A Correlational Study of Orthorexia and Positive Body Experiences
Ada H Zohar1,2*, Rachel Bachner-Melman1,3, Lilac Lev-Ari1,2
1Clinical Psychology Graduate Program, Ruppin Academic Center, Emek Hefer, Israel
2Lior Zfaty Suicide and Mental Pain Research Center, Emek Hefer, Israel
3Baerwald School of Social Work, Hebrew University Jerusalem, Jerusalem, Israel
*Corresponding Author: Ada H Zohar, Clinical Psychology Graduate Program, Ruppin Academic Center, Emek Hefer, Israel.
Received: 10 December 2023; Accepted: 22 December 2023 2023; Published: 29 December 2023
Article Information
Citation: Ada H Zohar, Rachel Bachner-Melman, Lilac Lev-Ari. A Correlational Study of Orthorexia and Positive Body Experiences. Journal of Orthopedics and Sports Medicine. 5 (2023): 459-468.
View / Download Pdf Share at FacebookAbstract
Background: In this study we tested the hypothesis that positive body experiences would offer some protection from symptoms of orthorexia nervosa (ONs).
Methods: A community sample of 561 adult volunteers aged 19-72 was recruited via social media networks. Participants self-reported on measures of ONs [DOS], compulsive exercise [CET], positive body experiences [DKB-35] including body acceptance, body narcissism, vitality, sexual satisfaction and physical contact, and disordered eating [EDE-Q-13].
Results: 2.2% [95%CI 1.1-3.7%] of the participants scored above the clinical cut-off point for ON. All positive body experiences except physical contact were significantly and negatively correlated with all disordered eating subscales. ONs correlated negatively with body acceptance and sexual satisfaction, and compulsive exercise correlated negatively with vitality, and positively with body narcissism. Body acceptance and sexual satisfaction were lowest for the group who scored above the clinical cutoff for orthorexia nervosa. In a linear regression analysis, positive body experiences contributed 14% to the explained variance, over and beyond the negative contribution of education. Body acceptance down-moderated the association between compulsive exercise and ONs.
Conclusions: Positive body experiences, in particular body acceptance and sexual satisfaction may be protective of ONs. Further research is needed to identify factors that offer protection from ONs and can therefore be targeted in treatment and prevention programs.
Keywords
<p>Orthorexia nervosa symptoms; Positive body experiences; Compulsive exercise, body acceptance; Body narcissism; Sexual satisfaction</p>
Article Details
Plain English Summary:
Orthorexia nervosa, a rigid, obsessive focus on healthy eating, is paradoxically detrimental to health, leading to extreme food restriction and often compulsive exercise. We examined whether positive body experiences would offer some protection. Self-report questionnaires were administered to 561 adult volunteers from the community, about orthorexia symptoms, compulsive exercise, positive body experiences (body acceptance, body narcissism, vitality, sexual satisfaction and physical contact), and disordered eating. All positive body experiences except physical contact were protective of disordered eating. Education was protective against orthorexia symptoms, and positive body experiences were protective of orthorexia, in particular body acceptance and sexual satisfaction. Treatment and prevention programs for orthorexia should focus not only on trying to contend with the symptoms which are causing suffering and distress, but also on enhancing the positive aspects of one’s body, accepting its form and weight, and deepening sexual satisfaction.
1. Background
Orthorexia nervosa (ON), a disordered eating pattern characterized by an attempt to eat for one’s health, in an ever-restrictive and proscriptive manner, has been a subject of study since the early 2000s. Bratman and Knight’s [1] book on the topic had the catchy title “Health Food Junkies” and its second chapter was entitled “A Disease Disguised as a Virtue.” The conception of ON as eating pathology disguised as a healthy lifestyle has been widely accepted.
ON is not a diagnostic entity and does not appear in the feeding and eating disorders chapter of the DSM-5 [2] or in the ICD-11 [3]. There are several issues that need to be resolved before it can be defined as an eating disorder and made a formal diagnosis. First and foremost, it may be a phase in the course of an extant eating disorder such as anorexia nervosa (AN) or bulimia nervosa (BN) or some combination of both. To establish it as a separate and new diagnosis, research over a period of a decade and longitudinal studies are required. It is also not clear if ON is a passing cultural phenomenon, or if it is here to stay [4]. However, full blown ON poses a serious threat to physical and mental health, and thus constitutes a clinical challenge for treatment.
The book by Bratman and Knight [1] helped to expedite research by them and others, aimed at suggesting diagnostic criteria for ON should there be a decision to include it as an eating disorder [1, pp 5-17; [5-7]] and identifying correlates of this condition and risk factors for developing it. Bundros et al. [8], found that ON symptoms (ONs) correlated with disordered eating and obsessive-compulsive symptoms, and were more common in respondents with high weight and those of Latino-Hispanic extraction. In their review of psychosocial risk factors for ON, McComb and Mills [9] identified as psychological and personal risk factors perfectionism, obsessive-compulsive traits, poor body image and low self-esteem, as well as a history of an eating disorder and current psychopathology. In an attempt to differentiate between correlations and predictors, Messer et al. [10] conducted a short-term prospective study with community volunteers and found that overvaluation of weight and shape at baseline predicted an increase in ONs over a three-month period. A compendium of risk factors for ON compiled by a panel of experts [6, p 5] includes participation in competitive sports, athletic performance concerns, and frequent physical exercise, as well as many others. However, the panel of experts did not list any protective factors.
