humerus Fractures. Archives of Osteoporosis 10 (2015).
- Johnell O, Kanis J. Epidemiology of Osteoporotic Fractures. Osteoporosis International: A Journal Established as Result of Cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. Osteoporosis International: A Journal Established as Result of Cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 16 (2005): S3-7.
- Südkamp N, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. J Bone Joint Surg Am 91 (2009): 1320-8.
- Neer CSII. Displaced proximal humeral fractures: PART II. Treatment of three- Part and Four-Part Displacement. J Bone Joint Surg Am 52 (1970): 1090.
- Hauschild O, Konrad G, Audige L, et al. Operative versus non-operative treatment for two-part surgical neck fractures of the proximal humerus. Arch Orthop Trauma Surg 133 (2013): 1385-93.
- Olerud P, Ahrengart L, Ponzer S, et al. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 20 (2011): 747-55.
- Lanting B, MacDermid J, Drosdowech D, et al. Proximal humeral fractures: A systematic review of treatment modalities. J Shoulder Elbow Surg 17 (2008): 42-54.
- Plath JE, Kerschbaum C, Seebauer T, et al. Locking nail versus locking plate for proximal humeral fracture fixation in an elderly population: a prospective randomised controlled trial. BMC Musculoskelet Disord [Internet] 20 (2019).
- Gurnani S, Pisal T, Phalak MO, et al. Assessment of surgical outcome in three- and four-part proximal humerus fracture treated with proximal humerus internal locking system (PHILOS) plate versus Neer’s prosthesis in elderly patients. Cureus [Internet] 14 (2022).
- Ethiraj P, Venkataraman S, S J K, et al. Does Proximal Humerus Interlocking System (PHILOS) Plating Provide a Good Functional Outcome in Proximal Humerus Fractures?. Cureus 14 (2022): e26474.
- Aditya Krishna Mootha, Dr. KV Ramana Kumar, Dr. B Saisaran Kumar, et al. A prospective study of outcome of fracture of proximal humerus treated with PHILOS plating. Int J Orthop Sci 7 (2021): 109-112. Clinical Orthopaedics www.orthoresearchjournal.com 2 (2018): 125-128.
- Fankhauser F, Boldin C, Schippinger G, et al. A new locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res 430 (2005): 176-81.
- Koukakis A, Apostolou CD, Taneja T, et al. Fixation of proximal humerus fractures using the PHILOS plate:
- early experience. Clin Orthop Relat Res 442 (2006): 115-20.
- Hente R, Kampshoff J, Kinner B, et al. Treatment of dislocated 3- and 4-part fractures of the proximal humerus with an angle-stabilizing fixation plate. [Article in German] Unfallchirurg 107 (2004): 769-82.
- Jhamnani R, Dhanda M, Surana A. Study of Functional Outcome and Postoperative Complications Among Proximal Humerus Fracture Patients Treated With Proximal Humerus Internal Locking System (PHILOS) Plating. Cureus 15 (2023): e42411.
- Emanuel V. Geiger MD. Department of Trauma, Hand and Reconstructive Surgery, Johann Wolfgang Goethe-University Frankfurt/Main, Theodor-Stern-Kai 7, D-60590 Frankfurt/Main, Germany.
- Egol KA, Ong CC, Walsh M, et al. Early complication of proximal humerus fractures treated with locked plates, J Orthop trauma 22 (2008): 159-64.



 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 