Prevalence estimates for ON are limited by the fact that ON is not a diagnostic entity. Thus, research has relied on ON symptom inventories that yield continuous scores rather than dichotomous diagnoses. However, Barthels and colleagues suggested cut-off points for three levels of ON symptoms as measured by the Düsseldorf Orthorexia Scale [11]: clinical level symptoms (score 30 and above); high-risk for ON (score 25-29, or 95th percentile); and low risk (score below 25). Using these cut-off points, Barthels and colleagues [12] identified 1-2% of the general German population as clinical-level ON while Depa et al. [13] found a higher prevalence in German college students of 3.3%. Chard et al. [14] found a prevalence of clinical level ON of 8.9% in American college students. The differences between American and German students suggest a cultural influence on ON prevalence; moreover the higher prevalence in student’s vs. the general adult community in Germany may indicate a rising secular trend in ONs, ON and compulsive exercise are closely linked [15]. As individuals at risk for ON develop their beliefs and attitudes about healthy eating, they often immerse themselves in physical exercise as well [16]. A diet regimen that grows in its rigidity and restriction over time is often accompanied by an increasingly rigorous and demanding exercise regimen. Often a ritualized interdependence between food consumption and exercise develops, with a combination of specific eating or restricting behaviours and exercise practices. Zohar et al. [17] showed a strong correlation between ONs and compulsive exercise. Moreover, both could be perceived as possible outcomes of the samset of risk factors that included insecure attachment, emotional dysregulation, disordered eating, and the parental feeding practices of restricting and monitoring their child’s food intake.
Both ON and compulsive exercise are related to a range of disordered eating behaviours, and not only to restriction. Barthels et al. [18] found that individuals in the community who reported more severe ONs also reported more frequent bingeing and purging. Zohar et al. [17] found that the individuals who scored above the clinical cut-off point for ON, reported significantly more restriction, bingeing and purging than those below the cut-off point [17]. This suggests that ONs go beyond extreme restriction and may swing between extremes of restriction, bingeing, and even purging, as a way of compensating for the loss of control over eating.
There is less research on protective factors for ON than for risk factors. Since positive body experiences are protective against eating disorders and disordered eating [19], it seems likely that they also offer protection from ONs and extremes of disordered eating in this context. Positive body experiences include accepting one’s body rather than rejecting it, taking pleasure in showing it to others, feeling vigorous and fit, experiencing sexual satisfaction, and engaging in casual, affiliative body contact [20]. Fewer positive body experiences are reported by patients with eating disorders than by patients with other psychiatric disorders [20], and these experiences are positively associated with the subjective well-being of individuals both with and without eating disorders [21]. Barthels et al. [18] found that respondents with more severe ONs reported experiencing the positive body experiences of body acceptance and sexual satisfaction less than the respondents with less severe ONs.
In general, much more research attention has been dedicated to risk factors than to protective factors in the field of psychopathology. The aim of the current study was to examine further the potential protective role of positive body experiences on ONs and compulsive exercise.
The study hypotheses were that:
- Positive body experiences will correlate negatively with disordered eating.
- Positive body experiences will correlate negatively with both ONs and compulsive exercise.
- The three groups defined by their level of ON symptomatology will be different for their positive body experiences; Individuals above the cutoff point for clinical ON will have the lowest levels of positive body experiences.
- Positive body experiences will contribute negatively and significantly to explained variance in ONs.
2. Methods
2.1 Participants
As described in Zohar et al. [10], 561 adult community volunteers ranging in age between 19 and 72 years of age (M=32.7+11) were recruited via social media networks. No exclusionary criteria other than age 18 and over were applied. Recruitment through Facebook pages and Whatsapp groups resulted in participants who were internet-connected. Completing the extensive self-report necessitated reading Hebrew, so participants whose Hebrew did not suffice probably did not attempt to participate. About 10% of the potential participants did not complete the self-report and were not included in the analyses. In general, online surveys tend to sample middle-class educated adults. Ninety-three (17.09%) of the participants were male. In general, participants had a high level of education, reporting between 12 and 25 years of education (M=15), so that most were college graduates. Their self-reported BMIs ranged from 15-55 (M=23.58+4.49). The sample could thus be characterized as educated Israeli Jewish adults.
2.2 Measures
Orthorexic eating behaviors and associated emotions were assessed using the 10-item Düsseldorf Orthorexia Scale (DOS; 22). A sample item is “My thoughts constantly revolve around healthy nutrition and I organize my day around it”. Each item is rated on a scale of 1–4 and the clinical cut-off point is 30, with respondents scoring 25-29 considered to be at risk for ON [22]. The English translation of the original German has good psychometric properties [22]. The English version was translated into Hebrew for the purpose of this study, with permission from the authors. It was translated into Hebrew and independently back-translated into English by two bilingual translators, who resolved discrepancies and agreed on the final wording. In this study Cronbach's alpha was α=0.83.
Level of compulsive exercise was assessed by the 24-item Compulsive Exercise Test (CET; [23]). A sample item is “I feel extremely guilty if I miss an exercise session”. Each item is rated on a scale of 0-5. The CET has good internal consistency, with Cronbach's alpha between 0.85-0.88 [8,24]. The questionnaire was translated into Hebrew, with permission from the authors, in the same way as the DOS. In this study the CET had an internal reliability of α=0.93.
Positive Body Experiences were assessed using the Dresdner Body Image Inventory-35 (DKB-35; 13). This inventory has five subscales: Body acceptance (BA) as in “there are many situations in which I feel satisfied with my body”; vitality (V) as in “I feel physically fit”; sexual satisfaction (SS) as in “I feel my body pleasantly and intensely in sexuality”; body narcissism (BN) as in “I find it pleasant and stimulating when someone looks at me attentively” and physical contact (PC) as in “physical contact is important to me to express closeness”. The DKB-35 was written in German and validated in clinical [20] and non-clinical samples. The DKB-35 in Hebrew has excellent psychometric properties [25]. It was validated against the Eating Disorders Examination – Questionnaire – 13 (EDE-Q-13), with all five subscales of the EDE-Q-13 correlating negatively and significantly with disordered eating [26]. Items are rated on a scale of 1-5. In the current study the internal reliabilities of the subscales were α=0.83 for V; α=0.91 for BA; α=0.89 for SS; α=0.74 for BN; and α=0.92 for PC.
Disordered eating was measured by the Eating Disorders Examination – Questionnaire-13 (EDE-Q-13; 26). The EDE-Q-13 is a short version of the EDE-Q, a 28-item questionnaire that assesses disordered eating attitudes and behaviors over the previous 28 days (EDE-Q; 27). The measure has been validated in Hebrew and has good psychometric properties [26]. It includes five subscales: Eating restraint, as in “On how many of the past 28 days have you tried to exclude from your diet any food that you like, in order to influence your shape or weight?”), body dissatisfaction, as in “On how many of the past 28 days have you been dissatisfied your weight?”, shape and weight over-evaluation, as in “On how many of the past 28 days have you been dissatisfied your shape?”, bingeing, as in “On how many of the past 28 days did you have a sense of having lost control over your eating (at the time when you were eating)?” and purging, as in “On how many of the past 28 days have you taken laxatives as a means of controlling your shape or weight?”. Responses are noted on a scale of 0-6. In this study, the Cronbach alpha coefficient for disordered eating was α=0.89.
2.3 Procedure
The study was approved by the Institutional Review Board. Participants were sent a link to the questionnaires via Qualtrics (www.qualtrics.com). On the opening screen, potential participants were given information about the study’s aims and content, and were informed they withdraw their participation at any point. Those participants who subsequently provided informed consent and completed the measures described above were included in this study. No compensation was offered for participation [27]. APA ethical guidelines were adhered to throughout. The anonymized data has been deposited at https://zenodo.org/record/8167063.
2.3.1 Data Analyses Pearson correlations were used to measure bivariate associations between the variables. A MANOVA was conducted to assess between-group differences for ONs and the other study indices. Hierarchical linear regression was used to test for the protective role of positive body experiences. Moderation analyses [28] were conducted using the Process Macro for SPSS. All analyses were tested for statistical significance at the p < 0.05 level. Statistical Package for the Social Sciences (SPSS, version 28) was used for all analyses.
3. Results
3.1 Prevalence of ON and its relationship to age
Of the 556 participants, 12 or 2.2% [95% CI 1/1-3/7%] scored above the cut-off point of 30 for clinical level symptoms of ON on the DOS. 36 or 6.4% [95% CI 4/6-8/9%] scored 25-29 on the DOS, i.e. are defined as “at risk” for ON. Merging these two categories results in 8.7% [95% CI 6/4-11/3%] of the sample at risk or having clinical level ON symptoms. We further explored the prevalence of ON, by dividing our sample into student age, 19-30, (N=308), and older adults 31-72 years of age (N=200). Clinical level ON, was present in 9 or 2.6% [95% CI 1.2-5%] of the younger adults, and 3 or 1.4% [95% CI 0/3-4/0%] of the older adults; Hhowever, the difference in the rates did not reach statistical significance. For at risk and clinical level ON symptoms together, 32 or 9.4% [95% CI 7-13%] of the younger adults scored 25 and above on the DOS and 16 or 7.2% [95% CI 4-12%] of the older adults. Again although the prevalence was numerically higher in the younger adults the rates were not statistically different.
3.2 Hypothesis 1: Positive body experiences will correlate negatively with disordered eating
To test this hypothesis, Pearson correlations were calculated between the study variables. Table 1 below shows that with the exception of physical contact, all positive body experience subscales were significantly and negatively correlated with all disordered eating subscales. Hypothesis 1 was therefore largely supported.
|
Restraint |
Shape and weight concerns |
Body dissatisfaction |
Purging |
Binging |
|
|
Vitality |
-.12** |
-.26*** |
-.39*** |
-.25*** |
-.11* |
|
Body acceptance |
-.40*** |
-.60*** |
-.72*** |
-.37*** |
-.22*** |
|
Body narcissism |
-0.01 |
-.14*** |
-.26*** |
-.10* |
-0.08 |
|
Sexual satisfaction |
-.13** |
-.26*** |
-.29*** |
-.17*** |
-.20*** |
|
Physical contact |
-.02 |
-.06 |
-.08 |
-.04 |
-.01 |
|
Note: DKB-35 subscales: Vitality, body acceptance, body narcissism, sexual satisfaction, physical contact. EDE-Q-13 subscales: Restraint, shape and weight concerns, body dissatisfaction, purging, binging. |
|||||
Table 1: Inter-correlations between positive body experiences and disordered eating subscales.
3.3 Hypothesis 2: Positive body experiences will correlate negatively with ONs and with compulsive exercise.
To test this hypothesis, Pearson correlations were calculated between the relevant variables. As can be seen from Table 2, ONs correlated significantly and negatively with body acceptance and sexual satisfaction, but not with the other three subscales of the DKB-35, vitality, body narcissism and physical contact. Compulsive exercise correlated significantly and negatively with vitality, and positively with body narcissism, but not with the other three positive body experience subscales. Hypothesis 2 was therefore partially supported.
|
CE |
Vitality |
Body acceptance |
Body narcissism |
Sexual satisfaction |
Physical contact |
MEAN (SD) |
|
|
ONs |
.53** |
.05 |
-.22** |
.06 |
-.10* |
-.03 |
17.0 (5.2) |
|
CE |
.26** |
-.11* |
.16** |
-.00 |
-.02 |
3.22 (1.0) |
|
|
Vitality |
.58** |
.41** |
.41** |
.19** |
3.42 (0.8) |
||
|
Body acceptance |
.57** |
.50** |
.19** |
3.15 (0.9) |
|||
|
Body Narcissism |
.47** |
.27** |
2.91 (0.7) |
||||
|
Sexual satisfaction |
.10* |
2.48 (1.0) |
|||||
|
Physical contact |
2.98 (0.4) |
||||||
|
Note: ONs=Orthorexia nervosa symptoms (DOS); CE= Compulsive exercise (CET); DKB-35 subscales: Vitality, body acceptance, body narcissism, sexual satisfaction, physical contact (DKB-35). *p<.05; **p<.01; ***p<.001 |
|||||||
Table 2: Inter-correlations between orthorexia nervosa symptoms, compulsive exercise and positive body experiences.
3.4 Hypothesis 3: Individuals above the cut-off point for clinical ON will have the lowest levels of positive body experiences
To test this hypothesis, we conducted a 3×5 MANOVA. The independent variable was group (low DOS score, at risk DOS score and clinical DOS score) and the dependent variables were the five scales of positive body experience. The overall model was statistically significant (F(10,1006)=4.05, p<.001). As can be seen in Figure 1, body acceptance was lowest for the group who scored above the clinical cut-off on the DOS and highest for the group with the lowest DOS scores (F(2,506)=6.74, p<.001). Sexual satisfaction was also lowest for the group who scored above the clinical cut-off on the DOS and highest for those with the lowest DOS scores (F(2,506)=5.32, p<.01). No other significant between-group differences emerged. Scheffe’s post hoc tests for body acceptance and sexual satisfaction revealed significant differences between the three groups. Hypothesis 3 was therefore supported in part.
As the at risk for ON and probable ON had small sample sizes, we decided to combine them into one group. After testing the difference between two groups, we found the same results as the previous MANOVA test. A significant difference was found between the groups (F(5,503)=7.36, p<.001; see Table 3). Low risk ONs had higher body acceptance and higher sexual satisfaction than high risk and probable ONs.
|
Low risk ON (n=463) Mean (SD) |
At risk and probable ON (n=46) Mean (SD) |
F(1,507) |
|
|
Vitality |
3.41 (.78) |
3.44 (.79) |
.07; p=.79 |
|
Body acceptance |
3.20 (.90) |
2.70 (1.13) |
12.28; p<.001 |
|
Body narcissism |
2.91 (.66) |
2.98 (.76) |
.51; p=.48 |
|
Sexual satisfaction |
3.39 (.93) |
2.98 (1.19) |
7.78; p=.005 |
|
Physical contact |
2.98 (.40) |
3.00 (.41) |
.13; p=.72 |
|
Note: ON=Orthorexia nervosa (DOS); DKB-35 subscales: Vitality, body acceptance, body narcissism, sexual satisfaction, physical contact (DKB-35). *p<.05; **p<.01; ***p<.001 |
|||
Table 3: Differences between at risk and probable ON (n=46) and low risk (n=463) on positive body experiences.
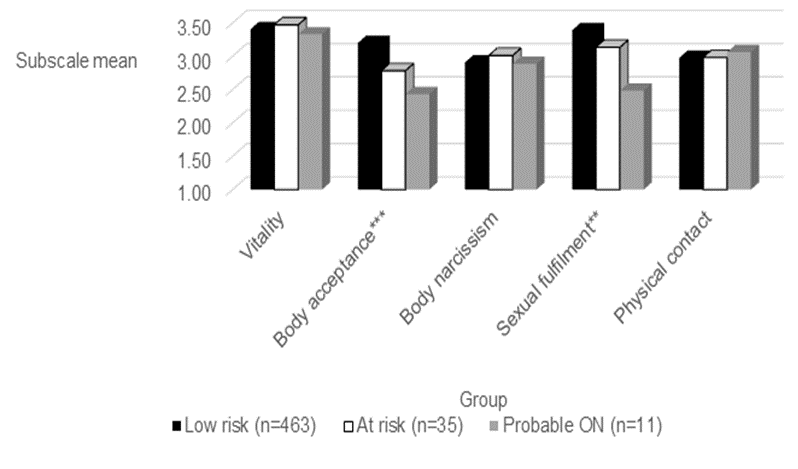
Figure 1: Between-group differences in ONs for body positive experiences (n=509).
Note: ON=Orthorexia nervosa; *p<.05; **p<.01; ***p<.001
3.5 Hypothesis4: Positive body experiences will contribute negatively and significantly to explained variance in ONs.
To test this hypothesis, we ran a hierarchical linear regression. In the first step we entered age, education, gender and BMI. In the second step we added the scores for the five positive body experience subscales. As can be seen in Table 4, in step 1, the background variables contributed 1% explained variance, most of which was due to the negative effect of age on ONs. In step 2, an additional 14% explained variance was contributed by positive body experiences, beyond the negative contribution of education. Altogether, body acceptance was the largest single contributor to ONs, and was negative as expected. Less expected were the positive and significant contributions of body narcissism and vitality to ONs. Sexual satisfaction had a negative contribution, but failed to reach significance. Hypothesis 3 was therefore partially supported.
|
Standardized β |
t |
Adj. R2 |
R2 |
F(df) |
p |
|
|
Step 1 |
.01 |
.02 |
2.40(4,506)* |
0.49 |
||
|
age |
0.051 |
1.008 |
314 |
|||
|
gender |
0.036 |
0.806 |
0.421 |
|||
|
education |
-.148** |
-3.027 |
0.003 |
|||
|
BMI |
-0.003 |
-0.068 |
0.946 |
|||
|
Step 2 |
.15 |
.16 |
10.98(9,501)*** |
<.001 |
||
|
age |
.101* |
2.159 |
0.031 |
|||
|
gender |
-0.006 |
-0.142 |
0.887 |
|||
|
education |
-.120** |
-2.639 |
0.009 |
|||
|
BMI |
-.101* |
-2.184 |
0.029 |
|||
|
VT |
.243*** |
4.725 |
<.001 |
|||
|
BA |
-.502*** |
-8.245 |
<.001 |
|||
|
BN |
.294*** |
5.524 |
<.001 |
|||
|
SS |
-0.083 |
-1.654 |
0.099 |
|||
|
PC |
-0.058 |
-1.346 |
0.179 |
|||
|
Note: VT=Vitality, BA=Body acceptance, BN=Body Narcissism, SS=Sexual satisfaction, PC=Physical contact (DKB-35). *p<.05; **p<.01; ***p<.001 |
||||||
Table 4: Hierarchical linear regression for orthorexia nervosa symptoms by positive body experiences.
3.5 Hypothesis 5: Positive body experiences will down-moderate the positive effect of compulsive exercise on ONs
Since Body acceptance, Body narcissism, and Vitality were statistically significant in the regression analysis above (albeit the latter two in the opposite direction), we conducted moderation analyses for these variables using Process Macro 3.4 [22], with CE as the independent variable and ONs as the dependent variable.
Figure 2 shows the moderating role of body acceptance on the association between compulsive exercise and ONs (p=.04). Overall, those scoring high on compulsive exercise had higher ONs scores than those scoring low on compulsive exercise. However, for participants with high body acceptance, high compulsive exercise was more weakly associated with ONs than for participants with low body acceptance. People with high compulsive exercise and low body acceptance were most likely to have high ONs scores.
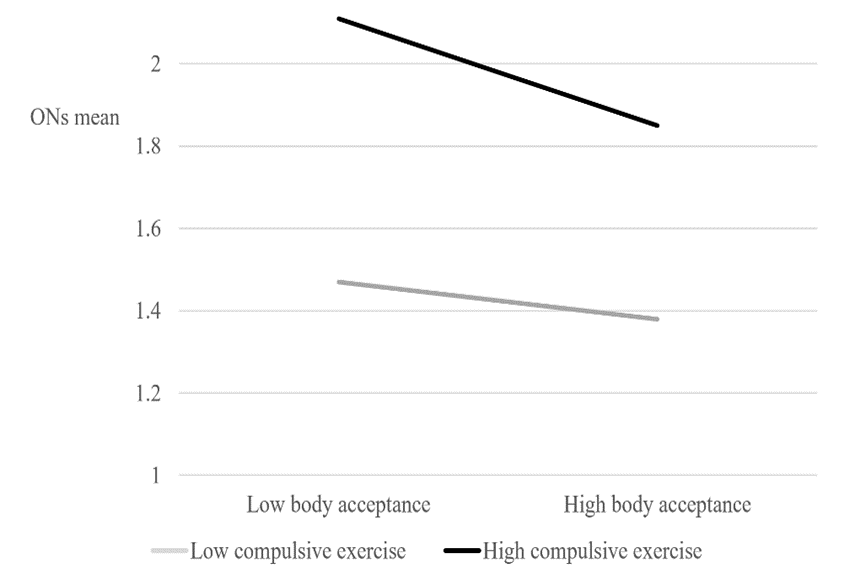
Figure 2: Moderating effect of body acceptance on the link between compulsive exercise and ONs.
Note: ONs=Orthorexia nervosa symptoms (DOS).
Body narcissism and vitality did not moderate the association between compulsive exercising and ONs. This part of Hypothesis 5 is rejected.
4. Discussion
The current study found that the positive body experiences of body acceptance and sexual satisfaction are significantly and negatively associated with ONs, In addition, the analysis of variance showed significant group differences in both body acceptance and sexual satisfaction between the three levels of ONs defined by Chard and her colleagues [22]; Clinical, at risk and low risk. Further support was provided by a regression analysis showing that the five positive body experience subscales contributed 14% of the explained variance in ONs, over and beyond the negative contribution of education. In addition, body acceptance negatively and significantly down moderated the effect of compulsive exercise on ONs, so that individuals who were higher in body acceptance and also compulsive exercisers, had lower levels of ONs.
The protection against ONs that body acceptance confers is reassuring and hardly surprising. Our findings replicate those of Barthels et al. [18], who found that community volunteers with many ONs reported lower body acceptance and sexual satisfaction than those with few ONs. Body acceptance can be seen as the inverse of body dissatisfaction, a core feature and diagnostic criterion of both anorexia and bulimia nervosa [2, pp 338 and 345 respectively). In their systematic review, Linardon et al. [29] provide overwhelming evidence for the protective role of body acceptance for both disordered eating and eating disorders. Whereas the negative association between body acceptance and ONs is not unexpected, it suggests that ON falls within the eating disorder spectrum.
Sexual satisfaction has not been widely studied in the context of eating disorders, so that the protective role we found for sexual satisfaction against ONs is an important one. Blais et al. [30] found that sexual satisfaction and disordered eating were negatively correlated in service and veteran women, and that sexual satisfaction had a mediating role in promoting relationship satisfaction. Lev-Ari et al. [26] found a negative correlation between sexual satisfaction and disordered eating in a large community sample. Individuals with clinical eating disorders experience both sexual dysfunction [31] and low sexual satisfaction [32]. Bachner-Melman et al. [33] found that individuals with a current eating disorder reported lower sexual satisfaction than individuals without a current eating disorder. Our finding that individuals with elevated ONs reported diminished sexual satisfaction is therefore in line with Barthels et al. [18] results and other research on levels of sexual (dis)satisfaction in people with disordered eating and eating disorders.
Unlike the other positive body experience subscales, body narcissism was positively, rather than negatively, associated with ONs. Far from playing a protective role, it significantly predicted ONs in a linear regression analysis. This finding was surprising, since Bachner-Melman et al. [33] observed a significant positive association between body narcissism and recovery from an eating disorder and Lev-Ari et al. [26] observed a significant negative correlation between body narcissism and eating disorder symptoms. The items in the body narcissism subscale e.g., “I find it pleasant and stimulating when somebody looks at me attentively” and “I use my body to attract attention” reflect pride and enjoyment from showing one’s body to others. Intuitively, this seems to imply enjoyment and thus acceptance of one’s body. It is nevertheless possible that in the context of ONs, body narcissism signifies self-objectification, which is associated with disordered eating [34], low self-esteem and symptoms of anxiety and depression across cultures [35]. It is important to point out that Barthels et al. [18] found no significant relationship between body narcissism and ONs, so that support for the connection between these variables is inconsistent, and should be further examined in research.
The role of positive body experiences in this study was observed both indirectly as well as directly, as some variance was also accounted for by the positive body experiences down-moderating the influence of compulsive exercise on ONs. Since ONs and compulsive exercise seem to be synergic [17], it is possible that positive body experiences dampen this positive feedback loop.
Although this study identified some positive body experiences as being protective against ON, it must be noted that their contribution is considerably weaker than that of known risk factors. Risk factors, such as compulsive exercise, disordered eating, emotion dysregulation, insecure attachment and parental feeding practices account for even more of the variance in ONs [17]. The relative weakness of protective vs. risk factors for orthorexia is disappointing since targeting protective factors is an effective strategy in prevention programs [36]. Whereas the list of risk factors in the consensus paper by Donini et al. [6] is quite long, no consensus was reported on protective factors. Research on protective factors from eating disorders in general has so far been limited. It is possible that positive body experiences play a protective role against the development of eating disorders [33]. Linardon [29] found that positive body image, intuitive eating, and self-compassion at baseline were protective against the onset of eating disorders. Further research is needed on protective factors for eating disorders in general, and for ON in particular, and positive body experiences should be further examined in this context.
The prevalence found for clinical level ON in Jewish Israeli adults in the community, of 2.2%, is very similar to the 1-2% found for adult Germans in the community [12]. Examination of prevalence by age did not yield significant differences between those under and over 30 in the current study. Further research is required in order to look for cultural and ethnic influences as well as secular trends in the prevalence of ON.
This study should be considered in the light of its limitations. It is a cross-sectional correlational study, so that interpretations about a risk-promoting or protective role for positive body experiences are, in fact, speculative. All measures were self-reported and thus social desirability might have influenced respondents’ reports. The sample was adequate in size and varied in age and education, but was a convenience rather than a random sample. The proportion of individuals above the clinical cut-off point for ON was small so that our findings may not be applicable to people with this purported clinical disorder. Many potential confounders were not measured, such as symptoms of depression and anxiety, perfectionism, and obsessive-compulsive symptoms.
A prospective study that included several time-points and clinical observation as well as self-reports would greatly enrich our understanding of the development of ON and ONs, and help to identify specific risk and protective factors.
5. Declarations
Ethical Approval: The study was approved by the IRB of Ruppin Academic Center, CP_108_2022. Participants signed their informed consent on the opening screen of the online self-report.
Competing interests: The authors declare no competing interests.
Authors' contributions:
AHZ conceived the study, oversaw its execution, curated the data, conducted some of the statistical analysis, and wrote the initial draft of the manuscript. LLA contributed to the statistical analyses, to the interpretation of the results, and to revisions of the text. RBM contributed throughout the process from the conception of the study until the last editing and revisions of the manuscript as it stands.
Funding:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials: The data has been deposited and can be accessed at https://zenodo.org/record/8167063 and will also be made available upon request from the corresponding author.
References
- Bratman S, Knight D. Health Food Junkies: The rise of orthorexia nervosa-The health food eating disorder. New York: Broadway (2000).
- Diagnostic and Statistical Manual of Mental Disorders (5th, text rev.; DSM-5-TR; American Psychiatric Association (2022).
- International Statistical Classification of Diseases and Related Health Problems (11th ed,; ICD-11; World Health Organization (2021).
- Neliubina AS, Sidorovich OI, Sysoeva EA. Orthorexia Nervosa as A Cultural Phenomenon. In: Martsinkovskaya T, Orestova V (Eds.), Psychology of Personality: Real and Virtual Context. European Proceedings of Social and Behavioural Sciences, European Publisher 94 (2020): 538-544.
- Cena H, Barthels F, Cuzzolaro M, et al. Definition and diagnostic criteria for orthorexia nervosa: a narrative review of the literature. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity 24 (2019): 209-246.
- Donini LM, Barrada JR, Barthels F, et al. A consensus document on definition and diagnostic criteria for orthorexia nervosa. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity 27 (2022): 3695-3711.
- Dunn TM, Bratman S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eating behaviors 21 (2016):11-7.
- Bundros J, Clifford D, Silliman K, et al. Prevalence of Orthorexia nervosa among college students based on Bratman's test and associated tendencies. Appetite 101 (2016): 86-94.
- McComb SE, Mills JS. Orthorexia nervosa: A review of psychosocial risk factors. Appetite 140 (2019): 50-75.
- Messer M, Liu C, McClure Z, et al. Negative body image components as risk factors for orthorexia nervosa: Prospective findings. Appetite 178 (2022): 106280.
- Barthels F, Meyer F, Pietrowsky R. Duesseldorf Orthorexia Scale construction and evaluation of a questionnaire measuring orthorexic eating behavior. Zeitschrift Fur Klinische Psychologie Und Psychotherapie 44 (2015): 97-105.
- Barthels F, Pietrowsky R. Orthorectic eating behavior nosology, and prevalence rates. Psychotherapie Psychosomatik Medizinische Psychologie 62 (2012): 445-449.
- Depa J, Schweizer J, Bekers SK, et al. Prevalence and predictors of orthorexia nervosa among German students using the 21-item-DOS. Eat Weight Disord 22 (2017): 193-199.
- Chard CA, Hilzendegen C, Barthels F, et al. Psychometric evaluation of the English version of the Düsseldorf Orthorexie Scale (DOS) and the prevalence of orthorexia nervosa among a US student sample. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 24 (2019): 275-281.
- Oberle CD, Watkins RS, Burkot AJ. Orthorexic eating behaviors related to exercise addiction and internal motivations in a sample of university students. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity 23 (2018): 67-74.
- Yilmaz H, Karakus G, Tamam L, et al. Association of orthorexic tendencies with obsessive-compulsive symptoms, eating attitudes and exercise. Neuropsychiatric Disease and Treatment 14 (2020): 3035-3044.
- Zohar AH, Zamir M, Lev-Ari L, et al. Too healthy for their own good: Orthorexia nervosa and compulsive exercise in the community. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity 28 (2023): 1-9.
- Barthels F, Kisser J, Pietrowsky R. Orthorexic eating behavior and body dissatisfaction in a sample of young females. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity 26 (2021): 2059-2063.
- Linardon J. Positive body image, intuitive eating, and self-compassion protect against the onset of the core symptoms of eating disorders: A prospective study. International Journal of Eating Disorders 54 (2021): 1967-1977.
- Pöhlmann K, Roth M, Brähler E, et al. The Dresden Body Image Inventory (DKB-35): validity in a clinical sample. Psychotherapie, Psychosomatik, Medizinische Psychologie 64 (2013): 93-100.
- Lev-Ari L, Zohar AH, Bachner-Melman R. Enjoying your body: The psychometric properties of an English version of the Dresden Body Image Questionnaire. Australian Journal of Psychology 72 (2020): 267-275.
- Chard CA, Hilzendegen C, Barthels F, et al. Psychometric evaluation of the English version of the Düsseldorf Orthorexie Scale (DOS) and the prevalence of orthorexia nervosa among a US student sample. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity 24 (2019): 275-281.
- Taranis L, Touyz S, Meyer C. Disordered eating and exercise: development and preliminary validation of the compulsive exercise test (CET). European Eating Disorders Review 19 (2011): 256-268.
- Plateau CR, Shanmugam V, Duckham RL, et al. Use of the compulsive exercise test with athletes: norms and links with eating psychopathology. Journal of Applied Sport Psychology 26 (2014): 287-301.
- Zohar AH, Ari LL, Bachner-Melman R, et al. The Well Rounded Body Image: The Dresdner Korperbildfragebogen DKB-35 in Hebrew. Israel Journal of Psychiatry and Related Sciences 54 (2017): 22-27.
- Lev-Ari L, Bachner-Melman R, Zohar AH. Eating Disorder Examination Questionnaire (EDE-Q-13): expanding on the short form. Journal of Eating Disorders 9 (2021): 57.
- Fairburn CG, Beglin SJ. Eating disorder examination questionnaire. Cognitive behavior therapy and eating disorders 309 (2008): 313.
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (Third Ed.). New York: The Guilford Press. (Second edition published in (2018); First edition published in (2013).
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ) (2013).
- Linardon J, McClure Z, Tylka TL, et al. Body appreciation and its psychological correlates: A systematic review and meta-analysis. Body Image 42 (2022): 287-296.
- Blais RK, Monson CM, Livingston WS, et al. The association of disordered eating and sexual health with relationship satisfaction in female service members/veterans. Journal of Family Psychology 33 (2019): 176.
- Pinheiro AP, Raney TJ, Thornton LM, et al. Sexual functioning in women with eating disorders. International Journal of Eating Disorders 43 (2010): 123-129.
- Spivak-Lavi Z, Gewirtz-Meydan A. Eating disorders and sexual satisfaction: The mediating role of body image self-consciousness during physical intimacy and dissociation. The Journal of Sex Research 59 (2022): 344-353.
- Bachner-Melman R, Lev-Ari L, Zohar AH, et al. The eating disorders recovery questionnaire: psychometric properties and validity. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity 26 (2021): 2633-2643.
- Xiao L. A Review of Self-Objectification Research. World Scientific Research Journal 8 (2022): 381-384.
- Gattino S, Czepczor-Bernat K, Fedi A, et al. Self-Objectification and its Biological, Psychological and Social Predictors: A Cross-Cultural Study in Four European Countries and Iran. Europe's Journal of Psychology 19 (2023): 27.
- Davydov DM, Stewart R, Ritchie K, et al. Resilience and mental health. Clinical psychology review 30 (2010): 479-495.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 